Abstract
Background
Ingestion of infective eggs and cysts of faecal orally transmissible parasites has been linked with the level of environmental and personal hygiene. The possibility of contamination of food with eggs and cysts by infected food vendors has also been recorded.
Objectives and methods
This study was aimed at assessing the prevalence of parasites with direct transmission and the level of hygiene among food vendors. Stools of randomly selected food vendors selling in schools and streets in Abeokuta were examined for ova and cysts of parasites using formo-ether concentration method. Questionnaires, interviews, and field observation were also used to assess the activities of food vendors.
Results
Ninety-seven (97%) percent of the food vendors were infected with one or more faecal-orally transmissible parasites while 3% were free from such parasites; Parasites observed were Entamoeba histolytica with a prevalence of 72% Ascaris lumbricoides (54%), Enterobius vermicularis (27%), Trichuris trichiura (24%) and Giardia duodenalis (13%). School food vendors recorded lower prevalence of infection (92%) than the street food vendors (98.7%) (P>0.05) Fifty-two percent (52%) of the food vendors have dewormed in the last four years; Eighty percent (80%) of this were school food vendors. Infections with helminthes were recorded in 63.5% of the dewormed food vendors. Food vendors involved in child care activities were found to be more infected than those not involved in such activities. Toilet facilities available to the vendors were mainly pit latrine and other related structure (75%) while 25% had access to water system closets. During hawking, dung hills were majorly used for defaecation. Hand washing after defaecation did not include the use of soap in the few vendors that were involved in hand washing.
Conclusion
There is need to enact food handling policies and implementation of such policies ensured in order to reduce transmission of oral faecal parasites.
Keywords: Food vendors, parasites, infection, feacal, helminths
Introduction
Parasitic infections, which have direct life cycle and do not need an intermediate host to infect a new host and are spread via faecal contamination of food and drinks are often referred to as faecal orally transmitted parasites. Infections acquired through direct ingestion of infective eggs or cyst is intimately linked with the level of personal hygiene and sanitation in the Community. The lack of latrines and adequate sewage disposal facilities has been known to contribute to the spread of the infective stages of the parasite thereby bringing about a widespread contamination of food and drinks.
Infections can also be acquired through contaminated unwashed fingers, insects, circulation of bank notes and by wind during dry conditions.6 Contamination of food with eggs and cysts especially those hawked by food vendors7 may also serve as a source of infection to consumers of such items.
These parasites include Entemoeba histolytica Giardia duodenale, Trichuris trichiura, Ascaris lumbricoides and Enterobius vermicularis. Ameobiasis is known to cause about 450 million infections per annum in developing world with an incidence of about 50 million and 100,000 deaths.3 Giadiasis is more common in children and has a worldwide prevalence of about 1– 30 percent (Woo and Paterson 1986. Ascarasis is the commonest nematode of man especially in tropical Africa with a prevalence of about 40% in Ogun State of Nigeria (Reinthaler et al 1988) and may be as high as 96–100 in the rural communities in Ogun State.1
The resistant capacity of the eggs and cysts of these parasites is a feature of profound influence on the epidemiology. Eggs of Ascaris can remain viable for up to six years.6
The control of parasites utilizing the faecal-oral route of transmission will depend on the knowledge of the factors contributing to the spread of such infection, therefore, this study aims at investigating the activities of food vendors (in schools and on the streets) and their effect on the distribution of these parasites in Abeokuta, Ogun State.
Materials and methods
Study area: Abeokuta a town in Ogun State is located approximately 7° 11'N and 3° 21'E in the rainforest belt. Temperature ranges between 22.8° C – 34.9° C. The residents are predominantly of the Yoruba ethnic group.
Survey method: The target populations were food vendor(in schools and on the streets) selling food items that are consumed directly (without the need to cook before consumption). The school food vendors sell food and fruits to school children within school premises; they are routinely subjected to stool examination for parasites and are regularly dewormed and enlightened about food handling by health officers from the ministry of health unlike the street vendors. The schools and streets used were randomly selected. The study was first introduced to the food vendors and their consent was obtained. Consented food vendors were given well labeled universal tubes in which they placed a little lump of freshly passed stool. The stool samples were later taken to the laboratory where direct smear method and formol ether concentration methods were used as described by W.H.O.11
Questionnaires were also administered to the food vendors to acquire information such as age, educational qualification, their knowledge, attitude and practices as regards parasite infestation. Oral interviews and field observations were also used to assess handling of food items and the activities of consumers.
Data analysis: Collected data were entered into a computer using Epi info version 6 software (CDC,Atlanta) and analysed accordingly. Chi-square method was used to test for significance in proportions.
Results
Food hawking is a common activity in Abeokuta with a very high patronage from low-income earners and traders. One hundred food vendors were examined for faecal - orally transmissible parasites (73 females and 27 males). There were 82 adults and 18 children.
The school food vendors (25) and the street food vendors (75) were the two main categories of food vendors observed in this study (Table 1). A higher proportion (59%) of the vendors has primary education especially among the school vendors while more of those with secondary education were found on the street. Fifteen percent of the vendors were without formal education, more of which were seen in schools.
Table 1.
Sex and age distribution of food vendors
| Vendors | Sex | Group | ||
| Male | Female | Adult | Children | |
| School (25) | - | 25 | 25 | - |
| Street (75) | 27 | 48 | 57 | 18 |
Ninety-seven (97) percent of the food vendors were infected with one or more faecal-orally transmissible parasites while 3% were free from such parasites; 66% of which were school food vendors. Prevalence of infection was found to be higher among street vendors (98.7%) than the school food vendors (92%)
Faecal orally transmissible parasites observed were Entamoeba histolytica recording the highest prevalence (72%) followed by Ascaris lumbricoides (54%) then Enterobius vermicularis (27%), Trichuris trichiura (24%) and Giradia duodenalis (13%) (Table 2). Children food vendors had higher prevalence of parasite infestation than the adult food vendors except in infection with E.histolytica which was higher among adult food vendors (Table 3). Cases of multiple infections were recorded in 67 vendors. There were more incidence of double infection compared to single or triple(p>0.05)The school vendors recorded more of single and double infection while the street vendors recorded more of double, triple or more infection (p>0.05)(Table 4). The infected vendors were however asymptomatic
Table 2.
Percentage distribution of parasite species among food vendors
| Parasite | Number of vendors examined |
Number of infection | % distribution in population |
| E. histolytica | 100 | 72 | 37.9 |
| A. lumbricoides | 100 | 54 | 28.4 |
| E.vermicularis | 100 | 27 | 14.2 |
| T. trichiura | 100 | 24 | 12.6 |
| G.duodenalis | 100 | 13 | 6.8 |
Table 3.
Percentage parasite distribution between adult and children food vendors.
| Parasite | Number of infection | %Children infection | %Adult infection |
| E. histolytica | 72 | (11) 57 | (61) 75 |
| A. lumbricoides | 54 | (13)68 | (41) 50 |
| E. vermicularis | 27 | (8) 42 | (19) 23 |
| T. trichiura | 24 | (7) 36 | (17) 20 |
| G. duodenalis | 13 | (9) 47 | (4) 4 |
Table 4.
Level of mixed infection by age among food vendors.
| School vendor | Street vendor | Total | |||||||
| Infection | Child | Adult | Total | Child | Adult | Total | Child | Adult | Total |
| Single | 0(0) | 11(47.8) | 11(47.8) | 4(22.2) | 14(25.0) | 18(24.3) | 4(22.2) | 25(31.7) | 29(29.9) |
| Double | 0(0) | 11(47.8) | 11(47.8) | 6(33.3) | 27(48.2) | 33(44.6) | 6(33.3) | 37(46.8) | 43(44.3) |
| Triple or more |
0(0) | 1 (4.4) | 1 (4.4) | 8(44.4) | 15(26.8) | 23(31.1) | 8(44.4) | 17(21.5) | 25(25.8) |
| Total | 0 | 23 | 23 | 18 | 56 | 74 | 18 | 79 | |
Prevalence of Entamoeba histolytica was found to be higher among the school food vendors (80%) than the street food vendors (69.3%) (p >0.05).
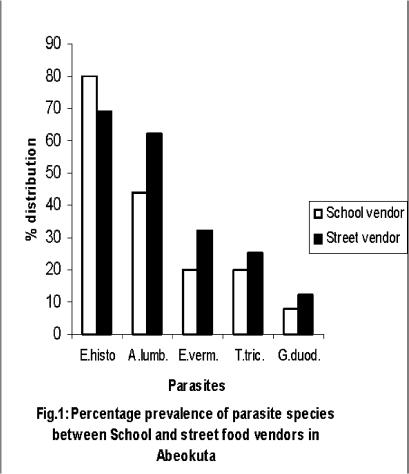
The prevalence of the other parasites was higher among the street food vendors (fig 1). The difference were however not statistically significant (P> 0.05).
Fig. 1.
Percentage prevalence of parasite species between School and street vendors in Abeokuta
Fifty-two percent (52%) of the food vendors had taken within the last 4 years drugs targeted at expelling worms, (20 of these were school food vendors consistuting 80% drug use among school food vendors) while 48% did not or remember using any antihelminthic drug. The drugs used were combatrin (Pyrantel Pamoate) and Ketrax (Levamisole). The difference in drug usage between the school and street vendors were found to be statistically significant (P< 0.05).
However, despite the use of the antihelminthic drugs, infection with helminthes were recorded in (33) 63.5% of the treated food handlers and 42 (80.8%) of them had protozoan infection.
Food vendors involved in child care activities such as changing diapers, cleaning children after defecation, packing faeces dropped on the floor were found to be more infected than those not involved in such activities.
Toilet facilities and hygiene status.
Only 25% of the food vendors have water system closets in their homes. 75% use pit latrine and other related structures. However, most of the food vendors do not have access to any toilet facility whenever they are out hawking; they therefore make use of dung hills and nearby bushes after which they clean up using sheets of papers; leaving their hands unwashed after defaecation.
The school food vendors make use of water in cleaning their hands after defaecation but none included the use of soap in such activity. They consider the use of soap an additional cost.
Food items were seen exposed to insects' contacts especially among the street vendors while all the school food vendors covered their wares neatly.
Knowledge Attitudes and Practices of Food Vendors
Eight-five percent (85%) of the food vendors (mostly street vendors 63 (84.0%) were of the opinions that worms are part of the human body and ‘’everybody was born with them and will die with them. They therefore considered deworming a fruitless effort. Some of the vendors (60%) also added that worms are useful in the body and that stomach aches are as a result of consuming food that the worms do not like. Knowledge, attitude and practices of school vendors were generally better than the vendors on the street.
Discussion
The high prevalence of faecel orally transmissible parasite recorded in this study (97%) is indicative of a high level of faecal contamination of the environment and low level of sanitation 6 since these parasites are acquired via accidental consumption of parasite eggs and cysts.
This prevalence signals high possibility of transmission of these parasites through these infected food vendors to their customers especially in cases where such food vendors are unhygienic in food handling. The facts that these food handlers are asymptomatic make them cysts and/ or egg passers and are unaware that they are possible transmitters of parasitic infections/diseases.
The lower incidence of infection among the school food vendors implies that the routine inspection and supposed periodic deworming have a reducing effect on infection especially with helminthes. Children are known to be more vulnerable to parasitic infection than adults because of their level of exposure to parasite eggs and cysts, their level of hygiene and immunity to infection. 5,6,8 This may account for higher prevalence of infection recorded among children food vendors (Table 3). The drugs used in deworming these groups of vendors were combatrin and ketrax which are only effective against helminthes and not protozoan parasites. This may be responsible for the high incidence of protozoan parasites (80.8%) among dewormed food vendors and a high prevalence of Entamoeba histolytica among school food vendors (80%) Fig. 1.
Infection with helminthes recorded in the dewormed vendors indicate re-infection with these parasites which may be as a result of high level of environmental contamination with helminth eggs; coupled with the fact that faecal-oral mode of transmission is the easiest and commonest mode of transmission of parasites in Abeokuta.4 The use of drugs for treatment of faecal orally transmitted parasites is less effective if factors promoting transmission have not been removed.6
Vendors involved in child care activity may have acquired infection from infected children since close relationship with infected children may predispose to infection.2
These vendors may also serve as ‘bridge’ of transmission of parasitic infection between infected children and consumers of their wares.
Poverty may be responsible for the prevalence and or re-infection with these parasites since the use of soap in cleaning of hands after defaecetion is considered an additional cost even by the school food vendors that are aware of the need for hygienic practices in food handling. None of the food vendors met the W.H.O requirement for effective hand wash which include washing of hands in hot soapy water before preparing food and after using the bathroom, changing diapers and handling pets.10 Ignorance is also a contributing factor to high prevalence of infection especially among the street food vendors.6 Majority of the food vendors (75%) use pit latrine and other related structures and/or dung hills for defecation, these structures may however, facilitate contact with stools from which they can either acquire infection or carry eggs and cysts of parasites with which contamination of their wares may be inevitable thereby leading to widespread contamination of food and drinks.
In addition, lack of public toilet may be one of the factors of epidemiology since food hawkers make use of dung hill for defaecetion while hawking their wares. The exposure of food items by street food vendors facilitated contact of insect with such food items, thereby increasing possible contamination, of such items with eggs and cyst of parasites since insects have been identified as carriers' of eggs and cysts of parasites.6
The routine inspection and enlightenment by health officers from the ministry of health may have enhanced the level of awareness among the school vendors.
This study has revealed the need to improve personal hygiene of food vendors in Abeokuta in order to reduce the prevalence of faecal-orally transmissible parasites. Based on this, there is the need for adequate enlightenment programmes for food handlers especially street food handlers. There is also the need to enact necessary food handling policies and appropriate implementation of such policies should be ensured. Thirdly, more public toilets should be provided in Abeokuta in order to reduce faecal contamination of the environment.
References
- 1.Mafiana CF, Sam-Wobo SO, Akinsete AA. Epidemiology of Ascariasis in some rural communities in Ogun State, Nigeria. Global Journal of Pure and Applied Sciences. 2000;6(1):23–26. [Google Scholar]
- 2.Obiamiwe B A, Nmorsi P. Human Gastro-Intestinal Parasite in Bendel State, Nigeria. Angrew Parasitol. 1991;32:177–136. [PubMed] [Google Scholar]
- 3.Ravdin J, editor. Amoebiasis: Human Infection by Entamoeba histolytica. New York: John Wiley and Sons; 1988. pp. 105–109. [Google Scholar]
- 4.Reinthaler FF, Mascher F, Klem G, Sixl W. A survey of gastrointestinal parasites in Ogun State, South west, Nigeria. Ann Trop Med Parasitol. 1988;82:181–184. doi: 10.1080/00034983.1988.11812226. [DOI] [PubMed] [Google Scholar]
- 5.Smyth JD. Animal Parasitology. UK: Cambridge University Press; 1994. pp. 351pp. 388–409. [Google Scholar]
- 6.Ukoli FMA. Introduction to parasitology in tropical Africa. New York: John Wiley and Sons; 1990. pp. 15–18.pp. 201–350. [Google Scholar]
- 7.Umeche N. Parasite ova and cysts in fruits in Calabar, Nigeria. The Nigeria Journal of Parasit. 1991;12:85–87. [Google Scholar]
- 8.Warren K. Immunology and Molecular Biology Of Parasitic Infections. Oxford: Blackwell Scientific Publications; 1993. pp. 25–31. [Google Scholar]
- 9.Woo PT K, Paterson W B. Giardia lamblia in children in day-care centers in Southern Ontario, Canada, and susceptibility of animals to G. lamblia. Transaction of the Royal Society of Tropical Medicine & Hygiene. 1986;80:56–59. doi: 10.1016/0035-9203(86)90195-1. [DOI] [PubMed] [Google Scholar]
- 10.World Health Organisation, author. Informal meeting on strategies for control of amoebiasis. WHO Ref: CDD/ PAR/ 1984;84:2. [Google Scholar]
- 11.World Health Organisation, author. Basic Laboratory Methods in Medical Parasitology. Geneva: World Health Organisation; 1991. [Google Scholar]