Abstract
Background
A 36-item version of the Response Inventory for Stressful Life Events (RISLE) was derived from the longer 100-item version. The 36-item version may be more appropriate for use in larger population sample.
Objective
To compare the responses of the 36-item RISLE to interview derived psychiatric diagnoses and suicidal ideation in a sub-sample of the general population and student samples reported in the accompanying paper.
Methods
Clinical interviews using the Mini International Neuropsychiatric Interview (MINI) were carried out on 67 members of the general population and 58 members of the student samples. Receiver Operating Characteristic (ROC) curves were constructed for the RISLE responses using current depressive disorder, any current psychiatric disorder, and past month suicidality variables. Sensitivities, specificities, predictive values and likelihood ratios were determined based on various cut-off points based on ROC curves. Kappa statistic was determined to evaluate the level of agreement between the result of questionnaire surveys and research clinical interviews at different cut-off points on the RISLE.
Results
The probability of correct detection of current depression was 79%, any current psychiatric disorder 83% and past month suicidality 83%. The optimal cut-offs for the general population was 10 and for the students 6. High scores on the 36-item RISLE were associated with a past history of suicide attempt and recent and past suicide ideation.
Conclusion
The 36-item RISLE appears to have good concurrent validity and may be a reasonable screening instrument for psychological distress in the Ugandan population. The results suggest that the RISLE alone is capable of screening for both depressive mood and suicidal ideation effectively at different cut-off points. Thus the RISLE is capable of achieving what normally takes two scales such as the BDI and BSS to do separately. However, further validation work is required using larger population samples in clinical interviews in prospective studies.
Introduction
Depression1–4 and suicide ideation5–10 are prevalent in the general population. However many cases of depression remain undiagnosed and do not receive appropriate medication or general psychosocial intervention. The present study investigated the feasibility of using a screening instrument to enhance the recognition and diagnosis of depression and significant suicidal thoughts in the general population. The accompanying paper11 presented the RISLE and the means by which the longer, 100-item version, was reduced to a more practical 36-item version. Since the instrument has to be utilized clinically it is essential to validate the shorter 36-item version as a screening instrument. This paper presents the results of further validation of the 36-item RISLE by comparing it to the results of clinical research diagnostic interviews conducted on a sub-sample of the original population and student samples.
Method
Study populations
For the further validation of the 36-item RISLE, subsamples of the population sample from the Adjumani District and from the fresher student sample described in Ovuga et al12–14 were used.
General population sample
At the beginning of questionnaire surveys in Adjumani district, every alternate participant out of a sub-sample of 117 respondents was informed that the author or his assistant would interview him or her further. Each of the participants selected for clinical interviews was notified that the outcome of his or her interview would be explained to him or her in confidence, and that appropriate advice for further action would be provided if required. At the end of questionnaire surveys interviewers selected 57 alternate respondents for research clinical interviews.
Student Sample
At the start of questionnaire surveys, the first author notified the participating students that all students who consented to participate in the study would be requested to report for clinical interviews within 2 weeks of the surveys. The first author informed students that he or his assistant would provide confidential feedback and appropriate advice to every student on the outcome of clinical interviews immediately after the interviews. Research clinical interviews were conducted for 58 students within three weeks of questionnaire surveys. A Master of Science clinical psychology student carried out ten interviews and the first author conducted the rest.
Research Clinical Interviews
Interviews were conducted using the Mini International Neuropsychiatric Interview (MINI)15. Interviewers were not aware of the RISLE scores of the subjects that were interviewed as data entry and analysis had not yet been carried out.
The MINI is a standardized clinical diagnostic interview schedule for DSM-IV Axis-I disorders. The instrument is a highly structured interview schedule, which uses diagnostic algorithm based on ICD-10 (WHO, 1987)16, and DSM-1V (APA, 1992)17. It can be reliably administered by lay interviewers using appropriate training. The depression, manic, anxiety, alcohol dependence, post-traumatic stress disorder, and past month suicidality modules of the schedule were used in the study. DSM-IV diagnoses are made according to diagnostic algorithms, which require a fixed number of symptoms, a minimum duration of symptoms as distressing, and a definite impairment of social functioning as a result of symptoms. The MINI was translated by independent translators; translated back and forth into the local languages of the participating communities by the interviewers under the supervision of EO, and pre-tested during a one-week intensive training workshop for the five interviewers and two research assistants. The training workshops were conducted in the district hospital in each district. Comments received from participants during the pre-testing exercise were used to modify the instrument where necessary.
Establishing the gold standard
Using the MINI, three standards were used to compare to the RISLE: current DSM-IV depressive disorder; any current DSM-IV psychiatric disorder (depressive disorder, anxiety, manic, alcohol dependence, post-traumatic stress disorder); and suicide ideation at clinical interview. The depression module of the MINI was used to make clinical diagnosis of any current depressive disorder, and the manic, anxiety, alcohol dependence or post-traumatic stress disorder modules were used to make additional diagnosis of any current psychiatric disorder. The proportion of respondents with suicide ideation, and risk of suicide potential among respondents over the preceding month was estimated using the suicidality module on the MINI.
Data management and analysis
Data was entered using Epi Info version 6.04 and analyzed with SPSS version 11.0. Receiver operating characteristic curves (ROC) 18, 19 were constructed for the shortened RISLE instrument using current depressive disorder, any current psychiatric disorder that considered all respondents with a psychiatric disorder, and past month suicidality rates derived from clinical interviews with the MINI. The ROCs were used to determine specificities, sensitivities for the new short form of the RISLE. Cohen's kappa values for the degree of agreement between the RISLE and clinical interview results were calculated to determine optimal cut-off points on the revised RISLE for students and members of the general population. Sensitivities, specificities, predictive values and likelihood ratios were calculated for varying cut-off scores of the 36-item RISLE.
Results
General population
Clinical interviews identified 49 out of 57 respondents (86.0%) who met DSM-IV diagnostic criteria for any current psychiatric disorder. Of the 57 respondents 35 (61.4%) met DSM-IV diagnostic criteria for any current depressive disorder.
Student population
Of the 101 students who completed study questionnaires, 58 (57.4%) agreed to be interviewed. Nineteen out the 58 respondents (32.8%) met diagnostic criteria for any current psychiatric disorder according to the MINI; nine students out of the 58 (15.5%) met clinical criteria for current depressive disorder. In 15 of 19 (78.9%) cases with any current psychiatric disorder, respondents had two or more diagnoses. The demographic characteristics of the students who participated in clinical interviews were not significantly different from those who did not take part in clinical interviews.
ROC analysis
The student and general population samples were combined for this analysis in order to increase the number of subjects available for analysis. ROC curves were constructed separately for current depressive disorder, any current psychiatric disorder, and past month suicidality (figures 1–3). The area under the curve represents the probability that an individual with a positive screen on a survey instrument has depressive disorder, any current psychiatric disorder or high risk suicide ideation.
Figure 1. ROC for any current psychiatric disorder among 115 study participants.
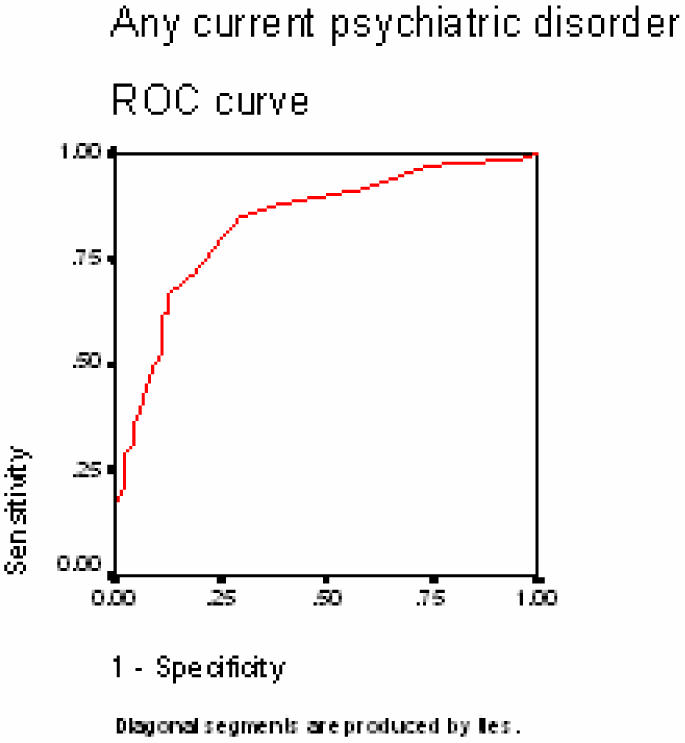
* Area under curve = 0.836 (95% CI 0.760–0.911)
Figure 3. ROC for past month suicidality among 115 study participants.
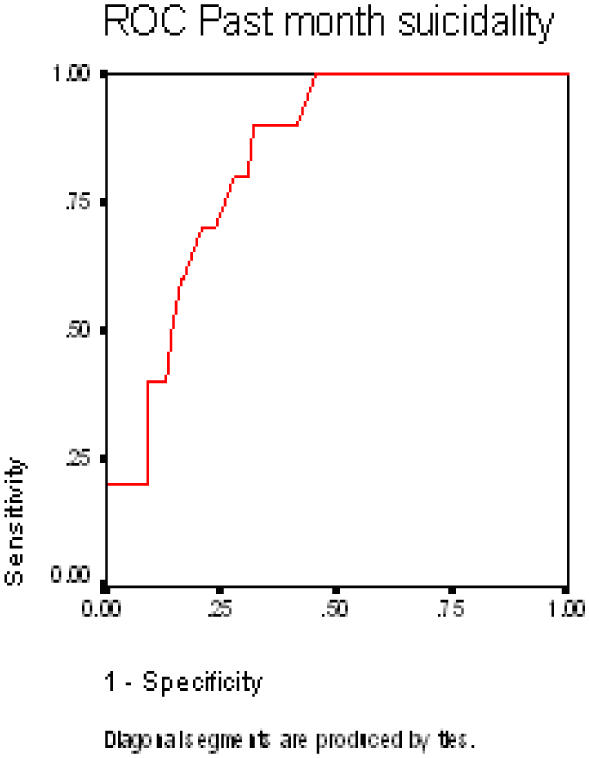
‡ Area under curve = 0.834 (95% CI 0.742–0.926)
The probability of a correct detection of an individual with current depressive disorder was fair at 79%; with any current psychiatric disorder the probability of a correct detection was good at 83%, and with past month suicidality probability was 83%.
Agreement between the RISLE and Clinical Interview Method
Cohen's kappa values indicated that the best agreement between the revised 36-item RISLE and clinical interview with the MINI among students for any current psychiatric disorder was achieved at a cut-off point of 6 (kappa = 0.501), and among the general population, the cut-off point was 10 (kappa = 0.508).
Cut-off Points and RISLE Sensitivity, Specificity
Table 1 depicts the sensitivities, specificities, positive predictive values and positive likelihood ratios of the 36-item RISLE. At a cut-off point of 6 for combined general population and student samples for any current psychiatric disorder, sensitivity was 88.1%, specificity was 60.4%, positive predictive value was 75.6%, negative predictive value was 78.4%, false positive rate was 11.9%, false negative rate was 39.6%, and positive likelihood ratio was 1.9.
Table 1.
Properties of the 36-item RISLE based on ROC curve with any current psychiatric disorder as selection variable derived from clinical interviews using the MINI.
| Risle cutoff | Sensitivity (%) |
Specificity (%) |
Positive Predictive value (%) |
Negative Predictive value (%) |
False Positive Rate (%) |
False Negative Rate (%) |
Likelihood Ratio |
| 5 | 94.0 | 33.3 | 66.3 | 80.0 | 6.0 | 66.7 | 1.0 |
| 6* | 88.1 | 60.4 | 75.6 | 78.4 | 11.9 | 39.6 | 1.9 |
| 10† | 74.6 | 77.1 | 82.0 | 68.5 | 25.4 | 22.9 | 3.6 |
| 12 | 68.7 | 83.3 | 85.2 | 65.6 | 31.3 | 16.7 | 5.1 |
| 15‡ | 61.2 | 87.5 | 87.2 | 61.8 | 38.8 | 12.5 | 7.0 |
| 19 | 40.3 | 91.7 | 87.1 | 52.4 | 59.7 | 8.3 | 10.5 |
| 20§ | 35.8 | 93.8 | 88.9 | 51.1 | 64.2 | 6.3 | 14.1 |
Cut-off point for student sample
Cut-off point for the general population
Cut-off point for past month suicidality
Cut-off point for probably clinically significant current psychiatric disorder
At a cut-off point of 10 for the combined samples for any current psychiatric disorder, sensitivity was 74.6%, specificity was 77.1%, positive predictive rate was 82.0%, negative predictive rate was 68.5%, false positive rate was 25.4%, false negative rate was 22.9% and positive likelihood ratio was 3.6.
Using a cut off of 10 the prevalence of current depressive disorder according to the 36-item RISLE among the general population was 61.1% and from the clinical interview technique was 61.4%. The prevalence rates among students at a cut-off point of 6 were 19.8% for the RISLE and 13.8% for clinical interview method. The prevalence of any current psychiatric disorder among members of the general population (cut point 10) and among students (cut point 6) according to the RISLE and clinical interview method were 89.6% and 86.0% respectively. The rates among students (cut point 6) for any current psychiatric disorder were 41.6% and 32.7% respectively.
Relationship between RISLE and suicidal behavior and ideation
People with scores of 10 or more on the 36 item RISLE were more than twice as likely to be associated with a past history of suicide attempt than those with scores of 9 or less (OR=2.25, 95% CI = 1.34–3.96, X2 = 9.61, df = 1, P = 0.002); almost four times as likely to be associated with lifetime suicide urge (OR=3.86, 95% CI =2.60–5.67, X2 = 53.01, df = 1, P = 0.0000) and almost three times as likely to be associated with lifetime death wish (OR=2.87, 95% CI = 2.00–4.18, X2 = 35.43, df = 1, P = 0.0000). Scores of 10 or above were also associated with presence of suicide ideation within the past week defined as suicide urge or death wish (OR=2.33, 95% CI = 1.32–4.40, X2 = 8.64, df = 1, P = 0.003).
Demographic characteristics, medical histories and RISLE performance
The individual demographic characteristics, histories of suicidal attempts and ideation, family history of completed suicides and attempts, and psychiatric disorders of the 57 interviewees in Adjumani district were compared to their 36-item RISLE scores. Of 50 interviewees with any current psychiatric disorder, the 36-item RISLE positively detected 46 (92.0%) and missed 4 respondents who met diagnostic criteria for any current psychiatric disorder, but mislabeled 7 (12.3%) other respondents out of the 57 interviewees as false positives at a cutoff point of 10. Though numbers were small for purposes of statistical analysis, the individuals who were false positives were more likely to have a positive personal lifetime history of suicide ideation defined as lifetime suicide wish and or lifetime death wish, and positive personal history of suicide attempt. In addition, the individuals concerned were more likely to report a positive family history of suicide behavior defined as family history of suicide and or suicide attempt.
A similar exercise conducted among the students showed that the 36-item RISLE did not do as well as among the general population. At a cut point of 10 the RISLE correctly detected 5 of 19 respondents (26.3%) who met diagnostic criteria for any current psychiatric disorder. Lowering the cut point to 6 for the student population improved the detection ability of the instrument from 5 to 14 out of 19 respondents (73.7%) with any current psychiatric disorder. The false negatives among students at a cut point of 6 were less likely to report a personal history of suicide ideation than students with true positives.
Discussion
This study has taken the 100-item RISLE and attempted to refine and validate the instrument using general population and student samples. The accompanying paper reduced the length of the RISLE to 36 items and found moderate correlations between the 36-item RISLE and two well known questionnaires, the BDI 20–22 and BSS23. Since the instrument has to be clinically utilized it was essential to validate the refined 36-item RISLE as a screening tool for use in the Ugandan general population. This paper examined the clinical validity of the 36-item RISLE by comparing it to standards obtained through a clinical diagnostic research interview.
Performance of the 36-item RISLE
The results from the ROC analysis suggests that overall the 36-item RISLE is better at detecting people with any current psychiatric disorders and people who had experienced recent suicidal thoughts than those with depressive disorders. This suggests that the RISLE may not be a specific measure of depression, possibly because of its composite nature, and may better reflect general psychological distress which correlates better with suicidal thoughts and acts and overall psychological morbidity. This is common to other questionnaires in this field such as the Beck Depression Inventory22 and General Health Questionnaire24.
The cut-off point for optimal detection for the entire sample appeared to be optimal at 10, giving a sensitivity of 74.6% and specificity of 77.1%. At this cutoff point the 36-item RISLE correctly detected 46 of 50 respondents (92.0%) from the general population with any form of current psychiatric illness and was associated with individual and family experiences of suicidal acts or thoughts. However it did less well at this cut-off point in the student population detecting only 5 of 19 students who met criteria for any current psychiatric disorder. The performance of the 36-item RISLE improved when the cut point for students was lowered to 6 at which the kappa value was 0.501, and the instrument correctly detected 14 out of 19 (73.7%) with any current psychiatric disorder.
This difference between RISLE performance for the general and student populations may reflect the differences in prevalence of disorder in the two populations, a parameter that determines the cut-off point for screening instruments. For example the GHQ optimal cut-off score is sensitive to the prevalence of psychiatric disorder and it has been suggested that the median of the GHQ score gives a reliable estimate of the cut-off score25. This may be the case for the RISLE.
Comparison with other studies
In a review of studies involving 18 case-finding instruments, Mulrow and colleagues26 reported that sensitivities and specificities for detecting major depression ranged from 67% to 99% and 40% to 95% respectively; overall sensitivity was 84% and specificity, 72%. In another review of the accuracy and precision of depression questionnaires and clinical examination, Williams and colleagues reported that the median positive likelihood ratio for major depression was 3.3 with a range of 2.3 to 12.2 27. These results are in overall agreement with the RISLE sensitivity, specificity and positive likelihood ratio for any current psychiatric disorder of 74.6%, 77.1% and 3.6 respectively at cut point of 10.
Eaton and colleagues28 have suggested that agreement between questionnaire surveys and clinical interview results was poor with agreement between the two methods being fair at a kappa value of 0.20. Similarly Regier and colleagues have reported that clinical interviews produced consistently higher prevalence rates for major depression than population-based surveys involving the use of questionnaires29. These findings have not been replicated in this study, which has produced a kappa value of 0.508 for any current psychiatric disorder and overall prevalence rates being higher on the RISLE than for clinical interview method.
Methodological issues
There were two main methodological drawbacks to the study. First the low numbers of individuals interviewed to provide the gold standard. This was the case for both the general population and student samples and has resulted in the need to combine samples for parts of the analysis. Further work on larger samples in prospective follow-up studies is required. The sample size however did not affect the first part of the study; the refinement of the 100-item version and the comparison to the BDI and BSS which, particularly for the general population sample, used sufficient numbers. A second problem was the time lapse between the administration of questionnaires and the conducting of the interviews during which time the clinical state of the subjects may have changed. However, some measures such as lifetime experience of suicidal thoughts which were unlikely to have changed did correlate with the RISLE. These limitations reinforce the preliminary nature of this validation exercise.
Implications
Reducing the number of items making it more adaptable to general population research has refined the RISLE. The resulting 36-item RISLE gives scores that are highly correlated with the 100-item RISLE and also with previously known and accepted questionnaires measuring depressive symptoms and suicidal thoughts. The validation of the 36-item RISLE suggests that, in common with other clinical questionnaires measuring psychological symptoms, it is a better measure of overall psychological distress than specific to depressive symptomatology. Its value as a screening instrument is perhaps less well established, but nonetheless the current findings suggest it is an adequate screening instrument in the general population at a cut-off score of 10. The results suggest that the RISLE is able to screen for both depressed mood and high-risk suicide behavior at recommended cut-off points. Further work is however required to establish its worth as a screening device and its performance in different populations. The present study suggests that it can be used in African populations and may be of value in establishing estimated levels of prevalence of psychological symptoms in such populations. We suggest, however, that the RISLE is a dimensional scale and should not be used as a categorical diagnostic instrument. As is the usual practice anyone who screens positive on the RISLE at the recommended cut-off points should undergo clinical diagnostic interview to ascertain the presence and nature of psychiatric disorder.
Figure 2. ROC for any current depressive episode among 115 study participants.
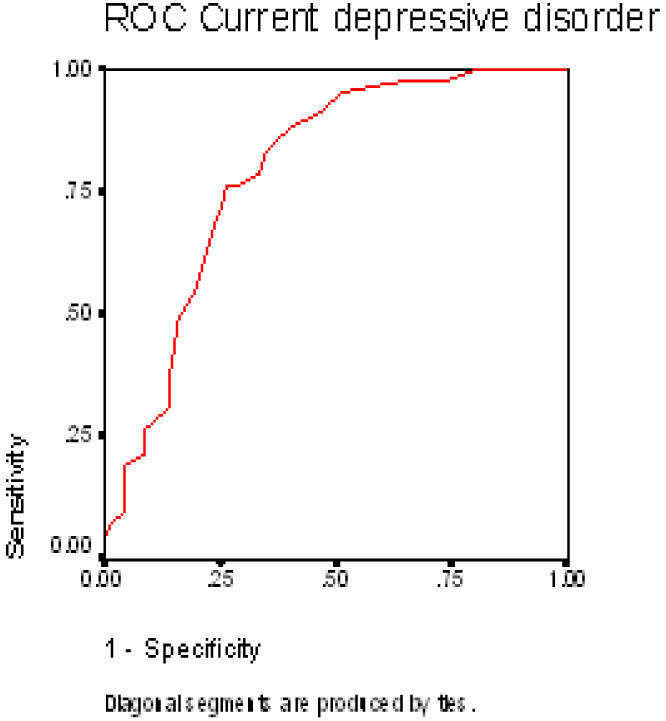
† Area under curve = 0.792 (95% CI 0.710–0.874)
Acknowledgments
Thanks to The Swedish National Center for Suicide Research and Prevention of Mental Ill-Health (NASP) and the Department of Public Health Sciences at the Karolinska Institute, Stockholm, Sweden for developing in collaboration with the Makerere University, Kampala, Uganda of a Ugandan National Plan for Prevention of Mental Ill-Health and Suicide. We are grateful to Dr Seggane Musisi for valuable comments and guidance.
DECLARATION OF INTEREST
This study was supported by SIDA/SAREC funds to build research capacity at Makerere University.
References
- 1.Vorcaro C, Costa MLe, Barreto S, Uchoa E. Unexpected high prevalence of 1-month depression in a small Brazilian community: the Bambui study. Acta Psychiatrica Scandinavica. 2001;104(4):257. doi: 10.1034/j.1600-0447.2001.00440.x. [DOI] [PubMed] [Google Scholar]
- 2.Weissman M, Bland R, Canino G, Faravelli C, Greenwald S, Joyce PH, Karam E, Lee C, Lellouch J, Lepine J, Newman S, Stipec MR, Wells J, Wickramaratne P, Yeh E. Cross-national epidemiology of major depression and bipolar disorder. JAMA. 1996;276(4):293–299. [PubMed] [Google Scholar]
- 3.Narrow W, Rae D, Robins L, Regier D. Revised prevalence estimates of mental disorders in the United States. Arch Gen Psychiatry. 2002;59(2):115–123. doi: 10.1001/archpsyc.59.2.115. [DOI] [PubMed] [Google Scholar]
- 4.Bolton P, Neugebauer R, Ndogoni L. Prevalence of depression in rural Rwanda based on symptom and functional criteria. J Nerv Ment Dis. 2002;190:631–637. doi: 10.1097/00005053-200209000-00009. [DOI] [PubMed] [Google Scholar]
- 5.Goldney R, Harris L, Badri A, Michael S, Fisher L. Suicidal ideation in Sudanese women. Crisis. 1998;19(4):14–18. doi: 10.1027/0227-5910.19.4.154. [DOI] [PubMed] [Google Scholar]
- 6.Pirkis J, Burgess P, Dunt D. Suicidal ideation and suicide attempts among Australian Adults. Crisis. 2000;21(1):16–25. doi: 10.1027//0227-5910.21.1.16. [DOI] [PubMed] [Google Scholar]
- 7.Ramberg I-L, Wasserman D. Prevalence of reported suicidal behavior in the general population and mental health care staff. Psychological Medicine. 2000;30:1189–1196. doi: 10.1017/s003329179900238x. [DOI] [PubMed] [Google Scholar]
- 8.Renberg E. Self-reported life-weariness, death wishes, suicidal ideation, suicidal plans and suicide attempts in general population surveys in the north of Sweden, 1986 and 1996. Umea, Umea: University of Umea; 2000. pp. 1–23. [DOI] [PubMed] [Google Scholar]
- 9.Thomas H, Crawford M, Meltzer H, Lewis G. Thinking life is not worth living. A population survey of Great Britain. Soc Psychiatry Psychiatr Epidemiol. 2002;37:351–356. doi: 10.1007/s00127-002-0556-5. [DOI] [PubMed] [Google Scholar]
- 10.Weissman M, Bland R, Canino G, Greenwald S, Hwu H, Joyce P, Karam E, Lee C, Lelluouch J, Lepine J, Newman S, Rubio-Stipec M, Wells J, Wickramaratne P, Wittchen H, Yeh E. Prevalence of suicide ideation and suicide attempts in nine countries. Psycological Medicine. 1999;29:9–17. doi: 10.1017/s0033291798007867. [DOI] [PubMed] [Google Scholar]
- 11.Ovuga E, Boardman J, Wasserman D. The Response Inventory for Stressful Life Events I: Refinement of the 100-item instrument. 2004. In Press. [PMC free article] [PubMed] [Google Scholar]
- 12.Ovuga E, Boardman J, Wasserman D. The prevalence of depression in two districts of Uganda. British Journal of Psychiatry. 2004 doi: 10.1007/s00127-005-0915-0. In press. [DOI] [PubMed] [Google Scholar]
- 13.Ovuga E, Boardman J, Wasserman D. The prevalence of suicide ideation in two districts of Uganda. Archives of Suicide Resarch. 2004 doi: 10.1080/13811110500182018. In press. [DOI] [PubMed] [Google Scholar]
- 14.Ovuga E, Boardman J, Wasserman D. The mental health of two student populations at Makerere University. 2004. In Press. [PMC free article] [PubMed] [Google Scholar]
- 15.Sheehan DV, Lecrubier Y, Harnett-Sheehan K, Amorim P, Janavs J, Weiller E, Hergueta T, Baker R, Dunbar G. The Mini International Neuropsychiatric Interview (M.I.N.I): The Development and Validation of a Structured Diagnostic Psychiatric Interview. Journal of Clinical Psychiatry. 1998;59(Suppl 20):22–33. [PubMed] [Google Scholar]
- 16.WHO, author. International Classification of Diseases. Geneva: World Health Organization; 1992. [Google Scholar]
- 17.APA, author. Diagnostic and Statistical Manual of Mental Disorders. Washington DC: American Psychiatric Association; 1992. [Google Scholar]
- 18.Fletcher R, Fletcher S, Wagner E. The Essentials. Baltimore: Williams & Wilkins; 1988. Clinical Epidemiology. [Google Scholar]
- 19.Sackett D, Haynes R, Guyatt G, Tugwell P. A Basic Science for Clinical Medicine. London: Little, Brown & Company; 1991. Clinical Epidemiology. [Google Scholar]
- 20.Beck A, Steer R. Manual. Harcourt Brace Jovanovich, Inc.; 1987. Beck Depression Inventory. [Google Scholar]
- 21.Beck A, Steer R, Brown G. BDI-II Manual. San Antonio: The Psychological Corporation; 1996. [Google Scholar]
- 22.Beck A, Ward C, Mendelson M, Mock J, Erbaugh J. An Inventory for Measuring Depression. Arch Gen Psychiatry. 1961;4(6):53–63. doi: 10.1001/archpsyc.1961.01710120031004. [DOI] [PubMed] [Google Scholar]
- 23.Beck A, Kovacs M, Weissman A. Assessment of suicidal intention: The Scale for Suicide Ideation. Journal of Consulting and Clinical Psychology. 1979;47(2):343–352. doi: 10.1037//0022-006x.47.2.343. [DOI] [PubMed] [Google Scholar]
- 24.Goldberg D. A technique for the identification and assessment of non-psychotic psychiatric illness. London: Oxford University Press; 1972. The Detection of Psychiatric Illness By Questionnaire. [Google Scholar]
- 25.Willmott S, Boardman J, Henshaw C, Jones P. Understanding the General Health Questionnaire (GHQ-28) score and its threshold. Soc Psychiatry Psychiatr Epidemiol. 2004;8:613–617. doi: 10.1007/s00127-004-0801-1. [DOI] [PubMed] [Google Scholar]
- 26.Mulrow C, Williams J, Gerety M, Ramirez G, Montiel O, Kerber C. Case-finding instruments for depression in primary care settings. Annals of Internal Medicine. 1995;123:913–921. doi: 10.7326/0003-4819-122-12-199506150-00004. [DOI] [PubMed] [Google Scholar]
- 27.Williams J, Noel P, Cordes J, Ramirez G, Pignone M. Is this patient clinically depressed? JAMA. 2002;287(9):1160–1170. doi: 10.1001/jama.287.9.1160. [DOI] [PubMed] [Google Scholar]
- 28.Eaton W, Neufield K, Chen L-S, Cai G. A comparison of self-report and clinical diagnostic interviews for depression. Diagnostic Interview Schedule and Schedules for Clinical Assessment in Neuropsychiatry in Baltimore Epidemiologic Catchment Area Follow-up. Arch Gen Psychiatry. 2000;57(3):217–222. doi: 10.1001/archpsyc.57.3.217. [DOI] [PubMed] [Google Scholar]
- 29.Regier D. Community diagnosis counts. Arch Gen Psychiatry. 2000;57:223–224. doi: 10.1001/archpsyc.57.3.223. [DOI] [PubMed] [Google Scholar]


