Abstract
Objective
The aim was to report the prevalence of oral diseases/conditions among a Ugandan population.
Methods
Subjects aged 12 (n=696) and 35-44 years (n=396) were chosen from randomly selected urban and peri-urban areas of Arua, Mbale, Kampala and Mbarara districts. They were clinically examined by 4 trained and calibrated dentists for oral diseases/conditions using criteria described by World Health Organisation.
Results
Dental caries (DMFT ≥1) was recorded in 40% and 62.5% of the children and adults, respectively. The overall mean DMFT score was 0.9 for children and 3.4 for adults. Caries was significantly more severe in females as compared to males in children (p<0.05), whereas in adults, there was no significant gender difference. Kampala had a significantly higher mean DMFT score compared to other districts in all age groups (p>0.05). Culculus deposits were generally, more prevalent in adults as compare to children except in Mbarara district. Gum bleeding was also significantly more prevalent among children as compared to adults (p<0.05). Significantly higher prevalence of gum bleeding in both children and adults was recorded in Arua district as compared to other areas (p<0.05). Each of the age groups had a prevalence of malocclusion of 61%. However, the severity of malocclusion varied between age groups and districts. The prevalence of dental fluorosis was 3% and 4% for children and adults, respectively. All subjects in Arua district were fluorosis-free. Tetracycline enamel staining was less than 1% in both age groups. Enamel attrition was more prevalent in adults as compared to children: 19% versus 1%.
Conclusion
The prevalence of oral diseases/conditions was generally low among the study population. Caries experience was significantly higher in the Kampala (urban) district as compared to rural districts in all age groups; the D - component being the major contributor.
Keywords: Prevalence, caries, periodontal disease, malocclusion, calculus, gum bleeding, enamel opacities, Uganda
Introduction
During a pilot survey, the purpose of which was district capacity building of dental personnel in methods of carrying out oral health survey, 1092 persons were clinically examined for oral diseases/conditions in four districts of Uganda. A few previous reports on oral health in Uganda have dealt with dental caries1–7, dental mutilation8, tooth eruption ages9, periodontal condition3,4,10, dental fluorosis6,11–15, enamel opacities and enamel hypoplasia2. Two of these surveys were aimed at national estimates2,4. To our knowledge, no studies on the prevalence of occlusal anomalies, dental attrition and tetracycline enamel stains had hitherto been carried out in Uganda. The aim of the present paper is to report on the prevalence of dental caries, dental fluorosis, periodontal condition, malocclusion, enamel opacities and other enamel disorders among 12-year-old school children and 35–44 year old adults in four districts of Uganda.
Material and Methods
Study areas
This epidemiological survey was conducted in 2002 in 4 districts of Arua, Mbale, Mbarara and Kampala. Schools were used as study areas for the 12 year-olds and Local Council (LC) Is or villages for the 35 – 44 year-olds. A list of primary schools located within 15 km from the district administrative centres was obtained from the respective District Education Officers and 4 schools were randomly selected using numbers in each district. For the 35 – 44 year-olds, a list of all parishes within a radius of 15 km from the district administrative centres was obtained from the district local authorities. Six parishes were randomly selected using numbers. Then, one LC I in each parish was also similarly randomly selected for the study
Selection of subjects
Two of the index age groups: 12 year-olds and 35 – 44 year-olds recommended by World Health Organization (WHO)16 for field surveys were considered in this study.
-
12 year-olds
From each of the school registers, all children whose age fell within a range of 11½ and 12½ years were requested to make two lines according to gender. Using random numbers, a total of 696 children (328 boys and 368 girls) were selected (Table 1). This was slightly in excess of the estimated sample size (n=656). There was no significant difference in the distribution of children according to gender within and between the districts (p>0.05, χ2 test).
-
35 – 44 year-olds
Due to the difficulties in establishing the actual age of the residents and mobilizing them in specific examination centres, the subjects were selected by convenience method. The LC officials were requested to mobilize all adults in their homesteads. Taking the residence of the LC I chairperson of the selected area as the focal point, the examiners moved from household to household examining adults whose age fell within 35 – 44 years, totalling 396 persons (170 males/226 females, Table 1). This was about 17% less the estimated study sample size. Significantly more females were recruited (p<0.05, χ2 test).
Table 1.
Distribution of number of subjects examined, prevalence of calculus deposit, gum bleeding and dental fluorosis in children and adults according to district.
| Variable | Children (12 years) | Adults (35–44 years) |
| Subjects | ||
| Arua | 181 | 106 |
| Kampala | 194 | 62 |
| Mbale | 152 | 109 |
| Mbarara | 169 | 119 |
| Total | 696 | 396 |
| Calculus | ||
| Arua | 96 (52.8) | 70 (66.0) |
| Kampala | 106 (54.5) | 48 (77.0) |
| Mbale | 28 (18.4) | 84 (77.1) |
| Mbarara | 164 (97.0) | 112 (94.1) |
| Total | 394 (56.0) | 314 (79.3) |
| Givgival bleeding | ||
| Arua | 139 (76.7) | 65 61.3) |
| Kampala | 101(52.1) | 22 (36.1) |
| Mbale | 74 (48.8) | 59 (54.1) |
| Mbarara | 61(36.2) | 38 (31.9) |
| Total | 375 (53.9) | 184 (46.5) |
| Dental fluorosis | ||
| Arua | 0 (0.0) | 0 (0.0) |
| Kampala | 1 (0.2) | 1 (0.7) |
| Mbale | 4 (2.5) | 9 (8.0) |
| Mbarara | 1(0.5) | 3 (2.5) |
| Total | 6 (0.8) | 13 (3.4) |
Percentage in parentheses
Informed consent
Permission to carry out the study was sought from and granted by the respective district local administrations. The health and school authorities also allowed the study to be conducted in their areas of jurisdiction. The head teachers (on behalf of children) and adult subjects gave verbal consent. In accordance with Helsinki Declaration17, the nature of the study and the subjects' right to accept or refuse to participate in the study were dully explained to the head teachers and adult subjects.
Calibration of examiners
Prior to the field survey, four trained dentists were calibrated in oral examination among the 12 year-olds (n=20) in St. Martin Primary School, Kampala, in order to minimize inter-examiner variability. The mean inter-examiner consistence in recording caries was found to be 96% (range, 93% – 98%).
Clinical examination
Intra-oral examination of subjects was carried out by four trained dentists, one in each district: LMM in Kampala district, JFT in Mbarara, AK in Arua and EMN in Mbale under field conditions according to criteria described by WHO16.
An assistant recorded the observations. The subjects were examined while lying on a couch in a supine position in a shade. Indirect sunlight was the source of illumination. Mouth mirror, periodontal and dental probes were used in the examination. Cotton wool was used to control bleeding if any after periodontal probing. Instruments were cleaned and sterilized by boiling in water for 1 hr, and kept in 0.2% chlorhexidine solution before use.
Malocclusion
Malocclusion was recorded as present if, one or combination of the following criteria was met:
Had a significant and unacceptable effect on facial appearance.
Caused significant reduction in masticatory function or resulted in significant speech impairment.
Had gross defect such as cleft lip, cleft palate or pathological or surgical injury that unquestionably had a high priority for treatment.
Constituted an occlusion predisposing to tissue destruction in the form of periodontal disease or caries.
All children who had previously undergone orthodontic treatment were to be excluded from this study.
Dental caries
Caries was assessed using Decayed Missing Filled Teeth (DMFT) index18 according to criteria described by WHO16. Caries was recorded as being present when a lesion in a pit/fissure or on a smooth surface had a detectable softened floor, undermined enamel, softened wall or temporary filling. On proximal surfaces, the probe had to enter the lesion with certainty. When in doubt, the carious lesion was not recorded. Stained pits or fissures that caught the probe, but did not have undermined enamel, softened floor or walls were not counted as carious lesions. A tooth was considered filled if it had a permanent restoration and it was considered missing due to caries if there was history of pain and or presence of a cavity prior to extraction.
Dental fluorosis
The vestibular surfaces of all the teeth were assessed for fluorosis using Dean's index19. Each subject was given a score equivalent to that attached to the most severely affected homologous pair of teeth. Questionable fluorosis was recorded as no fluorosis.
Enamel opacities and other disorders
Opacities and other disorders include hypoplasia, tetracycline discoloration, tooth mutilation and attrition. Care was taken to differentiate the enamel opacities from fluorosis. Fluorosis was ruled out if the opacity did not involve a homologous pair of teeth irrespective of the severity. Presence of the condition was given score “1” and score “0” for its absence.
Periodontal status
The mouth was divided into six sextants: anterior (from canine to canine), left and right posterior (from first premolar to second molar) for both the mandible and maxilla. Periodontal conditions were independently assessed: first, calculus deposits and later, gingival bleeding for each of the six arch sextants. The sequence of assessment was right posterior, anterior and left posterior sextants on both lingual and vestibular aspects of the maxilla and mandible. The assessment of a specific periodontal condition (calculus or gingival bleeding) in a particular sextant ceased when it was detected on any aspect of any tooth in that sextant. Any obvious deposit on the exposed tooth crown or root suspected of being calculus, as determined by direct inspection or with the aid of mouth mirror was tested with a periodontal probe to confirm that it was calcified. Absence of the deposit or presence of uncalcified deposit was given a score of “0”. If the deposit was calcified it was given a score of “1”. Gingival bleeding was assessed by inserting a periodontal probe not more than 2 mm into the gingival sulcus and moved around the circumference of each tooth. Score “1” was recorded if bleeding was elicited and “0” if there was no bleeding.
Reliability test
Separate duplicate examination for dental caries in about 10% of the children in each of the 4 districts a few days after the main examination for reproducibility test gave a substantial agreement. Cohen's kappa values ranged from 0.80 to 0.84 and no evidence of systematic error was found in both examiners (p>0.05, Wilcoxon test).
Statistical analyses
Data were analysed using the Statistical Package for Social Sciences Inc. Wilcoxon signed-ranks test for paired observations was used to check for significant intra-examiner differences in recording caries. Student's t test for independent samples was used to assess any significant differences between means of quantitative variables. Chisquare (χ2) statistics were used to compare frequency distributions of subjects on the basis of prevalence of oral conditions, gender, age, area of residence and other variables. The level of significance was set at 5%.
Results
Generally, there were no significant differences in oral diseases and conditions according to gender within districts.
Dental caries
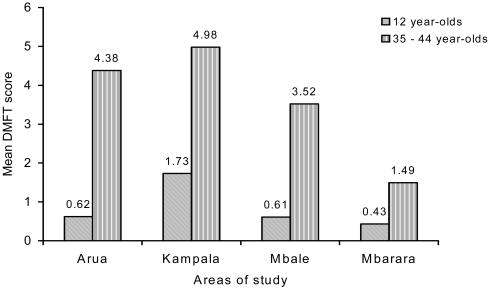
Dental caries (DMFT ≥1) was recorded in 40% of the children. The D- and M-components contributed 88% and 11% of the DMFT scores, respectively. The F-component had a negligible contribution. The overall mean DMFT score was 0.9, with a significantly lower value for males as compared to females: 0.7 versus 1.0 (p<0.05, t test). Based on the districts, children in Kampala had a significantly higher mean DMFT score compared to other districts (p<0.05, t test; Fig. 1).
Figure 1.
Caries experiences among children (n=696) and adults (n=396) according to district
Among the adults, there was no significant difference in caries between males and females (p>0.05, t test). About 65.2% of the adults had DMFT≥1 with about 81% of the DMFT scores being due to the D-component (Table 2). According to districts, the adults in Kampala had a higher caries experience as compared to other districts. The caries experience was significantly higher in adults as compared to children (p<0.05, t test; Fig 1).
Table 2.
Percentage distribution of individual diagnoses within the total numbers of decayed (D) missing (M) and filled (F) teeth in children and adults.
| Diagnosis | Children | Adults |
| D | 87.8 | 80.7 |
| M | 11.3 | 17.5 |
| F | 0.9 | 1.8 |
Periodontal status
Generally, calculus deposits were more prevalent in adults as compare to children except in Mbarara district (Table 1). Gum bleeding was also significantly more prevalent among children as compared to adults (p<0.05, χ2 test; Table 1). Arua district had a significantly higher disease condition in both children and adults as compared to other areas (p<0.05, χ2 test).
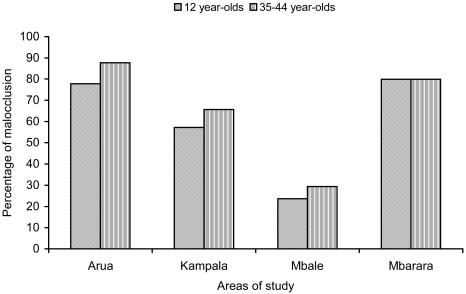
Malocclusion
Overall, the prevalence of malocclusion both in children and adults were of the same magnitude: 61% (Fig. 2). However, based on the districts, the prevalence of moderate to severe malocclusion varied between 6% and 14% in children and between 3% and 51 in adults.
Fig. 2.
Prevalence of malocclusion in children (n=696) and adults (n=396) according study areas
Dental fluorosis
The prevalence of dental fluorosis was low, being recorded in 3% and 4% of the children and adults, respectively. No subject exhibited severe form of fluorosis. All the subjects in Arua were fluorosis-free (Table.1).
Opacities and other enamel disorders
Among the enamel opacities, tetracycline enamel staining was less than 1% in both age groups. However, enamel attrition was found to be more prevalent in adults as compared to children: 19% versus 1% (Table 3).
Table 3.
Prevalence of enamel opacities, hypoplasia, tetracycline discoloration, tooth mutilation and attrition in children (n=696) and adults (n=396)
| Age group | Opacities | Hypoplasia | Tetracycline | Mutilation | Attrition |
| Children | 6.8 | 6.2 | 0.4 | 2.0 | 0.7 |
| Adults | 3.3 | 1.5 | 0.8 | 1.8 | 18.7 |
Discussion
Methodology
This epidemiological survey was conducted in the 4 different regions of Uganda in order to draw subjects from as closely similar areas as those in previous national surveys2,4 for comparison purposes. Inter-examiner variations in oral examination may give different results20. Although, in this study, different examiners were employed, it may not have influenced the findings since a high inter-examiner consistence was recorded during calibration and their reliability test gave a substantial agreement. Two index age groups of 12 and 35 – 44 years recommended by WHO16 for field surveys were considered in this study. The 12 year-olds were included in this study as they were assumed to have most of the permanent teeth erupted and have had a relatively sufficient time of exposure to the oral environment. The adult age group (35 – 44 years) was considered to be when oral diseases, especially those affecting the dentition, if any, to have been established.
A different sampling technique was employed for each age group. The 12 year-olds were adequately mobilised through schools, however, due to the difficult of mobilising the adults to a particular examination centre, a sample of convenience was obtained by visiting the subjects from their homesteads, which probably may not be a true representative of the adult population.
The areas of study were 15 km from the district administrative centres indicating that the subjects examined were both urban and semi-urban residents. Although these groups of subjects could have been living under slightly different conditions, assessment of factors that may have influenced the trend of oral diseases in these groups was beyond the scope of this study. Standardised criteria as described by WHO16 have been used in assessment of some of the oral conditions in this study. These methods are recommended for field surveys for global comparisons.
Findings
Similar to the findings in the previous studies in Uganda2,3, the prevalence of dental caries in this study was significantly higher in the more urban Kampala as compared to other districts and higher in females than males. Caries increase with age corroborates other previous studies at least in Uganda2,3,5,7. Although caries experience (mean DMFT score) was generally low both in children and adults: 0.9 versus 3.4, the respective contribution of the D-component by 88% and 81% (Table 2) indicate how much of the caries goes untreated. It was also evident that among the 35–44 year-old subjects only 35% were caries-free implying that even if the severity of the disease was low, it is wide spread and may be a cause for concern. Using similar diagnostic criteria, the previous study11 has reported the prevalence and severity of dental fluorosis in Uganda to vary from district to district. Although the specific areas previously studied were not precisely indicated, the prevalence and severity of dental fluorosis were substantially higher than in the present study.
Periodontal condition (gum bleeding) in both children and adults was generally moderate according to WHO21 criteria except in Arua district where it was more severe (Table 1). Despite the fact that calculus (causative agent for periodontal disease) was more prevalent among the adults except in Mbarara, gum bleeding was more common among the children as compared to the adults. This calls for more analytical studies to elucidate this observation. For the first time this is the study that has assessed malocclusion in Uganda and as such there is lack of previous data for comparison in this population. The diagnostic criteria used in this study were rather crude and subjective which could have either over- or under-estimated the prevalence compared to the more objective one22. Furthermore, due to the lack of categorising specific occlusal traits investigated makes the findings inconclusive. However, based on the large number of subjects examined, the effect of under- or over-estimation is likely to have been slight and the data is therefore valuable.
Opacities and other enamel disorders were found to be very rare in communities examined and details based on the district were considered meaningless and hence age groups. The findings from enamel opacities, enamel hypoplasia and mutilation favourably compared with findings from previous studies2,8.
Cultures like dental mutilations involving chipping off the mesial incisal angles of maxillary central incisors and extractions of anterior mandibular teeth8 in anticipation for easy management of lockjaw are no long practiced for over 30 years now. Of particular importance was attrition among adults, which was recorded in 19% of the subjects. Like malocclusion, the prevalence of dental attrition and tetracycline stains was for the first time assessed among Ugandans in this study and lacks previous data for comparison.
Conclusions
The prevalence of oral diseases/conditions was generally low among the study population. Caries experience was significantly higher in the Kampala (urban) district as compared to rural districts in both children and adults. The D component was the major contributor indicating that most of the caries goes untreated.
Acknowledgments
The authors are grateful to the subjects, school authorities and the district local leaders for their cooperation during the study. The Rockfeller Foundation through I@Mak financially supported the study.
References
- 1.Welbourn HF. The teeth of children attending Kampala child welfare clinics and schools. East African Medical Journal. 1956;33:181–187. [PubMed] [Google Scholar]
- 2.Møller IJ, Pindborg JJ, Roed-Petersen B. The prevalence of dental caries, enamel opacities and enamel hypoplasia in Ugandans. Archives of Oral Biology. 1972;17:9–22. doi: 10.1016/0003-9969(72)90129-x. [DOI] [PubMed] [Google Scholar]
- 3.Jensen K, Kizito EK, Langbæk J, Nyika TA. Dental caries, gingivitis and oral hygiene among schoolchildren in Kampala, Uganda. Community Dentistry and Oral Epidemiology. 1973;1:74–83. doi: 10.1111/j.1600-0528.1973.tb01863.x. [DOI] [PubMed] [Google Scholar]
- 4.Tirwomwe F, Ekoku Y, Bælum V, Fejerskov O. Oral health in Uganda: Results of a national survey 1987. Nairobi: Ministry of health, Uganda/Kenya Medical Research Institute; 1988. [Google Scholar]
- 5.Rwenyonyi CM, Birkeland JM, Haugejorden O, Bjorvatn K. Dental caries among 10- to 14-year-old children in Ugandan rural areas with 0.5 and 2.5 mg fluoride per liter in drinking water. Clinical Oral Investigations. 2001;5:45–50. doi: 10.1007/pl00010681. [DOI] [PubMed] [Google Scholar]
- 6.Wandera M, Twa-Twa J. Baseline survey of oral health of primary and secondary school pupils in Uganda. African Health Sciences. 2003;3:19–22. [PMC free article] [PubMed] [Google Scholar]
- 7.Okullo I, Astrom AN, Haugejorden O, Rwenyonyi CM. Variations in caries experience and sugar intake among secondary school students in urban and rural Uganda. Acta Odontologica Scandinavica. 2003;61:197–202. doi: 10.1080/00016350310003882. [DOI] [PubMed] [Google Scholar]
- 8.Pindborg JJ. Dental mutilation and associated abnormalities in Uganda. American Journal Physiology and Anthropology. 1969;31:383–390. doi: 10.1002/ajpa.1330310313. [DOI] [PubMed] [Google Scholar]
- 9.Krumholt L, Roed-Petersen B, Pindborg JJ. Eruption times of permanent teeth in 622 Uganda children. Archives of Oral Biology. 1971;16:1281–1288. doi: 10.1016/0003-9969(71)90031-8. [DOI] [PubMed] [Google Scholar]
- 10.Skougaard MR, Pindborg JJ, Roed-Petersen B. Periodontal conditions in 1394 Ugandans. Archives of Oral Biology. 1969;14:707–719. doi: 10.1016/0003-9969(69)90192-7. [DOI] [PubMed] [Google Scholar]
- 11.Møller IJ, Pindborg JJ, Gedalia I, Roed-Petersen B. The prevalence of dental fluorosis in the people of Uganda. Archives of Oral Biology. 1970;15:213–225. doi: 10.1016/0003-9969(70)90080-4. [DOI] [PubMed] [Google Scholar]
- 12.Rwenyonyi CM, Bjorvatn K, Birkeland JM, Haugejorden O. Altitude as a risk indicator of dental fluorosis in children residing in areas with 0.5 and 2.5 mg fluoride per litre in drinking water. Caries Research. 1999;33:267–274. doi: 10.1159/000016528. [DOI] [PubMed] [Google Scholar]
- 13.Rwenyonyi CM, Birkeland JM, Bjorvatn K, Haugejorden O. Age as a determinant of severity of dental fluorosis in children residing in areas with 0.5 and 2.5 mg fluoride per liter in drinking water. Clinical Oral Investigations. 2000;4:157–161. doi: 10.1007/pl00010677. [DOI] [PubMed] [Google Scholar]
- 14.Rwenyonyi CM, Birkeland JM, Haugejorden O. Assessment of the validity and consequences of different methods of expressing the severity of dental fluorosis in a subject. Acta Odontologica Scandinavica. 2000;58:148–154. doi: 10.1080/000163500429136. [DOI] [PubMed] [Google Scholar]
- 15.Rwenyonyi CM, Birkeland JM, Haugejorden O, Bjorvatn K. Dental variables associated with differences in severity of fluorosis within the permanent dentition. Clinical Oral Investigations. 2000;4:57–63. doi: 10.1007/s007840050114. [DOI] [PubMed] [Google Scholar]
- 16.World Health Organization, author. Basic methods. 3rd ed. Geneva: 1987. Oral health surveys. [Google Scholar]
- 17.World Medical Association, author. Declaration of Helsinki. Norske Medicin. 1992;107:25. [Google Scholar]
- 18.Klein H, Palmer CE, Knutson FW. Studies on dental caries. I. Dental status and dental needs of elementary school children. Public Health Report. 1938;53:751–765. [Google Scholar]
- 19.Dean HT. Classification of mottled enamel diagnosis. Journal of American Dental Association. 1934;21:1421–1426. [Google Scholar]
- 20.Manji F, Fejerskov O. Dental caries in developing countries in relation to the appropriate use of fluoride. Journal Dental Research. 1990;69:733–741. doi: 10.1177/00220345900690S143. [DOI] [PubMed] [Google Scholar]
- 21.World Health Organization, author. Preventive Methods and Programs for Oral Disease. 1984 Report of WHO Expert Committee Technical Support Series 713. Geneva.
- 22.Bjørk A, Krebs AS, Solow B. A method for epidemiologic registration of malocclusion. Acta Odontologica Scandinavica. 1964;22:27–41. doi: 10.3109/00016356408993963. [DOI] [PubMed] [Google Scholar]