The patient
A 72 year old multiparous woman presented with intermittent postmenopausal bleeding. The patient's relevant medical history included insulin dependent diabetes, hypertension, and recent breast cancer. She had been treated with tamoxifen for three years. On examination, the patient was obese (body mass index 32) and no cause for the bleeding was found in the introitus, vulva, vagina, cervix, uterus, or adnexa. She was referred to the cancer unit for gynaecological assessment in accordance with “improving outcomes in gynaecological cancers” 1999 guidelines.1
Learning points
Risk factors for endometrial cancer are prolonged (more than five years) use of unopposed oestrogen hormone replacement therapy, tamoxifen use, hereditary non-polyposis colorectal carcinoma, obesity combined with diabetes, hypertension, and endogenous or exogenous increase in oestrogens
Transvaginal ultrasound should be the primary imaging investigation for assessing the endometrium in postmenopausal women with vaginal bleeding
Endometrial thickness of 5 mm or more requires endometrial biopsy; thickness less than 5 mm has a negative predictive value for endometrial cancer of 98%
Magnetic resonance imaging is reserved for staging endometrial cancer before surgery
What imaging tests do I request?
The patient has several risk factors for endometrial hyperplasia and endometrial carcinoma including the use of tamoxifen, obesity, diabetes, and hypertension. Although the routine screening of patients is not recommended, postmenopausal bleeding is an indication for detailed evaluation of the endometrium.2
Transabdominal ultrasound of the pelvis
Transabdominal pelvic ultrasound is not appropriate in this patient. Adequate evaluation of the uterus—particularly the endometrium—cannot be performed transabdominally.
Transvaginal ultrasound of the pelvis
Transvaginal ultrasound of the pelvis is a highly reliable method for detecting endometrial cancer. In patients with postmenopausal bleeding, if the thickness of the endometrium is uniformly 5 mm or less, the probability of endometrial cancer is less than 1%.2 Sampling of the endometrium must be performed if there is diffuse thickening of the whole endometrium or focal thickening of part of the endometrium measuring 5 mm or more.1 The combination of abnormal vaginal bleeding and an endometrial thickness 5 mm or greater is 92% sensitive and 57% specific for endometrial cancer.3
Transvaginal ultrasound may indicate the type of abnormality seen within the endometrium—for example, endometrial hyperplasia, polyps, or carcinoma. Classically, endometrial hyperplasia affects the entire endometrium and results in widening of the endometrium. The endometrial hyperplasia has a cystic lace-like appearance on ultrasound. Endometrial polyps manifest as focal areas of endometrial thickening, and the stalk of the polyp may be seen if sufficient fluid is present in the endometrial cavity. Endometrial carcinoma may occur in the form of a polyp, within endometrial hyperplasia, or as a heterogeneous endometrial mass with a widened irregular cavity. Pathological confirmation of the histology is needed in all cases, as the ultrasound appearances overlap considerably. Endometrial biopsy is performed if the endometrial cavity is irregular, the endometrium has diffuse or focal widening greater than 5 mm, or if the whole endometrium has not been adequately assessed.4 5
Transvaginal ultrasound may also identify ovarian pathology, including polycystic ovaries in younger women and ovarian tumours secreting oestrogens, causing abnormal vaginal bleeding. The ovaries are atrophic in most postmenopausal women and cannot be identified on ultrasound in up to 20% of women.
Pelvic magnetic resonance imaging
The appearances of endometrial cancer, hyperplasia, and benign polyps also overlap on magnetic resonance imaging and its role is in the staging of biopsy confirmed endometrial cancer. Magnetic resonance imaging is more sensitive than transvaginal ultrasound or computed tomography in the detection of deep myometrial invasion and tumour spread beyond the uterus. The natural contrast between the endometrial tumour and surrounding myometrium is poor on transvaginal ultrasound. Consequently, magnetic resonance imaging is more sensitive than ultrasound (84-87% (specificity 91-94%) v 77%).5 6 7 Endometrial cancer is staged surgicopathologically according to FIGO (International Federation of Gynecology and Obstetrics) criteria. Preoperative magnetic resonance imaging is performed to identify patients with deep myometrial invasion, enlarged pelvic nodes, and extrauterine extension of disease, which alter the extent of surgery.
Outcome
Transvaginal ultrasound showed a normal sized uterus. The endometrium was 12 mm thick with a lace-like pattern; this was compatible with endometrial hyperplasia, probably secondary to treatment with tamoxifen. Because neither ovary was identified, they were assumed to be atrophic as a result of age. No other adnexal masses or ascites were identified.
After the ultrasound, the patient had a hysteroscopy and a pipelle biopsy of the endometrium. The pathological specimen confirmed a background of complex endometrial hyperplasia, but two small foci of grade 2 endometrial carcinoma were found within the endometrium.
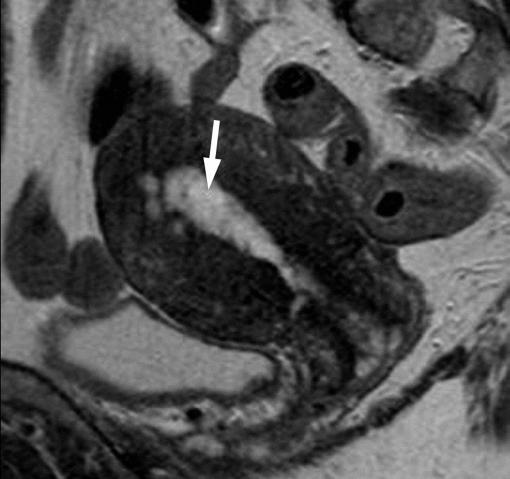
Magnetic resonance imaging of the pelvis demonstrated a FIGO stage 1a carcinoma (figure), and the patient had a total abdominal hysterectomy, bilateral salpingo-oophorectomy, and pelvic lymphadenectomy.
Sagittal T2 weighted image showing the mass within the endometrial cavity (arrow). No underlying myometrial invasion is present, indicating a stage 1a carcinoma of the endometrium with a background of endometrial hyperplasia
Competing interests: None declared.
This series provides an update on the best use of different imaging methods for common or important clinical presentations. The series editors are Fergus Gleeson, consultant radiologist, Churchill Hospital, Oxford, and Kamini Patel, consultant radiologist, Homerton University Hospital, London
References
- 1.NHS Executive. Guidance on commissioning cancer services. Improving outcomes in gynaecological cancers. London: Department of Health, 1999. Available from www.dh.gov.uk/PublicationsAndStatistics/Publications/
- 2.Gerber B, Krause A, Muller H, Reimer T, Kulz T, Makovitzky J, et al. Effects of adjuvant tamoxifen on the endometrium in postmenopausal women with breast cancer: a prospective long-term study using transvaginal ultrasound. J Clin Oncol 2000;18:3464-70. [DOI] [PubMed] [Google Scholar]
- 3.Ciatto S, Cecchini S, Gervasi G, Landini A, Zappa M, Crocetti E. Surveillance for endometrial cancer with transvaginal ultrasonography of breast cancer patients under tamoxifen treatment. Br J Cancer 2003;88:1175-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Scottish Intercollegiate Guidelines Network (SIGN). Investigation of post-menopausal bleeding. 2002. www.sign.ac.uk/guidelines/fulltext/61/index.html
- 5.Hulka CA, Hall DA, McCarthy K, Simeone JF. Endometrial polyps, hyperplasia and carcinoma in post-menopausal women: differentiation with endovaginal sonography. Radiology 1994;191:755-8. [DOI] [PubMed] [Google Scholar]
- 6.Fishman A, Altaras M, Bernheim J, Cohen I, Beyth Y, Tepper R. The value of transvaginal sonography in the preoperative assessment of myometrial invasion in high and low grade endometrial cancer and in comparison to frozen section in grade 1 disease. Eur J Gynaecol Oncol 2000;21:128-30. [PubMed] [Google Scholar]
- 7.Manfredi R, Mirk P, Maresca G, Marganti PA, Testa A, Zannoni G, et al. Local-regional staging of endometrial carcinoma: role of MR imaging in surgical planning. Radiology 2004;231:372-8. [DOI] [PubMed] [Google Scholar]