Abstract
Overactive bladder (OAB) and interstitial cystitis (IC) have similar symptoms, including urinary urgency/frequency and nocturia, making them difficult to differentiate on the basis of clinical presentation alone. Both conditions may represent a clinical manifestation of a hypersensitive bladder and should be included in the differential diagnosis for patients who present with urgency/ frequency. It is especially important that IC be considered in patients with OAB that is refractory to treatment. The proposed diagnostic framework may be useful for differentiating IC from OAB and for facilitating appropriate treatment.
Key words: Overactive bladder, Interstitial cystitis, Painful bladder syndrome, Detrusor overactivity
Interstitial cystitis (IC) is a syndrome characterized by urinary urgency and frequency, usually with pelvic pain and nocturia, in the absence of bacterial infection or any other identifiable pathology.1,2 The condition can be severely debilitating, interfering with employment, social relationships, and sexual activity. Over the past few years, the nomenclature has evolved to include painful bladder syndrome (PBS) along with IC (IC/PBS) to describe the symptom complex. This expanded term may be considered to be more inclusive of patients with this symptom complex.1,3
Interstitial cystitis may go undiagnosed for years, particularly in cases of mild or moderate disease.2,4 The symptoms typically associated with IC often overlap with other gynecologic and urologic conditions, including overactive bladder (OAB), which is characterized by urinary urgency, with or without urge urinary incontinence, usually with frequency and nocturia and the absence of obvious pathology to account for these symptoms.1
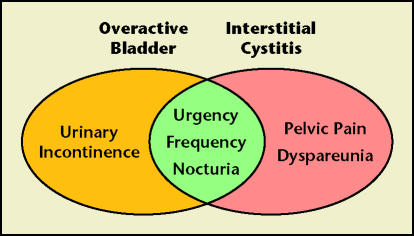
Although patients who present with urgency, frequency, and nocturia could potentially be diagnosed with either OAB or IC, there are certain symptoms that tend to differentiate the 2 conditions (Figure 1). Pelvic pain is a common symptom of IC, although one clinician reported that approximately 30% of patients with IC do not present initially with pain, but develop it only as the condition progresses.5 Pelvic pain is generally not present in patients with OAB.1,2 Urinary incontinence is not a typical feature of IC,6 whereas urge urinary incontinence is common in patients with OAB.7
Figure 1.
Some symptoms of overactive bladder and interstitial cystitis overlap, but other symptoms may differentiate the 2 conditions in some patients.
Both IC and OAB should be considered in the differential diagnosis of patients with symptoms of urgency and/or frequency. This review will discuss similarities and differences in the presentation of IC and OAB, and will address the possibility that the 2 conditions may occur concurrently or that some patients with refractory OAB may actually have IC. A diagnostic framework for differentiating IC from OAB will also be presented.
Overview of Interstitial Cystitis
Etiology
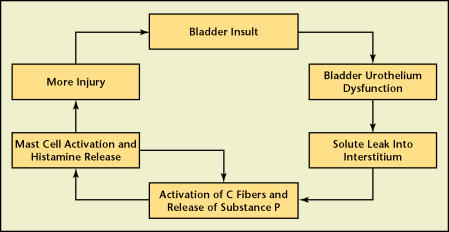
The pathogenesis of IC is still not completely understood, but it is likely multifactorial.5 One popular theory implicates a dysfunction of the normally impermeable bladder urothelial lining (Figure 2).8 Abnormalities in the lining increase its permeability, allowing passage through the bladder urothelium of urinary solutes such as potassium.5 Chronic diffusion of these irritants across the bladder urothelium may induce an inflammatory reaction marked by the proliferation and activation of mast cells.8
Figure 2.
Proposed model for the pathogenesis of interstitial cystitis. Adapted with permission from Evans RJ.8
Mast cell activation and neurogenic inflammation seem to play important roles in the pathogenesis of IC.5 Increased numbers of mast cells are detected in the bladder urothelium and detrusor muscle of patients with IC.9 Mast cell degranulation may activate capsaicin-sensitive nerve fibers, which, in turn, release substance P and other neuropeptides that cause cell damage. Prolonged activation of mast cells and capsaicinsensitive nerve fibers can lead to further injury to the bladder muscle, the development of fibrotic changes within the bladder, and neurogenic up-regulation. Sensory nerve activation in the bladder and development of neural changes within the spinal cord (up-regulation with spinal windup) are thought to be responsible for the chronic symptoms of urgency, frequency, and pelvic pain that characterize IC.8
Similarly, the pathophysiology of OAB has not been clearly established. An increasing body of knowledge supports the important role of increased sensory nerve activation and up-regulation in the pathogenesis of OAB symptoms.10 Afferent nerves innervating the urothelium and suburothelium may be stimulated by a number of pathologic processes, resulting in urinary frequency and urgency. The urothelium, once thought to be a passive barrier, is now believed to be an actively functioning sensory organ and a participant in the pathogenesis of OAB.11 Neurogenic inflammation and C-fiber activation may also play a role.10
Because of the potential for a common pathogenesis for IC and OAB, as well as the overlap in their clinical presentation, it is possible that IC may initially present in some patients with symptoms suggestive of OAB in the absence of pain. What differentiates the presence of storage symptoms associated with pain in these bladder sensory disorders remains to be determined.
Epidemiology
Interstitial cystitis is not a rare condition. Epidemiologic studies suggest that it may be more widespread than previously thought.12–15 However, IC is often not diagnosed during the first several years following the onset of symptoms.2,4
Signs and symptoms of IC early in the course of disease may be intermittent and variable, making IC difficult to recognize, thus delaying the diagnosis.2 At the onset of the disease, only 1 symptom was reported in 70% to 89% of patients with IC.2,4 In a retrospective study, simultaneous presentation of urgency, frequency, pain, and nocturia occurred in only 7% of patients diagnosed with the condition.2 Patients with IC may have symptoms for years and consult with many physicians, including psychiatrists, before the condition is correctly diagnosed.16
In the past, IC may have been underdiagnosed owing to over-adherence to the National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK) criteria for the diease.12,17 Originally designed for research studies, these criteria require the presence of Hunner’s ulcers, or the presence of 2 or more of the following: pain on bladder filling that is relieved by emptying; suprapubic, pelvic, urethral, vaginal, or perineal pain; glomerulations in at least 3 out of 4 quadrants of the bladder on cystoscopy12; and decreased compliance on cystometry (Table 1).17 Additionally, the criteria specify a number of automatic exclusion criteria, including nocturia fewer than 2 times per night, symptom duration of less than 12 months, bladder capacity greater than 400 mL, or involuntary bladder contractions.17 Evidence suggests that the NIDDK criteria may be too restrictive for clinical use. A retrospective study of 269 women judged to have a clinical diagnosis of IC found that more than 60% of those patients would not have been diagnosed with IC based on the NIDDK criteria.12
Table 1.
NIDDK Diagnostic Criteria for Interstitial Cystitis
| Automatic inclusion |
| Hunner’s ulcer |
| Positive factors (2 must be present for inclusion) |
| Pain on bladder filling relieved by emptying |
| Pain (suprapubic, pelvic, urethral, vaginal, or perineal) |
| Glomerulations on cystoscopy |
| Decreased compliance on cystometrogram |
| Exclusions |
| Nocturia < 2 times per night |
| Symptom duration < 12 mo |
| Bladder capacity > 400 mL |
| Involuntary bladder contractions |
| Other causes of symptoms: bladder cancer, cystitis (radiation, tuberculous, bacterial), vaginitis, active herpes, bladder or lower ureteral calculi, involuntary bladder contractions |
NIDDK, National Institute of Diabetes and Digestive and Kidney Diseases. Adapted with permission from Gillenwater JY and Wein AJ.17
There is increasing recognition that cystoscopy with hydrodistention, a requirement of the NIDDK criteria, may not be necessary for the diagnosis of IC/PBS.18,19 The key cystoscopic findings for the diagnosis of IC are the presence of Hunner’s ulcers and/or more than 10 glomerulations in 3 out of 4 quadrants of the bladder.12 However, Hunner’s ulcers are rare (present in as few as 4% of IC patients) and glomerulations (petechial hemorrhages) do not correlate with symptoms or histologic findings in IC, nor are they associated with differences in therapeutic response.18–20 There is also evidence that glomerulations are not specific for IC.19,21,22
Patients With Refractory Overactive Bladder May Have Interstitial Cystitis
Investigators have suggested that some patients diagnosed with OAB, particularly those refractory to treatment with anticholinergics, may have IC.7,23 One recent retrospective study examined the prevalence of IC in 47 symptomatic women diagnosed with idiopathic detrusor overactivity.7 Following a trial of oxybutynin and/or tolterodine or imipramine, 22 women (47%) had a satisfactory response to treatment (defined as > 50% improvement in urinary urgency, frequency, and/or urge incontinence).7 Of the 25 remaining women who were considered to have refractory detrusor overactivity, 24 (96%) had a positive potassium sensitivity test (PST), which supports the diagnosis of IC (80% sensitivity in IC patients).5,7 In a separate study of 28 women with refractory detrusor overactivity who had failed to respond to anticholinergics, 8 (29%) were found to have increased mast cell counts in the detrusor muscle, consistent with the histological features of IC. Five of the women with increased detrusor mast cell counts who also had clinical and cystoscopic features of IC, including petechial hemorrhages and decreased bladder capacity, were given treatment for IC, and in all cases the symptoms were relieved.24 These findings provide support for considering IC in patients with detrusor overactivity refractory to anticholinergic treatment.7
A prospective cohort study evaluated the prevalence of IC in 98 patients with symptoms of OAB, the majority of whom had not received any form of therapy.23 All patients underwent a PST, of whom 59 (60%) had a positive response. Cystoscopic hydrodistention under anesthesia was performed on 42 patients in the study, and 33 (79%) had glomerulations. Among the 42 patients who had cystoscopy in addition to the PST, 26 (62%) had positive findings on both tests, and only 4 patients (10%) had negative findings on both tests.23 In another study of 244 women who presented with mixed symptoms of stress incontinence and urge incontinence, a final diagnosis of IC was made in 19 patients (8%) according to criteria outlined by Messing, which included cystoscopic examination.25 These data provide further support that there should be a high index of suspicion for the diagnosis of IC in patients with symptoms of OAB who fail or have only a partial response to anticholinergic therapy and behavior modification.23
A recent case study of a 22-year-old woman who presented with a 3-year history of urgency, frequency, urge urinary incontinence, and dyspareunia illustrates the clinical challenge of differentiating OAB from IC based on clinical presentation.26 The patient had previously been treated with a prolonged course of nitrofurantoin following a diagnosis of chronic cystitis, and extended-release oxybutynin chloride and tolterodine for symptoms of OAB. She also practiced Kegel exercises with biofeedback, but she did not experience symptom improvement. On physical examination she had suprapubic tenderness, and on transvaginal palpitation had a tender bladder base that produced a “spasmlike” sensation identical to what she felt during coitus. Her maximum bladder capacity on cystometry was only 210 mL, and cystoscopy revealed mild erythema in her urethra, diffuse glomerulations throughout the bladder, and cascade bleeding with bladder refill. On the basis of these findings, her urogynecologist treated her for IC, including a dietary modification program and oral therapy with pentosan polysulfate sodium and hydroxyzine. On this treatment plan, the incontinence resolved and the patient reported a 90% improvement in urgency, frequency, and dyspareunia.26
Differentiating Interstitial Cystitis and Overactive Bladder
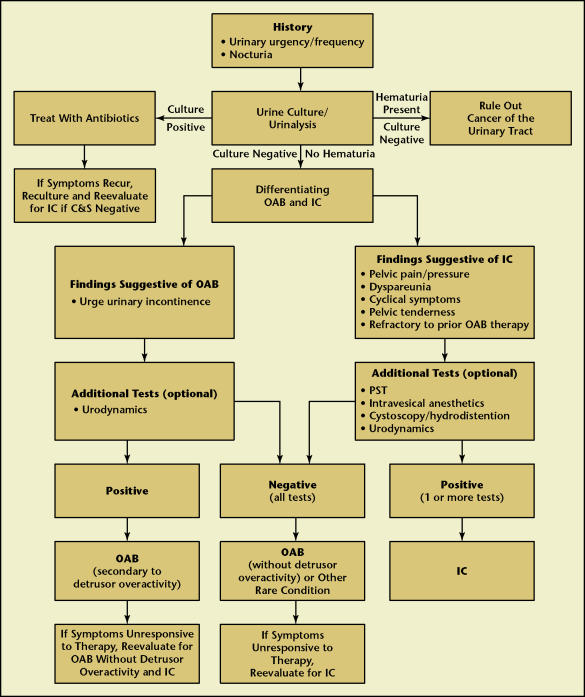
A diagnostic algorithm may be useful for differentiating IC from OAB in patients who present with urinary symptoms or in OAB patients who are refractory to treatment (Figure 3). Interstitial cystitis should be considered in any patient who fails to respond to therapy for OAB. It also is possible that the 2 conditions may exist concurrently. In 2 separate studies 14% to 15% of patients with IC also had detrusor overactivity.27,28 Other conditions that could potentially be responsible for a patient’s symptoms, such as neurologic disorders, gynecologic conditions, or infections, must also be ruled out during initial evaluations.
Figure 3.
Proposed diagnostic framework for differentiating interstitial cystitis and overactive bladder. IC, interstitial cystitis; C&S, culture and sensitivity; OAB, overactive bladder; PST, potassium sensitivity test.
The clinical evaluation should begin with a complete history and physical examination. Careful attention to the symptom history may help distinguish OAB from IC. Clinicians should be particularly attentive to reports of symptoms that occur with sexual intercourse or before menstruation, or those that are triggered by allergies, emotional stress, or certain foods, all of which may be associated with IC. Many patients with less severe IC may only report mild or intermittent pelvic discomfort or pressure rather than pelvic pain. Patients reporting only bladder storage symptoms should be questioned about dyspareunia. Patients with IC may experience a sense of bladder fullness even when the bladder contains only a small amount of urine, and may void frequently to avoid pain. Patients with OAB are more likely to report true urgency, defined as a sudden and compelling desire to void that cannot be easily deferred, and voiding out of fear of leakage.29 On physical examination, findings suggestive of IC include tenderness of the suprapubic area, anterior vaginal wall/bladder base, and/or levator ani musculature. The absence of other local pathologies, such as a urethral diverticulum, vulvodynia, or vaginitis should be ascertained. A voiding diary may play an important role in the evaluation of patients who have storage symptoms with or without pelvic pain. Patients with IC typically report more frequent urination than most patients with OAB.
Although not a characteristic feature of IC, detrusor instability and urge urinary incontinence have been reported in some cases of IC.7 Hohlbrugger and Riedl have suggested that in patients with IC who experience urgency, the pelvic floor may spontaneously go into a spasm (interpreted as pelvic pain) in order to avoid incontinence.30 Conversely, women with detrusor overactivity and good intrinsic urethral sphincteric function may be able to voluntarily contract their skeletal muscles during involuntary detrusor contractions to prevent leakage, but this may produce pain from high pressure detrusor contractions against a closed outlet. As a result, it may be difficult to distinguish the symptoms of OAB from IC in these patients, although transvaginal palpation of the bladder base that does not cause tenderness would suggest OAB.
The Pelvic Pain and Urgency/Frequency (PUF) and O’Leary-Sant (OLS) questionnaires are useful symptom screeners for IC.13,31 The PUF is an 8-question scale that measures both the severity of symptoms and the degree to which patients are troubled by them.13 Higher PUF scores have been shown to have a direct correlation with a greater likelihood of a positive PST.13 The OLS Symptom and Problem Indices each contain 4 questions that measure symptom severity and how problematic the symptoms are for patients.31
A number of other laboratory or office-based tests can also be helpful in narrowing the differential diagnosis. Urinalysis and urine culture should be performed to rule out bacterial cystitis. In patients with hematuria, urine cytology, cystoscopy, and radiography of the upper urinary tract should be done to exclude urolithiasis, cancer, or carcinoma in situ. Potassium sensitivity testing is useful for isolating the bladder as the source of pain and urgency symptoms. A positive PST suggests increased permeability of the bladder urothelium and lends support to the diagnosis of IC.32 In the PST, patients rate pain and urgency symptoms on a scale from 0 (none) to 5 (severe) after instillation of water into the bladder, and then again after instillation of potassium chloride.32 An increase in pain or urgency of 2 points or greater in response to the potassium solution compared with response from the control solution is considered a positive result.32 Conversely, improvement of pain upon intravesical instillation of an anesthetic solution can also be used to identify the bladder as the source of pain in patients with IC. The diagnostic role of the PUF questionnaire, PST, or intravesical anesthetic instillation in the evaluation of patients with OAB has not been established, although intravesical lidocaine has been used to treat detrusor overactivity and OAB symptoms.33 Urodynamic studies are useful for establishing the presence of detrusor overactivity in the OAB patient.34 Urodynamic findings commonly observed in women with IC include painful sensory urgency, elevated resting urethral closure pressures, and a dyssynergic-like voiding pattern.
For patients whose diagnosis remains unclear, cystoscopy with possible bladder biopsy may be helpful. Cystoscopy performed with hydrodistention may show certain characteristic findings in patients with IC, such as glomerulations (Figure 4) or Hunner’s ulcers (Figure 5). However, some investigators suggest that negative findings on cystoscopic examination alone are not sufficient to exclude the diagnosis of IC, and asymptomatic women have been found to have cystoscopic findings consistent with IC.21,35 Although bladder biopsy is primarily done to exclude carcinoma in situ, histological evidence of chronic inflammation, such as infiltration of mast cells into the submucosa and muscularis of the bladder, may be suggestive of IC.34 Bladder biopsies may also show normal findings in patients with IC.
Figure 4.
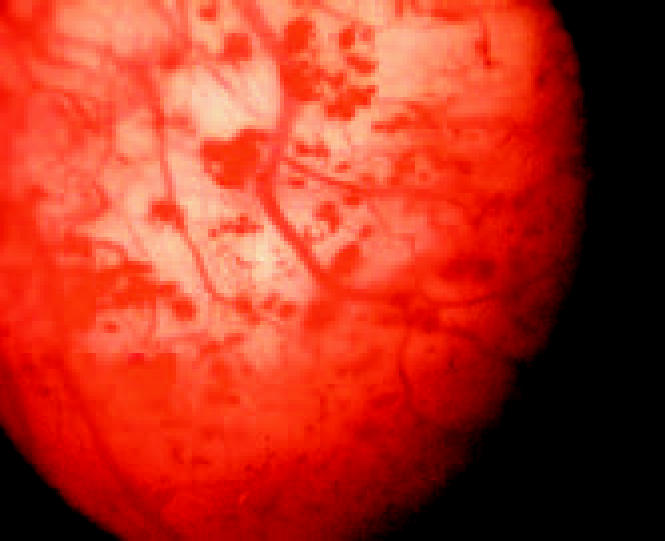
Glomerulations on cystoscopy.
Figure 5.
Hunner’s ulcer on cystoscopy. Photograph courtesy of Robert M. Moldwin, MD.
Conclusions
Overactive bladder and IC can present with similar symptoms, such as urinary urgency, frequency, and nocturia. Urge urinary incontinence is a common feature of OAB, whereas pelvic pain is typically associated with IC. Both OAB and IC, therefore, should be included in the differential diagnosis for any patient who presents with urgency and frequency. It is especially important that IC be considered in patients diagnosed with OAB who are refractory to therapy, such as antimuscarinics. It is possible that a significant percentage of these patients may respond successfully to treatment for IC. Differentiating IC from OAB continues to be challenging in the clinical setting, but the proposed diagnostic algorithm may be a useful tool for patient evaluation.
Main Points.
Both interstitial cystitis (IC) and overactive bladder (OAB) should be considered in the differential diagnosis for patients who present with urgency and/or frequency.
Urgency, frequency, and nocturia are symptoms of both IC and OAB, but the conditions may be differentiated by the presence of pelvic pain and dyspareunia in patients with IC, and urge urinary incontinence in patients with OAB.
Interstitial cystitis should be considered in any patient who is refractory to therapy for OAB, particularly anticholinergic therapy.
A history of symptoms that occur with sexual intercourse or before menstruation, or that are triggered by allergies, emotional stress, and certain foods may indicate IC.
A Pelvic Pain and Urgency/Frequency questionnaire or results from a potassium sensitivity test or intravesical anesthetic instillation procedure may aid in the diagnosis of IC, whereas urodynamics that establish the presence of detrusor overactivity and a voiding diary that identifies storage symptoms may help diagnose patients with OAB.
References
- 1.Abrams P, Cardozo L, Fall M, et al. The standardisation of terminology of lower urinary tract function: report from the Standardisation Sub-committee of the International Continence Society. Am J Obstet Gynecol. 2002;187:116– 126. doi: 10.1067/mob.2002.125704. [DOI] [PubMed] [Google Scholar]
- 2.Driscoll A, Teichman JMH. How do patients with interstitial cystitis present? J Urol. 2001;166:2118–2120. [PubMed] [Google Scholar]
- 3.Hanno P, Keay S, Moldwin R, Van Ophoven A. International Consultation on IC - Rome, September 2004/Forging an International Consensus: progress in painful bladder syndrome/interstitial cystitis. Report and abstracts. Int Urogynecol J Pelvic Floor Dysfunct. 2005;16(suppl 1):S2–S34. doi: 10.1007/s00192-005-1301-x. [DOI] [PubMed] [Google Scholar]
- 4.Porru D, Politano R, Gerardini M, et al. Different clinical presentation of interstitial cystitis syndrome. Int Urogynecol J Pelvic Floor Dysfunct. 2004;15:198–202. doi: 10.1007/s00192-004-1129-9. [DOI] [PubMed] [Google Scholar]
- 5.Parsons CL. Interstitial cystitis: epidemiology and clinical presentation. Clin Obstet Gynecol. 2002;45:242–249. doi: 10.1097/00003081-200203000-00025. [DOI] [PubMed] [Google Scholar]
- 6.Simon LJ, Landis JR, Erickson DR, et al. The Interstitial Cystitis Data Base Study: concepts and preliminary baseline descriptive statistics. Urology. 1997;49(suppl 5A):64–75. doi: 10.1016/s0090-4295(99)80334-3. [DOI] [PubMed] [Google Scholar]
- 7.Minaglia S, Özel B, Bizhang R, Mishell DR., Jr. Increased prevalence of interstitial cystitis in women with detrusor overactivity refractory to anticholinergic therapy. Urology. 2005;66:702–706. doi: 10.1016/j.urology.2005.04.042. [DOI] [PubMed] [Google Scholar]
- 8.Evans RJ. Treatment approaches for interstitial cystitis: multimodality therapy. Rev Urol. 2002;4(suppl 1):S16–S20. [PMC free article] [PubMed] [Google Scholar]
- 9.Theoharides TC, Kempuraj D, Sant GR. Mast cell involvement in interstitial cystitis: a review of human and experimental evidence. Urology. 2001;57(suppl 1):47–55. doi: 10.1016/s0090-4295(01)01129-3. [DOI] [PubMed] [Google Scholar]
- 10.Goldberg RP, Sand PK. Pathophysiology of the overactive bladder. Clin Obstet Gynecol. 2002;45:182–192. doi: 10.1097/00003081-200203000-00020. [DOI] [PubMed] [Google Scholar]
- 11.Kumar V, Templeman L, Chapple CR, Chess-Williams R. Recent developments in the management of detrusor overactivity. Curr Opin Urol. 2003;13:285–291. doi: 10.1097/00042307-200307000-00004. [DOI] [PubMed] [Google Scholar]
- 12.Hanno PM, Landis JR, Matthews-Cook Y, et al. The diagnosis of interstitial cystitis revisited: lessons learned from the National Institutes of Health Interstitial Cystitis Database study. J Urol. 1999;161:553–557. doi: 10.1016/s0022-5347(01)61948-7. [DOI] [PubMed] [Google Scholar]
- 13.Parsons CL, Dell J, Stanford EJ, et al. Increased prevalence of interstitial cystitis: previously unrecognized urologic and gynecologic cases identified using a new symptom questionnaire and intravesical potassium sensitivity. Urology. 2002;60:573–578. doi: 10.1016/s0090-4295(02)01829-0. [DOI] [PubMed] [Google Scholar]
- 14.Rosenberg MT, Hazzard M. Prevalence of interstitial cystitis symptoms in women: a population based study in the primary care office. J Urol. 2005;174:2231–2234. doi: 10.1097/01.ju.0000181203.82693.95. [DOI] [PubMed] [Google Scholar]
- 15.Nickel JC, Teichman JMH, Gregoire M, et al. Prevalence, diagnosis, characterization, and treatment of prostatitis, interstitial cystitis, and epididymitis in outpatient urological practice: the Canadian PIE Study. Urology. 2005;66:935–940. doi: 10.1016/j.urology.2005.05.007. [DOI] [PubMed] [Google Scholar]
- 16.Metts JF. Interstitial cystitis: urgency and frequency syndrome. Am Fam Physician. 2001;64:1199–1206. [PubMed] [Google Scholar]
- 17.Gillenwater JY, Wein AJ. Summary of the National Institute of Arthritis, Diabetes, Digestive and Kidney Diseases Workshop on Interstitial Cystitis, National Institutes of Health. J Urol. 1988;140:203–206. doi: 10.1016/s0022-5347(17)41529-1. [DOI] [PubMed] [Google Scholar]
- 18.Messing E, Pauk D, Schaeffer A, et al. Associations among cystoscopic findings and symptoms and physical examination findings in women enrolled in the Interstitial Cystitis Data Base (ICDB) Study. Urology. 1997;49(suppl 5A):81–85. doi: 10.1016/s0090-4295(99)80336-7. [DOI] [PubMed] [Google Scholar]
- 19.Ottem DP, Teichman JMH. What is the value of cystoscopy with hydrodistension for interstitial cystitis? Urology. 2005;66:494–499. doi: 10.1016/j.urology.2005.04.011. [DOI] [PubMed] [Google Scholar]
- 20.Erickson DR, Tomaszewski JE, Kunselman AR, et al. Do the National Institute of Diabetes and Digestive and Kidney Diseases cystoscopic criteria associate with other clinical and objective features of interstitial cystitis? J Urol. 2005;173:93–97. doi: 10.1097/01.ju.0000146466.71311.ab. [DOI] [PubMed] [Google Scholar]
- 21.Waxman JA, Sulak PJ, Kuehl TJ. Cystoscopic findings consistent with interstitial cystitis in normal women undergoing tubal ligation. J Urol. 1998;160:1663–1667. [PubMed] [Google Scholar]
- 22.Erickson DR. Glomerulations in women with urethral sphincter deficiency: report of 2 cases. J Urol. 1995;153:728–729. published correction appears in J Urol. 1995; 153:1955. [PubMed] [Google Scholar]
- 23.Chung MK, Butrick C, Chung RP, Shriver JS. The overlap of interstitial cystitis and overactive bladder. J Pelvic Med Surg. 2003;9:244. abstract. [Google Scholar]
- 24.Moore KH, Nickson P, Richmond DH, et al. Detrusor mast cells in refractory idiopathic instability. Br J Urol. 1992;70:17–21. doi: 10.1111/j.1464-410x.1992.tb15656.x. [DOI] [PubMed] [Google Scholar]
- 25.Awad SA, Gajewski JB, Katz NO, Acker-Roy K. Final diagnosis and therapeutic implications of mixed symptoms of urinary incontinence in women. Urology. 1992;39:352–357. doi: 10.1016/0090-4295(92)90212-f. [DOI] [PubMed] [Google Scholar]
- 26.Sand PK. Patient B: interstitial cystitis presenting as overactive bladder. Female Patient. 2002;(suppl):19–20. [Google Scholar]
- 27.Kirkemo A, Peabody M, Diokno AC, et al. Associations among urodynamic findings and symptoms in women enrolled in the Interstitial Cystitis Data Base (ICDB) Study. Urology. 1997;49(suppl 5A):76–80. doi: 10.1016/s0090-4295(99)80335-5. [DOI] [PubMed] [Google Scholar]
- 28.Awad SA, MacDiarmid S, Gajewski JB, Gupta R. Idiopathic reduced bladder storage versus interstitial cystitis. J Urol. 1992;148:1409–1412. doi: 10.1016/s0022-5347(17)36923-9. [DOI] [PubMed] [Google Scholar]
- 29.Abrams P. Describing bladder storage function: overactive bladder syndrome and detrusor overactivity. Urology. 2003;62(suppl 5B):28–37. doi: 10.1016/j.urology.2003.09.050. [DOI] [PubMed] [Google Scholar]
- 30.Hohlbrugger G, Riedl C. Non-bacterial cystitis. Curr Opin Urol. 2000;10:371–380. doi: 10.1097/00042307-200009000-00003. [DOI] [PubMed] [Google Scholar]
- 31.O’Leary MP, Sant GR, Fowler FJ, Jr, et al. The interstitial cystitis symptom index and problem index. Urology. 1997;49(suppl 5A):58–63. doi: 10.1016/s0090-4295(99)80333-1. [DOI] [PubMed] [Google Scholar]
- 32.Parsons CL, Greenberger M, Gabal L, et al. The role of urinary potassium in the pathogenesis and diagnosis of interstitial cystitis. J Urol. 1998;159:1862–1867. doi: 10.1016/S0022-5347(01)63178-1. [DOI] [PubMed] [Google Scholar]
- 33.Evans RJ. Intravesical therapy for overactive bladder. Curr Urol Rep. 2005;6:429–433. doi: 10.1007/s11934-005-0037-y. [DOI] [PubMed] [Google Scholar]
- 34.Selo-Ojeme DO, Onwude JL. Interstitial cystitis. J Obstet Gynaecol. 2004;24:216–225. doi: 10.1080/01443610410001660652. [DOI] [PubMed] [Google Scholar]
- 35.Clemons JL, Arya LA, Myers DL. Diagnosing interstitial cystitis in women with chronic pelvic pain. Obstet Gynecol. 2002;100:337–341. doi: 10.1016/s0029-7844(02)02087-2. [DOI] [PubMed] [Google Scholar]