Abstract
Objective
Puma (p53-upregulated modulator of apoptosis), a proapoptotic BH3-only member of the Bcl-2 protein family, has been implicated in the pathomechanism of several diseases, including cancer, AIDS, and ischemic brain disease. We have recently shown that Puma is required for cardiac cell death upon ischemia/reperfusion of mouse hearts. Since ischemia/reperfusion is also associated with endoplasmic reticulum (ER) stress, in the present study we investigated whether Puma contributes to the ER stress-dependent component of cardiomyocyte apoptosis.
Methods
Primary cultures of rat and mouse neonatal cardiomyocytes were treated with 3 μM thapsigargin or 100 ng mL−1 tunicamycin. Puma levels were suppressed by adenoviral delivery of shRNA or targeted deletion of the puma gene. Puma expression was detected by RT-PCR and Western blotting. Apoptosis was assessed by TUNEL assay, caspase-3 cleavage, and cytochrome c release.
Results
We have shown that in rat neonatal cardiac myocytes, thapsigargin or tunicamycin treatment led to ER-stress, transcriptional upregulation of Puma, and apoptosis. Most importantly, cardiac myocytes acquired resistance to ER stress-induced apoptosis if Puma expression was downregulated by adenoviral delivery of shRNA or eliminated by targeted deletion in knockout mice.
Conclusion
Taken together, our data indicate that Puma is a critical component of ER stress-induced apoptosis in cardiac myocytes, and inhibition of Puma activity may be used to treat cardiac infarcts or prevent heart failure by blocking ER stress-induced apoptosis.
Keywords: Myocytes, Apoptosis, SR function, Signal transduction
1. Introduction
Over recent years the endoplasmic reticulum (ER) has become increasingly recognized as a highly dynamic and multifunctional signaling organelle [1]. The ER is a principal site for secretory protein synthesis and folding, calcium (Ca2+) storage and signaling, and is also involved in the regulation of several other fundamental cellular processes, including programmed cell death (apoptosis) [1,2].
Nascent secretory proteins are synthesized on ER ribosomes and posttranslationally modified within the ER lumen to adopt their native conformation. In a normally functioning ER, there is a balance between the translocation of newly synthesized unfolded proteins into the ER and the secretion of mature, correctly folded proteins [3]. If this balance is disturbed, the ER responds by attempting to accommodate to the changes in its environment [3]. The adaptive mechanisms – collectively referred to as the Unfolded Protein Response (UPR) - include the activation of a highly conserved transcriptional program to increase the protein folding capacity of the ER, the degradation of misfolded proteins, and the inhibition of global protein synthesis [4].
The signaling pathways involved in the UPR are relatively well characterized [3–5]. In a normally functioning cell, the ER-resident chaperones, for example BiP (Grp78), bind to the ER sensory proteins PKR-like endoplasmic reticulum kinase (PERK), activating transcription factor 6 (ATF6) and endoribonuclease inositol-requiring enzyme-1 (Ire1) [3–5]. When unfolded proteins accumulate in the ER, however, they rapidly occupy the chaperones, and consequently, the ER sensory proteins are released, become activated and launch the UPR [3–5]. Upon removal of the chaperones, the protein kinase PERK oligomerizes, and phosphorylates the eukaryotic initiation factor 2-alpha (eIF2α), leading to transient suppression of protein synthesis and decreased ER workload [4]. Liberated ATF6 translocates to the Golgi apparatus and is cleaved by proteases, resulting in a highly potent transcription factor that promotes transcription of ER-resident chaperons and folding enzymes [4]. Oligomerized Ire1 results in production of the active form of X box-binding protein 1 (XBP-1), which is another transcription factor involved in induction of genes responsible for protein folding [5].
The ER also regulates Ca2+ homeostasis by governing the movement of Ca2+ between the ER lumen and the cytosol. Ca2+ exits the lumen through the inositol 1,4,5-triphosphate receptors and the ryanodine receptors and is actively pumped back into the ER by the sarcoplasmic/endoplasmic reticulum Ca2+ ATPases (SERCAs) [2,6]. Since the function of ER-resident chaperones is Ca2+-dependent, in addition to accumulation of unfolded proteins, aberrant Ca2+ regulation in the ER also leads to activation of the UPR [2,7].
By coordinating the suppression of global protein synthesis and the upregulation of ER-resident chaperones and other relevant proteins, the UPR is often able to restore homeostasis, and, therefore, is cytoprotective [4,5,7]. Intense or persistent ER stress, however, triggers cell death, usually in the form of apoptosis [4,5,7]. The mechanism of ER stress-induced apoptosis has already been extensively investigated and well-known general regulators of the central apoptotic machinery, including the Bcl-2 family, have been identified to play a role in UPR [5,7,8]. While the antiapoptotic Bcl-2-like proteins blocked ER stress-induced apoptosis, both BH3-only (Bim, BIK and Puma) and multidomain (Bax and Bak) proapoptotic Bcl-2 family members were induced or activated by ER stress [5,7,8]. Importantly, Puma appeared to be critical for ER stress-induced apoptosis in neuronal cells, mouse embryonic fibroblasts and MCF7 breast carcinoma cells [9–11]. Interestingly, C/EBP homologous protein (CHOP), a proapoptotic transcription factor induced by ER stress was also suggested to be a regulator of Bcl-2-like proteins [4,5].
Several recent studies have highlighted the importance of ER stress in cardiac diseases. It was shown that pressure overload by transverse aortic constriction induced prolonged ER stress during progression from cardiac hypertrophy to heart failure [12]. It was also demonstrated that AMP-activated protein kinase protected cardiac myocytes against hypoxic injury by attenuating ER stress [13]. Consistent with these observations, aberrant ER quality control in transgenic mice with mutant Lys-Asp-Glu-Leu (KDEL) receptor (a receptor for ER chaperons) caused dilated cardiomyopathy [14]. Lastly, it was described that the UPR was activated during ischemia/reperfusion, and that the induction of ER stress genes by ATF6 protected against ischemia/reperfusion injury [15,16]. These studies indicate that ER stress-induced apoptosis may be involved in the pathogenesis of a variety of different cardiac diseases, in particular ischemic heart disease and heart failure. The role of Bcl-2 family proteins in ER stress-induced apoptosis in cardiomyocytes, however, has not yet been elucidated.
In a recent paper we described that the proapoptotic Bcl-2 family protein Puma is critical for ischemia/reperfusion-induced cell death in cardiomyocytes [17]. Since cardiac ischemia/reperfusion has been demonstrated to induce ER stress [13,15,16], in the current paper we investigated whether ER stress requires Puma to promote the apoptotic response. To our knowledge, our experiments demonstrate for the first time that Puma is critical for ER stress-dependent apoptosis in cardiomyocytes. Puma, therefore, may provide a potential target to block apoptotic cell death in the ischemic heart.
2. Methods
2.1. Isolation and culture of primary rat cardiomyocytes
Neonatal cardiac myocytes were prepared using the Percoll gradient method, as described earlier [17,18]. Cardiomyocytes were cultured for 24 h in a serum containing medium (4:1 Dulbecco’s modified Eagle’s medium (DMEM):medium 199 (M199), 10% heat-inactivated horse serum (HS), 5% heat-inactivated fetal bovine serum (FBS), 100 units/ml penicillin, 100 μg/ml streptomycin, 10 mM glutamine, and 0.2 mM bromodeoxyuridine (BrdU)). Following a 24 h incubation period, serum containing medium was replaced with a low serum medium (4:1 DMEM:M199, 5% heat inactivated HS, 100 units/ml penicillin, 100 μg/ml streptomycin, 10 mM glutamine, and 0.2 mM BrdU) to prevent hypertrophy.
2.2. Isolation, culture, and genotyping of primary mouse cardiomyocytes
Cardiomyocytes were isolated from hearts of one-day-old pups of wild-type and Puma knockout mice, as described earlier for rats [17,18], with minor modifications. Briefly, non-myocyte contaminants were removed by 2 rounds of pre-plating for 2 h on 35-mm plastic tissue culture dishes in a humidified incubator at 37°C with 5% CO2. Cardiomyocytes from each animal were plated separately into 2 wells of a 24-well tissue culture plate and cultured in serum-containing medium. Following a 24 h incubation period, serum-containing medium was replaced with low-serum medium to prevent hypertrophy. Following seeding, mice were genotyped using tail DNA as described earlier [17,18].
This investigation conforms with the Guide for the Care and Use of Laboratory Animals published by the US National Institutes of Health (NIH Publication No. 85–23, revised 1996).
2.3. Preparation of adenoviral shRNA (Ad.shRNA)
Using the previously described pSuppressorAdeno gene suppression system [19], we generated several Ad.shRNA constructs and selected two for further experiments. The first -designated Ad.shRNA-p - led to a significant decrease in Puma levels, whereas the second –designated Ad.shRNA-c – was inactive. The sequence of the inserts in these recombinant adenoviruses corresponds to two distinct 21 base pair regions within the Rattus norvegicus Puma cDNA (accession number AY157758.1). Recombinant adenoviruses were generated according to the manufacturer’s instructions (Imgenex Corporation). Briefly, complementary oligonucleotides were synthesized representing 21-mer sense and anti-sense PUMA sequences with Xho I and Xba I overhangs, respectively. Sense and anti-sense sequences were separated by a short hairpin sequence (5’-ATCGAT-3’), which encodes a Cla I restriction endonuclease site. shRNA-c encodes a 21-mer sequence complementary to Rattus norvegicus Puma nucleotides 1324 – 1345 (5’-GAGCATATGAGCCAAACCTGA-3’). shRNA-p encodes a 21-mer sequence complementary to nucleotides 1560 – 1581 (5’-CGTGTGACCACTGGCATTCAT-3’). Sense and anti-sense oligonucleotides were annealed and the resulting hairpins cloned into Xho I and Xba I of the shuttle plasmid IMG-1200-1. Cloning was confirmed using Cla I digestion. Shuttle plasmids were then cotransfected into HEK293 cells along with adenovirus backbones for generation of adenoviral genomes. Adenoviruses were then amplified in HEK293 cells and purified as described earlier [17,18,20].
2.4. Adenovirus infections and induction of ER stress
Cardiac myocytes were infected with adenoviruses (multiplicity of infection of 25–50 plaque-forming units/cell) for 2 h, after which the virus-containing medium was replaced with a virus-free medium and cells were incubated for up to 72 h. ER stress was then induced by treating the cells with 3 μM thapsigargin or 100 ng mL−1 tunicamycin for the indicated times, or left untreated.
2.5. Cell culture and transfection
MCF7 cells were cultured in DMEM supplemented with 10% heat-inactivated FBS, 100 units/ml penicillin, 100 μg/ml streptomycin, and 10 mM glutamine. Transfection with pCDNA3.0-PUMA (rat) was performed using FuGENE 6 (Roche) according to the manufacturer’s instructions.
2.6. Immunoblot analysis
Immunoblot analysis was performed as described earlier [17,21]. Briefly, cells were lysed in radioimmunoprecipitation assay (RIPA) buffer complemented with protease inhibitors. Protein samples (10–20 μg) were electrophoresed in 15% denaturing polyacrylamide gels (BioRad) and then transferred onto nitrocellulose membranes. Membranes were incubated with primary antibodies specific for PUMAα NT (Imgenex), actin (Sigma), cleaved caspase 3 (Cell Signaling Technology), and cytochrome c (BD Biosciences), followed by incubation with horseradish peroxidase-conjugated secondary antibodies. Proteins were identified using the SuperSignal chemiluminescence system (Pierce).
2.7. Semi-quantitative RT-PCR
RNA was isolated from cardiomyocytes using Trizol reagent (Invitrogen) and processed according to the manufacturer’s instructions. Reverse transcription was performed with the iScript cDNA synthesis kit (BioRad) using 1μg total RNA, and semi-quantitative PCR was carried out using the following primers: PUMA 5’-TGGGTGCACTGATGGAGATA-3’ (sense), 5’-AACCTATGCAATGGGATGGA-3’ (anti-sense), BiP 5’-GCCACGGGATGGTTCCTTGCC-3’ (sense), 5’-GCGGATCCAGGTCGACGCCGG-3’ (anti-sense), CHOP 5’-CGGAACCTGAGGAGAGAGTG-3’ (sense), 5’-CGTTTCCTGGGGATGAGATA-3’ (anti-sense), 18S 5’-CGGCGACGACCCATTCGAAC-3’ (sense), 5’-GAATCGAACCCTGATTCCCCGTC-3’ (anti-sense).
2.8. Immunocytochemistry
Immunocytochemical analysis was performed as previously described [17,18], with minor modifications. Briefly, cardiac myocytes were cultured on gelatin-coated 8-well plastic chamber slides and fixed in 3.7% formaldehyde (in 1x PBS) for 10 min. Cells were then permeabilized with 0.5% Triton-X-100 in 1x PBS for 5 min, incubated in blocking buffer (5% goat serum and 1% BSA in 1x PBS) and then probed with primary and secondary antibodies in blocking buffer. Sections were analyzed by confocal fluorescence microscopy (Bio-Rad). Apoptotic cells were detected using the terminal deoxynucleotidyltransferase-mediated UTP in situ nick end labeling (TUNEL) method (Roche). Sections were costained with anti-sarcomeric actinin (Sigma).
2.9. Cell viability assays
Cell viability assays were performed using the CellTiter 96 Aqueous One Solution Cell Proliferation assay, according to the manufacturer’s instruction (Promega). Briefly, cells were cultured on gelatin-coated 96-well plates at a density of 8.0 x 104 cells/ml. Following treatment, cells were incubated in the presence of the assay reagent at 37°C for 4 h. Optical densities were recorded at 490 nm.
2.10. Detection of cytosolic cytochrome c
Isolation of the cytosolic fraction for the detection of cytochrome c was performed as previously described [21].
3. Results
3.1 Induction of ER stress promotes Puma expression and apoptosis in neonatal cardiac myocytes
To determine whether ER stress-induced apoptosis is mediated by expression of the Puma protein in cardiomyocytes, isolated cells from neonatal rat hearts were treated with the SERCA inhibitor thapsigargin or with tunicamycin, which blocks ER protein glycosylation. Both thapsigargin and tunicamycin were earlier shown to induce ER stress in cardiac cells [12]. We then followed the ER stress response by analyzing the mRNA levels of two ER stress-specific proteins, the chaperone BiP and the transcription factor CHOP, using RT-PCR. Following treatment with thapsigargin and tunicamycin, both BiP and CHOP were induced after 4 h of treatment, reached maximal levels at 12 h, and receded back to basal levels by 24 or 48 h (Fig. 1A–B).
Fig. 1.
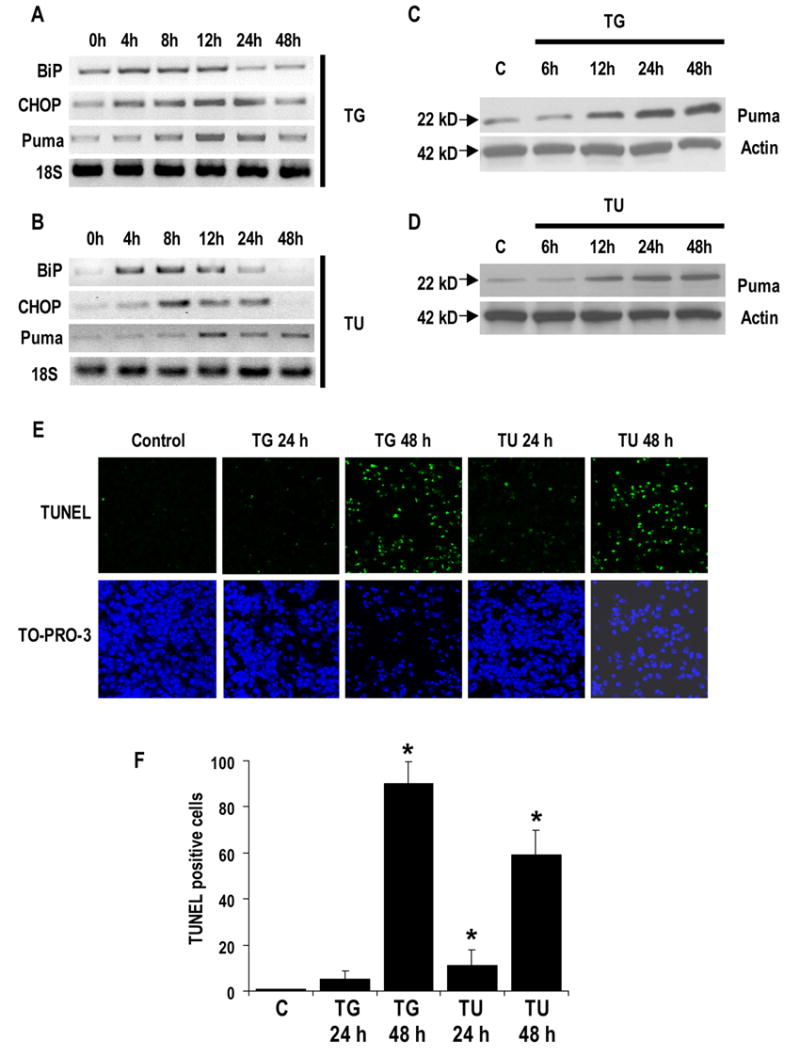
Thapsigargin and tunicamycin-induced ER stress promotes PUMA expression and apoptosis. A, B, C, and D, thapsigargin (TG) and tunicamycin (TU)-induced ER stress expression profiles in cardiac myocytes. Cardiomyocytes were grown in tissue culture dishes and exposed to 3 μM thapsigargin or 100 ng mL−1 tunicamycin for up to 48 h. A and B, samples were collected at 4, 8, 12, 24, and 48 h time points following the addition of thapsigargin or tunicamycin and semi-quantitative RT-PCR was performed using oligonucleotides directed against BiP, CHOP, Puma, and 18S as a loading control. C and D, samples were collected at 6, 12, 24, and 48 h time points after the addition of thapsigargin or tunicamycin. Immunoblot analysis was performed using anti-Puma antibodies. Actin is shown as a loading control. E, identification of apoptotic cardiac myocytes. Cardiomyocytes were grown on plastic chamber slides and treated with 3 μM thapsigargin or 100 ng mL−1 tunicamycin. At 24 and 48 h time points, cells were stained for apoptosis by TUNEL assay (green) and nuclei were identified by staining with TO-PRO-3 (blue). Images were taken using a confocal fluorescence microscope at 100X magnification. F, quantification of cardiomyocyte apoptosis. Apoptotic nuclei were scored on the basis of TUNEL positivity as described in E. Data are averaged from three experiments in 10 randomly selected fields (at least 200 cells) from each group. Error bars represent the S.E. of the mean. *, significant difference from the control (p < 0.01).
Following the induction of the ER-stress response, Puma mRNA was also upregulated, albeit delayed in comparison with BiP and CHOP, with the first signs of induction observed at 8 h and maximal induction at 12 h (Fig. 1A–B). By 48 h, Puma mRNA levels almost returned to the control level (Fig. 1A–B). This transcriptional Puma induction was accompanied by a corresponding increase in Puma protein levels (Fig. 1C–D). However, while Puma mRNA levels were barely detectable at 48 h, Puma protein was still highly elevated (Fig. 1C–D). Interestingly, the kinetics of Puma expression were comparable for both ER stress activators.
Since Puma is a proapoptotic member of the Bcl-2 family, we next determined whether Puma induction was followed by concomitant increase in apoptosis. As expected, elevated Puma expression was accompanied by apoptosis, as discerned using TUNEL assay. After 24 h of thapsigargin treatment, less than 10% of the cells were TUNEL positive. At the 48 h time-point, however, the majority of cells were apoptotic. A similar pattern was observed following tunicamycin treatment, however, overall, a lower percentage of apoptotic cell death was recorded for tunicamycin at 48 h (Fig.1 E–F).
These experiments demonstrate that thapsigargin-induced Ca++ release and tunicamycin-induced inhibition of ER protein glycosylation trigger Puma expression and cardiomyocyte apoptosis in parallel with the induction of ER-stress-specific chaperones and transcription factors.
3.2. Development of an adenoviral shRNA for knocking down Puma
To further investigate the importance of Puma in ER stress-induced apoptosis of cardiac myocytes, we developed recombinant adenoviruses encoding anti-Puma short hairpin RNA (shRNA) to suppress Puma mRNA levels. Several adenoviral constructs were generated and tested for anti-Puma activity. Two of these adenoviral shRNAs were selected and designated as Ad.shRNA-p and Ad.shRNA-c, based on their ability to knock down Puma. The efficacy of these constructs was validated by analyzing exogenous and endogenous Puma expression.
Ad.shRNAs were initially tested against exogenous Puma using MCF7 cells transfected with plasmids carrying the rat puma cDNA (pCMS-puma). While Ad.shRNA-p efficiently decreased the rat Puma protein levels, Ad.shRNA-c did not evoke any significant effect (Fig. 2A). To analyze the efficacy of the Ad.shRNA in cardiomyocytes, we infected isolated rat neonatal cardiac myocytes with different concentrations of shRNA adenoviruses and analyzed endogenous Puma protein expression levels. Consistent with the data obtained from MCF7 cells, endogenous Puma expression levels were reduced in a concentration-dependent manner when cardiomyocytes were infected with Ad.shRNA-p (Fig. 2B). In contrast, Ad.shRNA-c had no effect on endogenous rat Puma expression (Fig. 2B).
Fig. 2.
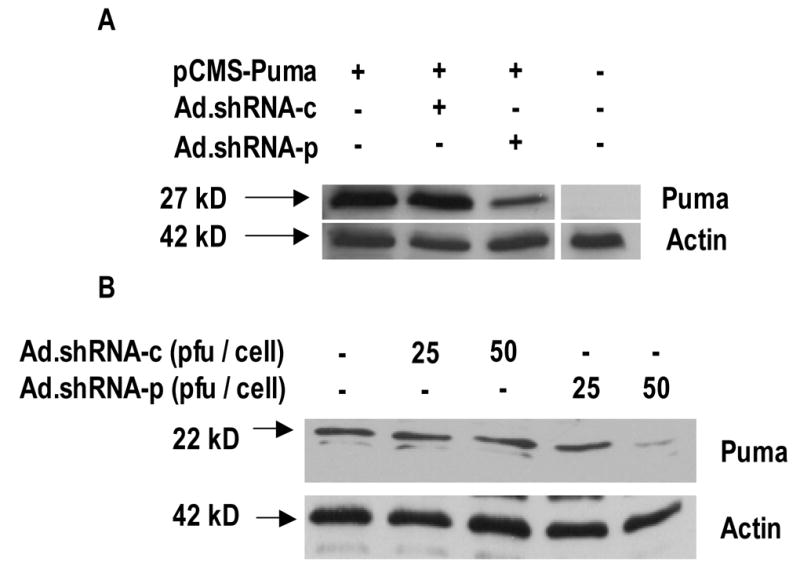
Ad.shRNA-p attenuates both exogenous and endogenous Puma expression. A, validation of shRNA by transient transfection. MCF7 cells plated at a density of 1.5 × 106 cells were infected with either the pSuppressorAdeno (non-recombinant virus), Ad.shRNA-c, or Ad.shRNA-p and incubated for 48 h. Cells were then transfected with pCMS-Puma and incubated for an additional 24 h - a total of 72 h. Immunoblot analysis was performed using anti-Puma antibody. The position of exogenous FLAG-tagged Puma band is indicated by an arrow. Actin is shown as a loading control. Results are representative of three independent experiments. B, validation of shRNA in cardiac myocytes. Cells were grown in tissue culture dishes and infected with either Ad.shRNA-c or Ad.shRNA-p for 72 h. Immunoblot analysis was performed using anti-Puma antibody. Actin is shown as a loading control. Results are representative of three independent experiments.
These data indicate that Ad.shRNA-p efficiently downregulates Puma levels whereas Ad.shRNA-c is ineffective. In later experiments these two viruses were used either to knock down Puma levels or as a negative control virus, respectively.
3.3. Inhibition of thapsigargin-induced Puma expression by adenoviral delivery of shRNA in cardiac myocytes
We next examined whether shRNA-p is able to effectively suppress the induction of Puma mRNA and protein by thapsigargin. Cardiac myocytes were infected with shRNA adenoviruses for 72 h prior to thapsigargin treatment to allow preloading of cytoplasmic shRNA. Cells were then exposed to thapsigargin for 12 h and collected for mRNA and protein analysis. Using RT-PCR we found that Ad.shRNA-p, but not Ad.shRNA-c, inhibited puma mRNA accumulation induced by thapsigargin (Fig. 3A). This effect was specific, because neither BiP, nor CHOP mRNA levels were affected in identical samples (Fig. 3A). Consistent with the mRNA changes, induction of the Puma protein by thapsigargin was blocked only by shRNA-p, whereas shRNAc did not have any effect (Fig. 3B).
Fig. 3.
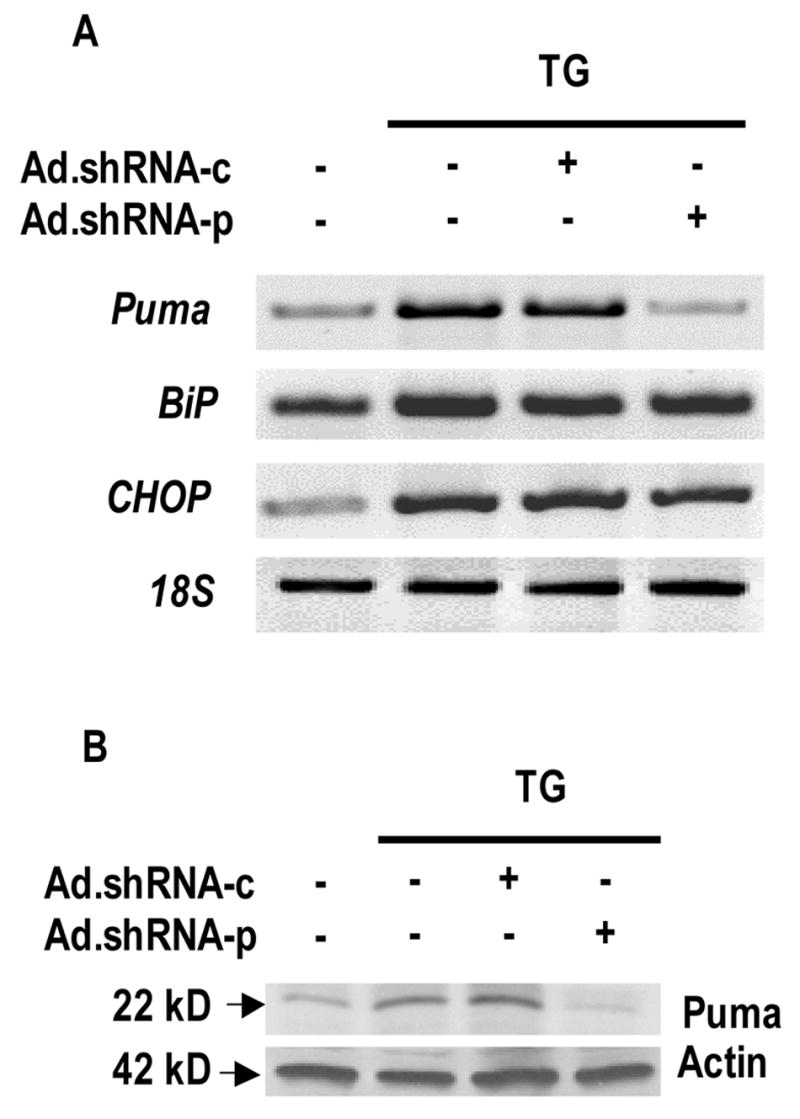
Ad.shRNA-p inhibits Puma expression during thapsigargin-induced ER stress in cardiac myocytes. Cardiomyocytes were grown in tissue culture dishes and infected with either Ad.shRNA-c or Ad.shRNA-p for 72 h. Cells were then exposed to 3 μM thapsigargin for an additional 12 h. A, semi-quantitative RT-PCR was performed using oligonucleotides directed against BiP, CHOP, Puma, and 18S as a loading control. B, immunoblot analysis was performed using anti-Puma antibodies. Actin is shown as a loading control.
In summary, the shRNA-p virus specifically blocks expression of the Puma mRNA and protein upon thapsigargin induction.
3.4. Inhibition of thapsigargin-induced apoptosis in cardiac myocytes
To determine if Puma is essential for ER-stress-induced cardiomyocyte apoptosis, we treated control and Ad.shRNA infected cells with thapsigargin and tunicamycin for 48 h, at which time-point we identified widespread apoptosis in earlier experiments (Fig. 1E–F). Subsequently, the rate of apoptosis was measured with TUNEL assay. In control cells or Ad.shRNA infected cells we observed less than 5% apoptosis (Fig. 4A–B). In contrast, more than 70% of the cells exposed to thapsigargin underwent apoptosis, and this was not significantly inhibited by Ad.shRNA-c (Fig. 4A–B). Importantly, Ad.shRNA-p, which was shown to decrease Puma expression under several different conditions (Fig. 2–3), reduced apoptosis to approximately 10% (Fig. 4A–B). Similarly, close to 50% of the cells exposed to tunicamycin underwent apoptosis, and again, this response was inhibited by Ad.shRNA-p to less than 20% (Fig. 4A–B). Ad.shRNA-c had no effect. Of note, representative high magnification micrographs of healthy (no virus), dead (TG) and rescued (Ad.shRNA-p) cardiac myocytes stained by alpha-actinin and TO-PRO3 are shown in Fig. 4C.
Fig. 4.
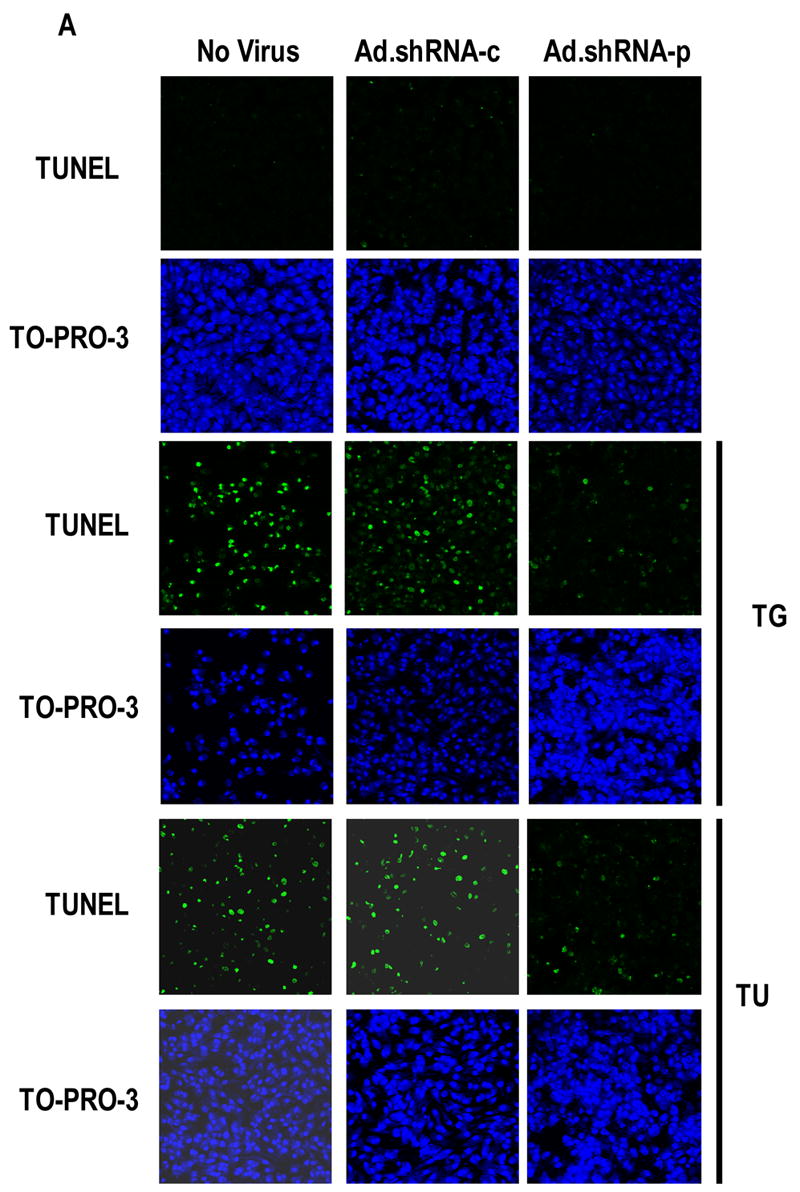
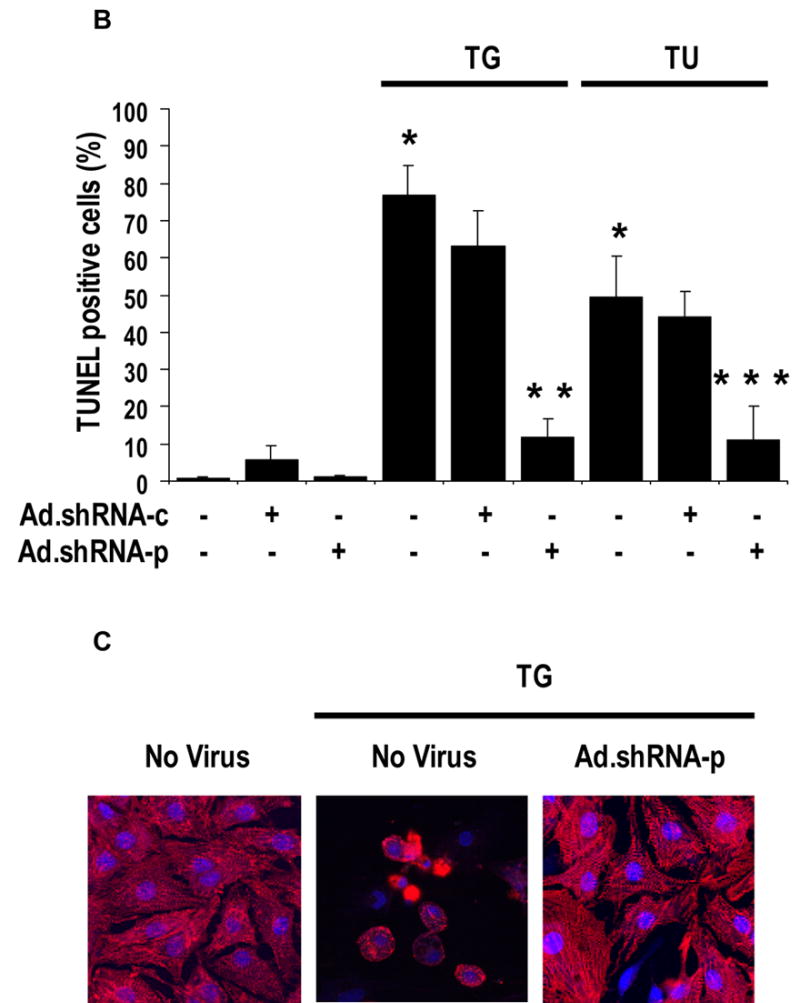
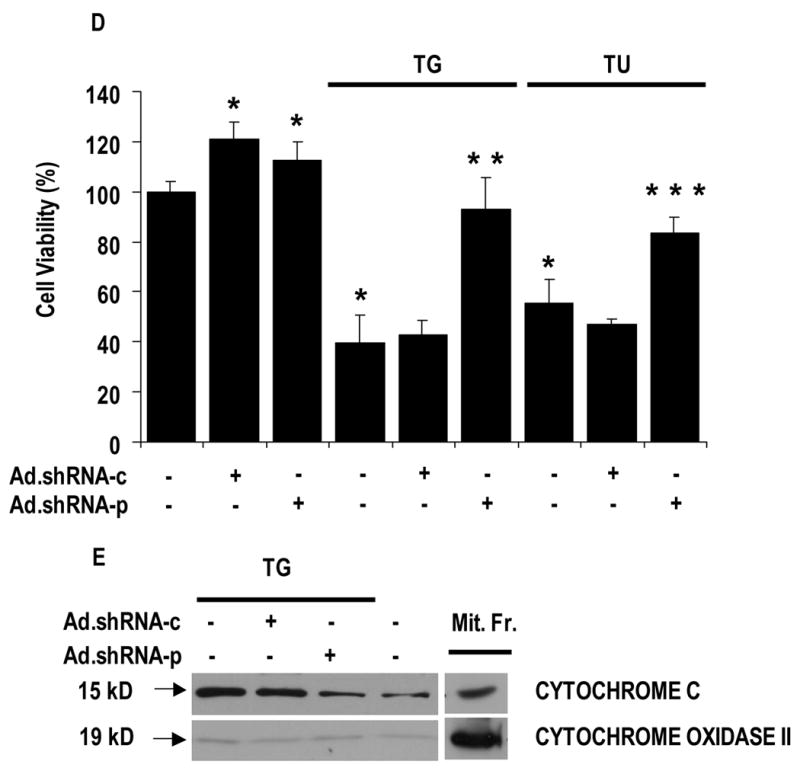
Suppression of Puma attenuates thapsigargin and tunicamycin-induced apoptosis in cardiac myocytes. A, Ad.shRNA-p reduces thapsigargin and tunicamycin-induced apoptosis. Cardiomyocytes were grown in tissue culture dishes and infected with either Ad.shRNA-c or Ad.shRNA-p for 48 h. Cells were then exposed to 3 μM thapsigargin or 100 ng mL−1 tunicamycin for an additional 48 h. Cells were stained for apoptosis by TUNEL assay (green) and nuclei were identified by staining with TO-PRO-3 (blue). Images were taken using a confocal fluorescence microscope at 100X magnification. B, quantification of cardiomyocyte apoptosis. Apoptotic nuclei were scored on the basis of TUNEL positivity as described in A. Data are averaged from three experiments in 10 randomly selected fields (at least 200 cells) from each group. Error bars represent the S.E. of the mean. *, significant difference from the control (p < 0.01). **, significant difference from the TG group (p < 0.01). ***, significant difference from the TU group (p < 0.01). C. High magnification micrographs of cardiomyocytes subjected to treatment with TG, TG plus Ad.shRNA-p, or left untreated, as described in A. Cells were stained with anti-sarcomeric actinin (red) and TO-PRO-3 (blue). Images were taken using a confocal fluorescence microscope at 400X magnification. D, quantification of cardiomyocyte viability. Cardiomyocytes were grown in 96-well tissue culture plates and were infected with either Ad.shRNA-c or Ad.shRNA-p for 48 h. Cells were then exposed to 3 μM thapsigargin or 100 ng mL−1 tunicamycin for an additional 48 h. Cell viability was then assessed using the CellTiter 96 Aqueous One solution. Optical densities were recorded at 490 nm. Data are averaged from 3 independent experiments, each comprising 5 independent replicates. Error bars represent the S.E of the mean. *, significant difference from the control (p < 0.01). **, significant difference from the TG group (p < 0.01). ***, significant difference from the TU group (p < 0.01). E. Ad.shRNA-p prevents thapsigargin-induced cytochrome c release into the cytosol. Cardiomyocytes were grown and treated as described in A. Equal amounts of cytosolic proteins were immunoblotted for cytochrome c and cytochrome oxidase subunit 2 (as control), along with similar amounts of mitochondrial fractions of non-treated cells (Mit.Fr.).
To ascertain the viability of the TUNEL negative cells, we determined the number of viable cells following the various treatments, using a Promega kit (see Methods). In thapsigargin treated cells, the number of viable cells decreased to less than half of the control and this was unaffected by the presence of Ad.shRNA-c, whereas the viability of Ad.shRNA-p treated cells remained close to 100% (Fig. 4D). Importantly, a similar pattern of viability changes was observed upon tunicamycin treatment (Fig. 4D). In summary, the viability data shown in Fig. 4D are consistent with the TUNEL assay measurements presented in Fig. 4A–B.
These data were corroborated by analyzing the amount of cytochrome c in the cytosol. We detected a small amount of cytochrome c in the cytosol, probably due to partial disruption of mitochondria during cell fractionation (Fig. 4E). Cytochrome c release was significantly induced upon thapsigargin treatment or if thapsigargin was combined with infection with Ad.shRNA-c (Fig. 4E). In contrast, Ad.shRNA-p effectively decreased cytosolic cytochrome c to a level comparable to the control (Fig. 4E). Collectively, these data provide evidence that Puma is a critical factor for ER stress-induced apoptosis in cardiomyocytes, because downregulation of Puma blocks cardiomyocyte apoptosis.
3.5. ER stress-induced apoptosis is inhibited in puma−/− neonatal mouse cardiac myocytes
To corroborate that Puma is a critical factor for ER stress-induced apoptosis in cardiac myocytes, we compared the sensitivity of isolated mouse wild-type, puma+/− and puma−/−cardiomyocytes to thapsigargin treatment. Based on data of Fig. 1, isolated cells were exposed to 3 μM thapsigargin for 48 h and then assayed for caspase-3 cleavage and Puma expression by immunoblotting. Following the induction of ER stress, we observed a significant increase in the proteolytic cleavage of caspase-3 in samples obtained from both wild-type and heterozygous animals (Fig. 5). In contrast, in puma−/− cardiomyocytes, thapsigargin treatment did not affect the cleavage of caspase-3 (Fig. 5). Consistent with the genotypes, the basal level of Puma was detected only in puma+/+ cardiomyocytes, where Puma was strongly induced by thapsigargin (Fig. 5). Basal Puma expression was not detected in heterozygous cells, but was increased following thapsigargin treatment, albeit at a lower level than in puma+/+ cells (Fig. 5). Finally, in puma−/− cardiomyocytes, Puma was not detected, independently of the thapsigargin treatment (Fig. 5).
Fig. 5.
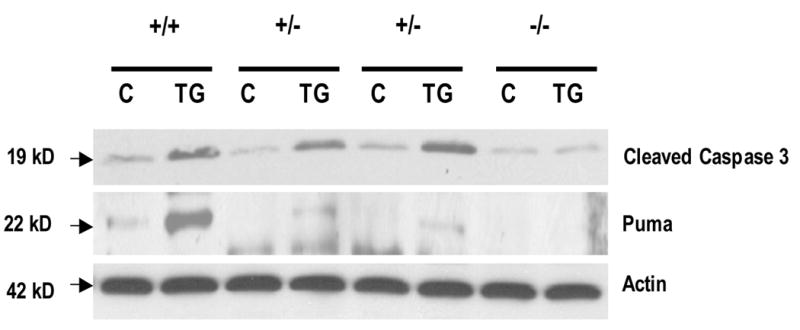
Targeted deletion of Puma inhibits thapsigargin-induced apoptosis. Cardiomyocytes isolated from wild-type (n = 5), puma+/− (n = 4), and Puma−/− (n = 3) mice were grown in tissue culture dishes and exposed to 3 μM thapsigargin for 48 h, or left untreated. Immunoblot analysis was performed using cleaved capase 3 and Puma antibodies. Actin is shown as a loading control. Data are representative of at least three independent experiments.
These data together confirm that Puma is a critical factor for ER stress-induced cardiomyocyte apoptosis. They also suggest that reaching a threshold in Puma levels is sufficient to induce apoptosis, resulting in similar sensitivity of wild-type and heterozygote cardiomyocytes to ER stress-induced apoptosis. Importantly, this phenomenon was also seen by other investigators earlier in other cell types using different apoptosis inducers [27].
4. Discussion
In a recent study, we demonstrated that cardiomyocytes with Puma deletion acquire resistance to ischemia/reperfusion-induced cell death [17]. Since ischemia/reperfusion causes protein misfolding and consequent ER stress [15,16], in our current study we aimed to determine whether the ER stress component of ischemia/reperfusion injury is also dependent on Puma activity in cardiac myocytes. There are three well-characterized experimental ways to provoke ER stress by pharmacological inducers. These include agents that interfere with the function of ER-resident glycosylases, such as tunicamycin, that inhibit the formation of disulfide bonds, such as dithiothreitol, and that lower calcium levels in the ER, such as thapsigargin [3]. In these studies, we used the SERCA inhibitor thapsigargin, which promotes leakage of Ca2+ from the ER [22] and, thereby, blocks the function of Ca2+-dependent ER-resident chaperons, including BiP (Grp78), Grp94 and calreticulin [4]. We have also applied tunicamycin, which induces accumulation of misfolded proteins and ER stress without directly causing cytoplasmic Ca2+ overload.
We have demonstrated with multiple assays that Puma is a critical component of ER stress-induced apoptosis in cardiomyocytes. Our data provide evidence that Puma is transcriptionally activated during ER stress and that its expression is clearly necessary for the development of apoptosis. However, our studies do not identify the transcription factor responsible for ER stress-related induction of Puma. Puma was originally described as a p53-inducible target gene [23,24]. Despite this, it is less likely that induction of Puma during ER stress of cardiac myocytes is p53-dependent for several reasons. Firstly, in cardiac myocytes hypoxia/reoxygenation-induced apoptosis requires Puma [17], but not p53 [25,26]. Secondly, Puma is known to be activated in a p53-independent manner by several inducers, including cytokine removal, dexamethasone and serum starvation [27–29]. Finally, in neuronal cells and in embryonic mouse fibroblasts, the induction of Puma by ER stress does not depend on p53 [9–11]. Moreover, in recent studies, p53 was inhibited, not activated by ER stress, probably through a glycogen synthase kinase-3-dependent mechanism [30,31]. Our experiments rather suggest that CHOP could be responsible for ER stress-induced Puma activation, because CHOP activation preceeds Puma activation in cardiac myocytes (Fig. 1). In addition, upon CHOP overexpression, induction of apoptosis can be inhibited by Bcl-2 [4,5], suggesting that CHOP activates a proapoptotic Bcl-2 family member, potentially Puma. Consistent with this hypothesis, the CHOP promoter contains binding sites for all major inducers of the ER stress response, such as ATF4, ATF6 and XBP-1. Finally, CHOP is activated by two well known proapoptotic proteins, p38-MAP kinase and JNK [4,5]. The hypothesis that CHOP activates the Puma gene in cardiomyocytes exposed to ER stress is now under investigation in our laboratory.
ER stress-induced cell death appears to be especially important in the heart where increased protein synthesis triggered by hypertrophy of cardiomyocytes may overload the ER chaperone system, leading to cell death. This may further aggravate cardiac remodeling, eventually culminating in dilatation of the heart and heart failure. In fact, recent papers have described that ER stress occurs in the heart upon ischemia/reperfusion, which is suggested to contribute to the pathogenesis of heart failure [12–16]. Our current paper provides evidence that Puma is an essential component of the ER stress pathway in cardiac myocytes, because suppressed Puma expression leads to inhibition of experimentally induced ER stress. Similarly, we showed earlier that ischemia/reperfusion-induced cell death also required Puma [17]. Together these studies strongly suggest that Puma provides a novel therapeutic target to block apoptosis associated with ischemic heart disease and heart failure. In addition, inhibition of Puma may improve the viability of transplanted cells used for cardiac cell therapy.
Acknowledgments
The authors are grateful to Dr. Noriaki Ikemoto (Boston Biomedical Research Institute) for critically reading the manuscript, to Dr. Subhas Biswas (Columbia University) for the rat puma plasmid, and to Drs. John Jeffers and Gerald Zambetti (St. Jude Children’s Hospital) for the Puma knockout mice. This work was supported by grants from NIH (HL-68126 to P.E.), from NSF (MCB-9982789 to P.E.), and by an American Heart Association fellowship (to A.T.).
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Berridge M. The endoplasmic reticulum: a multifunctional signaling organelle. Cell Calcium. 2002;32:235–49. doi: 10.1016/s0143416002001823. [DOI] [PubMed] [Google Scholar]
- 2.Wehrens X, Lehnart S, Marks A. Intracellular calcium release and cardiac disease. Annu Rev Physiol. 2005;67:69–98. doi: 10.1146/annurev.physiol.67.040403.114521. [DOI] [PubMed] [Google Scholar]
- 3.Stavridi E, Halazonetis T. p53 and stress in the ER. Genes Dev. 2004;18:241–4. doi: 10.1101/gad.1181704. [DOI] [PubMed] [Google Scholar]
- 4.Xu C, Bailly-Maitre B, Reed J. Endoplasmic reticulum stress: cell life and death decisions. J Clin Invest. 2005;115:2656–64. doi: 10.1172/JCI26373. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Boyce M, Yuan J. Cellular response to endoplasmic reticulum stress: a matter of life or death. Cell Death Differ. 2006;13:363–73. doi: 10.1038/sj.cdd.4401817. [DOI] [PubMed] [Google Scholar]
- 6.Diaz M, Graham H, O neill S, Trafford A, Eisner D. The control of sarcoplasmic reticulum Ca content in cardiac muscle. Cell Calcium. 2005;38:391–6. doi: 10.1016/j.ceca.2005.06.017. [DOI] [PubMed] [Google Scholar]
- 7.Crow M, Mani K, Nam Y, Kitsis R. The mitochondrial death pathway and cardiac myocyte apoptosis. Circ Res. 2004;95:957–70. doi: 10.1161/01.RES.0000148632.35500.d9. [DOI] [PubMed] [Google Scholar]
- 8.Foo R, Mani K, Kitsis R. Death begets failure in the heart. J Clin Invest. 2005;115:565–71. doi: 10.1172/JCI24569. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Rao R, Ellerby H, Bredesen D. Coupling endoplasmic reticulum stress to the cell death program. Cell Death Differ. 2004;11:372–80. doi: 10.1038/sj.cdd.4401378. [DOI] [PubMed] [Google Scholar]
- 10.Reimertz C, Kgel D, Rami A, Chittenden T, Prehn J. Gene expression during ER stress-induced apoptosis in neurons: induction of the BH3-only protein Bbc3/PUMA and activation of the mitochondrial apoptosis pathway. J Cell Biol. 2003;162:587–97. doi: 10.1083/jcb.200305149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Li J, Lee B, Lee A. Endoplasmic reticulum stress-induced apoptosis: multiple pathways and activation of p53-up-regulated modulator of apoptosis (PUMA) and NOXA by p53. J Biol Chem. 2006;281:7260–70. doi: 10.1074/jbc.M509868200. [DOI] [PubMed] [Google Scholar]
- 12.Okada K, Minamino T, Tsukamoto Y, Liao Y, Tsukamoto O, Takashima S, et al. Prolonged endoplasmic reticulum stress in hypertrophic and failing heart after aortic constriction: possible contribution of endoplasmic reticulum stress to cardiac myocyte apoptosis. Circulation. 2004;110:705–12. doi: 10.1161/01.CIR.0000137836.95625.D4. [DOI] [PubMed] [Google Scholar]
- 13.Terai K, Hiramoto Y, Masaki M, Sugiyama S, Kuroda T, Hori M, et al. AMP-activated protein kinase protects cardiomyocytes against hypoxic injury through attenuation of endoplasmic reticulum stress. Mol Cell Biol. 2005;25:9554–75. doi: 10.1128/MCB.25.21.9554-9575.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Hamada H, Suzuki M, Yuasa S, Mimura N, Shinozuka N, Takada Y, et al. Dilated cardiomyopathy caused by aberrant endoplasmic reticulum quality control in mutant KDEL receptor transgenic mice. Mol Cell Biol. 2004;24:8007–17. doi: 10.1128/MCB.24.18.8007-8017.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Martindale J, Fernandez R, Thuerauf D, Whittaker R, Gude N, Sussman M, et al. Endoplasmic Reticulum Stress Gene Induction and Protection From Ischemia/Reperfusion Injury in the Hearts of Transgenic Mice With a Tamoxifen- Regulated Form of ATF6. Circ Res. 2006;98:1186–93. doi: 10.1161/01.RES.0000220643.65941.8d. [DOI] [PubMed] [Google Scholar]
- 16.Azfer A, Niu J, Rogers L, Adamski F, Kolattukudy P. Activation of endoplasmic reticulum stress response during the development of ischemic heart disease. Am J Physiol Heart Circ Physiol. 2006;291:1411–20. doi: 10.1152/ajpheart.01378.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Toth A, Jeffers J, Nickson P, Min J, Morgan J, Zambetti G, et al. Targeted Deletion of Puma Attenuates Cardiomyocyte Death and Improves Cardiac Function during Ischemia/reperfusion. Am J Physiol Heart Circ Physiol. 2006;291:52–60. doi: 10.1152/ajpheart.01046.2005. [DOI] [PubMed] [Google Scholar]
- 18.Toth A, Nickson P, Qin L, Erhardt P. Differential regulation of cardiomyocyte survival and hypertrophy by MDM2, an E3 ubiquitin ligase. J Biol Chem. 2006;281:3679–89. doi: 10.1074/jbc.M509630200. [DOI] [PubMed] [Google Scholar]
- 19.Xia H, Mao Q, Paulson H, Davidson B. siRNA-mediated gene silencing in vitro and in vivo. Nat Biotechnol. 2002;20:1006–10. doi: 10.1038/nbt739. [DOI] [PubMed] [Google Scholar]
- 20.Anderson R, Haskell R, Xia H, Roessler B, Davidson B. A simple method for the rapid generation of recombinant adenovirus vectors. Gene Ther. 2000;7:1034–8. doi: 10.1038/sj.gt.3301197. [DOI] [PubMed] [Google Scholar]
- 21.Erhardt P, Schremser E, Cooper G. B-Raf inhibits programmed cell death downstream of cytochrome c release from mitochondria by activating the MEK/Erk pathway. Mol Cell Biol. 1999;19:5308–15. doi: 10.1128/mcb.19.8.5308. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Inesi G, Sagara Y. Specific inhibitors of intracellular Ca2+ transport ATPases. J Membr Biol. 1994;141:1–6. doi: 10.1007/BF00232868. [DOI] [PubMed] [Google Scholar]
- 23.Yu J, Zhang L, Hwang P, Kinzler K, Vogelstein B. PUMA induces the rapid apoptosis of colorectal cancer cells. Mol Cell. 2001;7:673–82. doi: 10.1016/s1097-2765(01)00213-1. [DOI] [PubMed] [Google Scholar]
- 24.Nakano K, Vousden K. PUMA, a novel proapoptotic gene, is induced by p53. Mol Cell. 2001;7:683–94. doi: 10.1016/s1097-2765(01)00214-3. [DOI] [PubMed] [Google Scholar]
- 25.Bialik S, Geenen D, Sasson I, Cheng R, Horner J, Evans S, et al. Myocyte apoptosis during acute myocardial infarction in the mouse localizes to hypoxic regions but occurs independently of p53. J Clin Invest. 1997;100:1363–72. doi: 10.1172/JCI119656. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Webster K, Discher D, Kaiser S, Hernandez O, Sato B, Bishopric N. Hypoxia-activated apoptosis of cardiac myocytes requires reoxygenation or a pH shift and is independent of p53. J Clin Invest. 1999;104:239–52. doi: 10.1172/JCI5871. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Jeffers J, Parganas E, Lee Y, Yang C, Wang J, Brennan J, et al. Puma is an essential mediator of p53-dependent and -independent apoptotic pathways. Cancer Cell. 2003;4:321–8. doi: 10.1016/s1535-6108(03)00244-7. [DOI] [PubMed] [Google Scholar]
- 28.Han J, Flemington C, Houghton A, Gu Z, Zambetti G, Lutz R, et al. Expression of bbc3, a pro-apoptotic BH3-only gene, is regulated by diverse cell death and survival signals. Proc Natl Acad Sci U S A. 2001;98:11318–23. doi: 10.1073/pnas.201208798. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Villunger A, Michalak E, Coultas L, Mllauer F, Bock G, Ausserlechner M, et al. p53- and drug-induced apoptotic responses mediated by BH3-only proteins puma and noxa. Science. 2003;302:1036–8. doi: 10.1126/science.1090072. [DOI] [PubMed] [Google Scholar]
- 30.Pluquet O, Qu L, Baltzis D, Koromilas A. Endoplasmic reticulum stress accelerates p53 degradation by the cooperative actions of Hdm2 and glycogen synthase kinase 3beta. Mol Cell Biol. 2005;25:9392–405. doi: 10.1128/MCB.25.21.9392-9405.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Qu L, Koromilas A. Control of tumor suppressor p53 function by endoplasmic reticulum stress. Cell Cycle. 2004;3:567–70. [PubMed] [Google Scholar]


