Abstract
Background
Intimate partner abuse is very common among female patients in family practice. In general, doctors overlook the possibility of partner abuse.
Aim
To investigate whether awareness of intimate partner abuse, as well as active questioning, increase after attending focus group and training, or focus group only.
Design of study
Randomised controlled trial in a stratified sample.
Setting
Family practices in Rotterdam and surrounding areas.
Method
A full-training group (n = 23), a group attending focus group discussions alone (n = 14), and a control group (n = 17) were formed. Data were collected with incident reporting of every female patient (aged >18 years) that was suspected of, or presented, partner abuse during a period of 6 months. The primary outcome measure was the number of reported patients; the secondary outcome measure was the number of patients with whom the GP had non-obvious reasons to suspect/discuss abuse.
Results
Comparison of the full-training group (n = 87 patients) versus the control group (n = 14 patients) resulted in a rate ratio of 4.54 (95% confidence interval [CI] = 2.55 to 8.09, P<0.001); the focus group only group (n = 30 cases) versus control group: rate ratio of 2.2 (95% CI = 1.14 to 4.26, P = 0.019); full-training versus the focus group only group: rate ratio of 2.19 (95% CI = 1.36 to 3.52, P = 0.001). Comparison of the full-training group with the untrained groups for awareness of partner abuse in case of non-obvious signs resulted in: odds ratio 5.92 (95% CI = 2.25 to 15.62, P<0.01) all corrected for sex, district, practice setting, working part-/full-time, experience, and age of the doctor.
Conclusions
Training was the most significant determinant to improve awareness and identification of intimate partner abuse. Active questioning increased, especially where there were non-obvious signs. The focus group on its own doubled the awareness of partner abuse.
Keywords: abused women, family medicine, general practitioners, intimate partner abuse, randomised controlled trial, training
INTRODUCTION
Increasingly, research shows that there is a high prevalence of intimate partner abuse worldwide.1 Cross-sectional studies among female patients in waiting rooms of family practices consistently report that 37–41% of women have experienced physical, sexual, and/or emotional abuse by an intimate partner at some stage in their lives.2–4 These studies found that most women who experienced violence in their relationship are not identified, that only 5% had been asked about it by their family doctor, and that there is a poor recording of abuse in medical records.3,4 Family doctors, although in a unique position to identify abuse, are in general not aware of the possibility of partner abuse.5,6 Also, barriers such as fear of opening ‘Pandora's box,’ time constraints, aversion of the problem, and discomfort with the double role of caring for both victim and perpetrator, are universal in this respect.7,8
On the other hand, a majority of female patients approve of being asked about abuse during consultation.3,4,9 This suggests that doctors should take a more active role in addressing abuse. However, training in identifying and responding to partner abuse is mostly lacking.10,11 Disappointing results from educational programmes, screening protocols, guidelines, and mandatory continuing medical education (CME) to increase identification, indicate that there is still a lack of knowledge on how to reach healthcare professionals on this subject.12,13
How this fits in
Intimate partner abuse is highly prevalent among women visiting family practice although doctors, in general, are not aware of the possibility of partner abuse. As such, training should focus on recognising patients with non-obvious signs of partner abuse. The health consequences of partner abuse are underestimated.
The debate between experts, arguing that all women in healthcare settings should be routinely questioned about partner abuse versus those that underline more targeted case-finding, continues.13–17 Intimate partner abuse is not a disease that can simply meet the accepted screening criteria and, moreover, physicians, in the majority, do not favour screening.13,17 Consultation time in medical practice is limited and medical visits should be effective and meaningful.
Many consultations with abused women result in diagnostic tests, referrals to medical specialists and physiotherapists, as well as the prescribing of medication in search of explanations for chronic somatic complaints. However, the real nature of their problem remains concealed.18 Being aware and recognising non-obvious signs related to partner abuse followed by active questioning, could be a more appropriate way to identify abused women and lower the barriers to talking about their problem. This method reflects the common situation in family practice, where a doctor is familiar with a patient's medical history, personal background and, ideally, provides confidentiality and continuity of care.
Considering these facts, the following questions are raised:
Will training be effective in stimulating family doctors to question women more actively about partner abuse when they suspect it and will identification increase?
Can doctors' awareness of the possibility of partner abuse in patients presenting non-obvious signs increase through training?
METHOD
Definitions
According to the literature we defined ‘intimate partner abuse’ as physical, sexual, emotional, or psychological abuse.19 We focused on female victims (≥18 years) who had been abused by a male partner.
Participants
To calculate the sample size we combined findings from a systematic review and cross-sectional studies.2–4,13 We judged that prevalence figures of partner abuse among female patients in waiting rooms of family practice in Australia, Ireland, and the UK with a comparable system of family practice would match the situation in the Netherlands. In order to calculate the proportion of cases that would occur during our intervention period of 6 months, we used the estimate that a full-time practitioner sees one to two female patients a week, who are undetected victims of partner abuse.2 Together with the baseline identification of 0–3% by Ramsay et al,13 we estimated the proportion of case-finding in 6 months in the control group to be 0.5 cases (0.01 of the total) and the proportion in the experimental group on 2.5 cases (0.05). A sample of 50 participants was needed for a significance level of 0.05 and a power of 80%.
All registered family doctors (n = 412) in Rotterdam and surrounding areas were mailed in October 2002 and invited to participate in the study. Fifty-four family doctors agreed to join the study (26 male, 28 female) and were included. Most participants were keen to join in and only 18 doctors had to be approached actively to maximise the diversity of the sample in order to cover all types of districts (wealthy, mixed, deprived), practice settings (solo-group practices, health centres), their age groups (<40 years, 40–50 years, >50 years), and sex.
Design
The design and process of this study is outlined in Figure 1.
Figure 1.
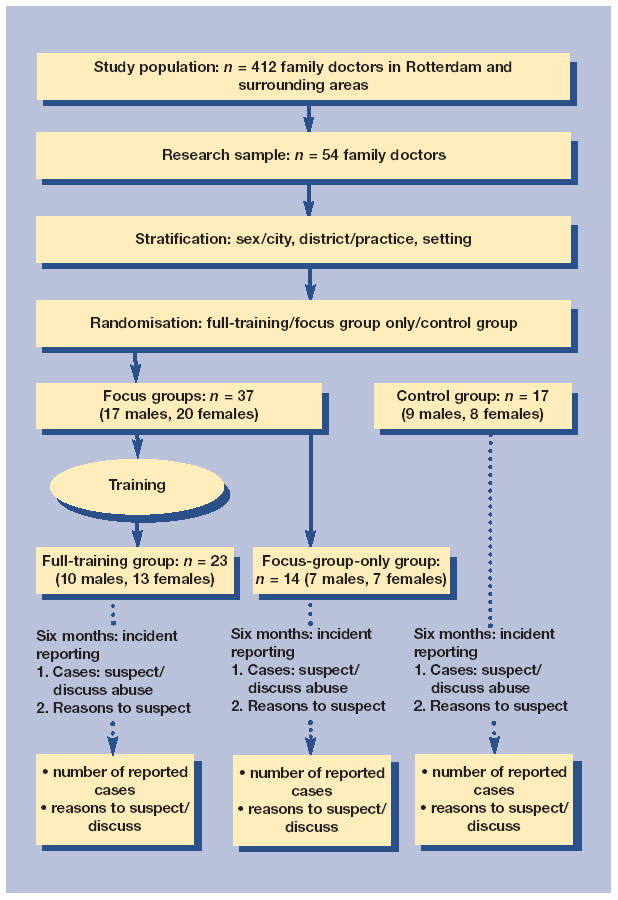
Design intervention study.
Randomisation
Participants were numbered at first and then grouped into strata, according to sex, district type (wealthy-mixed-deprived), and finally to practice type (solo-working in group practice or health centre). Members of a team, (group practice or health centre), were linked to each other and marked with a team letter. The research assistant, blinded against the participants' name and that of the group practice or health centre, executed the randomisation by sequential assignment of a number to a group.
The study groups
Three groups were formed: ‘full-training’ (n = 24), ‘focus-group alone’ (n = 14), and control (n = 16). After one male participant in the full-training group fell ill, he had to be moved to the control group. The study groups were intentionally different due to the training, which required 12 participants per training group in order to maximise comfort in dealing with a sensitive matter; in this way groups were neither too large nor too small. This resulted in a full-training group of two subgroups. In the course of preparing the training, the insight arose that the focus group discussion in itself was an experiment and had to be compared as such. Furthermore, we chose to enlarge the control group as opposed to the others to cope with eventual fallout.
Participants working in the same practice were allocated to the same group to avoid contamination of the intervention. After randomisation we distinguished, both in the full-training and control group, four clusters of two participants and in the focus-group alone group, one cluster of three participants. This resulted finally in a cluster-size of 1.2. Nevertheless, we assumed that asking women about partner abuse took place during a one-to-one conversation, as part of the consultation. Moreover, most cluster members worked part-time hours, and on different days. We, therefore, did not take clustering into account in recruiting our sample.
Effect measures
The dependant variable of the study was the doctor's performance. Our primary effect measure was the number of reported cases wherein partner abuse was discussed or suspected. Our secondary effect measure was the number of cases with non-obvious signs to suspect/discuss partner abuse.
We aimed to improve doctors' awareness of non-obvious complaints/disorders presented by women, as signs of a hidden background of partner abuse. These signs were dealt with, and listed, as key features of partner abuse in the handout notes of the training.
Key features were derived from studies on health consequences of violence against women and consisted, among others, of increased healthcare utilisation, unexplained chronic pain, depression, sleeping problems, and somatisation disorder in particular.18,20–26 Seven categories were formed to cover all signs to suspect and discuss abuse. Categories 1, 2, and 3 were defined as obvious signs; categories 4, 5, 6, and 7 were defined as non-obvious signs (Box 1).
Box 1. Categories and signs to suspect/discuss intimate partner abuse.
Obvious signs
-
▸
Patient initiated disclosure of abuse
-
▸
Recently abused or abuse known to the doctor
-
▸
Injury
Non-obvious signs
-
▸
Undefined somatic complaints/chronic pain
-
▸
Mental complaints/disorder: for example, depression, sleeping problems, anxiety, substance abuse
-
▸
Combination of somatic and mental complaints/disorders
-
▸
Others
Data collection
In line with our study aim to measure awareness of partner abuse and active questioning, we used incident reporting to collect data. The participants registered and reported cases during 6 months when:
The doctor suspected and asked about abuse, whether the abuse was confirmed or not, taking into account that denial is common in abused women who are asked for the first time.6,18,27
The doctor suspected but did not ask, mostly for safety reasons.
The patient initiated disclosure of abuse.
Cases were registered on numbered forms, anonymously, with a patient's study number and electronic medical file number alone. Each case could only be reported once.
Doctors were asked to specify their reasons for suspecting and/or discussing abuse briefly, in their own words:
The control group (n = 17) started with the registration and reporting of cases after personal instruction by the research assistant (weeks 12–38 in 2003).
The focus group only group (n = 14) took part in a focus group discussion in February 2003; they then began to register and report cases after personal instruction by the research assistant (weeks 12–38 in 2003).
The full-training group (n = 23) took part in the focus group discussion and followed a 1.5 day training session on partner abuse in May 2003. After this, they started to register and report cases. Instruction took place at the end of the training (weeks 20–46 in 2003).
All registered cases were reported to the researcher. At the end of the 6-month period, all signs filled out on the forms were categorised by the researcher.
Focus groups and training
The focus group discussion that preceded the training was considered a low-grade intervention. We conducted six group discussions, led by a qualified social scientist, and explored, in a focused way, views, experiences, barriers, and practices regarding partner abuse. In these structured group discussions, which took 1.5 hours each, participants were encouraged to question one another and discuss the subject. The topics that emerged from the focus groups were applied in the training.
The training (Box 2) was developed to deal with all the negative associations towards abused patients and provide tools to overcome these barriers. The aim was to enhance awareness of non-obvious signs, to increase active questioning, and to improve professional attitude in responding to abused women. (The training provided nine CME credits).
Box 2. Contents of 1.5 day training.
-
▸
Attitude: aversions, prejudices and barriers; small group discussion; plenary clarification
-
▸
Theory: background and coping strategies in intimate partner abuse; profiles of perpetrators; effects on children
-
▸
Epidemiology: prevalence; clinical presentation and key features; patient's views
-
▸
Consultation skills: role play with diagnostic tool and clinic with simulation patient
-
▸
Information: Police Domestic Violence Programme; Abused Women's Agency
-
▸
Legal aspects: lawyer specialised in abuse
-
▸
Vignettes: pre- and post-testing of written cases
If partner abuse was discussed during consultation, the patient was informed about the study. Patients were unaware of the intervention the doctor received.
Analysis
Data of the participating doctors and the reported cases on the registration forms were entered into an SPSS statistical data file (12.0.1). We did not take clustering into account in the analysis due to the rather small cluster-size (1.2).
The main effect measure was the ‘number of reported cases’ followed a Poisson distribution in all three arms. First, we compared the full-training group with the control group, next we compared the focus group only group with the control group and, finally, the full-training group with the focus group only group. We compared all groups by using a multivariate Poisson regression analysis with the SAS statistical package (8.2 Genmode procedure). Comparison between the focus group only group and the full-training and control groups was done to assess part of our experiment: the effect of just talking in a focused way about the subject.
Regarding the secondary effect measure — number of cases with non-obvious signs — the trained group (full-training) and the untrained groups (focus group only group and control group) were compared by a multivariate logistic regression analysis with the SAS statistical package (8.2 Logistic procedure). To overcome possible imbalances, all computations were corrected for sex, age, experience, working hours, type of practice setting, and residential district.
RESULTS
The demographics of the study groups in the research sample compared with the study population are detailed in Table 1. Of all the family doctors in Rotterdam and its surrounding areas, 13% took part in the study. The research sample was more often female, younger, working part-time hours, shorter in residence, and practising in cooperation with others. None of the participants received previous training on any form of domestic violence. (This has not been on the programme of continuous medical education for more than 20 years and the number of papers on the subject that have been published in national medical journals has, until recently, been negligible.)
Table 1.
Demographics of study groups, research sample, population of family physicians of Rotterdam and surroundings.
| Demographic | Full-training n = 23 | Focus group only n = 14 | Control n = 17 | Research sample n = 54 (%) | Rotterdam family physicians populationa % (n = 415) |
|---|---|---|---|---|---|
| Sex | |||||
| Male | 10 | 7 | 9 | 26 (48.1) | 74 |
| Female | 13 | 7 | 8 | 28 (51.9) | 26 |
| Working hours | |||||
| Full-time ≥4 days | 8 | 5 | 4 | 17 (31.5) | 77 |
| Part-time <4 days | 15 | 9 | 13 | 37 (68.5) | 23 |
| Age category | |||||
| <40 years | 6 | 5 | 4 | 15 (27.8) | 13 |
| 40–50 years | 8 | 4 | 8 | 20 (37.0) | 43 |
| >50 years | 9 | 5 | 5 | 19 (35.2) | 44 |
| In residence | |||||
| <15 years | 11 | 9 | 9 | 29 (53.7) | 32 |
| ≥15 years | 12 | 5 | 8 | 25 (46.3) | 68 |
| District | |||||
| Wealthy | 7 | 3 | 3 | 13 (24.1) | |
| Mixed | 6 | 3 | 5 | 14 (25.9) | Not asked |
| Deprived | 10 | 8 | 9 | 27 (50.0) | |
| Practice type | |||||
| Solo practice | 4 | 5 | 2 | 11 (20.4) | 43 |
| Duo/group practiceb | 14 | 4 | 7 | 25 (46.3) | 42 |
| Health centrec | 5 | 5 | 8 | 18 (33.3) | 14 |
Source: Survey of the District Association of Family Physicians Rotterdam and Surroundings 2003.
Two or more doctors in one family practice.
Cooperation of family doctors with other primary healthcare professionals.
Number of reported cases
A total of 131 cases were reported in 6 months; Table 2 outlines the types of reported cases. The full-training group with 23 doctors (trained in two subgroups) reported 87 cases (mean 3.78; subgroups: 3.67, 3.91). In 11 of these cases (12.6%), partner abuse was not confirmed after questioning and in two cases (2.3%) the doctor did not ask because of an accompanying partner or child. The focus group only group, with 14 doctors, reported 30 cases (mean 2.14). The control group, with 17 doctors, reported 14 cases (mean 0.82).
Table 2.
Number (percentages) and type of reported cases (n = 131).
| Type of reported case | Full-training n (%) | Focus group only n (%) | Control n (%) | Total n (%) |
|---|---|---|---|---|
| Asked/abuse confirmed | 53 (60.9) | 17 (56.7) | 7 (50) | 77 (58.8) |
| Asked/abuse not confirmed | 11 (12.6) | 0 (0) | 0 (0) | 11 (8.4) |
| Suspected/not asked | 2 (2.3) | 0 (0) | 0 (0) | 2 (1.5) |
| Patient initiated disclosure | 21 (24.1) | 13 (43.3) | 7 (50) | 41 (31.3) |
| Total cases | 87 (99.9) | 30 (100) | 14 (100) | 131 (100) |
Regarding the reported cases of partner abuse, the number of patient-initiated disclosures decreased in the focus group only group and the full-training group in favour of more active questioning.
Analysis
As there was no difference between the two full-training subgroups, we performed all computations on the aggregate. All computations were corrected for sex, district, practice setting, working part-/full-time, experience, and age of the doctor.
Comparison of the full-training and control groups resulted in a rate ratio of 4.54 (95% confidence interval [CI] = 2.5 to 8.09, P<0.001), a significant effect of the training. Comparison of the focus group only group and control group resulted in a rate ratio of 2.20 (95% CI = 1.4 to 4.26, P = 0.019). Comparison of the full-training group and the focus group only group resulted in a rate ratio of 2.19 (95% CI = 1.36 to 3.52, P<0.001), reflecting the single effect of education. To assess the influence of sex on our outcomes, we compared the full-training and control groups, after correction for sex. We obtained the following outcomes: full-training versus control group, rate ratio of 0.90 (95% CI = 0.59 to 1.37, P = 0.612), a non-significant outcome.
In total, 11 women who were asked, did not confirm abuse. Comparing the study groups without these cases led to the following outcomes:
full-training and control group resulted in a rate ratio of 4.26 (95% CI = 2.35 to 7.74, P<0.001);
focus group only group and control group resulted in a rate ratio: 2.35 (95% CI = 1.19 to 4.66, P = 0.014);
full-training and focus-group-only group resulted in a rate ratio: 1.81 (95% CI = 1.13 to 2.90, P = 0.014).
Non-obvious reasons to suspect or discuss partner abuse
For an overview of reported categories of reasons, see Figure 2. This overview shows the variety of reasons to suspect or discuss partner abuse across the study groups with in the control group the highest percentages of ‘obvious’ signs (Box 1) versus the full-training group that shifted to the ‘non-obvious’ signs.
Figure 2.
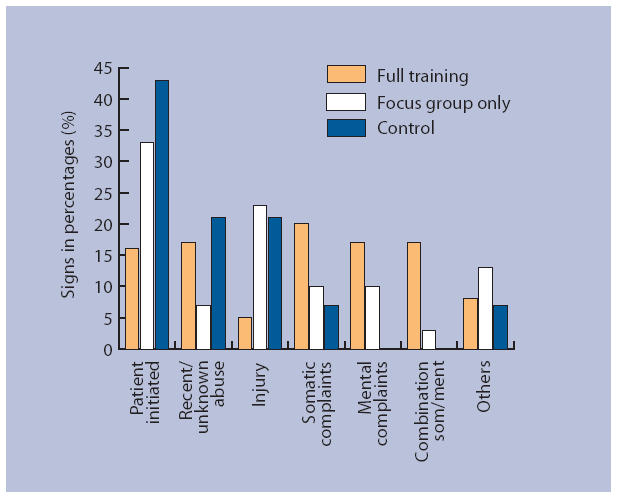
Signs (in percentages) to suspect/discuss intimate partner abuse, per study group.
In the category ‘others’, a mixture of non-obvious signs were presented. The most remarkable one was ‘behavioural problems of a child,’ sometimes referred by a school nurse or brought up by the mother.
Suspicions of partner abuse following the detection of non-obvious signs were greater in the full-training group compared with the focus group only and control groups (Figure 3).
Figure 3.
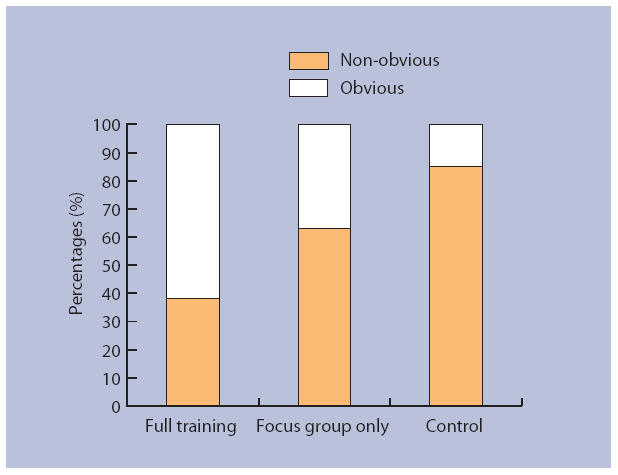
Percentages obvious versus non-obvious signs to suspect/discuss intimate partner abuse, per study group.
Analysis
We compared the full-training group with the other two groups that received no training (focus group only and control groups). The odds ratio to suspect or discuss partner abuse for non-obvious reasons or signs was 5.92 (95% CI = 2.25 to 15.62, P< 0.01) in the full-training group — a significant effect. The analysis was corrected for sex, district, practice setting, working part-/full-time, experience, and age of the doctor.
Several participants informed us during the 6-month intervention period that the training also provided them with tools to deal with other types of family violence. They also raised the issue of a gap during the intervention period, due to the summer holidays (3–4 weeks per participant) that may have reduced the number of reported cases. A future paper will explore extensively the hidden effects of the training.
DISCUSSION
Summary of main findings
This study demonstrates that a 1.5-day training session for family doctors increases awareness and identification of partner abuse in female patients by up to 4.5 times, while active questioning about abuse increases almost six times in the case of ‘non-obvious’ signs. In this respect the training is successful in overcoming existing barriers in attitude (such as feelings of powerlessness, fear to offend) and lack of knowledge.
The finding that focus group discussion alone doubled the rate of active questioning should be viewed as remarkable. Discussing one's prejudices and experiences on this subject with colleagues proved to make family doctors more alert. Although it lacks the effectiveness of knowledge, information, and practising of skills, its value lies in increased awareness.
Comparison with existing literature
An increase in the identification of topics that have been the subject of a training course, directly after it has taken place is a well-known positive effect. Most intervention studies assess numbers of screened patients according to a protocol with a short follow-up period and often show a decrease to baseline in the long term.28,29 Some experts stress that the effects of training without structural changes in the regular curriculum of CME are unlikely to change clinical practice.30 One of the differences with other studies is that in measuring the effects of brief training, these studies retrieve data from medical records with the number of screened patients as primary outcome.13,31 Our design focused more on the doctor–patient encounter and we measured doctors' performance, which is mostly evaluated in self-administered surveys or medical record reviews and rarely with incident reporting as we did. We also did not find any other study that evaluated training with the effect measure of recognising abuse in patients with non-obvious signs. However, our method proved to be reliable and can be duplicated.
Research on predictive indicators of partner abuse is ongoing and shows that injury is not a major indicator.32 There is enough evidence to suspect partner abuse in women with chronic undefined somatic complaints and mental complaints/disorders such as sleeping problems, anxiety, and depression.3,4,18,20–26,33 We used this evidence to provide a set of key features of the clinical presentation of partner abuse, which the intervention group applied successfully. Questioning women with these indicators (in fact the use of a ‘risk profile’) proved to lead to an increase of identification.
Strengths and limitations of the study
Several limitations of this study should be discussed. First, it is likely that family doctors with more interest in partner abuse than the norm signed up. Despite their supposed interest, however, there was much room to improve their awareness of partner abuse. Second, half of the participants were female, which may have influenced the outcomes, as some studies claim that female doctors detect more abuse in women.34 However, statistical analysis did not support a significant difference between male and female doctors.
Further, we did not take clustering into account in recruiting our final sample, mainly because of the cluster size (1.2), resulting in a somewhat underpowered study. However, the relative underpower of our study did not influence the effects and considering the significant outcomes, small P-values, and acceptable confidence intervals, our final sample size was justified.
Another limitation lies in the follow-up period of 6 months. Generally the effect of training tends to diminish in time;13,28 this aspect of longer-term follow-up was not included in our study.
Altogether the research sample represents 13% of the family doctors in Rotterdam and its surrounding areas. Comparison with the general population of family doctors could lead to even more striking results.
Thoughts on why we succeeded so well in this study must be viewed in the context of the prevalence of partner abuse among female patients in family practice. Hegarty et al estimated that every full-time family doctor sees one or two undetected cases every week.2 In this respect our results reveal just a bit more of the tip of the iceberg. Looking from another perspective, thorough training in recognising, responding to, and managing partner abuse in a population with a high prevalence and low baseline recognition, is bound to yield high results. Our trained participants, by overcoming their barriers, were able to lower the threshold to disclosing abuse. This change in attitude regarding female abuse is as much a benefit of the training sessions as knowledge on the subject.
Implications for clinical practice and future research
In the absence of solid evidence that training improves awareness and case finding, the debate continues between proponents of routinely questioning all women in the surgery on partner abuse (screening) and those who favour questioning of women who present symptoms and a medical history that could hide abuse (selective questioning and case-finding).17
It is known that doctors do not favour screening, mostly because of lack of education, effective interventions, and fear of offending and endangering patients.14 This study provides substantial evidence that training improves awareness as well as identification of partner abuse.
Patients, ideally, should disclose abuse in a safe environment where their motives of remaining with their abuser and assessment of their situation are professionally met. Disclosure is only the start of an intensive process for abused women and their children. It takes much effort and is often not without risk to their safety.36 Formerly abused patients can experience long-term health effects and disclosing their background can open up possibilities to start to come to terms with their past. From the literature it is known that female patients often do not reveal their past (of partner abuse) because they feel guilty, ashamed, embarrassed, or fear to be judged or that a doctor is not interested in a non-somatic background.6,22
Primary care researchers need to go beyond a superficial view of chronic complaints and disorders in female patients. Surveys on mental health problems, chronic undefined pain, and somatisation should consider partner abuse as an important variable in a patient's background and include abuse-related questions. Producers of guidelines on these topics can no longer ignore the growing knowledge of health problems that are highly related to history of abuse.21 Finally, when doctors ask female patients more frequently about abuse, they should keep in mind that denial inevitably will occur more often than before. As much as women may not feel able to disclose abuse, doctors may wrongly suspect it.
In the debate between proponents of routinely questioning every woman about partner abuse (screening) and those who favour selective questioning and case finding, our findings support the latter.18 Our study shows that training improves awareness of abuse, which leads to active questioning of women showing non-obvious signs, and results in increased identification of abused women. Disclosure may lead to more effective and meaningful consultations both for abused women and doctors.
Our training programme on intimate partner abuse provided a feasible and evidence-based method for daily practice. Educating doctors can make a difference.
Acknowledgments
We wish to thank the family doctors for participating in the study; the research assistant Margriet Straver for her field work, introducing the registration forms, and data entry; Ellen Nijenhuis, senior trainer–psychologist for training the participants; Roos Bernsen, Erasmus Medical Centre, for statistical advice; Hans Bor, Radboud University Medical Centre, for statistical advice and for executing the analysis; Jan-Marc van Dam (Chelmsford, UK) for English-language corrections.
Funding body
This project received a research grant from Theia Foundation, Zilveren Kruis Achmea Health Insurance (project number 200173)
Ethics committee
The study was undertaken with the consent of the ethical committee of the Radboud University Medical Centre: Commissie Mensgebonden Onderzoek, region Arnhem — Nijmegen (CMO number 2002/275)
Competing interests
The authors have stated that there are none
REFERENCES
- 1.Watts C, Zimmerman C. Violence against women: global scope and magnitude. Lancet. 2002;359:1232–1237. doi: 10.1016/S0140-6736(02)08221-1. [DOI] [PubMed] [Google Scholar]
- 2.Hegarty KL, Bush R. Prevalence and associations of partner abuse in women attending general practice: a cross-sectional survey. Aust N Z J Public Health. 2002;26(5):437–442. doi: 10.1111/j.1467-842x.2002.tb00344.x. [DOI] [PubMed] [Google Scholar]
- 3.Bradley F, Smith M, Long J, O'Dowd T. Reported frequency of domestic violence: cross sectional survey of women attending general practice. BMJ. 2002;324:271. doi: 10.1136/bmj.324.7332.271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Richardson J, Coid J, Petruckevitch A, et al. Identifying domestic violence: cross sectional study in primary care. BMJ. 2002;324:274. doi: 10.1136/bmj.324.7332.274. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Cohen S, De Vos E, Newberger E. Barriers to physician identification and treatment of family violence: lessons from five communities. Acad Med. 1997;72(1 Suppl):S19–25. [PubMed] [Google Scholar]
- 6.Hegarty KL, Taft AJ. Overcoming the barriers to disclosure and inquiry of partner abuse for women attending general practice. Aust N Z J Public Health. 2001;25(5):433–437. [PubMed] [Google Scholar]
- 7.Taft A, Broom DH, Legge D. General practitioner management of intimate partner abuse and the whole family: qualitative study. BMJ. 2004;328:618–620. doi: 10.1136/bmj.38014.627535.0B. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Sugg NK, Inui T. Primary care physicians' response to domestic violence. Opening Pandora's box. JAMA. 1992;267(23):3157–3160. [PubMed] [Google Scholar]
- 9.Brown JB, Lent B, Schmidt G, Sas G. Application of the Woman Abuse Screening Tool (WAST) and WAST-short in the family practice setting. J Fam Pract. 2000;49(10):896–903. [PubMed] [Google Scholar]
- 10.Taket A, Nurse J, Smith K, et al. Routinely asking women about domestic violence in health settings. BMJ. 2003;327:673–676. doi: 10.1136/bmj.327.7416.673. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Garcia-Moreno C. Dilemmas and opportunities for an appropriate health-service response to violence against women. Lancet. 2002;359:1509–1514. doi: 10.1016/S0140-6736(02)08417-9. [DOI] [PubMed] [Google Scholar]
- 12.Zachary MJ, Schechter CB, Kaplan ML, Mulvihill MN. Provider evaluation of a multifaceted system of care to improve recognition and management of pregnant women experiencing domestic violence. Womens Health Issues. 2002;12(1):5–15. doi: 10.1016/s1049-3867(01)00142-6. [DOI] [PubMed] [Google Scholar]
- 13.Ramsay J, Richardson J, Carter YH, et al. Should health professionals screen women for domestic violence? Systematic review. BMJ. 2002;325:314. doi: 10.1136/bmj.325.7359.314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Sugg NK, Thompson RS, Thompson DC, et al. Domestic violence and primary care. Attitudes, practices, and beliefs. Arch Fam Med. 1999;8(4):301–306. doi: 10.1001/archfami.8.4.301. [DOI] [PubMed] [Google Scholar]
- 15.Nelson HD, Nygren P, McInerney Y, et al. Screening women and elderly adults for family and intimate partner violence: a review of the evidence for the US Preventive Services Task Force. Ann Intern Med. 2004;140(5):387–396. doi: 10.7326/0003-4819-140-5-200403020-00015. [DOI] [PubMed] [Google Scholar]
- 16.Rhodes KV, Levinson W. Interventions for intimate partner violence against women: clinical applications. JAMA. 2003;289(5):601–605. doi: 10.1001/jama.289.5.601. [DOI] [PubMed] [Google Scholar]
- 17.Taket A, Wathen CN, Macmillan H. Should health professionals screen all women for domestic violence? PLoS Med. 2004;1(1):7–10. doi: 10.1371/journal.pmed.0010004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Hamberg K, Johansson EE, Lindgren G. ‘I was always on guard’ an exploration of woman abuse in a group of women with musculoskeletal pain. Fam Pract. 1999;16(3):238–244. doi: 10.1093/fampra/16.3.238. [DOI] [PubMed] [Google Scholar]
- 19.American Medical Association. American Medical Association diagnostic and treatment guidelines on domestic violence. Arch Fam Med. 1992;1(1):39–47. doi: 10.1001/archfami.1.1.39. [DOI] [PubMed] [Google Scholar]
- 20.Campbell J, Jones AS, Dienemann J, et al. Intimate partner violence and physical health consequences. Arch Intern Med. 2002;162(10):1157–1163. doi: 10.1001/archinte.162.10.1157. [DOI] [PubMed] [Google Scholar]
- 21.Coid J, Petruckevitch A, Feder G, et al. Relation between childhood sexual and physical abuse and risk of revictimisation in women: a cross-sectional survey. Lancet. 2001;358:450–454. doi: 10.1016/s0140-6736(01)05622-7. [DOI] [PubMed] [Google Scholar]
- 22.Dickinson LM, deGruy FV, 3rd, Dickinson WP, Candib LM. Health-related quality of life and symptom profiles of female survivors of sexual abuse. Arch Fam Med. 1999;8(1):35–43. doi: 10.1001/archfami.8.1.35. [DOI] [PubMed] [Google Scholar]
- 23.Elliott BA, Johnson MM. Domestic violence in a primary care setting. Patterns and prevalence. Arch Fam Med. 1995;4(2):113–119. doi: 10.1001/archfami.4.2.113. [DOI] [PubMed] [Google Scholar]
- 24.McCauley J, Kern DE, Kolodner K, et al. The ‘battering syndrome’: prevalence and clinical characteristics of domestic violence in primary care internal medicine practices. Ann Intern Med. 1995;123(10):737–746. doi: 10.7326/0003-4819-123-10-199511150-00001. [DOI] [PubMed] [Google Scholar]
- 25.Hathaway JE, Mucci LA, Silverman JG, et al. Health status and health care use of Massachusetts women reporting partner abuse. Am J Prev Med. 2000;19(4):302–307. doi: 10.1016/s0749-3797(00)00236-1. [DOI] [PubMed] [Google Scholar]
- 26.Plichta S. The effects of woman abuse on health care utilization and health status: a literature review. Womens Health Issues. 1992;2(3):154–163. doi: 10.1016/s1049-3867(05)80264-6. [DOI] [PubMed] [Google Scholar]
- 27.Chang JC, Decker M, Moracco KE, et al. What happens when health care providers ask about intimate partner violence? A description of consequences from the perspectives of female survivors. J Am Med Womens Assoc. 2003;58(2):76–81. [PubMed] [Google Scholar]
- 28.Fanslow J, Norton R, Robinson EM. One year follow-up of an emergency department protocol for abused women. Aust N Z J Public Health. 1999;23(4):418–420. doi: 10.1111/j.1467-842x.1999.tb01286.x. [DOI] [PubMed] [Google Scholar]
- 29.Krueger PM, Schafer S. Physician awareness of domestic violence: does continuing medical education have an impact? J Am Osteopath Assoc. 2000;100(3):145–148. [PubMed] [Google Scholar]
- 30.Saunders DG, Kindy P., Jr Predictors of physicians' responses to woman abuse: the role of gender, background, and brief training. J Gen Intern Med. 1993;8(11):606–609. doi: 10.1007/BF02599714. [DOI] [PubMed] [Google Scholar]
- 31.Campbell JC, Coben JH, McLoughlin E, et al. An evaluation of a system-change training model to improve emergency department response to battered women. Acad Emerg Med. 2001;8(2):131–138. doi: 10.1111/j.1553-2712.2001.tb01277.x. [DOI] [PubMed] [Google Scholar]
- 32.Zachary MJ, Mulvihill MN, Burton WB, Goldfrank LR. Domestic abuse in the emergency department: can a risk profile be defined? Acad Emerg Med. 2001;8(8):796–803. doi: 10.1111/j.1553-2712.2001.tb00209.x. [DOI] [PubMed] [Google Scholar]
- 33.Hegarty K, Gunn J, Chondros P, Small R. Association between depression and abuse by partners of women attending general practice: descriptive, cross sectional survey. BMJ. 2004;328:621–624. doi: 10.1136/bmj.328.7440.621. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Rose K, Saunders D. Nurses' and physicians' attitudes about women abuse: the effects of gender and professional role. Health Care Women Int. 1986;7(6):427–438. doi: 10.1080/07399338609515757. [DOI] [PubMed] [Google Scholar]
- 35.Zink T, Elder N, Jacobson J, Klostermann B. Medical management of intimate partner violence considering the stages of change: precontemplation and contemplation. Ann Fam Med. 2004;2(3):231–239. doi: 10.1370/afm.74. [DOI] [PMC free article] [PubMed] [Google Scholar]


