Abstract
Background
There has been much debate as to whether quality points allocated through the new general medical services contract are more difficult to achieve for practices in deprived and rural areas. We used multiple regression to assess the relationships between deprivation, rurality and the number of overall quality points achieved by each practice. Multiple deprivation was significantly inversely related to quality points achieved. Practices in villages and towns gained 2% more quality points than urban areas and hamlets.
Keywords: healthcare, population characteristics, primary health care, quality indicators, residence characteristics, rural health services
INTRODUCTION
In April 2004 most GP practices in the UK enrolled into a new general medical services contract with the government. Practices are remunerated under this contract broadly through two streams. The Carr-Hill formula calculates a per capita payment, weighted according to workload, while additional payments may be made to practices based on their quality of care as measured through a Quality and Outcomes Framework (QOF).1 It is important to recognise that practices will have adopted different strategies towards QOF, taking account of previous priorities and performance.
There has been debate as to whether quality points allocated through QOF are easier to achieve for certain types of practice than for others. For example, it has been argued that practices in deprived areas may find it more difficult to achieve QOF points for diabetes than surgeries in less deprived areas.2 There is evidence that patients from deprived areas are less likely to consult their GPs for preventative reasons or follow-up3 and health outcomes among these groups are likely to be poorer. Similarly, service delivery in rural areas is challenged by accessibility problems, although the relationship between accessibility and health is not simple.4 The recent release of the QOF database at practice level (http://www.ic.nhs.uk/services/qof/data/) provides an opportunity to evaluate whether the number of QOF points achieved is related to the level of deprivation and/or rurality of a practice's location.
METHOD
Detailed points summaries for 8569 general practices in England were linked by postcode and address to statistical areas. This allowed each practice to be associated with the Office of the Deputy Prime Minister's Indices of Deprivation (ID2004)5 for super output areas and the Office for National Statistics (ONS) Urban/Rural Classification of output areas.6 Output areas are the smallest geographical unit for which 2001 census results were published, typically having populations of around 300. Super output areas are official groupings of output areas for the publication of statistical data derived from government administrative sources, with populations of approximately 1500. Successful matches were achieved for 99.92% of practices. ID2004 uses census and administrative data to calculate seven domains of deprivation, of which only the overall summary has been used here. The ONS classification divides output areas into four categories of settlement size, located within either sparsely or less sparsely populated regions. We then used stepwise multiple regression to assess the relationship between the number of overall QOF points achieved by each practice, deprivation and rurality.
RESULTS
As shown by its negative coefficient in the table of regression results (Table 1), ID2004 was significantly inversely related to overall QOF points achieved. The difference between the most and least deprived practices translates into a reduction of approximately 11% in the overall QOF score. This is illustrated by the plotted line in Figure 1.
Table 1.
Regression results for percentage of total quality points achieved by practice, compared to the Office of the Deputy Prime Minister's Indices of Deprivation (ID2004) and the Office for National Statistics' urban/rural classification.
| Variables | Coefficient (95% CI) | P-value |
|---|---|---|
| ID2004 | −0.12 (−0.14 to −0.11) | <0.001 |
| Practice located in town or village | 1.98 (1.28 to 2.69) | <0.001 |
| Constant | 94.35 (93.87 to 94.83) | <0.001 |
| R2 (proportion of variation in QOF explained by the regression) | 0.05 | |
Figure 1.
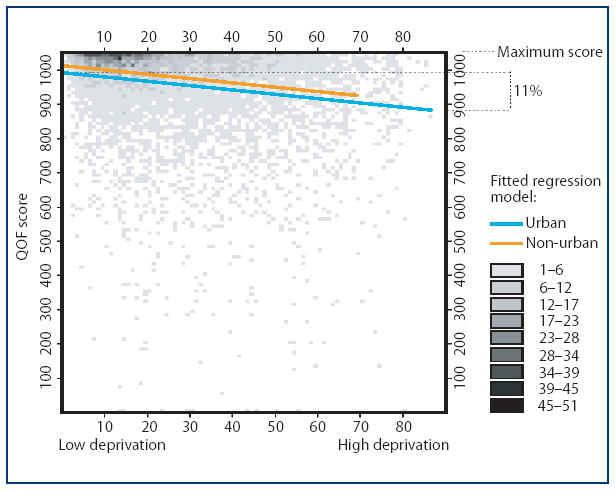
Relationship between overall Quality and Outcomes Framework score and the Office of the Deputy Prime Minister's Indices of Deprivation (ID2004) (the dotted line shows the fitted regression model for urban practices and the solid line shows the fitted regression model for village and town practices).
After allowing for deprivation, practices in villages and towns gained 1.98% more QOF points than urban areas and hamlets, as shown by the positive coefficient in Table 1 and illustrated by the solid line in Figure 1. Deprivation and rurality together only explained about 5% of the variation in QOF between practices (as indicated by the wide scatter in the figure), so most of the influences on a practice's QOF score remain unexplained by this initial analysis.
DISCUSSION
General practices in deprived areas of England are scoring fewer points under the QOF. The pattern across urban and rural areas is complex. This analysis suggests that deprivation does affect a practice's ability to score quality points. With each QOF point being worth £75 in 2004–2005,1 this translates into £8400 less income for the most deprived compared to the least deprived practices (Table 1). This calculation assumes an average practice list size and disease prevalence. This shortfall may, however, be balanced by payments through the Carr-Hill formula and adjustments for greater disease prevalence. After allowing for deprivation, the best-performing practices appear to be in villages and small towns, although this analysis is complicated by the very large number of practices located in large urban areas.
In line with recent commentaries on variation in achievement for quality points for diabetes,2 there is thus evidence of significantly fewer quality points being awarded in deprived areas. Contrary to expectations that rural practices might achieve fewer QOF points because of limited accessibility, these results suggest that practices in villages and towns achieved slightly more points than those in urban areas. The reasons for this difference require further investigation, but one possible explanation may be lower turnover in patient lists in rural areas.
This analysis represents a preliminary assessment of the QOF data set. We have not explored the effect of the individual domains of multiple deprivation in isolation, nor have we assessed the factors influencing the constituent domains of the overall quality points score. Furthermore, 85% of the practices are in urban areas and these vary widely in terms of their quality performance. This intra-urban variation remains largely unexplained.
How this fits in
The QOF will change the economics of primary care in the UK. Practices in deprived areas have scored significantly fewer quality points under the new QOF than those elsewhere, but the pattern across urban and rural areas is complex.
In understanding these patterns further it will be necessary to explore the distinctive contributions of the various domains within the ID2004 and QOF scores, and also to subdivide the major urban areas according to neighbourhood type. It will also be necessary to understand whether practice-level variation in performance is related to primary care trust or strategic health authority membership.
Acknowledgments
Urban/rural classifications and indices of deprivation are Crown Copyright. Sources www.statistics.gov.uk and www.odpm.gov.uk (accessed 28 February 2006).
Funding body
None
Ethics committee
Ethics approval was not necessary since all of the data are in the public domain and no issues regarding breach of confidentiality were identified
Competing interests
The authors have stated that there are none
REFERENCES
- 1.British Medical Association. Investing in general practice: the new general medical services contract. London: British Medical Association; 2003. [Google Scholar]
- 2.Hippisley-Cox J, O'Hanlon S, Coupland C. Association of deprivation, ethnicity, and sex with quality indicators for diabetes: population based survey of 53 000 patients in primary care. BMJ. 2004;329:1267–1269. doi: 10.1136/bmj.38279.588125.7C. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Goddard M, Smith P. Equity of access to health care services: theory and evidence from the UK. Soc Sci Med. 2001;53:1149–1162. doi: 10.1016/s0277-9536(00)00415-9. [DOI] [PubMed] [Google Scholar]
- 4.Jordan H, Roderick P, Martin D. The Index of Multiple Deprivation 2000 and accessibility effects on health. J Epidemiol Community Health. 2004;58:250–257. doi: 10.1136/jech.2003.013011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Office of the Deputy Prime Minister. The English Indices of Deprivation 2004 (revised) London: ODPM; 2004. http://www.odpm.gov.uk/stellent/groups/odpm_urbanpolicy/documents/page/odpm_urbpol_029534.pdf (accessed 28 Feb 2006) [Google Scholar]
- 6.Bibby J, Shepherd J. Developing a new classification of urban and rural areas for policy purposes — the methodology. London: Office for National Statistics; 2004. http://www.statistics.gov.uk/geography/downloads/Methodology_Report.pdf (accessed 28 Feb 2006) [Google Scholar]


