Abstract
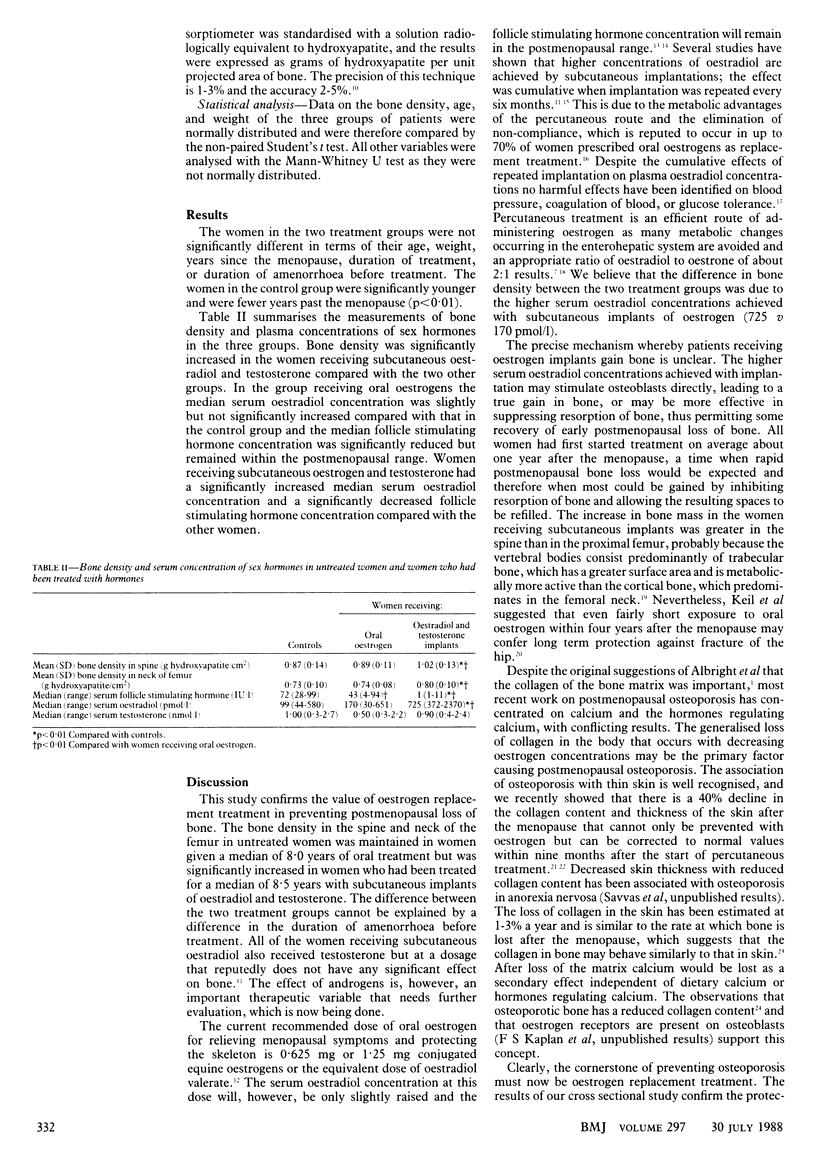
STUDY OBJECTIVE--To compare oral and implanted oestrogens for their effects in preventing postmenopausal osteoporosis. DESIGN--Non-randomised cohort study of postmenopausal women treated with oral or depot oestrogens and postmenopausal controls. SETTING--Gynaecological endocrine clinic in tertiary referral centre. PATIENTS--Oral treatment group of 37 postmenopausal women (mean age 57.5 years, median 8.75 years from last menstrual period), compared with 41 women given oestrogen implants (mean age 56.2 years, median 9.5 years from last menstrual period) and 36 controls (mean age 51.8 years, median 2.0 years from last menstrual period). Weight was not significantly different among the groups. INTERVENTIONS--Oral treatment group was given continuous treatment with cyclic oestrogen and progesterone preparations (Prempak C or Cycloprogynova) for a median of 8.0 years. Implant group was given subcutaneous implants of oestradiol 50 mg combined with testosterone 100 mg, on average six monthly for a median of 8.5 years. Controls were not treated. END POINT--Significant increase in bone density. MEASUREMENTS AND MAIN RESULTS--Bone density measured by dual beam photon absorptiometry was 1.02 (SD 0.13) g hydroxyapatite/cm2 in implant group versus 0.89 (0.11) in oral group (p less than 0.01) and 0.87 (0.14) in controls (p less than 0.01). Serum oestradiol concentration in implant group was (median) 725 pmol/l versus 170 pmol/l in oral group (p less than 0.01) and 99 pmol/l in controls (p less than 0.01). Serum follicular stimulating hormone was median 1 IU/l (range 1-11) in implant group (equivalent to premenopausal values) versus 43 (4-94) IU/l in oral group (p less than 0.01) and 72 (28-99) IU/l in controls (p less than 0.01). CONCLUSIONS--Subcutaneous oestrogen is more effective than oral oestrogen in preventing osteoporosis, probably owing to the more physiological (premenopausal) serum oestradiol concentrations achieved. It also avoids problems of compliance that occur with oral treatment.
Full text
PDF
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Barlow D. H., Abdalla H. I., Roberts A. D., Al Azzawi F., Leggate I., Hart D. M. Long-term hormone implant therapy--hormonal and clinical effects. Obstet Gynecol. 1986 Mar;67(3):321–325. [PubMed] [Google Scholar]
- Brincat M., Moniz C. J., Studd J. W., Darby A., Magos A., Emburey G., Versi E. Long-term effects of the menopause and sex hormones on skin thickness. Br J Obstet Gynaecol. 1985 Mar;92(3):256–259. doi: 10.1111/j.1471-0528.1985.tb01091.x. [DOI] [PubMed] [Google Scholar]
- Brincat M., Versi E., Moniz C. F., Magos A., de Trafford J., Studd J. W. Skin collagen changes in postmenopausal women receiving different regimens of estrogen therapy. Obstet Gynecol. 1987 Jul;70(1):123–127. [PubMed] [Google Scholar]
- Cardozo L., Gibb D. M., Studd J. W., Tuck S. M., Thom M. H., Cooper D. J. The use of hormone implants for climacteric symptoms. Am J Obstet Gynecol. 1984 Feb 1;148(3):336–337. doi: 10.1016/s0002-9378(84)80080-0. [DOI] [PubMed] [Google Scholar]
- Chetkowski R. J., Meldrum D. R., Steingold K. A., Randle D., Lu J. K., Eggena P., Hershman J. M., Alkjaersig N. K., Fletcher A. P., Judd H. L. Biologic effects of transdermal estradiol. N Engl J Med. 1986 Jun 19;314(25):1615–1620. doi: 10.1056/NEJM198606193142505. [DOI] [PubMed] [Google Scholar]
- Christiansen C., Christensen M. S., Transbøl I. Bone mass in postmenopausal women after withdrawal of oestrogen/gestagen replacement therapy. Lancet. 1981 Feb 28;1(8218):459–461. doi: 10.1016/s0140-6736(81)91848-1. [DOI] [PubMed] [Google Scholar]
- Kiel D. P., Felson D. T., Anderson J. J., Wilson P. W., Moskowitz M. A. Hip fracture and the use of estrogens in postmenopausal women. The Framingham Study. N Engl J Med. 1987 Nov 5;317(19):1169–1174. doi: 10.1056/NEJM198711053171901. [DOI] [PubMed] [Google Scholar]
- Lindsay R., Hart D. M., Aitken J. M., MacDonald E. B., Anderson J. B., Clarke A. C. Long-term prevention of postmenopausal osteoporosis by oestrogen. Evidence for an increased bone mass after delayed onset of oestrogen treatment. Lancet. 1976 May 15;1(7968):1038–1041. doi: 10.1016/s0140-6736(76)92217-0. [DOI] [PubMed] [Google Scholar]
- Lindsay R., Hart D. M., Clark D. M. The minimum effective dose of estrogen for prevention of postmenopausal bone loss. Obstet Gynecol. 1984 Jun;63(6):759–763. [PubMed] [Google Scholar]
- Murby B., Fogelman I. Bone mineral measurements in clinical practice. Br J Hosp Med. 1987 May;37(5):453–458. [PubMed] [Google Scholar]
- Nachtigall L. E., Nachtigall R. H., Nachtigall R. D., Beckman E. M. Estrogen replacement therapy I: a 10-year prospective study in the relationship to osteoporosis. Obstet Gynecol. 1979 Mar;53(3):277–281. [PubMed] [Google Scholar]
- Powers M. S., Schenkel L., Darley P. E., Good W. R., Balestra J. C., Place V. A. Pharmacokinetics and pharmacodynamics of transdermal dosage forms of 17 beta-estradiol: comparison with conventional oral estrogens used for hormone replacement. Am J Obstet Gynecol. 1985 Aug 15;152(8):1099–1106. doi: 10.1016/0002-9378(85)90569-1. [DOI] [PubMed] [Google Scholar]
- Ravnikar V. A. Compliance with hormone therapy. Am J Obstet Gynecol. 1987 May;156(5):1332–1334. doi: 10.1016/0002-9378(87)90173-6. [DOI] [PubMed] [Google Scholar]
- Savvas M., Brincat M., Studd J. W. Postmenopausal osteoporosis. Br J Hosp Med. 1987 Jul;38(1):16-8, 22, 24. [PubMed] [Google Scholar]
- Studd J., Magos A. Hormone pellet implantation for the menopause and premenstrual syndrome. Obstet Gynecol Clin North Am. 1987 Mar;14(1):229–249. [PubMed] [Google Scholar]
- Thom M. H., Collins W. P., Studd J. W. Hormonal profiles in postmenopausal women after therapy with subcutaneous implants. Br J Obstet Gynaecol. 1981 Apr;88(4):426–433. doi: 10.1111/j.1471-0528.1981.tb01008.x. [DOI] [PubMed] [Google Scholar]


