Abstract
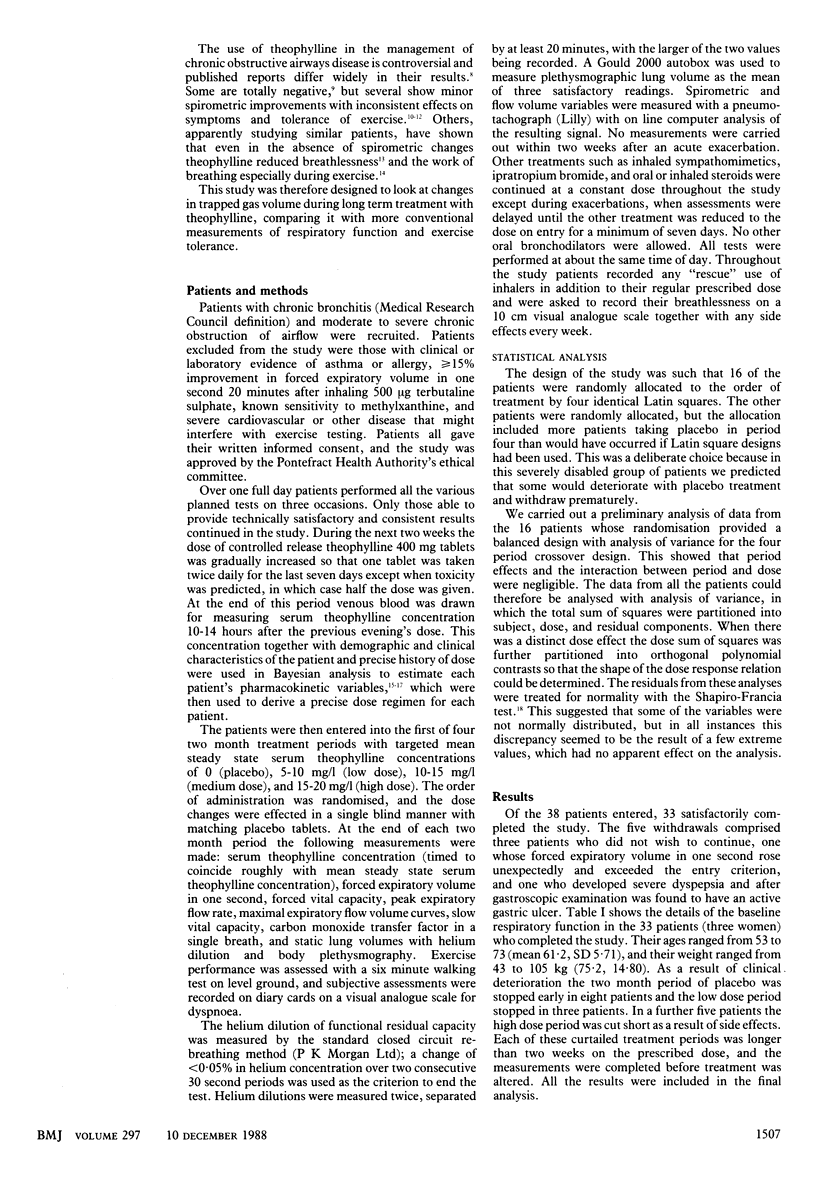
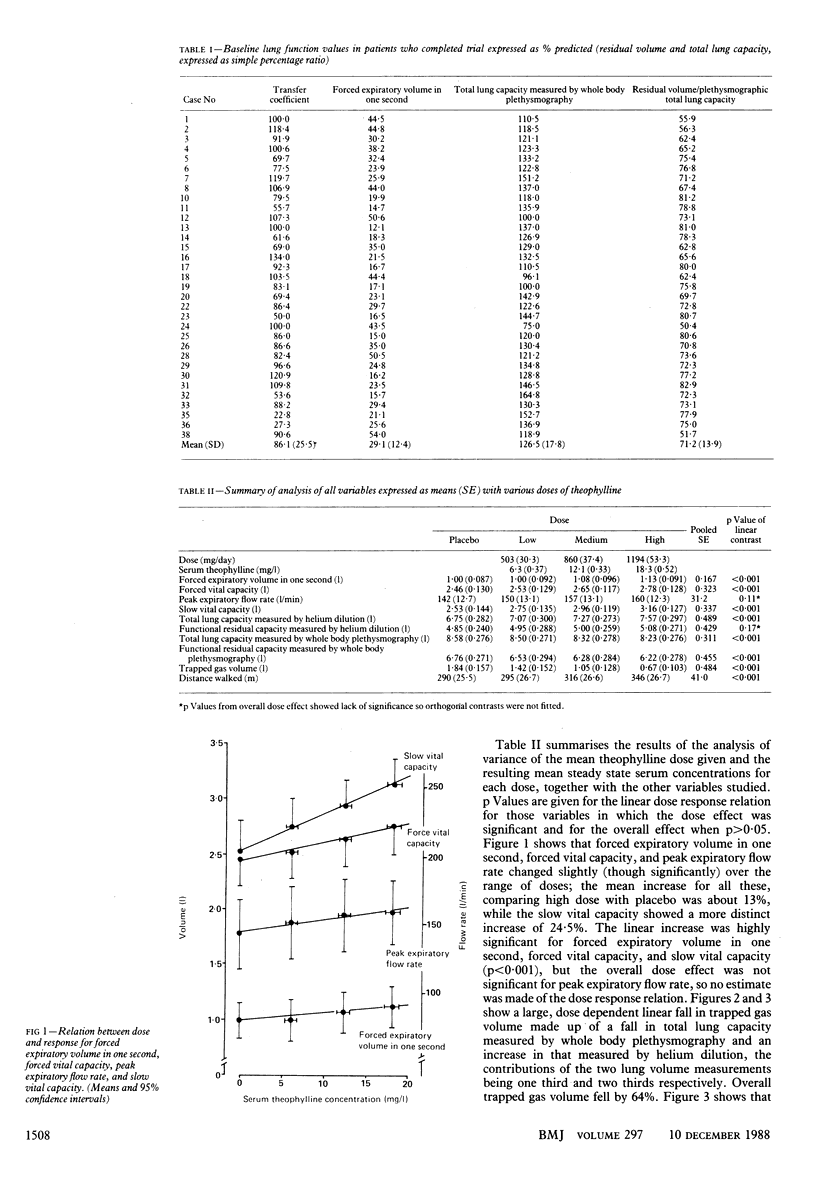
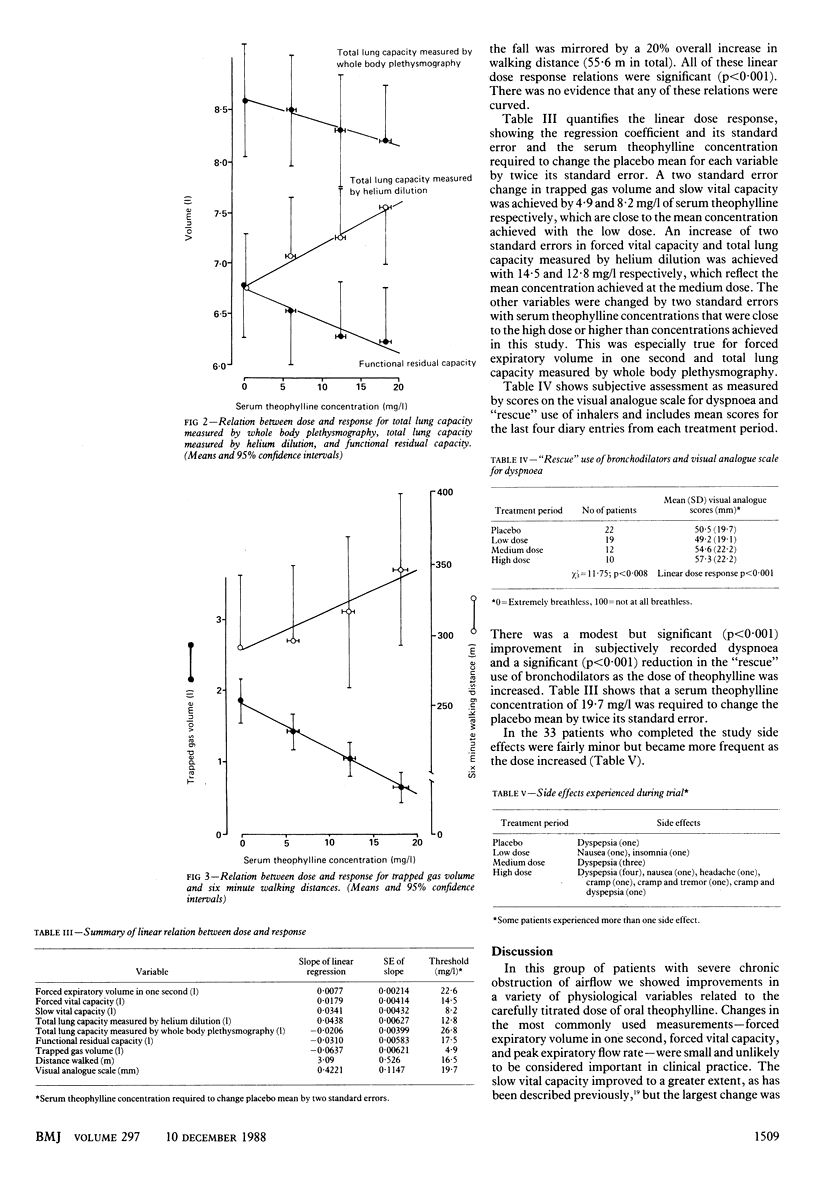
OBJECTIVE--To evaluate measurement of the trapped gas volume as a measure of respiratory function in patients with chronic obstructive airways disease and their response to treatment with theophylline. DESIGN--Patients able to produce consistent results on testing of respiratory function spent two weeks having dosage of theophylline adjusted to give individual pharmacokinetic data. This was followed by random assignment to four consecutive two month treatment periods--placebo and low, medium, and high dose, as assessed by serum concentrations of theophylline. Respiratory function and exercise performance was assessed at the end of each two month period. SETTING--Chest unit in district hospital. PATIENTS--Thirty eight patients with chronic bronchitis and moderate to severe chronic obstruction to airflow were recruited; 33 aged 53-73 years completed the study. INTERVENTIONS--Dosage of oral theophylline increased during two week optimisation period to 800 mg daily unless toxicity was predicted, when 400 mg was given. Targets for the steady state serum theophylline concentrations were 5-10 mg/l in the low dose period, 10-15 mg/l in the medium dose, and 15-20 mg/l in the high dose period. ENDPOINTS--Respiratory function as measured by forced expiratory volume in one second, forced vital capacity, peak expiratory flow rate, slow vital capacity, and static lung volumes using helium dilution and body plethysmography from which trapped gas volume was derived. Exercise performance assessed by six minute walking test and diary cards using visual analogue scale. MEASUREMENTS AND MAIN RESULTS--The forced expiratory volume in one second, forced vital capacity, and peak expiratory flow rate changed only slightly (about 13%) over the range of doses. There was a linear dose dependent fall of trapped gas volume from 1.84 l (SE 0.157) to 1.42 l (0.152), 1.05 l (0.128), and 0.67 l (0.102) during the placebo and low, medium, and high dose treatment periods. Mean walking distance increased by up to 55.6 m (20%). There was a modest improvement in dyspnoea as the dose of theophylline was increased. Side effects were mostly minor but they became more frequent as the dose was increased. CONCLUSION--The fall in trapped gas volume may reflect an improvement in peripheral ventilation (associated with treatment with theophylline) which is less apparent in the more common tests of lung function used in patients with chronic obstructive airways disease.
Full text
PDF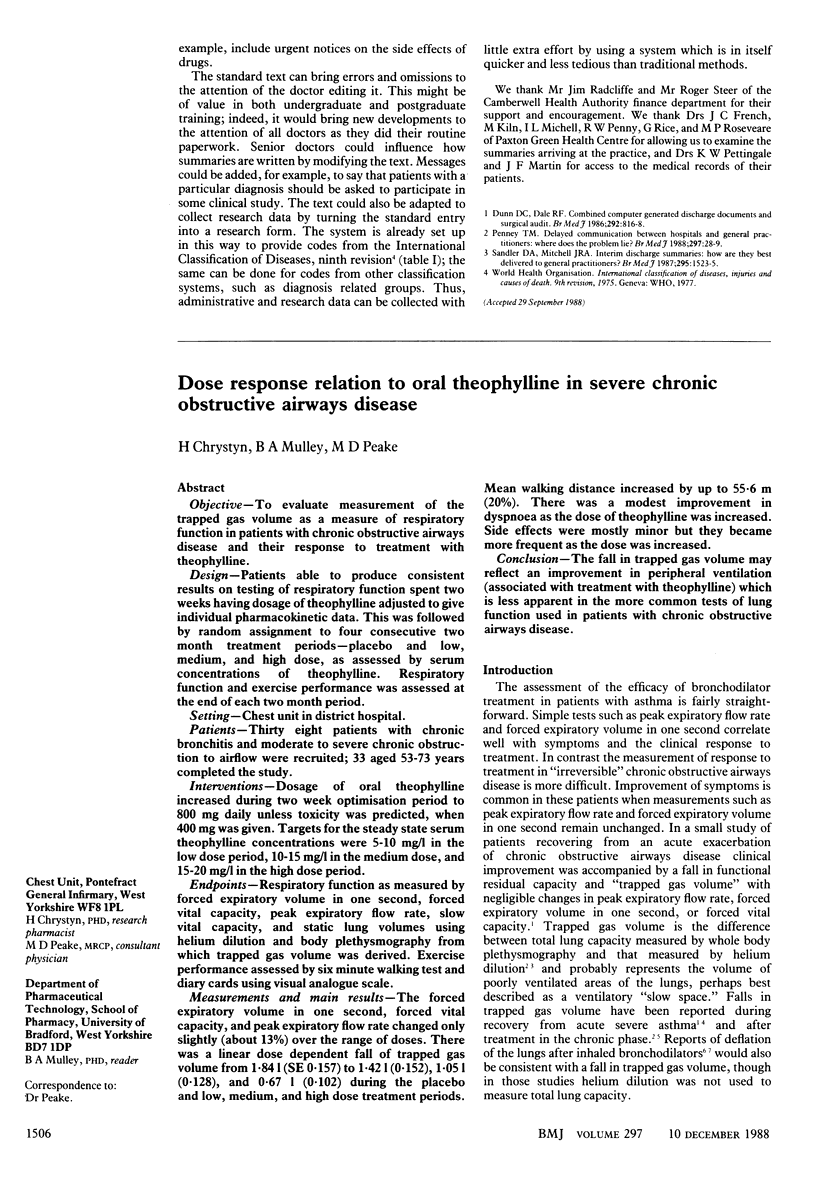

Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Adams L., Chronos N., Lane R., Guz A. The measurement of breathlessness induced in normal subjects: validity of two scaling techniques. Clin Sci (Lond) 1985 Jul;69(1):7–16. doi: 10.1042/cs0690007. [DOI] [PubMed] [Google Scholar]
- Alexander M. R., Dull W. L., Kasik J. E. Treatment of chronic obstructive pulmonary disease with orally administered theophylline. A double-blind, controlled study. JAMA. 1980 Nov 21;244(20):2286–2290. [PubMed] [Google Scholar]
- Aubier M., De Troyer A., Sampson M., Macklem P. T., Roussos C. Aminophylline improves diaphragmatic contractility. N Engl J Med. 1981 Jul 30;305(5):249–252. doi: 10.1056/NEJM198107303050503. [DOI] [PubMed] [Google Scholar]
- BEDELL G. N., MARSHALL R., DUBOIS A. B., COMROE J. H. Plethysmographic determination of the volume of gas trapped in the lungs. J Clin Invest. 1956 Jun;35(6):664–670. doi: 10.1172/JCI103323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bellamy D., Hutchison D. C. The effects of salbutamol aerosol on lung function in patients with pulmonary emphysema. Br J Dis Chest. 1981 Apr;75(2):190–196. doi: 10.1016/0007-0971(81)90052-8. [DOI] [PubMed] [Google Scholar]
- Belman M. J., Sieck G. C., Mazar A. Aminophylline and its influence on ventilatory endurance in humans. Am Rev Respir Dis. 1985 Feb;131(2):226–229. doi: 10.1164/arrd.1985.131.2.226. [DOI] [PubMed] [Google Scholar]
- Chrystyn H., Mulley B. A., Peake M. D. The accuracy of a pharmacokinetic theophylline predictor using once daily dosing. Br J Clin Pharmacol. 1987 Sep;24(3):301–307. doi: 10.1111/j.1365-2125.1987.tb03173.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cochrane G. M. Slow release theophyllines and chronic bronchitis. Br Med J (Clin Res Ed) 1984 Dec 15;289(6459):1643–1644. doi: 10.1136/bmj.289.6459.1643. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Douglas N. J., Davidson I., Sudlow M. F., Flenley D. C. Bronchodilatation and the site of airway resistance in severe chronic bronchitis. Thorax. 1979 Feb;34(1):51–56. doi: 10.1136/thx.34.1.51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eaton M. L., Green B. A., Church T. R., McGowan T., Niewoehner D. E. Efficacy of theophylline in "irreversible" airflow obstruction. Ann Intern Med. 1980 Jun;92(6):758–761. doi: 10.7326/0003-4819-92-6-758. [DOI] [PubMed] [Google Scholar]
- Eaton M. L., MacDonald F. M., Church T. R., Niewoehner D. E. Effects of theophylline on breathlessness and exercise tolerance in patients with chronic airflow obstruction. Chest. 1982 Nov;82(5):538–542. doi: 10.1378/chest.82.5.538. [DOI] [PubMed] [Google Scholar]
- Evans W. V. Plasma theophylline concentrations, six minute walking distances, and breathlessness in patients with chronic airflow obstruction. Br Med J (Clin Res Ed) 1984 Dec 15;289(6459):1649–1651. doi: 10.1136/bmj.289.6459.1649. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jenne J. W., Siever J. R., Druz W. S., Solano J. V., Cohen S. M., Sharp J. T. The effect of maintenance theophylline therapy on lung work in severe chronic obstructive pulmonary disease while standing and walking. Am Rev Respir Dis. 1984 Oct;130(4):600–605. doi: 10.1164/arrd.1984.130.4.600. [DOI] [PubMed] [Google Scholar]
- Mahler D. A., Matthay R. A., Snyder P. E., Wells C. K., Loke J. Sustained-release theophylline reduces dyspnea in nonreversible obstructive airway disease. Am Rev Respir Dis. 1985 Jan;131(1):22–25. doi: 10.1164/arrd.1985.131.1.22. [DOI] [PubMed] [Google Scholar]
- Moxham J., Miller J., Wiles C. M., Morris A. J., Green M. Effect of aminophylline on the human diaphragm. Thorax. 1985 Apr;40(4):288–292. doi: 10.1136/thx.40.4.288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Murciano D., Aubier M., Lecocguic Y., Pariente R. Effects of theophylline on diaphragmatic strength and fatigue in patients with chronic obstructive pulmonary disease. N Engl J Med. 1984 Aug 9;311(6):349–353. doi: 10.1056/NEJM198408093110601. [DOI] [PubMed] [Google Scholar]
- Ramsdell J. W., Tisi G. M. Determination of bronchodilation in the clinical pulmonary function laboratory. Role of changes in static lung volumes. Chest. 1979 Dec;76(6):622–628. doi: 10.1378/chest.76.6.622. [DOI] [PubMed] [Google Scholar]
- Rodenstein D. O., Stănescu D. C. Reassessment of lung volume measurement by helium dilution and by body plethysmography in chronic air-flow obstruction. Am Rev Respir Dis. 1982 Dec;126(6):1040–1044. doi: 10.1164/arrd.1982.126.6.1040. [DOI] [PubMed] [Google Scholar]
- Sheiner L. B., Beal S. L. Bayesian individualization of pharmacokinetics: simple implementation and comparison with non-Bayesian methods. J Pharm Sci. 1982 Dec;71(12):1344–1348. doi: 10.1002/jps.2600711209. [DOI] [PubMed] [Google Scholar]
- Stănescu D. C., Rodenstein D., Cauberghs M., Van de Woestijne K. P. Failure of body plethysmography in bronchial asthma. J Appl Physiol Respir Environ Exerc Physiol. 1982 Apr;52(4):939–948. doi: 10.1152/jappl.1982.52.4.939. [DOI] [PubMed] [Google Scholar]
- Woolcock A. J., Rebuck A. S., Cade J. F., Read J. Lung volume changes in asthma measured concurrently by two methods. Am Rev Respir Dis. 1971 Nov;104(5):703–709. doi: 10.1164/arrd.1971.104.5.703. [DOI] [PubMed] [Google Scholar]


