Abstract
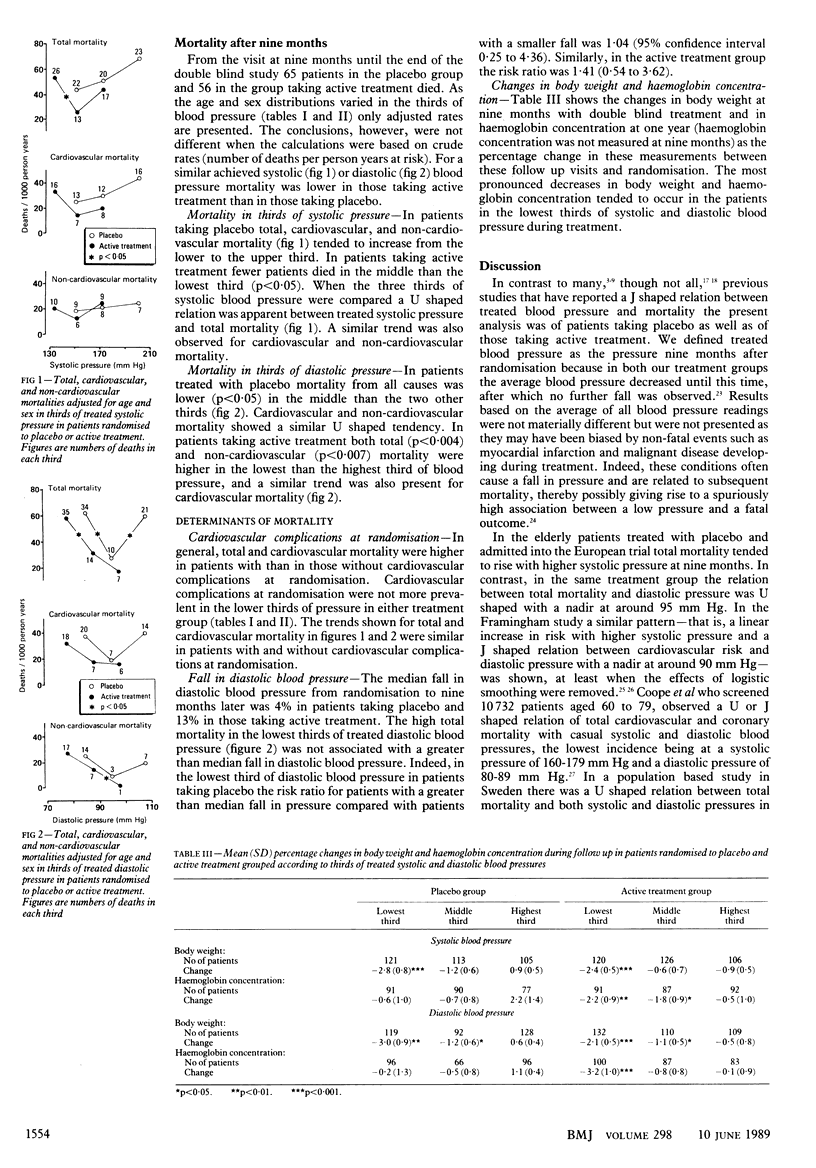
OBJECTIVE--To investigate the relation between mortality and treated systolic and diastolic blood pressures. DESIGN--Randomised double blind placebo controlled trial. Mortality in the two treatment groups was examined in thirds of treated systolic and diastolic blood pressures. PATIENTS--339 And 352 patients allocated to placebo and active treatment, respectively. The groups were similar at randomisation in sex ratio (70% women), mean age (71.5 years), blood pressure (182/101 mm Hg), and proportion of patients with cardiovascular complications (35%). MEASUREMENTS AND MAIN RESULTS--In the placebo group total mortality rose with increasing systolic pressure whereas it had a U shaped relation with diastolic pressure, the total lowest mortality being in patients in the middle third of the distribution of diastolic pressure. In the group given active treatment total mortality showed a U shaped relation with systolic pressure and an inverse association with treated diastolic pressure. In both groups cardiovascular and non-cardiovascular mortality followed the same trends as total mortality. The increased mortality in the lowest thirds of pressure was not associated with an increased proportion of patients with cardiovascular complications at randomisation or with a fall in diastolic pressure exceeding the median fall in pressure in each group. In contrast, patients in the lowest thirds of pressure showed greater decreases in body weight and haemoglobin concentration than those in the middle and upper thirds of pressure. CONCLUSIONS--In patients taking active treatment total mortality was increased in the lowest thirds of treated systolic and diastolic blood pressures. This increased mortality is not necessarily explained by an exaggerated reduction in pressure induced by drugs as for diastolic pressure a U shaped relation also existed during treatment with placebo. In addition, patients in the lowest thirds of systolic and diastolic pressures were characterised by decreases in body weight and haemoglobin concentration, and the patients in the lowest thirds of diastolic pressure taking active treatment also by an increased non-cardiovascular mortality, suggesting some deterioration of general health.
Full text
PDF



Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Amery A., Birkenhäger W., Brixko P., Bulpitt C., Clement D., Deruyttere M., De Schaepdryver A., Dollery C., Fagard R., Forette F. Mortality and morbidity results from the European Working Party on High Blood Pressure in the Elderly trial. Lancet. 1985 Jun 15;1(8442):1349–1354. doi: 10.1016/s0140-6736(85)91783-0. [DOI] [PubMed] [Google Scholar]
- Amery A., Birkenhäger W., Brixko R., Bulpitt C., Clement D., Deruyttere M., De Schaepdryver A., Dollery C., Fagard R., Forette F. Efficacy of antihypertensive drug treatment according to age, sex, blood pressure, and previous cardiovascular disease in patients over the age of 60. Lancet. 1986 Sep 13;2(8507):589–592. doi: 10.1016/s0140-6736(86)92424-4. [DOI] [PubMed] [Google Scholar]
- Anderson T. W. Re-examination of some of the Framingham blood-pressure data. Lancet. 1978 Nov 25;2(8100):1139–1141. doi: 10.1016/s0140-6736(78)92288-2. [DOI] [PubMed] [Google Scholar]
- Beevers D. G. Overtreating hypertension. BMJ. 1988 Nov 12;297(6658):1212–1213. doi: 10.1136/bmj.297.6658.1212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bulpitt C. J., Beevers D. G., Butler A., Coles E. C., Fletcher A. E., Hunt D., Munro-Faure A. D., Newson R., O'Riordan P. W., Petrie J. C. Treated blood pressure, rather than pretreatment, predicts survival in hypertensive patients. A report from the DHSS Hypertension Care Computing Project (DHCCP). J Hypertens. 1988 Aug;6(8):627–632. doi: 10.1097/00004872-198808000-00005. [DOI] [PubMed] [Google Scholar]
- Coope J., Warrender T. S. Lowering blood pressure. Lancet. 1987 Jun 13;1(8546):1380–1380. doi: 10.1016/s0140-6736(87)90683-0. [DOI] [PubMed] [Google Scholar]
- Coope J., Warrender T. S., McPherson K. The prognostic significance of blood pressure in the elderly. J Hum Hypertens. 1988 Aug;2(2):79–88. [PubMed] [Google Scholar]
- Coope J., Warrender T. S. Randomised trial of treatment of hypertension in elderly patients in primary care. Br Med J (Clin Res Ed) 1986 Nov 1;293(6555):1145–1151. doi: 10.1136/bmj.293.6555.1145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cruickshank J. M. Coronary flow reserve and the J curve relation between diastolic blood pressure and myocardial infarction. BMJ. 1988 Nov 12;297(6658):1227–1230. doi: 10.1136/bmj.297.6658.1227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cruickshank J. M., Pennert K., Sörman A. E., Thorp J. M., Zacharias F. M., Zacharias F. J. Low mortality from all causes, including myocardial infarction, in well-controlled hypertensives treated with a beta-blocker plus other antihypertensives. J Hypertens. 1987 Aug;5(4):489–498. [PubMed] [Google Scholar]
- Cruickshank J. M., Thorp J. M., Zacharias F. J. Benefits and potential harm of lowering high blood pressure. Lancet. 1987 Mar 14;1(8533):581–584. doi: 10.1016/s0140-6736(87)90231-5. [DOI] [PubMed] [Google Scholar]
- Fletcher A. E., Beevers D. G., Bulpitt C. J., Butler A., Coles E. C., Hunt D., Munro-Faure A. D., Newson R., O'Riordan P. W., Petrie J. C. The relationship between a low treated blood pressure and IHD mortality: a report from the DHSS Hypertension Care Computing Project (DHCCP). J Hum Hypertens. 1988 Jun;2(1):11–15. [PubMed] [Google Scholar]
- Green K. G. The role of hypertension and downward changes of blood pressure in the genesis of coronary atherosclerosis and acute myocardial ischemic attacks. Am Heart J. 1982 Apr;103(4 Pt 1):579–582. doi: 10.1016/0002-8703(82)90353-2. [DOI] [PubMed] [Google Scholar]
- Kannel W. B. Role of blood pressure in cardiovascular disease: the Framingham Study. Angiology. 1975 Jan;26(1 Pt 1):1–14. doi: 10.1177/000331977502600101. [DOI] [PubMed] [Google Scholar]
- Lindholm L., Lanke J., Bengtsson B., Ejlertsson G., Thulin T., Scherstén B. Both high and low blood pressures risk indicators of death in middle-aged males. Isotonic regression of blood pressure on age applied to data from a 13-year prospective study. Acta Med Scand. 1985;218(5):473–480. doi: 10.1111/j.0954-6820.1985.tb08876.x. [DOI] [PubMed] [Google Scholar]
- Lindholm L., Lanke J., Bengtsson B. U-shaped association between mortality and blood pressure in a thirteen-year prospective study. Fam Pract. 1986 Mar;3(1):3–8. doi: 10.1093/fampra/3.1.3. [DOI] [PubMed] [Google Scholar]
- Samuelsson O., Wilhelmsen L., Andersson O. K., Pennert K., Berglund G. Cardiovascular morbidity in relation to change in blood pressure and serum cholesterol levels in treated hypertension. Results from the primary prevention trial in Göteborg, Sweden. JAMA. 1987 Oct 2;258(13):1768–1776. [PubMed] [Google Scholar]
- Stewart I. M. Relation of reduction in pressure to first myocardial infarction in patients receiving treatment for severe hypertension. Lancet. 1979 Apr 21;1(8121):861–865. doi: 10.1016/s0140-6736(79)91274-1. [DOI] [PubMed] [Google Scholar]
- Strandgaard S., Haunsø S. Why does antihypertensive treatment prevent stroke but not myocardial infarction? Lancet. 1987 Sep 19;2(8560):658–661. doi: 10.1016/s0140-6736(87)92444-5. [DOI] [PubMed] [Google Scholar]
- Waller P. C., Isles C. G., Lever A. F., Murray G. D., McInnes G. T. Does therapeutic reduction of diastolic blood pressure cause death from coronary heart disease? J Hum Hypertens. 1988 Jun;2(1):7–10. [PubMed] [Google Scholar]


