Abstract
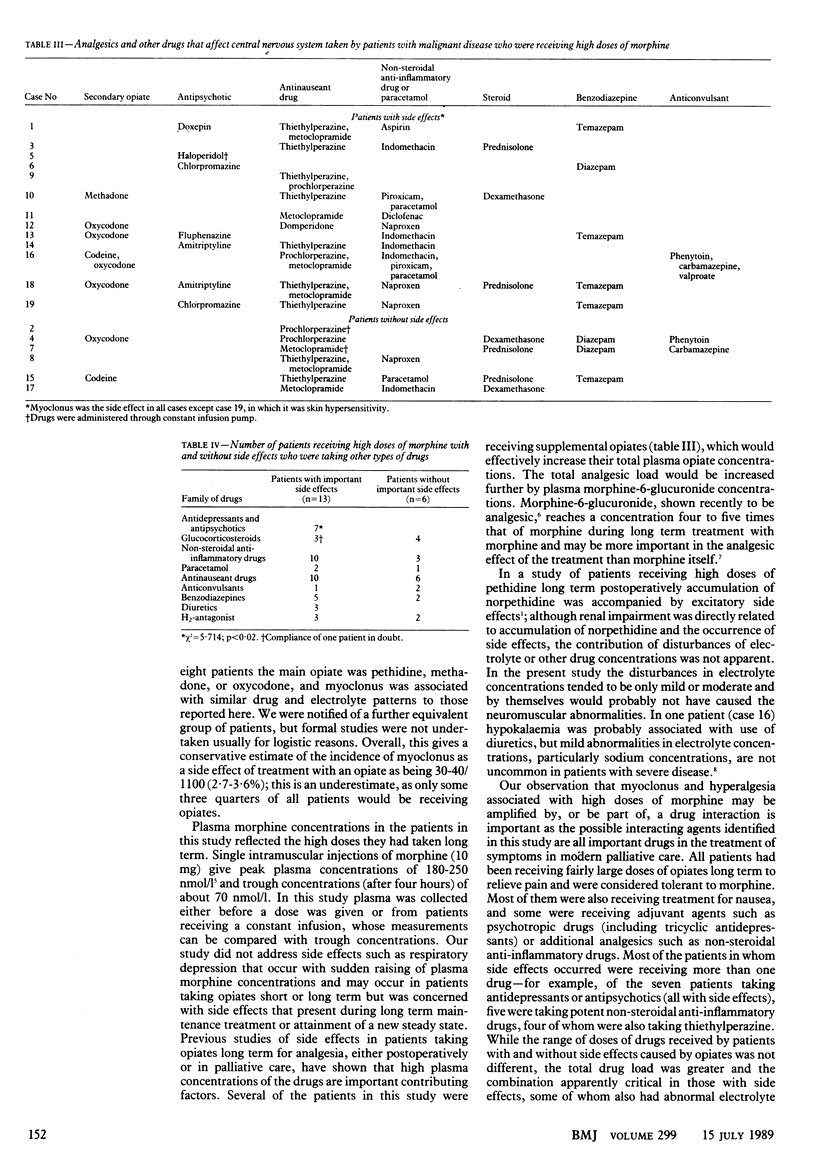
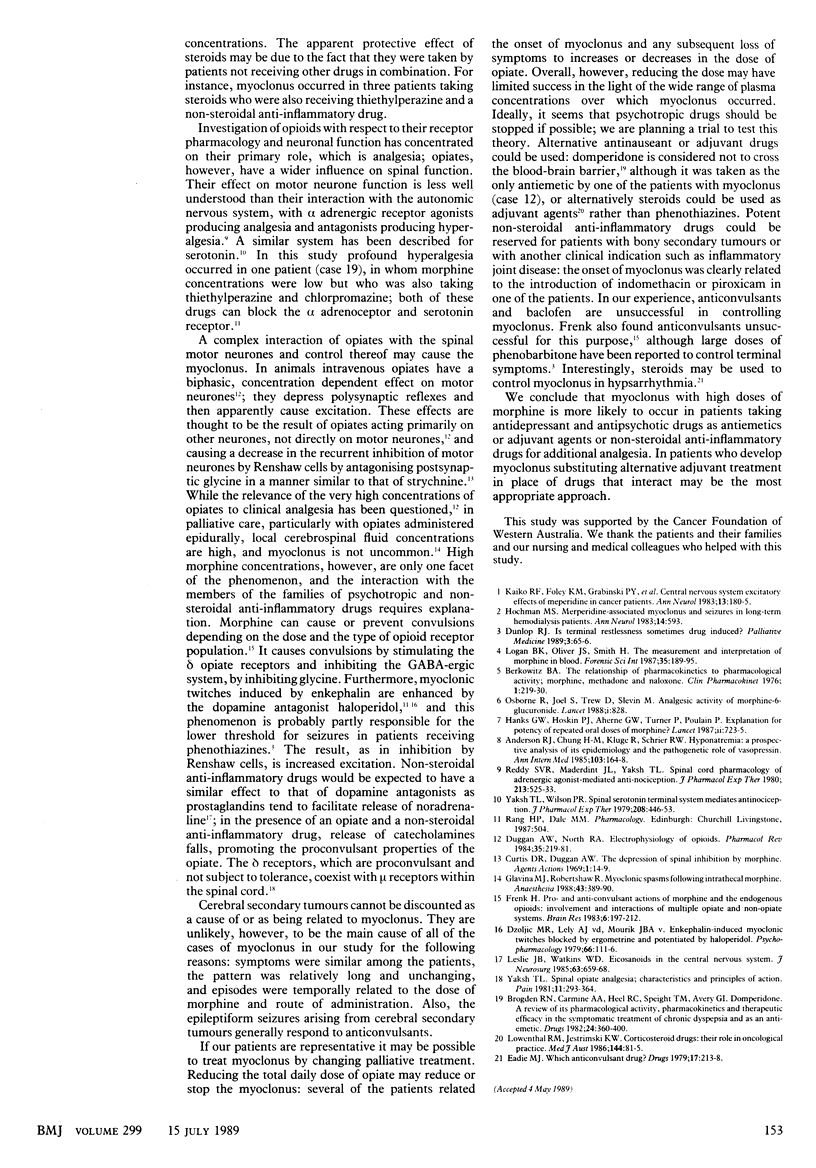
OBJECTIVE--To estimate the prevalence of important side effects in patients with malignant disease who were receiving high doses of morphine as part of their palliative treatment. DESIGN--Data on patients were collected over 12 months. SETTING--Two palliative care units in Western Australia. PATIENTS--19 Patients with malignant disease who were receiving morphine either subcutaneously or orally as the main analgesic. 10 Patients receiving a total daily dose of morphine of at least 500 mg orally or 250 mg parenterally were enrolled in the study. The other 9 patients were enrolled after an important problem thought to be related to the morphine had been identified. All of the patients were taking drugs to supplement the treatment. INTERVENTIONS--The dose of morphine or route of administration, or both, was changed in three patients. MAIN OUTCOME MEASURE--Determination of the prevalence of side effects in the patients. Assessment of the relation of any side effects with the supplemental drugs taken by the patients. MAIN RESULTS--Plasma morphine and electrolyte concentrations were measured and a full history taken for each patient. Thirteen of the 19 patients had an important side effect; 12 of them had myoclonus and one had hyperalgesia of the skin. Plasma morphine concentrations were similar in patients with and without myoclonus, ranging from 158 to 3465 nmol/l and 39 to 2821 nmol/l respectively. Eight of the patients with side effects were taking an antipsychotic drug concurrently compared with none of those without side effects. A greater proportion of patients with side effects were taking the antinauseant drug thiethylperazine (6/13 v 2/6) and at least one non-steroidal anti-inflammatory drug (10/13 v 2/6), whereas a smaller proportion were taking a glucocorticosteroid (3/13 v 4/6). The estimated prevalence of important side effects in the total population of patients receiving palliative treatment in the two units was 2.7-3.6%. CONCLUSIONS--Myoclonus as a side effect of treatment with morphine is more likely to occur in patients taking antidepressant or antipsychotic drugs as antiemetics or as adjuvant agents or non-steroidal anti-inflammatory drugs for additional analgesia. If a patient develops myoclonus the best approach may be to change the supplemental treatment.
Full text
PDF

Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Anderson R. J., Chung H. M., Kluge R., Schrier R. W. Hyponatremia: a prospective analysis of its epidemiology and the pathogenetic role of vasopressin. Ann Intern Med. 1985 Feb;102(2):164–168. doi: 10.7326/0003-4819-102-2-164. [DOI] [PubMed] [Google Scholar]
- Berkowitz B. A. The relationship of pharmacokinetics to pharmacological activity: morphine, methadone and naloxone. Clin Pharmacokinet. 1976;1(3):219–230. doi: 10.2165/00003088-197601030-00004. [DOI] [PubMed] [Google Scholar]
- Brogden R. N., Carmine A. A., Heel R. C., Speight T. M., Avery G. S. Domperidone. A review of its pharmacological activity, pharmacokinetics and therapeutic efficacy in the symptomatic treatment of chronic dyspepsia and as an antiemetic. Drugs. 1982 Nov;24(5):360–400. doi: 10.2165/00003495-198224050-00002. [DOI] [PubMed] [Google Scholar]
- Curtis D. R., Duggan A. W. The depression of spinal inhibition by morphine. Agents Actions. 1969 Jul;1(1):14–19. doi: 10.1007/BF01990015. [DOI] [PubMed] [Google Scholar]
- Dzoljic M. R., van der Lely A. J., von Mourik J. B. Enkephalin-induced myoclonic twitches blocked by ergometrine and potentiated by haloperidol. Psychopharmacology (Berl) 1979 Nov;66(2):111–116. doi: 10.1007/BF00427616. [DOI] [PubMed] [Google Scholar]
- Eadie M. J. Which anticonvulsant drug? Drugs. 1979 Mar;17(3):213–218. doi: 10.2165/00003495-197917030-00006. [DOI] [PubMed] [Google Scholar]
- Frenk H. Pro- and anticonvulsant actions of morphine and the endogenous opioids: involvement and interactions of multiple opiate and non-opiate systems. Brain Res. 1983 Oct;287(2):197–210. doi: 10.1016/0165-0173(83)90039-5. [DOI] [PubMed] [Google Scholar]
- Glavina M. J., Robertshaw R. Myoclonic spasms following intrathecal morphine. Anaesthesia. 1988 May;43(5):389–390. doi: 10.1111/j.1365-2044.1988.tb09020.x. [DOI] [PubMed] [Google Scholar]
- Hanks G. W., Hoskin P. J., Aherne G. W., Turner P., Poulain P. Explanation for potency of repeated oral doses of morphine? Lancet. 1987 Sep 26;2(8561):723–725. doi: 10.1016/s0140-6736(87)91083-x. [DOI] [PubMed] [Google Scholar]
- Hochman M. S. Meperidine-associated myoclonus and seizures in long-term hemodialysis patients. Ann Neurol. 1983 Nov;14(5):593–593. doi: 10.1002/ana.410140520. [DOI] [PubMed] [Google Scholar]
- Kaiko R. F., Foley K. M., Grabinski P. Y., Heidrich G., Rogers A. G., Inturrisi C. E., Reidenberg M. M. Central nervous system excitatory effects of meperidine in cancer patients. Ann Neurol. 1983 Feb;13(2):180–185. doi: 10.1002/ana.410130213. [DOI] [PubMed] [Google Scholar]
- Leslie J. B., Watkins W. D. Eicosanoids in the central nervous system. J Neurosurg. 1985 Nov;63(5):659–668. doi: 10.3171/jns.1985.63.5.0659. [DOI] [PubMed] [Google Scholar]
- Logan B. K., Oliver J. S., Smith H. The measurement and interpretation of morphine in blood. Forensic Sci Int. 1987 Oct-Nov;35(2-3):189–195. doi: 10.1016/0379-0738(87)90055-7. [DOI] [PubMed] [Google Scholar]
- Lowenthal R. M., Jestrimski K. W. Corticosteroid drugs: their role in oncological practice. Med J Aust. 1986 Jan 20;144(2):81–85. [PubMed] [Google Scholar]
- Osborne R., Joel S., Trew D., Slevin M. Analgesic activity of morphine-6-glucuronide. Lancet. 1988 Apr 9;1(8589):828–828. doi: 10.1016/s0140-6736(88)91691-1. [DOI] [PubMed] [Google Scholar]
- Reddy S. V., Maderdrut J. L., Yaksh T. L. Spinal cord pharmacology of adrenergic agonist-mediated antinociception. J Pharmacol Exp Ther. 1980 Jun;213(3):525–533. [PubMed] [Google Scholar]
- Yaksh T. L. Spinal opiate analgesia: characteristics and principles of action. Pain. 1981 Dec;11(3):293–346. doi: 10.1016/0304-3959(81)90633-3. [DOI] [PubMed] [Google Scholar]
- Yaksh T. L., Wilson P. R. Spinal serotonin terminal system mediates antinociception. J Pharmacol Exp Ther. 1979 Mar;208(3):446–453. [PubMed] [Google Scholar]


