Abstract
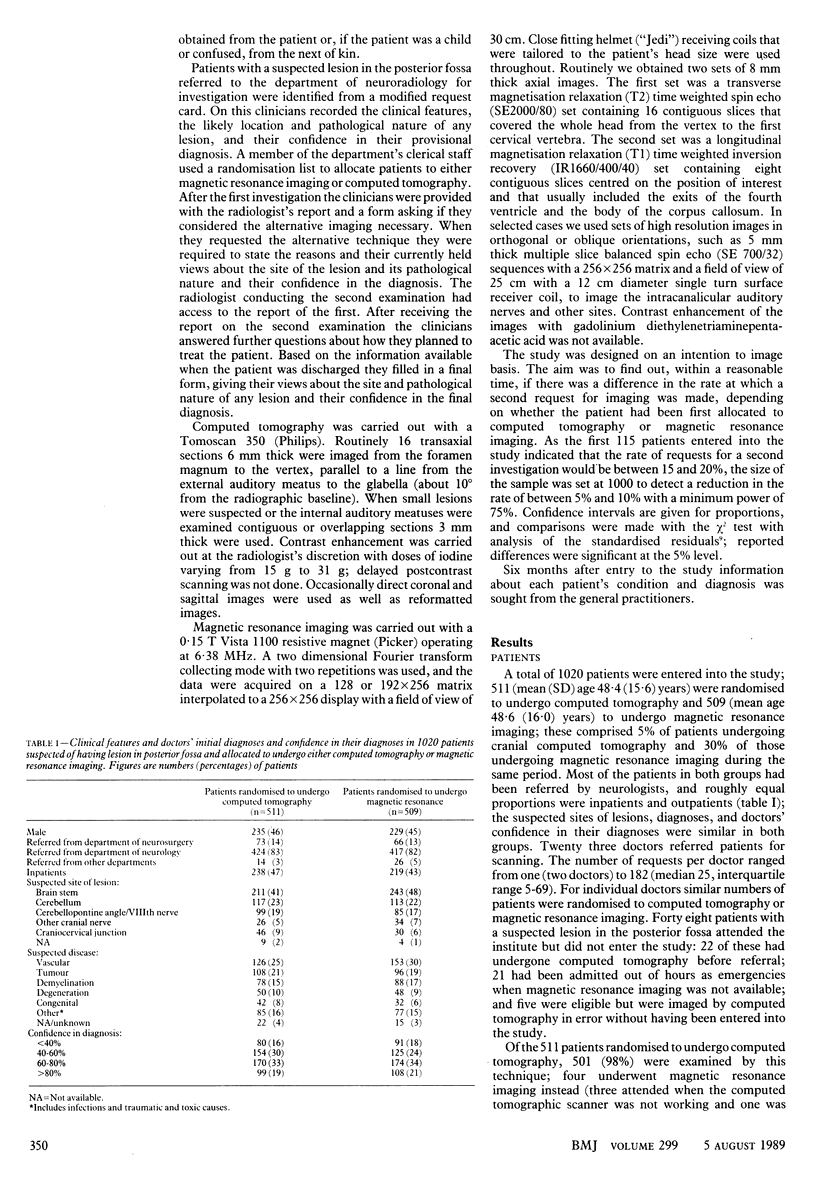
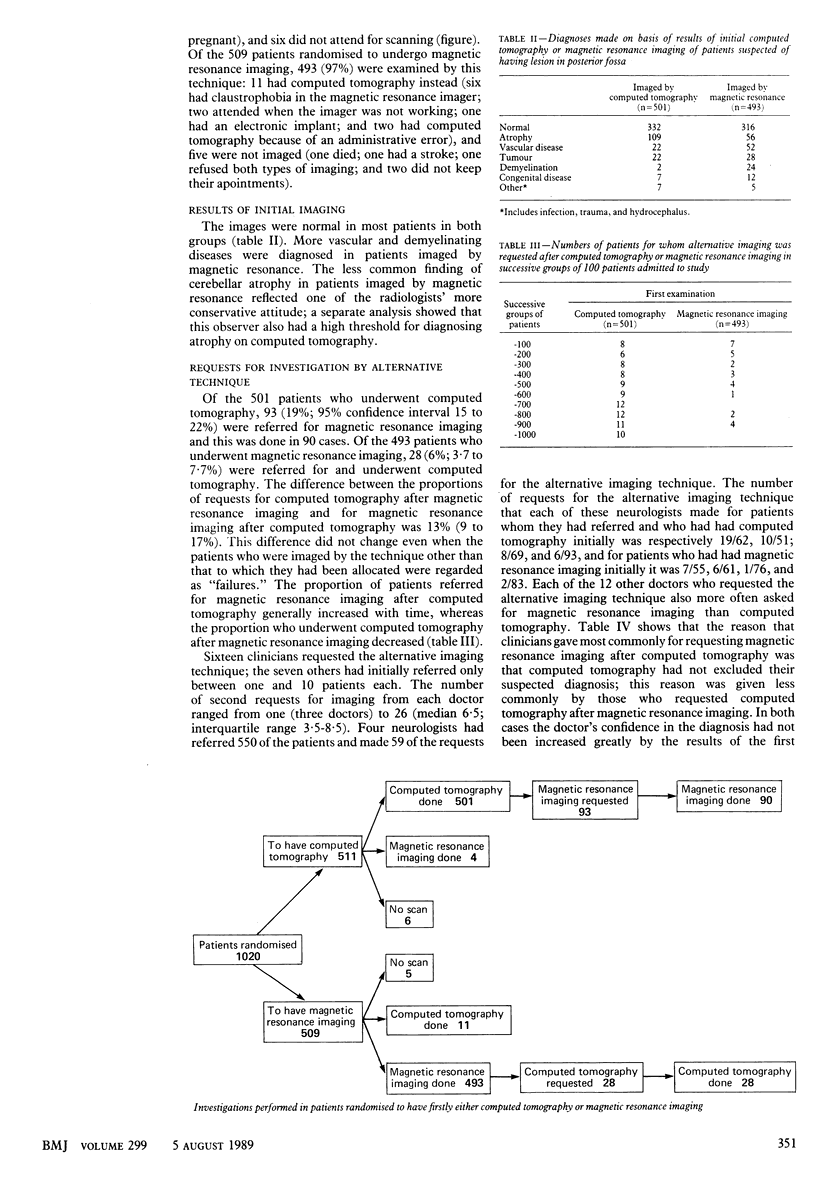
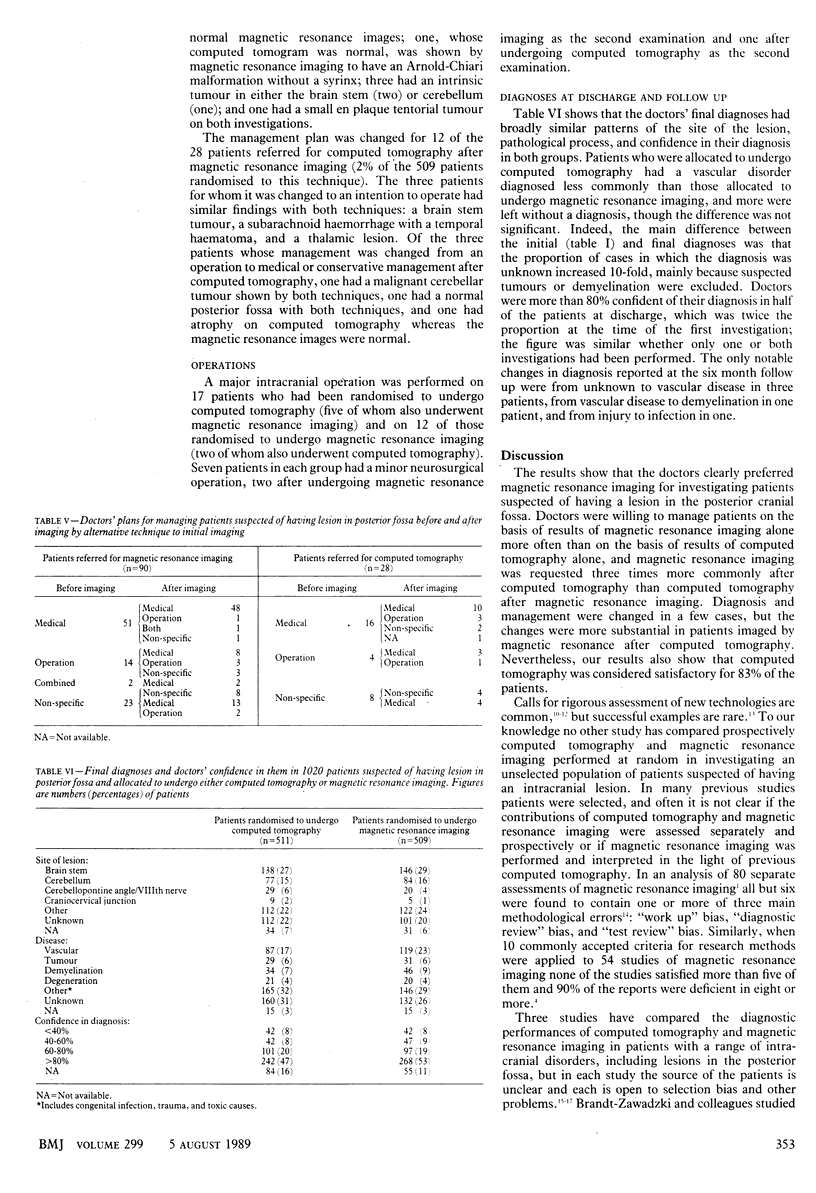
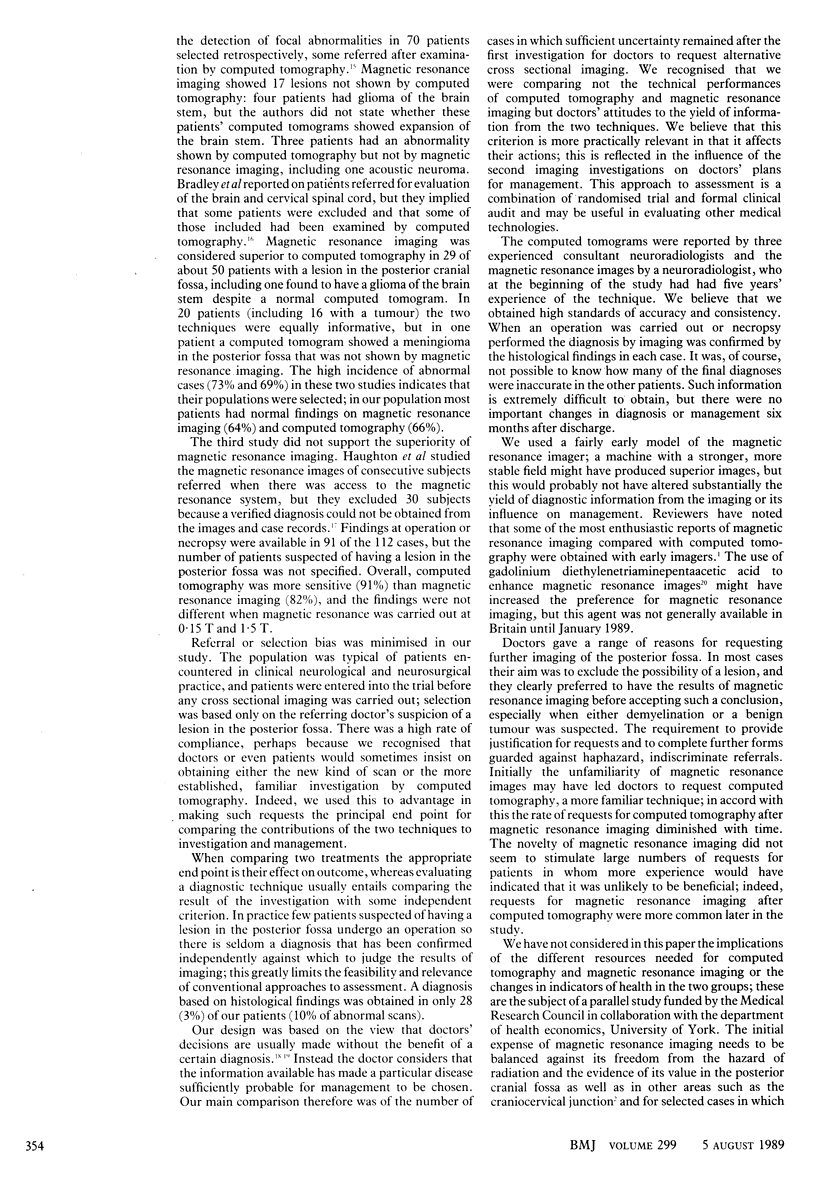
OBJECTIVE--To compare computed tomography and magnetic resonance imaging in investigating patients suspected of having a lesion in the posterior cranial fossa. DESIGN--Randomised allocation of newly referred patients to undergo either computed tomography or magnetic resonance imaging; the alternative investigation was performed subsequently only in response to a request from the referring doctor. SETTING--A regional neuroscience centre serving 2.7 million. PATIENTS--1020 Patients recruited between April 1986 and December 1987, all suspected by neurologists, neurosurgeons, or other specialists of having a lesion in the posterior fossa and referred for neuroradiology. The groups allocated to undergo computed tomography or magnetic resonance imaging were well matched in distributions of age, sex, specialty of referring doctor, investigation as an inpatient or an outpatient, suspected site of lesion, and presumed disease process; the referring doctor's confidence in the initial clinical diagnosis was also similar. INTERVENTIONS--After the patients had been imaged by either computed tomography or magnetic resonance (using a resistive magnet of 0.15 T) doctors were given the radiologist's report and a form asking if they considered that imaging with the alternative technique was necessary and, if so, why; it also asked for their current diagnoses and their confidence in them. MAIN OUTCOME MEASURES--Number of requests for the alternative method of investigation. Assessment of characteristics of patients for whom further imaging was requested and lesions that were suspected initially and how the results of the second imaging affected clinicians' and radiologists' opinions. RESULTS--Ninety three of the 501 patients who initially underwent computed tomography were referred subsequently for magnetic resonance imaging whereas only 28 of the 493 patients who initially underwent magnetic resonance imaging were referred subsequently for computed tomography. Over the study the number of patients referred for magnetic resonance imaging after computed tomography increased but requests for computed tomography after magnetic resonance imaging decreased. The reason that clinicians gave most commonly for requesting further imaging by magnetic resonance was that the results of the initial computed tomography failed to exclude their suspected diagnosis (64 patients). This was less common in patients investigated initially by magnetic resonance imaging (eight patients). Management of 28 patients (6%) imaged initially with computed tomography and 12 patients (2%) imaged initially with magnetic resonance was changed on the basis of the results of the alternative imaging. CONCLUSIONS--Magnetic resonance imaging provided doctors with the information required to manage patients suspected of having a lesion in the posterior fossa more commonly than computed tomography, but computed tomography alone was satisfactory in 80% of cases...
Full text
PDF

Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Balla J. I., Elstein A. S., Christensen C. Obstacles to acceptance of clinical decision analysis. BMJ. 1989 Mar 4;298(6673):579–582. doi: 10.1136/bmj.298.6673.579. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bradley W. G., Jr, Waluch V., Yadley R. A., Wycoff R. R. Comparison of CT and MR in 400 patients with suspected disease of the brain and cervical spinal cord. Radiology. 1984 Sep;152(3):695–702. doi: 10.1148/radiology.152.3.6463251. [DOI] [PubMed] [Google Scholar]
- Brant-Zawadzki M., Norman D., Newton T. H., Kelly W. M., Kjos B., Mills C. M., Dillon W., Sobel D., Crooks L. E. Magnetic resonance of the brain: the optimal screening technique. Radiology. 1984 Jul;152(1):71–77. doi: 10.1148/radiology.152.1.6729138. [DOI] [PubMed] [Google Scholar]
- Bydder G. M., Steiner R. E., Thomas D. J., Marshall J., Gilderdale D. J., Young I. R. Nuclear magnetic resonance imaging of the posterior fossa: 50 cases. Clin Radiol. 1983 Mar;34(2):173–188. doi: 10.1016/s0009-9260(83)80302-x. [DOI] [PubMed] [Google Scholar]
- Cooper L. S., Chalmers T. C., McCally M., Berrier J., Sacks H. S. The poor quality of early evaluations of magnetic resonance imaging. JAMA. 1988 Jun 10;259(22):3277–3280. [PubMed] [Google Scholar]
- Dumoulin C. L., Hart H. R., Jr Magnetic resonance angiography. Radiology. 1986 Dec;161(3):717–720. doi: 10.1148/radiology.161.3.3786721. [DOI] [PubMed] [Google Scholar]
- Hadley D. M., Teasdale G. M. Magnetic resonance imaging of the brain and spine. J Neurol. 1988 Mar;235(4):193–206. doi: 10.1007/BF00314347. [DOI] [PubMed] [Google Scholar]
- Haughton V. M., Rimm A. A., Sobocinski K. A., Papke R. A., Daniels D. L., Williams A. L., Lynch R., Levine R. A blinded clinical comparison of MR imaging and CT in neuroradiology. Radiology. 1986 Sep;160(3):751–755. doi: 10.1148/radiology.160.3.3737914. [DOI] [PubMed] [Google Scholar]
- Hillman B. J. Comparison of CT and MR in 400 patients with suspected disease of the brain and cervical spinal cord. Invest Radiol. 1986 Mar;21(3):289–292. doi: 10.1097/00004424-198603000-00019. [DOI] [PubMed] [Google Scholar]
- Hyman R. A., Gorey M. T. Imaging strategies for MR of the spine. Radiol Clin North Am. 1988 May;26(3):505–533. [PubMed] [Google Scholar]
- Jennett B. Assessment of clinical technologies. Importance for provision and use. Int J Technol Assess Health Care. 1988;4(3):435–445. doi: 10.1017/s0266462300000374. [DOI] [PubMed] [Google Scholar]
- Kent D. L., Larson E. B. Diagnostic technology assessments: problems and prospects. Ann Intern Med. 1988 May;108(5):759–761. doi: 10.7326/0003-4819-108-5-759. [DOI] [PubMed] [Google Scholar]
- Kent D. L., Larson E. B. Magnetic resonance imaging of the brain and spine. Is clinical efficacy established after the first decade? Ann Intern Med. 1988 Mar;108(3):402–424. doi: 10.7326/0003-4819-108-3-402. [DOI] [PubMed] [Google Scholar]
- Macartney F. J. Diagnostic logic. Br Med J (Clin Res Ed) 1987 Nov 21;295(6609):1325–1331. doi: 10.1136/bmj.295.6609.1325. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ransohoff D. F., Feinstein A. R. Problems of spectrum and bias in evaluating the efficacy of diagnostic tests. N Engl J Med. 1978 Oct 26;299(17):926–930. doi: 10.1056/NEJM197810262991705. [DOI] [PubMed] [Google Scholar]
- Sheps S. B. Technological imperatives and paradoxes. JAMA. 1988 Jun 10;259(22):3312–3313. [PubMed] [Google Scholar]
- Smith T. Taming high technology. Br Med J (Clin Res Ed) 1984 Aug 18;289(6442):393–394. doi: 10.1136/bmj.289.6442.393. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thomson J. L. Experiences at the new magnetic resonance imaging centre at Bristol. Br J Radiol. 1989 Feb;62(734):134–137. doi: 10.1259/0007-1285-62-734-134. [DOI] [PubMed] [Google Scholar]


