Abstract
Background
Patients may adopt active and/or passive coping strategies in response to pain. However, it is not known whether these strategies may also precede the onset of chronic symptoms and, if so, whether they are independent predictors of prognosis.
Aim
To examine, in patients with low back pain in general practice, the prognostic value of active and passive coping styles, in the context of baseline levels of pain, disability and pain duration.
Design of study
Prospective cohort study.
Setting
Nine general practices in north west England.
Method
Patients consulting their GP with a new episode of low back pain were recruited to the study. Information on coping styles, pain severity, disability, duration, and a brief history of other chronic pain symptoms was recorded using a self-completion postal questionnaire. Participants were then sent a follow-up questionnaire, 3 months after their initial consultation, to assess the occurrence of low back pain. The primary outcome was persistent disabling low back pain, that is, low back pain at 3-month follow-up self-rated as ≥20 mm on a 100 mm visual analogue scale, and ≥5 on the Roland and Morris Disability Questionnaire.
Results
A total of 974 patients took part in the baseline survey, of whom 922 (95%) completed a follow-up questionnaire; 363 individuals (39%) reported persistent disabling pain at follow-up. Persons who reported high levels of passive coping experienced a threefold increase in the risk of persistent disabling low back pain (relative risk [RR] = 3.0; 95% confidence interval [CI] = 2.3 to 4.0). In contrast, active coping was associated with neither an increase nor a decrease in the risk of a poor prognosis. After adjusting for baseline pain severity, disability, and other measures of pain and pain history, persons who reported a high passive coping score were still at 50% increased risk of a poor outcome (RR = 1.5; 95% CI = 1.1 to 2.0).
Conclusion
Patients who report passive coping strategies experience a significant increase in the risk of persistent symptoms. Further, this risk persists after controlling for initial pain severity and disability. The identification of this low back pain subgroup may help target future treatments to those at greatest risk of a poor outcome.
Keywords: coping behavior, general practice, low back pain, prognosis
INTRODUCTION
Each year around 7% of the UK adult population consult their GP with low back pain and, for the majority, this is of non-specific origin.1,2 The costs associated with the condition are considerable. It is estimated that in the UK the economic burden of back pain in terms of healthcare costs and lost productivity is around £12 billion per annum,3 and the majority of these costs are attributable to the subset of individuals with persistent or recurrent disabling symptoms. It is generally perceived that, of those patients with acute low back pain, most cases resolve spontaneously and only a small proportion experience chronic symptoms. However, recent studies have shown that around half of patients who present with low back pain in primary care still experience pain and disability 3 months after their initial consultation.4
A number of factors have been shown to be associated with poor prognosis, including episode-specific factors and duration of symptoms.5–7 Further, recent evidence has highlighted the role of psychological and psychosocial factors in the aetiology of low back pain.8–10 At a consultation, however, although adequate markers for poor outcome, these factors are difficult to identify and to modify or treat. Available evidence suggests that a bio-psychosocial approach, encouraging better self-management, may be effective at reducing pain and disability in the long term.11 It is important, therefore, to identify factors that are clinically useful in terms of a practical intervention.12,13
How this fits in
Recent work in patients with low back pain has shown that patient coping strategies predict self-rated outcome and functional disability at 3 months, although it is not known to what extent coping style is independent of baseline levels of pain severity and disability. The current study shows that after adjusting for pain and disability, and a number of other pain-related variables, patients who adopt passive coping strategies are still significantly more likely to report persistent disabling low back pain 3 months after their initial consultation. The early identification of this group may help clinicians target treatment to those at greatest risk of persistent symptoms.
A number of recent studies have demonstrated that patient coping strategies predict self-rated outcome and functional disability at 3 months,7,14 and emerging psychological therapies have been shown to result in improvements in coping and disability.15–17 It is not known, however, to what extent coping style is a separate phenomenon, or whether it is a marker for more severe pain initially, and/or higher disability. Thus, the aim of the current study was to examine, in persons consulting their GP with a new episode of low back pain, the prognostic value of active and passive coping styles, in the context of baseline levels of pain intensity, disability and pain duration.
METHOD
A prospective cohort study was conducted involving nine general practices in Cheshire, UK. All patients, aged 18–65 years, consulting their GP with a new episode of low back pain between January 2002 and July 2003 were invited to participate in the study. Those who had consulted with low back pain in the 6 months prior to the index consultation were excluded. Consenting patients were sent a postal questionnaire to collect information on potential risk factors for symptom persistence. Reminder questionnaires were sent to non-responders.
Baseline questionnaire
This questionnaire collected data on age, sex and socioeconomic status using the occupation-based National Statistics Socio-Economic Classification system.18 Information was gathered on the extent to which participants employed active and/or passive coping strategies, with respect to their low back pain, using the Vanderbilt Pain Management Inventory (examples of items from this instrument can be seen in Box 1).19 In addition, data were collected on a number of potential confounding variables: low back pain intensity ‘during the past week’ and disability were measured using a 100 mm visual analogue pain scale and the Roland and Morris Disability Questionnaire,20 respectively. This latter instrument is well validated for use in population samples and the scale ranges from 0 (no disability) to 24, with a score of 5 being considered disabling. A brief history of other chronic pain symptoms was recorded and also whether the patient had ever previously consulted their GP with low back pain (although, by definition, this would be not within the 6 months prior to the current consultation).
Box 1. Items from the Vanderbilt Pain Management Inventory.19.
Subjects were asked to rate how frequently (never, rarely, occasionally, frequently, very frequently) they undertake the following, when their back pain is at a moderate level of intensity, or greater.
Active coping (examples)
-
▸
Staying busy or active
-
▸
Distracting your attention from the pain
-
▸
Taking part in physical activity or physical therapy
Passive coping (examples)
-
▸
Saying to yourself: ‘I wish my doctor would prescribe better pain medication for me’
-
▸
Depending on others for help with your daily tasks
-
▸
Thinking: ‘I can't do anything to lessen this pain’
Follow-up questionnaire
All baseline participants were sent a follow-up questionnaire, to arrive 3 months after their initial GP consultation. Subjects were asked to self-rate their back pain ‘during the past week’ using a 100 mm visual analogue scale and the Roland and Morris Disability Questionnaire. Participants were rated as having persistent disabling low back pain if they reported pain intensity of ≥20 mm on the visual analogue scale, and scored ≥5 on the Roland and Morris Disability Questionnaire.
Analysis
Active and passive coping styles were examined for their ability to predict persistent disabling low back pain using Poisson regression. Thus, results are expressed as relative risks (RR) with 95% confidence intervals (95% CI), the latter being derived using robust estimators of standard error.21 The predictive ability of other baseline variables was assessed in the same manner. Variables that predicted persistent disabling low back pain with a significance of P<0.2, as assessed using a Wald test, were entered into a forward stepwise Poisson regression model. This statistical criterion was chosen to ensure that all variables that predicted the outcome with significance, or even marginal significance, were considered for the final model. An ‘intelligent’ modelling procedure was adopted whereby variables were selected for potential inclusion in the model based on both statistical and biological criteria. Coping style, age, sex and socioeconomic status were forced into the model; other variables were accepted into the final model at P<0.10 and removed at P>0.15. Thus, the relative contribution of coping style to the predictive model could be assessed, after adjusting for any potential confounding effect of other variables.
All analyses were undertaken using Stata v8.2 (Stata Corporation, Texas) and, unless otherwise stated, were adjusted for age, sex and socioeconomic status.
External validity
Because of only a moderate participation rate at baseline, there was concern over the external validity of the study. The only available data on non-participants were age and sex. Thus, to assess external validity, a second multivariable model was constructed, weighting the results back to the age/sex distribution of the target population. Differences between the weighted and unweighted models were then assessed.
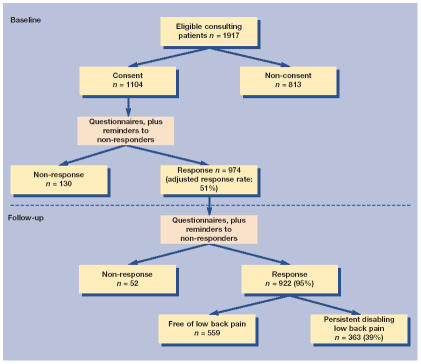
RESULTS
Of 1917 eligible consulting patients, 1104 agreed to participate in the study. Of these, 974 subsequently returned a completed baseline questionnaire (adjusted response rate: 51%). The median age of participants was 47 years (interquartile range: 38–56 years), 577 (59%) were female, and 608 (62%) were known to be in paid employment. Pain severity (visual analogue scale) and disability (Roland and Morris Disability Questionnaire) were moderate: median (interquartile range): 30 mm (12–50 mm) and 8 (4–13), respectively. Nine-hundred and twenty-two participants returned a 3-month follow-up questionnaire (follow-up response rate: 95%), of whom 363 (39%) reported persistent disabling low back pain (hereafter referred to, more simply, as ‘low back pain’). The flow of patients through the study can be seen in Figure 1.
Figure 1.
Flow of patients through the study.
The relationship between demographic characteristics and low back pain at follow-up can be seen in Table 1. Neither age (quartiles) nor sex was associated with low back pain at follow-up. However, persons with a lower income were 50% more likely to report a poor outcome than other individuals (RR = 1.5; 95% CI = 1.3 to 1.9). Similarly, persons not currently in paid employment experienced an increased risk of low back pain at follow-up.
Table 1.
Predictors of persistent disabling low back pain at follow-up: demographic characteristics and coping styles.
| Exposure | Persistent disabling low back pain n (%) | Crude RR (95% CI) | Adjusted RRa (95% CI) |
|---|---|---|---|
| Age (quartiles) years | |||
| 18–38 | 97 (42.0) | 1.0 | 1.0 |
| 38–48 | 95 (41.1) | 1.0 (0.8 to 1.2) | 1.0 (0.8 to 1.3) |
| 48–56 | 86 (37.2) | 0.9 (0.7 to 1.1) | 0.9 (0.7 to 1.2) |
| 56–65.9 | 85 (37.1) | 0.9 (0.7 to 1.1) | 0.9 (0.7 to 1.1) |
| Sex | |||
| Male | 135 (36.8) | 1.0 | 1.0 |
| Female | 228 (41.1) | 1.1 (0.9 to 1.3) | 1.1 (0.9 to 1.3) |
| Socioeconomic status | |||
| High income | 128 (32.0) | 1.0 | 1.0 |
| Medium income | 92 (41.1) | 1.3 (1.04 to 1.6) | 1.3 (1.03 to 1.6) |
| Low income | 131 (49.4) | 1.5 (1.3 to 1.9) | 1.5 (1.3 to 1.9) |
| Currently in paid employment | |||
| Yes | 224 (37.0) | 1.0 | 1.0 |
| No | 107 (49.8) | 1.3 (1.1 to 1.6) | 1.5 (1.2 to 1.8) |
| Active coping (score out of a possible 35) | |||
| 7–19 (low) | 97 (41.8) | 1.0 | 1.0 |
| 20–22 | 93 (37.1) | 0.9 (0.7 to 1.1) | 0.9 (0.7 to 1.1) |
| 23–25 | 90 (39.1) | 0.9 (0.7 to 1.2) | 1.0 (0.8 to 1.2) |
| 26–34 (high) | 72 (38.5) | 0.9 (0.7 to 1.2) | 1.0 (0.8 to 1.3) |
| Passive coping (score out of a possible 55) | |||
| 11–24 (low) | 50 (18.9) | 1.0 | 1.0 |
| 25–28 | 67 (32.8) | 1.7 (1.3 to 2.4) | 1.7 (1.2 to 2.4) |
| 29–33 | 114 (48.3) | 2.6 (1.9 to 3.4) | 2.5 (1.9 to 3.3) |
| 34–51 (high) | 123 (61.2) | 3.2 (2.5 to 4.3) | 3.0 (2.3 to 4.0) |
Adjusted for age, sex and socioeconomic status, where appropriate. RR = relative risk.
Coping strategies
A high score on the active coping scale was associated with neither an increase nor a decrease in the risk of low back pain at follow-up (Table 1). In contrast, persons who adopted high levels of passive coping behaviour experienced a threefold increase in the risk of poor outcome (RR = 3.0; 95% CI = 2.3 to 4.0).
Episode-specific factors
After adjusting for age, sex and socioeconomic status, a number of episode-specific factors were identified that were significantly predictive of pain outcome (Table 2). There was a significant trend to suggest that patients who, at baseline, reported higher levels of pain intensity experienced a increase in the risk of low back pain at follow-up: persons who rated their pain at 80–100 mm were five times more likely to report low back pain at follow-up than those who rated their pain at 0–20 mm (RR = 5.1; 95% CI = 3.8 to 7.0). Similarly, patients with high levels of disability were at increased risk of poor outcome: (RR = 4.8; 95% CI = 3.3 to 6.8). Subjects reporting low back pain every day, and those whose low back pain episode had lasted over 3 months prior to GP consultation were also at increased risk.
Table 2.
Predictors of persistent disabling low back pain at follow-up: episode-specific factors and pain history.
| Exposure | Persistent disabling low back pain n (%) | Crude RR (95% CI) | Adjusted RRa (95% CI) |
|---|---|---|---|
| Pain score (mm) (100 mm visual analogue scale) | |||
| 0–19 | 46 (14.5) | 1.0 | 1.0 |
| 20–39 | 85 (37.1) | 2.6 (1.9 to 3.5) | 2.6 (1.9 to 3.6) |
| 40–59 | 73 (48.3) | 3.3 (2.4 to 4.6) | 3.3 (2.4 to 4.6) |
| 60–79 | 101 (68.7) | 4.7 (3.6 to 6.3) | 4.8 (3.5 to 6.4) |
| 80–100 | 55 (76.4) | 5.3 (3.9 to 7.1) | 5.1 (3.8 to 7.0) |
| Low back pain disability (Roland and Morris Disability Questionnaire20) | |||
| 0–4 (low disability) | 30 (12.4) | 1.0 | 1.0 |
| 5–8 | 87 (39.0) | 3.2 (2.2 to 4.6) | 3.0 (2.1 to 4.4) |
| 9–13 | 105 (45.1) | 3.7 (2.5 to 5.3) | 3.4 (2.4 to 4.9) |
| 14–23 (high disability) | 141 (63.2) | 5.1 (3.6 to 7.3) | 4.8 (3.3 to 6.8) |
| Occurrence of low back pain every day | |||
| No | 72 (19.5) | 1.0 | 1.0 |
| Yes | 291 (52.6) | 2.7 (2.2 to 3.4) | 2.5 (2.0 to 3.1) |
| Duration of current episode | |||
| <1 week | 66 (29.7) | 1.0 | 1.0 |
| 1–4 week | 92 (29.9) | 1.0 (0.8 to 1.3) | 1.0 (0.8 to 1.3) |
| 1–3 months | 51 (38.1) | 1.3 (0.95 to 1.7) | 1.2 (0.9 to 1.7) |
| >3 months | 154 (59.7) | 2.0 (1.6 to 2.5) | 2.0 (1.6 to 2.5) |
| Previous history of low back pain | |||
| No low back pain | 45 (28.7) | 1.0 | 1.0 |
| Low back pain, without previous consultation | 60 (28.0) | 1.0 (0.7 to 1.4) | 1.0 (0.7 to 1.4) |
| Low back pain, with ≥1 previous consultation b | 258 (46.8) | 1.6 (1.3 to 2.1) | 1.7 (1.3 to 2.3) |
| Previous history of other chronic pain symptoms | |||
| No | 145 (26.8) | 1.0 | 1.0 |
| Yes | 218 (57.4) | 2.1 (1.8 to 2.5) | 2.0 (1.7 to 2.4) |
Adjusted for age, sex and socioeconomic status, where appropriate.
Previous consultation, by definition, not within the 6 months prior to baseline survey. RR = relative risk.
Pain history
Persons with a prior history of non-consulting low back pain were no more likely to report low back pain at follow-up than those with no history (Table 2). However, those who had previously consulted their GP with low back pain (although not within the 6 months prior to the baseline consultation) experienced a 70% increase in the risk of poor outcome (RR = 1.7; 95% CI = 1.3 to 2.3). Also, those with a history of other chronic pain symptoms were at significant increased risk (RR = 2.0; 95% CI = 1.7 to 2.4).
Multivariable analysis
A multivariable prediction model was constructed into which age, sex, socioeconomic status and passive coping score were forced. Because of the absence of any association between active coping and low back pain at follow-up, this variable was excluded from further analysis. Six episode-specific factors or variables relating to pain history entered the final model. Even after adjusting for these variables, passive coping significantly contributed to the final model (Wald χ2 = 7.87; P = 0.048); persons with high passive coping score experienced a significant increase in the risk of poor outcome (RR = 1.5; 95% CI = 1.1 to 2.0; Table 3, Model 1). The final model was highly discriminatory with respect to low back pain prognosis: among patients with none of the factors in the final model (at baseline), only 5% reported persistent disabling low back pain at 3 months. In contrast, among those with all seven factors, 87% reported a poor outcome.
Table 3.
Predictors of persistent disabling low back pain at follow-up: multivariable model.
| RRa (95%CI) | ||
|---|---|---|
| Exposure | Model 1 (unweighted) | Model 2 (weighted)b |
| Passive coping (score out of a possible 55) | ||
| 11–24 (low) | 1.0 | 1.0 |
| 25–28 | 1.3 (1.0 to 1.8) | 1.2 (0.9 to 1.7) |
| 29–33 | 1.5 (1.1 to 2.0) | 1.5 (1.1 to 2.0) |
| 34–51 (high) | 1.5 (1.1 to 2.0) | 1.4 (1.01 to 1.9) |
| Pain score (mm) (100mm visual analogue scale) | ||
| 0–19 | 1.0 | 1.0 |
| 20–39 | 1.6 (1.2 to 2.3) | 1.7 (1.2 to 2.4) |
| 40–59 | 1.7 (1.2 to 2.4) | 1.7 (1.2 to 2.5) |
| 60–79 | 2.0 (1.4 to 2.9) | 2.1 (1.5 to 3.0) |
| 80–100 | 2.1 (1.5 to 3.1) | 2.2 (1.5 to 3.2) |
| Previous history of other chronic pain symptoms | ||
| No | 1.0 | 1.0 |
| Yes | 1.4 (1.2 to 1.7) | 1.4 (1.1 to 1.6) |
| Duration of current episode | ||
| <1 week | 1.0 | 1.0 |
| 1–4 week | 1.0 (0.8 to 1.3) | 1.04 (0.8 to 1.4) |
| 1–3 months | 1.1 (0.8 to 1.4) | 1.1 (0.8 to 1.4) |
| >3 months | 1.3 (1.04 to 1.6) | 1.3 (1.04 to 1.7) |
| Roland and Morris Disability Questionnaire20 disability (quartiles) | ||
| 0–4 (low disability) | 1.0 | 1.0 |
| 5–8 | 2.0 (1.3 to 2.9) | 2.2 (1.4 to 3.3) |
| 9–13 | 1.8 (1.2 to 2.7) | 2.0 (1.3 to 3.0) |
| 14–23 (high disability) | 2.1 (1.4 to 3.2) | 2.3 (1.5 to 3.5) |
| Currently in paid employment | ||
| Yes | 1.0 | 1.0 |
| No | 1.2 (1.04 to 1.4) | 1.2 (1.03 to 1.4) |
| Occurrence of low back pain every day | ||
| No | 1.0 | 1.0 |
| Yes | 1.3 (1.02 to 1.7) | 1.3 (1.04 to 1.7) |
Adjusted for age, sex and socioeconomic status.
Weighted to age and sex distribution of target population.
External validity
Of the 1917 eligible consulting patients, only 974 returned a completed baseline questionnaire. Participants were more likely to be female (59%, versus 49% of non-participants; χ2 = 20.7; P<0.001) and were slightly older (median age = 47 years and 40 years, respectively; Mann–Whitney Z = 9.63; P<0.001). However, weighting the analysis back to the age/sex distribution of the original target population did not alter the multivariable model to any great extent (Table 3, Model 2) and did not change the study interpretation. Persons with high passive coping score still experienced a significantly elevated risk of low back pain at follow-up (RR = 1.4; 95% CI = 1.01 to 1.9).
DISCUSSION
Summary of main findings
This study has demonstrated that approximately 40% of patients who consult their GP with low back pain still report persistent disabling symptoms 3 months subsequently. Further, patients who adopt high levels of passive coping strategies experience a significant increase in the risk of poor short-term outcome, and this relationship persists even after adjusting for baseline levels of pain intensity, disability and duration. In contrast, the adoption of active coping strategies appears not to confer any benefit.
Strengths and limitations of the study
There are a number of methodological aspects to consider. Firstly, baseline participation was low and it is important, therefore, to assess whether selection bias, caused by selective participation and/or follow-up, may have influenced results. Of 1917 individuals invited to participate in the study, 58% agreed to participate, although only 88% of these subsequently returned a completed full-length baseline questionnaire. By definition, little data are available on non-participants. However, one can calculate that if all non-participants were pain-free at 3-month follow-up the prevalence of persistent disabling low back pain would still be around 20%.
Although participants and non-participants differed by age and sex, a weighted analysis, weighting the population back to the age/sex distribution of the target population, revealed similar results to the main findings. This would suggest that the demographic differences between participants and non-participants (insofar as we are able to examine them using available data) have not introduced a bias to the current study. Further, follow-up participation was high (95%) and it is unlikely, therefore, that bias was introduced through loss to follow-up.
Secondly, although we purport to have measured persistent low back pain, our exposures and outcome were measured in two consecutive cross-sectional surveys. Not having information about pain status between the two time points, it is possible that in some individuals we have identified recurrent low back pain, rather than persistent symptoms. Notwithstanding the fact that this may also be a valid outcome in general practice, this would serve to overestimate the prevalence of persistent low back pain. A corollary of this, however, is that the true associations between passive coping (and other risk factors) and outcome will actually be greater than we report here.
Thirdly, it seems somewhat counterintuitive that active and passive strategies do not elicit contrary responses: persons who reported high levels of passive coping behaviour experienced a significant increase in the risk of low back pain at follow-up, whereas those who adopted active coping strategies did not experience a decrease in risk. Active coping in the current study was defined as positive responses to statements such as, ‘I am able to ignore my pain’ and ‘I participate in all my usual leisure activities’; whereas a high passive coping score required positive responses to statements such as, ‘I wish my doctor would prescribe better pain medication’ and ‘I restrict or cancel my social activities’. However, rather than showing a strong inverse correlation between active and passive coping strategies, the current results show only a poor correlation (r = −0.13). This slight inverse correlation, confirming previous findings,19 goes some way to explaining the specificity of the results for passive coping. Furthermore, it could be argued that persons who consult their GP are already exhibiting characteristics of passive coping behaviour and, therefore, the range of coping strategies in our cohort may be restricted. However, this would make it more difficult to detect any association between passive coping strategy and low back pain. Despite this, individuals in the highest quartile of passive coping score were more than three times more likely to report a poor outcome at 3-month follow-up than those in the lowest quartile. This would suggest that across the full range of coping strategies the effect might be even greater.
Fourthly, a number of factors previously shown to be important in the epidemiology of low back pain are missing from our model. Previous studies have demonstrated that psychological distress and work-related psychosocial factors are important predictors of low back pain outcome,6 and these factors may influence coping strategies. However, our multivariable model performs well and among persons with all seven factors in the final model (that is, excluding age, sex and socioeconomic status), 87% report low back pain at follow-up. We suggest that the addition of other variables, such as psychological distress, would actually add little to the overall model.
Finally, some have suggested that a high passive coping score is only a proxy for severe baseline pain.22 Our results only partly support this theory — the risk ratio associated with a high passive coping score drops from 3.0 (2.3 to 4.0) to 1.5 (1.1 to 2.0) on adjustment for pain severity, disability and other baseline variables. However, passive coping remains independently and significantly predictive in the final model, suggesting that it is an independent construct and can precede chronic pain symptoms.
Comparison with existing literature
We have shown that, in a population of adults with a new consulting episode of low back pain, 39% report persistent disabling low back pain 3 months subsequently. This is in contrast to the common preconception that only a small proportion of patients experience chronic disabling symptoms. However, other authors have demonstrated similar findings: Croft et al showed that 50% of patients reported pain and disability 3 months after their initial consultation.4 Further, these authors also demonstrated that the same proportion were reporting symptoms 12 months post-consultation, although the majority will have stopped consulting with this pain.
Some authors have demonstrated the ability to identify patients at risk of poor work and functional outcome using a combination of pain intensity, fear avoidance, function and mood, but have been unable to predict persistent pain.23 Others have shown that psychological factors, in particular distress and somatisation, are strong predictors of chronic low back pain,24 and there is an emerging body of evidence to support the involvement of various aspects of coping behaviours in the epidemiology of low back pain, to which this study adds.
Our results are consistent with recent findings of Smith et al who reported that at 4-year follow-up, in addition to clinical factors, health-seeking behaviour was significantly associated with the onset, and persistence, of chronic back pain in the community.13 A smaller study, in general practice, demonstrated that initial pain intensity, a prior pain history, and low levels of active coping were predictive of low back pain outcome 3 months after consultation,14 and Burton et al report that aspects of coping strategy are important predictors of low back pain in acute patients (pain ≤3 weeks) but not those with subacute symptoms (>3 and <52 weeks).25 In addition, other authors have shown the importance of strategies for coping with pain in the prognosis of other musculoskeletal conditions: whiplash disorder,26,27 and rheumatoid- and osteo-arthritis.28,29
To focus on coping strategies, rather than other psychological and psychosocial indicators is important, as patients' coping strategies may be modified through cognitive-behavioural therapy.30 Several studies have demonstrated that intensive cognitive-behavioural treatments can be effective in improving pain, coping and disability in chronic low back pain patients,15–17 and others have shown that in patients with subacute low back pain a cognitive-behavioural therapy-based educational programme results in demonstrable improvements in pain and disability at 3- and 6-month follow-up.31 Other authors have shown that exercise programmes using cognitive-behavioural therapy principles can be effective at reducing pain and disability for up to a year,11 and these authors subsequently demonstrated that cognitive-behavioural therapy-based exercise programmes were most effective in patients with high fear avoidance behaviour.32 Although few GPs have quick access to individuals trained in cognitive-behavioural therapy, they may still provide education reassurance and advice, encouraging early mobilisation and recommending light activity.
Implications for clinical practice and future research
In summary, this is one of the first studies to examine, prospectively, the role of coping strategies in the prognosis of low back pain in primary care. While not dismissing the notion that chronic pain may lead to an increase in passive coping, our findings demonstrate that such coping strategies can also precede the occurrence of persistent disabling low back pain and that patients who report high passive coping strategies experience a significant increase in the risk of persistent symptoms. Further, although somewhat attenuated, this risk remains after adjusting for baseline levels of pain severity, disability and other measures of pain and pain history. We propose that the identification of such an ‘at risk’ group may help inform future treatment and management decisions — in particular, in targeting treatments that have been shown to be effective, but resource intensive, to the subgroup of patients who are at highest risk of a poor outcome.
Acknowledgments
We acknowledge the help of a number of staff at the University of Manchester, in particular Miss Alison Littlewood, for help with study conduct. In addition, we are grateful for the help and support of the general practices and patients involved in this study.
Funding body
Arthritis Research Campaign, Chesterfield, UK (M0637)
Ethics committee
South Cheshire Local Research Ethics Committee, (M134/01)
Competing interests
The authors have stated that there are none
REFERENCES
- 1.McCormick A. Morbidity statistics from general practice: fourth national study 1991–92. A study carried out by the Royal College of General Practitioners, the Office of Population Censuses and Surveys, and the Department of Health. London: HMSO; 1995. [Google Scholar]
- 2.Deyo RA, Rainville J, Kent DL. What can the history and physical examination tell us about low back pain? JAMA. 1992;268:760–765. [PubMed] [Google Scholar]
- 3.Maniadakis N, Gray A. The economic burden of back pain in the UK. Pain. 2000;84:95–103. doi: 10.1016/S0304-3959(99)00187-6. [DOI] [PubMed] [Google Scholar]
- 4.Croft PR, Macfarlane GJ, Papageorgiou AC, et al. Outcome of low back pain in general practice: a prospective study. BMJ. 1998;316:1356–1359. doi: 10.1136/bmj.316.7141.1356. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Coste J, Lefrancois G, Guillemin F, Pouchot J. French Study Group for Quality of Life in Rheumatology. Prognosis and quality of life in patients with acute low back pain: insights from a comprehensive inception cohort study. Arthritis Rheum. 2004;51:168–176. doi: 10.1002/art.20235. [DOI] [PubMed] [Google Scholar]
- 6.Thomas E, Silman AJ, Croft PR, et al. Predicting who develops chronic low back pain in primary care: a prospective study. BMJ. 1999;318:1662–1667. doi: 10.1136/bmj.318.7199.1662. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Van der Weide WE, Verbeek JH, Salle HJ, van Dijk FJ. Prognostic factors for chronic disability from acute low-back pain in occupational health care. Scand J Work Environ Health. 1999;25:50–56. doi: 10.5271/sjweh.383. [DOI] [PubMed] [Google Scholar]
- 8.Papageorgiou AC, Macfarlane GJ, Thomas E, et al. Psychosocial factors in the workplace — do they predict new episodes of low back pain? Evidence from the South Manchester Back Pain Study. Spine. 1997;22:1137–1142. doi: 10.1097/00007632-199705150-00014. [DOI] [PubMed] [Google Scholar]
- 9.Harkness EF, Macfarlane GJ, Nahit ES, et al. Risk factors for new-onset low back pain amongst cohorts of newly employed workers. Rheumatology. 2003;42:959–968. doi: 10.1093/rheumatology/keg265. [DOI] [PubMed] [Google Scholar]
- 10.Jones GT, Watson KD, Silman AJ, et al. Predictors of low back pain in British schoolchildren: a population-based prospective cohort study. Pediatrics. 2003;111:822–828. doi: 10.1542/peds.111.4.822. [DOI] [PubMed] [Google Scholar]
- 11.Klaber Moffett JA, Torgerson D, Bell-Syer S, et al. Randomised controlled trial of exercise for low back pain: clinical outcomes, costs, and preferences. BMJ. 1999;319:279–283. doi: 10.1136/bmj.319.7205.279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Linton SJ. A review of psychological risk factors in back and neck pain. Spine. 2000;25:1148–1156. doi: 10.1097/00007632-200005010-00017. [DOI] [PubMed] [Google Scholar]
- 13.Smith BH, Elliott AM, Hannaford PC, et al. Factors related to the onset and persistence of chronic back pain in the community: results from a general population follow-up study. Spine. 2004;29:1032–1040. doi: 10.1097/00007632-200405010-00016. [DOI] [PubMed] [Google Scholar]
- 14.Potter RG, Jones JM, Boardman AP. A prospective study of primary care patients with musculoskeletal pain: the identification of predictive factors for chronicity. Br J Gen Pract. 2000;50:225–227. [PMC free article] [PubMed] [Google Scholar]
- 15.Alaranta H, Rytokoski U, Rissanen A, et al. Intensive physical and psychosocial training program for patients with chronic low back pain. A controlled clinical trial. Spine. 1994;19:1339–1349. doi: 10.1097/00007632-199406000-00007. [DOI] [PubMed] [Google Scholar]
- 16.Basler HD, Jakle C, Kroner-Herwig B. Incorporation of cognitive-behavioral treatment into the medical care of chronic low back patients: a controlled randomized study in German pain treatment centers. Patient Educ Couns. 1997;31:113–124. doi: 10.1016/s0738-3991(97)00996-8. [DOI] [PubMed] [Google Scholar]
- 17.Bendix AF, Bendix T, Vaegter K, et al. Multidisplinary intensive treatment for chronic low back pain: a randomised, prospective study. Cleve Clin J Med. 1996;63:62–69. doi: 10.3949/ccjm.63.1.62. [DOI] [PubMed] [Google Scholar]
- 18.Rose D, Pevalin DJ. A researcher's guide to the national statistics socio-economic classification. London: Sage Publications; 2003. [DOI] [PubMed] [Google Scholar]
- 19.Brown GK, Nicassio PM. Development of a questionnaire for the assessment of active and passive coping strategies in chronic pain patients. Pain. 1987;31:53–64. doi: 10.1016/0304-3959(87)90006-6. [DOI] [PubMed] [Google Scholar]
- 20.Roland M, Morris R. A study of the natural history of back pain. Part I: Development of a reliable and sensitive measure of disability in low-back pain. Spine. 1983;8:141–144. doi: 10.1097/00007632-198303000-00004. [DOI] [PubMed] [Google Scholar]
- 21.Greenland S. Model-based estimation of relative risks and other epidemiologic measures in studies of common outcomes and in case-control studies. Am J Epidemiol. 2004;160:301–305. doi: 10.1093/aje/kwh221. [DOI] [PubMed] [Google Scholar]
- 22.Carroll L, Mercado AC, Cassidy JD, Cjte P. A population-based study of factors associated with combinations of active and passive coping with neck and low back pain. J Rehabil Med. 2002;34:67–72. doi: 10.1080/165019702753557854. [DOI] [PubMed] [Google Scholar]
- 23.Linton SJ, Boersma K. Early identification of patients at risk of developing a persistent back problem: the predictive validity of the Orebro Musculoskeletal Pain Questionnaire. Clin J Pain. 2003;19:80–86. doi: 10.1097/00002508-200303000-00002. [DOI] [PubMed] [Google Scholar]
- 24.Pincus T, Burton AK, Vogel S, Field AP. A systematic review of psychological factors as predictors of chronicity/disability in prospective cohorts of low back pain. Spine. 2002;27:E109–E120. doi: 10.1097/00007632-200203010-00017. [DOI] [PubMed] [Google Scholar]
- 25.Burton AK, Tillotson KM, Main CJ, Hollis S. Psychosocial predictors of outcome in acute and subchronic low back trouble. Spine. 1995;20:722–728. doi: 10.1097/00007632-199503150-00014. [DOI] [PubMed] [Google Scholar]
- 26.Bosma FK, Kessels RP. Cognitive impairments, psychological dysfunction, and coping styles in patients with chronic whiplash syndrome. Neuropsychiatry Neuropsychol Behav Neurol. 2002;15:56–65. [PubMed] [Google Scholar]
- 27.Soderlund A, Lindberg P. Long-term functional and psychological problems in whiplash associated disorders. Int J Rehabil Res. 1999;22:77–84. doi: 10.1097/00004356-199906000-00001. [DOI] [PubMed] [Google Scholar]
- 28.Evers AW, Kraaimaat FW, Geenen R, Bijlsma JW. Psychosocial predictors of functional change in recently diagnosed rheumatoid arthritis patients. Behav Res Ther. 1998;36:179–193. doi: 10.1016/s0005-7967(98)00019-9. [DOI] [PubMed] [Google Scholar]
- 29.Steultjens MP, Dekker J, Bijlsma JW. Coping, pain, and disability in osteoarthritis: a longitudinal study. J Rheumatol. 2001;28:1068–1072. [PubMed] [Google Scholar]
- 30.Enright SJ. Cognitive behaviour therapy — clinical applications. BMJ. 1997;314:1811–1816. doi: 10.1136/bmj.314.7097.1811. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Moore JE, Von Korff M, Cherkin D, et al. A randomized trial of a cognitive-behavioral program for enhancing back pain self care in a primary care setting. Pain. 2000;88:145–153. doi: 10.1016/S0304-3959(00)00314-6. [DOI] [PubMed] [Google Scholar]
- 32.Klaber Moffett JA, Carr J, Howarth E. High fear-avoiders of physical activity benefit from an exercise program for patients with back pain. Spine. 2004;29:1167–1172. doi: 10.1097/00007632-200406010-00002. [DOI] [PubMed] [Google Scholar]