Abstract
Background
The UK urgent cancer referral guidance was introduced between 1999–2000. There is a dearth of literature relating to the effectiveness in detecting cancer of urgent suspected cancer referrals and general practitioners' compliance with the guidance.
Aims
This paper aims to determine the diagnostic yield from urgent referrals for suspected colorectal, lung, ovarian and prostate cancer, and the proportion of patients with cancer who were urgently referred. Secondary aims are to determine the association of these findings with age, ethnicity, sex and marital status, and to determine the proportions of patients who fulfilled the urgent referral criteria.
Design
Detailed notes analysis of all urgent referrals and all cancer diagnoses.
Setting
One hospital trust in England.
Method
Data regarding all urgent referrals and all cancer diagnoses were obtained from one hospital trust over a 2-year period. Data analysis was undertaken to determine, diagnostic yields and their association with sociodemographic factors, trends over time and fulfilment of the guidance.
Results
The percentages of urgent referrals diagnosed with cancer were colorectal 11%, lung 42%, ovarian 20%, and prostate 50%. The percentages of patients with cancer referred urgently were colorectal 21%, lung 23%, ovarian 24%, and prostate 32%. Patients who were urgently referred without cancer were younger than those with cancer for all but prostate. There were no significant differences by sex, marital status or ethnicity. For patients with cancer there were no differences for any sociodemographic factors in whether or not they were referred urgently.
Conclusions
The predictive power of the referral guidance as a marker for cancer is low, resulting in significant numbers of patients being urgently referred without cancer. A large majority of patients not diagnosed with cancer through the urgent referral route did fulfil the criteria for urgent referral, suggesting that with more widespread use of the guidance the diagnostic yields will be higher. This has implications for patients, on hospital diagnostic systems, and for patients presenting through other pathways.
Keywords: colorectal cancer, lung cancer, ovarian cancer, prostate cancer, referral
INTRODUCTION
All patients with suspected cancer are guaranteed to see a hospital doctor within 2 weeks of their GP requesting an urgent appointment.1 The urgent cancer referral guidelines were implemented in stages between 1999–2000.2 These guidelines aim to facilitate appropriate referral from primary to secondary care for patients whom a GP suspects may have cancer.3 Patients whose symptoms fulfil the criteria should be referred using dedicated forms faxed through to a dedicated number for fast-track assessment. At the time of their introduction, there was a lack of evidence concerning their effectiveness, in particular their diagnostic yield.4 The original guidance has recently been updated,5 and is a further step in the evolutionary process of improving cancer diagnosis.6
Since the introduction of the guidance, several studies have reported findings in colorectal cancer. Studies have reported 26.1%7 and 17.9%8 of patients diagnosed with cancer being referred urgently by GPs. Approximately one-third present as emergencies.7,9 Of the remainder, 16.1% are non-urgent referrals, and 21.7% referred from other clinics;7 and a small percentage are diagnosed through screening. One-third to one-half of patients with colorectal malignancy are not perceived as urgent by the GP.9–12 For patients who are referred urgently, reported rates of malignancy vary between 6% (compared with 1% for non urgent referrals),10 8.9%,13 9.4%,7 14.4%,8 and 16%.14 Recent data relating to suspected prostate cancer found that of 35 patients referred with raised PSA (prostate specific antigen), 11 had prostate cancers, most of which were advanced.15 No similar data have been reported for lung or ovarian cancer. Few studies have reported compliance with the guidance. For colorectal cancer, only 6 out of 390 urgent referrals were shown to be compliant with the guidance.10 However, for urological cancers, few urgent referrals for suspected cancer complied with the guidance.16 Patients who are referred urgently do experience considerable distress while waiting to be seen.17
How this fits in
The urgent cancer referral guidance was introduced as a UK government policy. The predictive power of the guidance for these four cancers is low with the majority of cancers being diagnosed in patients referred via other routes. More widespread application of the guidance is likely to lead to higher diagnostic yields.
The aim of this paper is to determine from a large sample of patients:
the proportion of patients urgently referred by their GP (through the fast-track system) for suspected colorectal, lung, ovarian and prostate cancer who were diagnosed with cancer, and any association of this with sociodemographic factors (age, ethnicity, sex and marital status);
the proportion of patients diagnosed with colorectal, lung, ovarian and prostate cancer who were urgently referred by their GP (through the fast-track system), and any association of this with sociodemographic factors (age, ethnicity, sex and marital status);
the proportion of patients who fulfilled the urgent referral criteria; and
trends in GP urgent referrals for suspected cancer, and their diagnostic yield, over time.
METHOD
Baseline population
The quarterly monitoring central return (QMCW) is used to monitor the performance of the urgent (2-week) standard. The QMCW return was obtained for a 2-year period between 1 January 2001 and 31 December 2002 from Bradford Hospitals NHS Trust. We obtained details of all patients who attended for a hospital outpatient appointment for suspected colorectal, lung, ovarian or prostate cancer in this same time period. The urgent referrals for suspected ovarian and prostate cancer are included within gynaecological cancer (which also includes suspected cancers of the cervix, endometrium and vagina/vulva), and urological cancer (which includes suspected cancers of the testis, kidney and bladder) respectively. In total, 2082 urgent referrals were identified: lung (n = 352), colorectal (n = 764), urology (n = 510), and gynaecology (n = 456). Data were also obtained from histopathology, enabling us to obtain the total sample of new (not recurrent) cancer diagnoses for the same time period. This identified 1778 patients: lung (n = 672), colorectal (n = 500), prostate (n = 448), and ovarian (158). These datasets were amalgamated to determine which of the urgent referrals had a cancer diagnosis in the study period, and which did not. This resulted in a total of 3581 patients falling into one of three groups: patients with cancer who were referred as an urgent referral; patients not diagnosed as having cancer who were referred as an urgent referral; and patients with cancer who were not referred as an urgent referral.
Throughout this paper we refer to urgent referrals as those made according to the guidance for suspected cancer as a fast track referral. Patients referred by a GP letter were classified as non-urgent, even if they were marked ‘urgent’; this was because such referrals were dealt with in a non-uniform way by the trust, and because they are outside the reporting and monitoring system for the urgent suspected cancer referral guidance.
Data extraction and cleaning
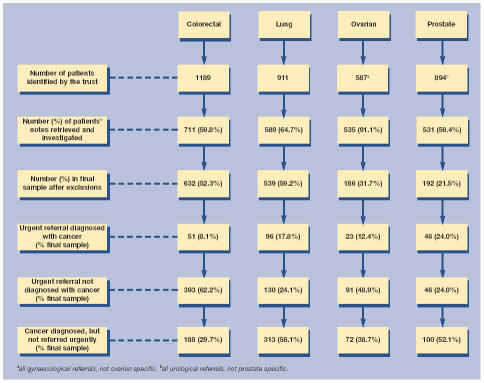
The notes of 2366 (66%) patients were investigated (Figure 1). The remaining notes either could not be found in the medical records department or were booked out and unavailable throughout the study's phase of data collection, despite considerable and repeated efforts to trace them. The number of patients referred urgently but not diagnosed with cancer are inflated for suspected prostate and ovarian cancer as these included all gynaecology and urology referrals. These could not be distinguished from other cancers until we had investigated the patient's referral form and medical records. A range of data was extracted from the patients' medical records; this included:
demographic data: age; sex; marital status (only recorded as married, single, divorced or widowed); and ethnicity (only recorded as white, South Asian, black or other);
source of referral: urgent GP suspected cancer referral; non-urgent GP-referral; inter-speciality referral; accident and emergency (A&E); screening; or other;
dates of events: date of referral (taken from either: the date of GP referral letter or urgent referral form; the date of inter-speciality referral; the date of A&E attendance; or the date of a screening referral); date of the first hospital appointment (from urgent appointment slip, or from clinic notes, and cross checked); date of cancer diagnosis (from specialist's letter to GP, or if unavailable from results letter, multidisciplinary team meeting notes, or histology report); and date of death (taken from the death certificate, or from patient notes, or PAS (Patient Administration System) database; and
detail of GP referral: for urgent referrals, data about the referral were gathered from the urgent referral form, with symptoms being recorded in a tick-box format mirroring the urgent referral guidance. For non-urgent GP, inter-speciality and A&E referrals, information about referring symptoms was obtained from the referral letter.
Figure 1.
Flow diagram showing identification of patients into the final sample.
Outcomes from some of these data are not reported in this paper
As a result of data cleaning, some patients were excluded from the analysis (if their first outpatient appointment was prior to 2001 or after 2002, or if their records were missing details of referral or diagnosis) and some were reclassified into the correct outcome group (Figure 1). Suspected ovarian and prostate cancers were included within the larger groupings of suspected gynaecological and urological cancers respectively; hence the proportion of patients in the final sample appears much smaller than for the other two cancers.
Statistical analysis
Numbers, percentages, means and standard deviations are presented. Fisher's Exact and χ2 were used to compare categorical variables. ANOVA and t-tests were used to compare continuous variables. A P-value of <0.01 was considered to indicate statistical significance. All analyses were performed on SPSS (Version 11). For trends over time, the numbers of patients per quarter was too small for formal statistical testing.
Fulfilment of the referral criteria
For patients urgently referred, this was determined from the urgent referral form. For patients not referred urgently this was determined by the researchers from symptoms documented in the referral letter (where there was one) or, retrospectively, referring symptoms were determined from records made at the initial outpatient appointment. All the researchers were trained in the collection of such data and queries resolved by others in the research team.
RESULTS
Proportions of urgent referrals diagnosed with cancer and of cancer patients who were referred urgently
The proportions of urgent referrals who were diagnosed with cancer were 51/444 (11%) for suspected colorectal cancer, 96/226 (42%) for suspected lung cancer, 23/114 (20%) for suspected ovarian cancer, and 46/92 (50%) for suspected prostate cancer. The proportions of patients with cancer who were referred urgently were 51/239 (21%) for colorectal cancer, 96/409 (23%) for lung cancer, 23/95 (24%) for ovarian cancer, and 46/146 (32%) for prostate cancer.
Sociodemographics factors
Patients who were urgently referred but did not have cancer were younger than those who did have cancer for lung ([n = 224] t = 2.17, P = 0.031), colorectal ([n = 442] t = 3.50, P = 0.001) and ovarian cancer ([n = 112] t = 3.338, P = 0.001), but there was no difference for prostate cancer (Table 1). For colorectal cancer there was no significant difference in the proportion of patients who were male and female (Fisher's Exact, P = 0.016), however, females were less likely than males to be diagnosed with cancer (9 versus 16%); there were no age differences for lung cancer. There was no significant difference by marital status or ethnicity, for any of the cancers. For patients who did have cancer, there were no differences for any of the sociodemographic factors in whether they were referred urgently or not.
Table 1.
Patient characteristics by cancer type and group.
| Patients with cancer diagnoses and non-urgent referrals | Patients with cancer diagnoses and urgent referrals | Patients without cancer diagnoses and urgent referrals | Total | |
|---|---|---|---|---|
| Age (mean [SD]) | ||||
| Colorectal | 71.1 (12.3) | 70.4 (11.7) | 63.1(14.3) | 66.0 (14.0) |
| Lung | 66.5 (11.6) | 67.2 (11.0) | 63.6 (13.3) | 65.9 (12.0) |
| Ovarian | 64.6 (13.4) | 68.2 (11.2) | 56.5 (15.8) | 60.7 (15.2) |
| Prostate | 73.1 (9.7) | 70.4 (8.8) | 66.3 (11.1) | 70.9 (11.1) |
| Sex (n [%]) | ||||
| Colorectal | ||||
| Male | 97 (52) | 27 (53) | 142 (36%) | 266 |
| Female | 90 (48) | 24 (47) | 251 (64%) | 365 |
| Lung | ||||
| Male | 153 (57) | 48 (55) | 80 (62) | 204 |
| Female | 117 (43) | 39 (45) | 49 (38) | 205 |
| Ethnic group (n [%]) | ||||
| Colorectal | ||||
| White | 144 (96) | 44 (100) | 254 (93) | 442 |
| South Asian | 4 (3) | 0 (0) | 15 (5) | 19 |
| Black | 2 (1) | 0 (0) | 4 (1) | 6 |
| Other | 1 (1) | 1 | ||
| Lung | ||||
| White | 151 (97) | 60 (97) | 69 (88) | 280 |
| South Asian | 5 (3) | 2 (3) | 8 (10) | 15 |
| Chinese | 0 (0) | 0 (0) | 1 (1) | 1 |
| Ovarian | ||||
| White | 46 (94) | 12 (100) | 59 (87) | 117 |
| South Asian | 3 (6) | 0 (0) | 8 (12) | 11 |
| Black | 0 (0) | 0 (0) | 1 (1) | 1 |
| Prostate | ||||
| White | 54 (92) | 29 (100) | 28 (93) | 111 |
| South Asian | 2 (3) | 0 (0) | 2 (7) | 4 |
| Black | 2 (3) | 0 (0) | 0 (0) | 2 |
| Other | 1 (2) | 0 (0) | 0 (0) | 1 |
| Marital status (n [%]) | ||||
| Colorectal | ||||
| Divorced | 9 (5) | 3 (6) | 27 (7) | 39 |
| Married | 108 (60) | 30 (60) | 243 (66) | 381 |
| Single | 19 (11) | 5 (10) | 47 (13) | 71 |
| Widowed | 43 (24) | 12 (24) | 49 (13) | 104 |
| Lung | ||||
| Divorced | 14 (7) | 8 (10) | 7 (6) | 29 |
| Married | 141 (67) | 60 (77) | 72 (66) | 273 |
| Single | 21 (10) | 4 (5) | 12 (11) | 37 |
| Widowed | 36 (17) | 6 (8) | 18 (17) | 60 |
| Ovarian | ||||
| Divorced | 4 (7) | 1 (7) | 5 (6) | 10 |
| Married | 38 (69) | 9 (64) | 58 (75) | 105 |
| Single | 5 (9) | 0 (0) | 4 (5) | 9 |
| Widowed | 8 (15) | 4 (29) | 10 (13) | 22 |
| Prostate | ||||
| Divorced | 3 (3) | 2 (5) | 1 (3) | 6 |
| Married | 75 (81) | 36 (82) | 32 (80) | 143 |
| Single | 2 (2) | 1 (2) | 3 (8) | 6 |
| Widowed | 13 (14) | 5 (11) | 4 (10) | 22 |
SD = standard deviation.
Variation over time of referrals and cancer diagnoses from these referrals
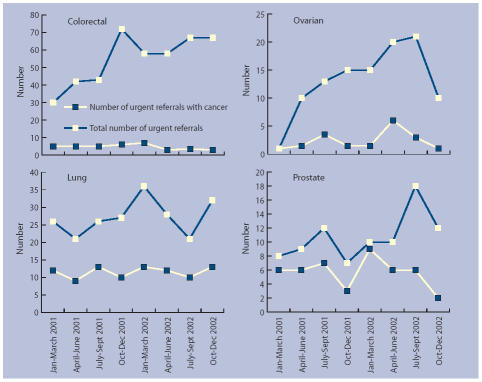
Figure 2 shows the number of urgent referrals over time and the number of those patients who were diagnosed with cancer. This clearly shows that the number of referrals for suspected lung and prostate cancer remained fairly constant, but with some quarterly variation. For colorectal and ovarian cancer, there was a steady increase in the number of referrals over time. The number of urgent referrals diagnosed with all four cancers remained fairly constant, again with some quarterly variation. Hence, overall, the proportion of urgent referrals that were diagnosed with cancer over the 2-year period fell over time.
Figure 2.
Number of urgent referrals and number of urgent referrals with cancer, by cancer diagnosis and quarter.
Fulfilment of urgent referral criteria
Colorectal
Eighty per cent of patients who were urgently referred fulfilled the criteria for urgent referral (Table 2). There was a non-significant difference between cancer and non-cancer patients, with 92% of cancer patients fulfilling the criteria, compared with 79% of the non-cancer patients (Fisher's Exact, P = 0.024). Two-thirds of the non-urgent cancer patients also fulfilled the criteria.
Table 2.
Fulfilment of referral guidance.
| Urgent referral with cancer n (%) | Urgent referral without cancer n (%) | Non-urgent cancer n (%) | |
|---|---|---|---|
| Colorectal | 51 | 393 | 185 |
| Guidance fulfilled? | 47(92) | 309(79) | 125(68) |
| Specific criteria: (each patient may fulfil none or any number) | |||
| • A definite palpable right sided abdominal mass | 14 (28) | 53 (14) | 14 (8) |
| • A definite palpable rectal (not pelvic) mass | 13 (26) | 37 (9) | 11 (6) |
| • Rectal bleeding with a change in bowel habit to looser stools and/or increased frequency of defecation persistent for 6 weeks | 15 (29) | 101 (26) | 22 (12) |
| • Rectal bleeding persistently without anal symptoms and >60 years old | 15 (29) | 76 (19) | 52 (28) |
| • Change in bowel habit to looser stools and/or increased frequency without rectal bleeding and persistent for 6 weeks and >60 years old | 13 (26) | 96 (24) | 18 (10) |
| • Iron deficiency anaemia | 9 (18) | 43 (12) | 47 (25) |
| Lung | 76 | 107 | 170 |
| Guidance fulfilled? | 72 (95) | 99 (93) | 128 (75) |
| Specific criteria: (each patient may fulfil none or any number) | |||
| • Chest X-ray | 71 (93) | 95 (89) | 126 (74) |
| • Persistent haemoptysis | 8 (11) | 10 (9) | 12 (7) |
| • Superior vena cava obstruction | 0 (0) | 0 (0) | 0 (0) |
| • Stridor | 0 (0) | 0 (0) | 0 (0) |
| Ovarian (gynaecological) | 11 | 59 | 31 |
| Guidance fulfilled? | 4 (36) | 37 (63) | 3 (10) |
| Specific criteria: (each patient may fulfil none or any number) | |||
| • Bleeding — intermenstrual | 0 (0) | 1 (1) | 2 (6) |
| • Bleeding — postcoital | 0 (0) | 0 (0) | 0 (0) |
| • Bleeding — postmenopausal | 2 (18) | 10 (17) | 3 (10) |
| • Abdominal symptoms | 7 (64) | 35 (59) | 15 (48) |
| • Abdominal mass | 4 (36) | 13 (22) | 3 (10) |
| • Pelvic mass | 4 (36) | 37 (63) | 3 (10) |
| Prostate (urological) | 44 | 45 | 92 |
| Guidance fulfilled? | 19 (43) | 4 (9) | 5 (5) |
| Specific criteria: (each patient may fulfil none or any number) | |||
| • Macroscopic haematuria | 5 (5) | 1 (2) | 5 (5) |
| • Loin pain | 1 (1) | 4 (9) | 1 (1) |
| • Testicular swelling | 1 (1) | 1 (2) | 1 (1) |
| • Bone pain | 1 (1) | 5 (11) | 1 (1) |
| • Lower urinary tract symptoms | 56 (61) | 30 (67) | 56 (61) |
| • Renal mass | 0 (0) | 0 (0) | 0 (0) |
| • Swelling in body of testis | 0 (0) | 0 (0) | 0 (0) |
| • Prostate feels malignant on rectal examination | 9 (10) | 19 (42) | 9 (10) |
| • Microscopic haematuria | 9 (10) | 3 (7) | 9 (10) |
| • Mass detected on imaging | 1 (1) | 0 (0) | 1 (1) |
| • PSA>20 ng/ml | 31 (76) | 6 (21) | 19 (21) |
Lung
Ninety-two per cent of patients who were urgently referred fulfilled the criteria for urgent referral. There was no significant difference between the cancer (95%) and non-cancer patients (93%). Of those who fulfilled the guidance, the majority satisfied only one of the guidance criteria, with a chest X-ray suggestive of cancer being the most used referral criteria. Three-quarters of the non-urgent cancer patients also fulfilled the criteria.
Ovarian
Fifty-nine per cent of patients who were referred urgently fulfilled the criteria for pelvic mass. There was a difference between the patients with and without cancer, with a third of the cancer patients having a pelvic mass, compared to two-thirds of the non-cancer patients (not significant, Fisher's Exact, P = 0.181). One-tenth of the non-urgent cancer patients also fulfilled the criteria for pelvic mass. Other symptoms recorded on the referral form included: postmenopausal bleeding (17% of the patients without cancer, and 18% of cancer patients); abdominal symptoms (60% of the urgently referred patients); and abdominal mass (24% of the urgently referred patients).
Prostate
From the form it was difficult to determine what an appropriate referral should be for suspected prostate cancer. Table 2 show the individual signs and symptoms that patients were referred for. Almost half of the urgently referred cancer patients were referred for ‘prostate feels malignant on rectal examination’, compared to a quarter of the non-cancer patients. Three-quarters of the urgently referred cancer patients were referred with a PSA>20 ng/ml, compared to one-fifth of the non-cancer patients. One-third had lower urinary tract symptoms. For the non-urgent cancer patients, one-tenth had a prostate that felt malignant on rectal examination, and one-fifth were referred with a PSA>20 ng/ml. One-third had lower urinary tract symptoms. Almost one-half of the urgently referred cancer patients fulfilled the criteria ‘A high PSA in men with a clinically malignant prostate or bone pain’, compared to one-tenth of the non-cancer patients. For the non-urgent cancer patients, one-twentieth satisfied this criteria.
DISCUSSION
Summary of main findings
The diagnostic yield from the urgent referral guidelines varied between cancers, ranging from one in 10 (colorectal cancer), to one in two (prostate cancer) of patients who were urgently referred and subsequently diagnosed with cancer. The proportion of patients with cancer who were urgently referred also varied between cancers, from one in five (colorectal cancer), to one in three (prostate cancer). Of those patients referred urgently, older patients were more likely to have a cancer diagnosis for colorectal, lung and ovarian cancer. This was largely expected given the age related incidence. Less clear is why females were less likely to be diagnosed with colorectal cancer than males. No other associations between sociodemographic factors were found, demonstrating the absence of systematic biases in the assessment and selection of patients for urgent or non-urgent referral.
The total number of urgent referrals, over time, remained fairly constant for lung and prostate cancer, but showed an increase for colorectal and ovarian cancer. Most notably, the number of cancers diagnosed from the urgent referrals remained fairly constant, especially for colorectal cancer, despite the increase in the number of referrals. Potential explanations for this finding include greater implementation of the guidance over time (although not borne out by a corresponding increase in cancer diagnoses), an increase in total referrals caused by GPs ‘gaming’ the system by referring patients in order to get them seen within 2 weeks, and GPs being anxious at missing diagnoses.17 As a result of this, the proportion of urgent referrals diagnosed with cancer fell over the time period resulting in greater workload for fewer cancer diagnoses. A significant knock-on effect on non-urgent outpatient clinics (from where the majority of patients were diagnosed) seems likely as a result. Perversely, overall diagnostic waiting times may therefore be longer as a result of the urgent cancer guidance. Research is needed to explore this. A significant majority of patients who were not urgently referred did indeed fulfil the referral criteria. More widespread use of the referral guidance may therefore lead to higher cancer diagnostic yields, especially for colorectal and lung cancer.
Comparison with existing literature
Limited research has been undertaken looking at effectiveness of the guidelines;4 much of what has been done has been in breast cancer, and shows that the guidance is working to some extent.18 Our findings suggest that while a number of patients are subsequently diagnosed with cancer, there is a significant proportion who are not, confirming the lack of an evidence base regarding the predictive value of signs and symptoms used in the urgent referral guidance. The findings from this study are similar to other studies in terms of the proportion of patients diagnosed with colorectal cancer, who were an urgent referral,7,8 and the diagnostic yield of cancer from patients urgently referred for suspected cancer.10,13 These findings confirm the acknowledged poor evidence base for the predictive values of symptoms and signs in prostate, colorectal and lung cancer.19–21
Strengths and limitations of the study
The main strengths of this study are that it is the first large UK study to link symptoms, referral pathways and cancer outcomes in this important area for policy and clinical practice, and its rigorous records-based data collection.
While the study was only conducted within one NHS trust we are not aware of any reason why this trust should differ significantly from others. We acknowledge that there are methodological limitations when undertaking retrospective data collection, especially where there are missing data. Across all the groups, the notes of 66% of the patients were investigated. The remaining notes were unavailable, despite considerable effort to trace them. This does introduce a potential bias in that those patients whose notes were unavailable may have differed in some way (for example, more likelihood of a cancer diagnosis) than those whose notes we traced. However, we did conduct a sensitivity analysis, working out the crude rates of cancer diagnosis in the four cancers from the data, prior to searching for records, before there were cleaned; this showed very similar proportions to those presented in this paper, suggesting the bias caused by missing data may be minimal (details available from the authors).
We specifically chose to define urgent referrals as those made through the dedicated fast-track system, and not to include referral letters that were marked as ‘urgent’ within this group. Had we done so, the results may have differed but would not have been a reflection of the effectiveness of the urgent cancer referral guidance, which was the main aim of this work. The data regarding marital status were limited for four groups only and made no allowance for patients who were cohabiting or separated; this was outside our control. We acknowledge that the process of documenting presenting symptoms from different sources and at different time points is somewhat imprecise, but would argue that these data still provide valid information regarding compliance with the guidance.
Implications for policy, clinical practice and future research
The predictive power of the referral guidelines as a marker for cancer diagnosis is low, resulting in significant numbers of patients who are urgently referred but do not have cancer. This has implications for patients (potentially causing unnecessary worry), on the hospital diagnostic systems (pressure on clinics and diagnostics), and for those patients presenting through other pathways (potential for later stage diagnosis).
Current efforts to improve cancer outcomes are, in many cases, seeking small improvements from several different interventions. It is therefore unsurprising that the urgent referral system alone has not been shown to be the answer. Recently published data have shown that the urgent referral guidance has made little difference to the proportion of cases selected for urgent referral,22 and that there is nationally a wide variation in compliance with the guidelines.23 Our data suggest that educational initiatives to improve GPs' compliance and use of the guidance may be of questionable benefit, since the proportion of urgent referrals for some cancers has fallen over time. However, the overall programme of improvement in the patient experience does require a healthcare system that is prompt, efficient and effective in diagnosing and treating potentially curable disease. Efforts must continue throughout the NHS, and working with the public, to increase awareness of suspicious symptoms and ensure that the NHS is able to respond in a prompt and effective manner. Patient and primary care delays in cancer diagnosis account for more delay than referral delay;24,25 interventions aimed at reducing such delays may therefore be more likely to lead to earlier stage diagnosis and improved morbidity and mortality. GPs, however, do play a significant role in the diagnosis of cancer,26 and it is therefore appropriate that attention continues to focus on referral delay, although many patients do present with vague and atypical presentations. There remains a danger that if referral thresholds for suspected cancer are lowered, there may be a significant increase in referral rates for many non-malignant conditions.
Further analysis of the data collected for this study will focus on delays in diagnosis, stage at diagnosis, and survival from different referral sources. Future research efforts need to concentrate on the effect of the urgent referral guidance on waiting times for all patients, on the predictive value of signs symptoms, on the implementation of the guidance, and on the effect of the revised guidance that has now been issued.5 This will inform the appropriate application and future development of the guidelines.
Acknowledgments
Thanks go to staff at the Bradford Hospitals NHS Trust medical records library, who were highly cooperative in helping us locate the notes of patients in the study. We would also like to thank: Kath Nuttall, Gillian Hollingsworth and Helena Berry from the Bradford Royal Infirmary, who were supportive in helping set up the project in the early stages, for supplying the initial patient data, and continued feedback on the findings throughout the data collection. We are also grateful to all the members of the advisory group for their invaluable comments: Chris Bradley, Gillian Hollingsworth, Kath Nuttall, Andrew O'Shaughnessy, Joan Stone and John Sullivan.
Funding body
The study was funded by Bradford primary care trusts
Ethics committee
Research ethics approval was received from Bradford Hospitals NHS Trust Local Research Ethics Committee (03/02/297)
Competing interests
The authors have stated that there are none
REFERENCES
- 1.NHS Executive. The New NHS modern and dependable: a national framework for assessing performance. London: 1998. [Google Scholar]
- 2.Department of Health. Referral guidelines for suspected cancer. London: Department of Health; 2000. [Google Scholar]
- 3.Department of Health. The NHS cancer plan. London: Department of Health; 2000. [Google Scholar]
- 4.Jones R, Rubin G, Hungin P. Is the two week rule for cancer referrals working? BMJ. 2001;322:1555–1556. doi: 10.1136/bmj.322.7302.1555. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.National Institute for Health and Clinical Excellence. Referral guidelines for suspected cancer. Clinical guideline 27. London: National Institute for Health and Clinical Excellence; 2005. [Google Scholar]
- 6.Mulka O. NICE suspected cancer guidelines. Br J Gen Pract. 2005;55:580–581. [PMC free article] [PubMed] [Google Scholar]
- 7.Flashman K, O'Leary DP, Senapati A, Thompson MR. The Department of Health's ‘two week standard’ for bowel cancer: is it working? Gut. 2004;53:387–391. doi: 10.1136/gut.2003.020503. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Eccersley AJ, Wilson EM, Makris A, Novell JR. Referral guidelines for colorectal cancer — do they work? Ann R Coll Surg Engl. 2003;85:107–110. doi: 10.1308/003588403321219885. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kiran PR, Glass RE. Duration of symptoms and spread of colorectal cancer: a short history does not mean early disease. Ann R Coll Surg Eng. 2002;84:381–385. doi: 10.1308/003588402760978157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Martin JP, Gabe SM, Pitcher MC, Jacyna MR. Referral patterns to a district general hospital gastroenterology outpatient clinic: implications for the ‘two-week target’. Int J Clin Pract. 2002;56:26–28. [PubMed] [Google Scholar]
- 11.Davies RJ, Welboune R, Collins C, et al. A prospective study to assess the implementation of a fast track system to meet the two week target for colorectal cancer. Gut. 2001;48:A53. doi: 10.1046/j.1463-1318.2002.00289.x. [DOI] [PubMed] [Google Scholar]
- 12.Moreea S, Green J, MacFie J, Mitchell CJ. Impact of the two week waiting time standard on the gastroenterology service of a district general hospital. Gut. 2001;48:A3. [Google Scholar]
- 13.Debnath D, Dielehner N, Gunning KA. Guidelines, compliance, and effectiveness: a 12 months' audit in an acute district general healthcare trust on the two week rule for suspected colorectal cancer. Postgraduate Med J. 2002;78:748–751. doi: 10.1136/pmj.78.926.748. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Boulton-Jones JR, Gamble S, Robinson MH, et al. The impact of the two-week wait scheme for suspected gastrointestinal cancers. Clin Med. 2003;3:483–484. doi: 10.7861/clinmedicine.3-5-483a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Allen D, Popert R, O'Brien T. The two-week-wait cancer initiative in urology: useful modernization? J R Soc Med. 2004;97:279–281. doi: 10.1258/jrsm.97.6.279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Coxon JP, Harris HJ, Watkin NA. A prospective audit of the implementation of the 2-week rule for assessment of suspected urological cancers. Ann R Coll Surg Engl. 2003;85:347–350. doi: 10.1308/003588403769162486. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Cornford CS, Harley J, Oswald N. The ‘2-week rule’ for suspected breast carcinoma: a qualitative study of the views of patients and professionals. Br J Gen Pract. 2004;54:584–588. [PMC free article] [PubMed] [Google Scholar]
- 18.Allgar VL, Neal RD, Pascoe SW. Grading referrals to specialist breast units: guidance on referral needs to be evidence based. BMJ. 2002;325:392. [PMC free article] [PubMed] [Google Scholar]
- 19.Hamilton W, Sharp D. Symptomatic diagnosis of prostate cancer in primary care: a structured review. Br J Gen Pract. 2004;54:617–621. [PMC free article] [PubMed] [Google Scholar]
- 20.Hamilton W, Sharp D. Diagnosis of lung cancer in primary care: a structured review. Fam Pract. 2004;21:605–611. doi: 10.1093/fampra/cmh605. [DOI] [PubMed] [Google Scholar]
- 21.Hamilton W, Sharp D. Diagnosis of colorectal cancer in primary care: the evidence base for guidelines. Fam Pract. 2004;21:99–106. doi: 10.1093/fampra/cmh121. [DOI] [PubMed] [Google Scholar]
- 22.Jiwa M, Hamilton W. Referral of suspected colorectal cancer: have guidelines made a difference? Br J Gen Pract. 2004;54:608–610. [PMC free article] [PubMed] [Google Scholar]
- 23.Lewis R, Collins R, Flynn A, et al. A systematic review of cancer waiting time audits. Qual Saf Health Care. 2005;14:62–66. doi: 10.1136/qshc.2004.013359. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Allgar VL, Neal RD. Delays in the diagnosis of six cancers: analysis of data from the National Survey of NHS Patients: Cancer. Br J Cancer. 2005;92:1959–1970. doi: 10.1038/sj.bjc.6602587. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Neal RD, Allgar VL. Sociodemographic factors and delays in the diagnosis of six cancers: analysis of data from the ‘National Survey of NHS Patients: Cancer’. Br J Cancer. 2005;92:1971–1975. doi: 10.1038/sj.bjc.6602623. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Allgar VL, Neal RD. General practitioners' management of cancer: secondary analysis of data from the National Survey of NHS Patients: Cancer. Eur J Cancer Care. 2005;14:409–416. doi: 10.1111/j.1365-2354.2005.00600.x. [DOI] [PubMed] [Google Scholar]