Abstract
OBJECTIVES--To estimate the cost effectiveness of giving prophylactic antibiotics routinely to reduce the incidence of wound infection after caesarean section. DESIGN--Estimation of cost effectiveness was based, firstly, on a retrospective overview of 58 controlled trials and, secondly, on evidence about costs derived from data and observations of practice. SETTING--Trials included in the overview were from obstetric units in several different countries, including the United Kingdom. The costing study was based on data referring to the John Radcliffe Maternity Hospital, Oxford. SUBJECTS--A total of 7777 women were included in the 58 controlled trials comparing the effects of giving routine prophylactic antibiotics at caesarean section with either treatment with a placebo or no treatment. Cost estimates were based on data on 486 women who had caesarean sections between January and September 1987. MAIN OUTCOME MEASURE--Cost effectiveness of prophylaxis with antibiotics. RESULTS--The odds of wound infection are likely to be reduced by between about 50 and 70% by giving antibiotics routinely at caesarean section. Forty one (8.4%) women who had caesarean section were coded by the Oxford obstetric data system as having developed wound infection. The additional average cost of hospital postnatal care for women with wound infection (compared with women who had had caesarean section and no wound infection) was estimated to be 716 pounds; introducing routine prophylaxis with antibiotics would reduce average costs of postnatal care by between 1300 pounds and 3900/100 pounds caesarean sections (at 1988 prices), depending on the cost of the antibiotic used and its effectiveness. CONCLUSIONS--The results suggest that giving antibiotics routinely at caesarean section will not only reduce rates of infection after caesarean section but also reduce costs.
Full text
PDF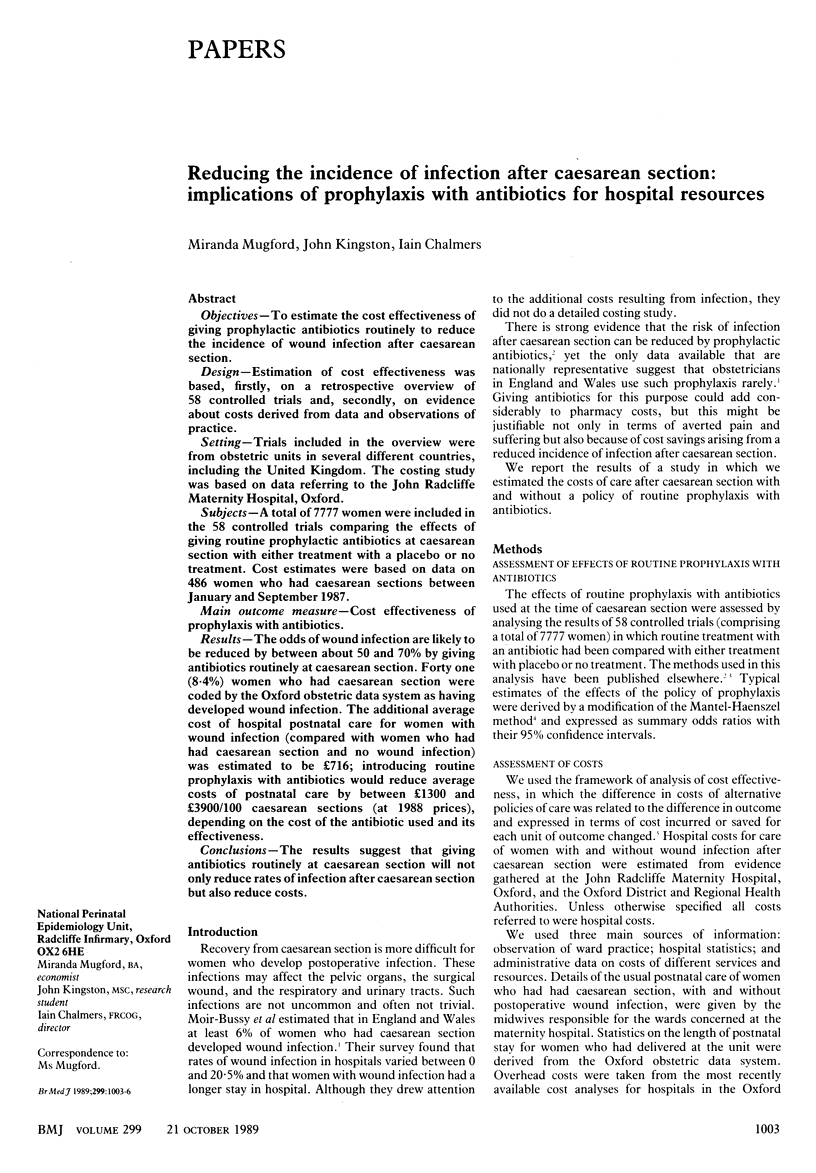


Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Davey P. G., Duncan I. D., Edward D., Scott A. C. Cost-benefit analysis of cephradine and mezlocillin prophylaxis for abdominal and vaginal hysterectomy. Br J Obstet Gynaecol. 1988 Nov;95(11):1170–1177. doi: 10.1111/j.1471-0528.1988.tb06796.x. [DOI] [PubMed] [Google Scholar]
- Mead P. B. Prophylactic antibiotics and antibiotic resistance. Semin Perinatol. 1977 Jan;1(1):101–111. [PubMed] [Google Scholar]
- Moir-Bussy B. R., Hutton R. M., Thompson J. R. Wound infection after caesarean section. J Hosp Infect. 1984 Dec;5(4):359–370. doi: 10.1016/0195-6701(84)90003-3. [DOI] [PubMed] [Google Scholar]
- Pelle H., Jepsen O. B., Larsen S. O., Bo J., Christensen F., Dreisler A., Jørgensen P. J., Kirstein A., Kjøller M., Lange A. Wound infection after cesarean section. Infect Control. 1986 Sep;7(9):456–461. doi: 10.1017/s019594170006495x. [DOI] [PubMed] [Google Scholar]
- Pollock A. V. Surgical prophylaxis--the emerging picture. Lancet. 1988 Jan 30;1(8579):225–230. doi: 10.1016/s0140-6736(88)91074-4. [DOI] [PubMed] [Google Scholar]
- Tullus K., Burman L. G. Ecological impact of ampicillin and cefuroxime in neonatal units. Lancet. 1989 Jun 24;1(8652):1405–1407. doi: 10.1016/s0140-6736(89)90122-0. [DOI] [PubMed] [Google Scholar]
- Webster J. Post-caesarean wound infection: a review of the risk factors. Aust N Z J Obstet Gynaecol. 1988 Aug;28(3):201–207. doi: 10.1111/j.1479-828x.1988.tb01664.x. [DOI] [PubMed] [Google Scholar]


