Abstract
Background
Antidepressant prescribing in general practice has dramatically increased since the beginning of the last decade.
Aim
To determine if the increase in antidepressants prescribed in Scotland between 1995 and 2001 was due to increase in incidence, prevalence, care-seeking behaviour by patients, or identification by GPs of depression.
Method
Secondary analysis of routine data. Prescribing information was obtained from Information and Statistics Division Scotland, psychosocial morbidity from the Scottish Health Surveys of 1995 and 1998 and GP consultations from the continuous morbidity recording (CMR) dataset. Annual trends in antidepressant prescribing for prescriptions, gross ingredient cost and defined daily doses (DDDs) were examined for all Scottish Practices and 54 stable CMR practices (175 955 patients). Prevalence of psychological morbidity in responders with a General Health Questionnaire score ≥4, their contact probability and contact frequency was compared in the 1995 and 1998 Scottish Health Surveys. Changes in diagnostic and GP consultation patterns in CMR practices were compared.
Results
Total prescriptions for antidepressants increased from 1.5 million in 1995–1996 to 2.8.million in 2000–2001. The gross ingredient cost increased from £20 to £44 million and total DDDs from 44.5 to 93.2 million. Prescription trends in CMR practices were similar. Overall prevalence of psychological morbidity was the same in the 1995 and 1998 Scottish Health Surveys. Percentage of consultations in CMR practices for new diagnoses of depression decreased from 1.7 to 1.3%, the depression-related contact rate decreased and annual prevalence rates for depressive illness were stable between 1998–1999 and 2000–2001.
Conclusions
There is no evidence of an increase in incidence, prevalence, care-seeking behaviour or identification of depression during the period of a sharp increase in antidepressant prescribing. Further work is required to explain the increase.
Keywords: depression, drugs, health services, mental health, primary care
INTRODUCTION
Antidepressant prescribing rapidly changed during the 1990s in Scotland.1 Over the period 1992 to 2001 the number of prescriptions for antidepressants dispensed in the community in Scotland increased from 1.2 to 2.8 million per year and they accounted for £44.5 million of the £60.6 million spent on mental health drugs in the 1999–2000 financial year.
The reasons for this dramatic increase in antidepressant prescribing are not clear. In speculating about the causes for any increase in prescribing levels, it is reasonable to start by looking at the possibility that the main condition that the drugs are commonly used to treat has increased, either in incidence or prevalence. Alternatively, patients may be presenting with the problem more or GPs may be diagnosing the condition more.
This study aimed to investigate these potential explanations using a range of secondary data.
METHOD
Sources of data
Data on prescribing were taken from the prescribing information system maintained by the Healthcare Information Group at Information Services (NHS National Services Scotland). The information relates to prescriptions dispensed in the community by pharmacists, dispensing doctors and appliance suppliers. The vast majority of these prescriptions are written by GPs. The data include a small number of prescriptions written in the UK outside Scotland but dispensed in Scotland. Prescriptions written in Scotland but dispensed outside Scotland are excluded, as are private prescriptions.
Data were extracted for five financial years, April 1995–March 1996 through to April 2000–March 2001. Each prescription was classified based on the therapeutic groupings used in the British National Formulary (BNF). All drugs in BNF section 4.3 were included.2 This section includes: 4.3.1 tricyclic and related antidepressant drugs; 4.3.2 monoamine oxidase inhibitors; 4.3.3 selective serotonin re-uptake inhibitors; 4.3.4 other antidepressant drugs. The amount of prescribing was measured in three ways: the number of prescribed items, the gross ingredient cost and defined daily doses (DDDs). The gross ingredient cost is the cost of an item excluding discounts, dispensing costs or fees, and fees paid by the recipient. The DDD is a system developed and maintained by the World Health Organisation.3 Each drug is given a value that represents the assumed average maintenance dose per day for a drug used for its main indication in adults. Using this measurement enables the true volume of a drug prescribed to be compared at different time points across the world.
Prescribing information was extracted by prescriber and linked to general practices using prescriber-practice lookup files. The information relates to prescribers rather than patients so that prescriptions written by prescribers that are not partners at particular practices (for example, out-of-hours cover, locums and GP registrars) are not attributed to practices.
Data were also obtained from two waves of the Scottish Health Survey, undertaken in 19954 and 1998.5 The Scottish Health Survey is a representative survey of individuals living in private households. In both surveys psychological morbidity was measured using the 12-item General Health Questionnaire (GHQ-12).6 An overall GHQ-12 score of four or more has been used to identify informants with a potential psychiatric disorder. This instrument was only applied to responders aged 16–74 years in 1998. Responders were also asked how many times they had seen a GP in the last fortnight.
Data on GP consultations were also obtained from the Continuous Morbidity Recording (CMR) dataset.7 This dataset collects information on every face-to-face doctor–patient contact for a sample of Scottish practices. Every doctor is asked to describe the problem in as specific diagnostic terms as possible. They can record up to 10 problems for each contact. Each diagnosis is given a Read code8 along with an appropriate modifier to specify whether it is the first contact, a persistent condition or a recurrent condition.
Analysis was restricted to data from 175 995 patients that had been registered with one of 54 practices in September 1999, 2000 and 2001 and had had at least one contact in the period April 1998–March 2001. The 54 practices had been continuously part of the CMR scheme from April 1998 to March 2001 and had returned consistent levels of activity throughout the period. Depression-related contacts were identified using Read codes (the selected Read codes are available in Supplementary Appendix 1).
Population figures were also used for some of the analysis. The new Scottish-level mid-year estimates from the General Registrar's Office for Scotland, which have been rebased to take account of the more accurate population counts produced by the 2001 census, were included.
Analysis
Annual trends in antidepressant prescribing were studied by looking at numbers of prescriptions, gross ingredient cost and DDDs for all Scottish practices and for the 54 practices in the CMR dataset. The trends in each variable were indexed to a value of 100 in the base year (1995–1996). DDDs for the four BNF drug groups were analysed further.
To investigate changes in the prevalence of psychological morbidity, the percentages of responders with a GHQ-12 score ≥4, were compared by age and sex in the 1995 and 1998 Scottish Health Surveys. Comparisons were restricted to the age bands covered in both surveys (16–64 years). The potential role of changes in the size and demographic composition of the Scottish population was considered by applying the 1998 prevalence rates to the population figures at the start (1995) and end (2000) of our study period.
Changes in the propensity of the population to seek care from GPs were considered using contact information from the Scottish Health Surveys. Each of the waves of the surveys were divided into responders with and without psychological caseness using GHQ-12 scores. The proportions of each group that had at least one GP contact in the last fortnight (contact probability) and the average number of visits for those with at least one GP visit (contact frequency) were compared. This distinction has been used in previous studies to make an approximate differentiation between patient-initiated and doctor-initiated contacts.9 By comparing figures from these 2 years, any changes in frequency of care-seeking can be determined.
How this fits in
Antidepressant prescribing has been increasing rapidly in the UK since the beginning of the 1990s. The increase cannot be explained by an increase in the incidence or prevalence of depression. There is no evidence that people are presenting more frequently with depression to their GP or that GPs are making a diagnosis of depression more frequently. There is a need to explore other causes for the increase in antidepressant prescribing by GPs.
To examine changes in diagnosis and patterns of GP consultation in the CMR practices, mean numbers of contacts were analysed by year of contact and year of first diagnosis of depression. This permitted comparisons of numbers of contacts in the first year of diagnosis across 3 years (1998–1999, 1999–2000 and 2000–2001) and the year following diagnosis across 2 years (1999–2000 and 2000–2001). We analysed average contacts for all diagnoses and contacts in which a diagnosis of depression was recorded. We compared the all-cause contact rate with that for the group with no diagnosis of depression throughout the study period to benchmark the trends against the population's GP contact rate. Depression related contact rates were analysed to assess whether the contact rate changed for incident cases and whether there were changes in follow-up care following first diagnosis.
The data analysis was carried out using STATA version 7.0.
RESULTS
Trends in volume of prescribing
The total number of prescriptions for antidepressants increased from 1.5 million in year 1995–1996 to 2.8 million in year 2000–2001 (Table 1). The gross ingredient cost increased from £20 to £44 million and the DDDs also increased from 44.5 to 93.2 million. Comparing the index figures with the base year (1995–1996) the antidepressant prescribing gross ingredient cost increased for the first 5 years and then started showing a slight decrease in 2000–2001.
Table 1.
Trends in antidepressant prescribing for Scotland and for 54 CMR practices.
| Prescriptions | Gross ingredient cost | Defined daily doses | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Scotland | CMR practices | Scotland | CMR practices | Scotland | CMR practices | ||||||||
| Scotland Population 30 June | n | Index (95/6 = 100) | n | Index (95/6 = 100) | n | Index (95/6 = 100) | n | Index (95/6 = 100) | n | Index (95/6 = 100) | n | Index (95/6 = 100) | |
| 1995–1996 | 5 103 690 | 1 547 915 | 100 | 88 395 | 100 | 20 726 983 | 100 | 1 121 306 | 100 | 44 555 090 | 100 | 2 499 875 | 100 |
| 1996–1997 | 5 092 190 | 1 804 435 | 116.57 | 102 261 | 115.69 | 27 567 208 | 133.00 | 1 496 358 | 133.45 | 54 335 830 | 121.95 | 3 052 754 | 122.12 |
| 1997–1998 | 5 083 340 | 2 103 400 | 135.89 | 118 324 | 133.86 | 34 880 820 | 168.29 | 1 872 123 | 166.96 | 65 073 284 | 146.05 | 3 620 928 | 144.84 |
| 1998–1999 | 5 077 070 | 2 319 384 | 149.84 | 125 275 | 141.72 | 40 101 163 | 193.47 | 2 083 142 | 185.78 | 72 910 782 | 163.64 | 3 919 425 | 156.78 |
| 1999–2000 | 5 071 950 | 2 541 691 | 164.20 | 141 809 | 160.43 | 44 633 684 | 215.34 | 2 411 555 | 215.07 | 82 653 450 | 185.51 | 4 609 649 | 184.40 |
| 2000–2001 | 5 062 940 | 2 768 190 | 178.83 | 155 932 | 176.40 | 44 096 952 | 212.75 | 2 389 188 | 213.07 | 93 209 951 | 209.20 | 5 225 203 | 209.02 |
GRO mid-population estimates. CMR = continuous morbidity recording.
The prescription trends for CMR practices demonstrated a very similar pattern to the whole of Scotland (Table 1). Prescribing by these 54 practices accounted for about 5% of the total volume of prescribing for Scotland. To determine whether the increase in antidepressant prescribing was due to an increase in the practice population, the practices' list sizes were compared at the beginning and at the end of the 3-year period. In three cases, the practice populations changed because they merged with other practices, although overall the population only decreased by 0.1%.
Trends in prescribing by BNF drug groups
DDDs of selective serotonin reuptake inhibitors (SSRIs) increased by 171% from 1995–1996 to 2000–2001 (Table 2). DDDs of tricyclic antidepressants increased by 14% and monoamine oxidase inhibitors decreased by 18%. The DDDs of ‘other antidepressants’ increased mainly due to new drugs such as venlafaxine and mirtazapine coming onto the market. Venlafaxine was originally included in the SSRI section of the BNF but it was placed in the ‘other antidepressant’ section in 2000–2001. In order to make comparisons, it was classified in ‘other antidepressants’ throughout this study.
Table 2.
Defined daily doses trends by British National Formulary groups.
| Tricyclics | Monoamine oxidase inhibitors | SSRIs | Others | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Year | Scotland Population 30 June | DDDs | Index (1995–1996 = 100) | DDDs | Index (1995–1996 = 100) | DDDs | Index (1995–1996 = 100) | DDDs | Index (1995–1996=100) |
| 1995/1996 | 5 103 690 | 22 559 280 | 100 | 630 133 | 100 | 21 258 796 | 100 | 106 874 | 100 |
| 1996/1997 | 5 092 190 | 23 702 350 | 105.07 | 627 300 | 99.55 | 29 899 071 | 140.64 | 107 101 | 100.21 |
| 1997/1998 | 5 083 340 | 25 480 270 | 112.95 | 640 197 | 101.60 | 38 726 741 | 182.17 | 226 075 | 211.53 |
| 1998/1999 | 5 077 070 | 26 065 480 | 115.54 | 584 354 | 92.74 | 41 020 207 | 192.96 | 5 240 741 | 4903.68 |
| 1999/2000 | 5 071 950 | 26 044 424 | 115.45 | 532 847 | 84.56 | 49 096 252 | 230.95 | 6 979 926 | 6531.01 |
| 2000/2001 | 5 062 940 | 25 917 347 | 114.89 | 521 659 | 82.79 | 57 618 447 | 271.03 | 9 152 498 | 8563.85 |
DDD = defined daily dose. SSRI = selective serotonin reuptake inhibitor.
Trends in GHQ-12 caseness from the Scottish Health Surveys
The overall prevalence of reported potential psychological morbidity was slightly decreased in the 1998 Scottish Health Survey compared with the 1995 survey (Table 3) but the difference was not statistically significant (P-value = 0.86).
Table 3.
Prevalence of GHQ–12 >4 in the 1995 and 1998 Scottish Health Surveys.
| Percentage (n) | ||||
|---|---|---|---|---|
| 1995 | 1998 | |||
| Age (years) | Men | Women | Men | Women |
| 16–24 | 10 (709) | 16 (684) | 9 (702) | 17 (672) |
| 25–34 | 12 (962) | 22 (975) | 12 (939) | 18 (935) |
| 35–44 | 12 (834) | 19 (854) | 13 (894) | 19 (902) |
| 45–54 | 17 (737) | 22 (768) | 12 (766) | 20 (795) |
| 55–64 | 17 (583) | 16 (645) | 20 (599) | 19 (651) |
| Overall prevalence (95%CI) | 0.02 (0.02 to 0.03) | 0.02 (0.01 to 0.03) | ||
Trends in reported GP contact in Scottish Health Surveys
People scoring ≥4 on the GHQ-12 were twice as likely to have seen their GP in the previous 2 weeks than people scoring <4 but these figures did not change between 1995 and 1998. The average number of visits in the last fortnight for those with at least one visit by people with a GHQ-12 score of ≥4 was 1.38. The same number of visits for those with a score <4 was 1.17. None of these averages were significantly different in 1998.
The percentage of consultations in CMR practices for a new diagnosis of depression decreased from 1.7% in 1998/9 to 1.3% in 2000–2001.
The GP contact rate for all patients for all conditions increased from 1998–1999 to 2000–2001 Table 4). However, the depression-related contact rate decreased in the same period. The contact rates for all-causes for those who had a diagnosis of depression was stable. The contact rates for the follow up period after the diagnosis of depression decreased for depression and all-cause related contacts.
Table 4.
Mean GP contact rates for patients with or without a depression diagnosis in 54 CMR practices from April 1998 until 2000.
| GP contacts (95% CI) | ||||
|---|---|---|---|---|
| Diagnosis | 1998–1999 | 1999–2000 | 2000–2001 | |
| In year of first diagnosis of depression for people with depression | All causes | 7.10 (7.08 to 7.12) | 7.13 (7.11 to 7.14) | 7.10 (7.08 to 7.12) |
| Depression | 2.54 (2.53 to 2.55) | 2.45 (2.44 to 2.46) | 2.52 (2.51 to 2.53) | |
| In year after first diagnosis of depression (persistent or recurrent) for people with depression | All causes | 5.73 (5.71 to 5.75) | 5.50 (5.47 to 5.52) | |
| Depression | 1.17 (1.16 to 1.18) | 1.05 (1.04 to 1.06) | ||
| For people with no diagnosis of depression | All causes | 2.65 (2.64 to 2.66) | 2.75 (2.74 to 2.76) | 2.78 (2.77 to 2.80) |
Annual incidence rates for depressive illness per 1000 patients by age and sex according to data collected in the CMR practices did not show any increase between 1998 and 2000 (Figure 1). Comparing the recording of presenting problems of depression in these 54 practices from 1998–2000 with the volume of dispensed daily doses of antidepressants prescribed in them confirms that the recording of new or follow-up contacts for depression did not increase although prescribing of antidepressants increased. The cost of prescriptions for antidepressants rose in line with the volume prescribed between 1998–1999 and 1999–2000 but levelled off between 1999–2000 and 2000–2001 when SSRIs became more readily available as generic prescriptions.
Figure 1.
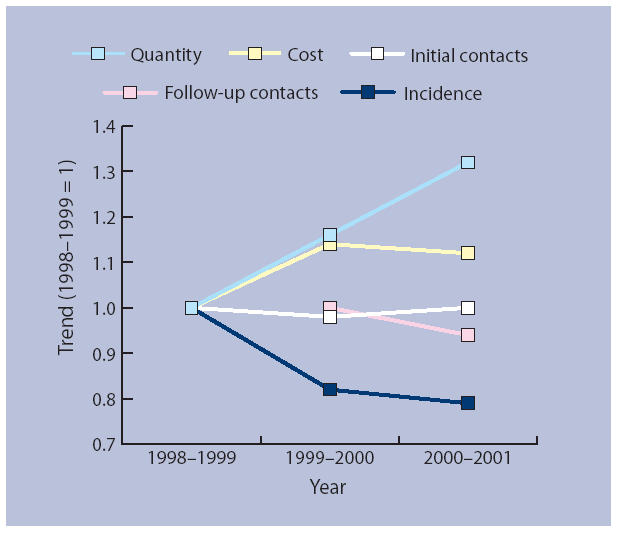
Activity and prescribing in the 54 stable CMR practices.
DISCUSSION
Summary of main findings
The dramatic increase in antidepressant prescribing during the 1990s and into this decade occurred not just in Scotland but across the UK10 and there is no clear evidence of a levelling off in the rate of increase (Prescribing Information Systems for Scotland, unpublished data, 2005).
There was no evidence from the routine data examined in our study to support any of the four potential explanations for the increase in antidepressant prescribing in Scotland that we investigated: there was no evidence of an increase in the incidence or prevalence of depression; people did not present more often to their GPs with symptoms leading to a diagnosis of depression; and GPs did not record more diagnoses of depression.
A Dutch study that looked at national surveys of general practice suggested that there was an increase in mental and social problems in the population between 1987 and 2001 but GPs diagnosed fewer patients as having a mental disorder in 2001 than they did in 1987.11 The authors of this study concluded that the role of primary care has changed in The Netherlands in that, although GPs diagnose a lower percentage of mental problems, they refer an increasingly larger proportion of these to secondary care. We were unable to find any evidence of an increase in depression, nor would we suggest that the role of primary care has changed, in Scotland.
In a recent editorial in this Journal, Kessler and colleagues suggested a range of possible reasons for the increase in antidepressant prescribing.12 These included an effect of the drive by the Royal Colleges of General Practitioners and Psychiatrists in the ‘Defeat Depression Campaign’ to identify and treat more cases of depression. Our study suggests that GPs did not identify more cases of depression but they seem to be treating more cases with antidepressants. Perhaps the ‘Defeat Depression Campaign’ has been a partial success. Kessler and colleagues also suggested that perhaps there is a greater openness about depression and an accompanying willingness to seek help.12 We could not find evidence for this but perhaps people are more willing to ask for, or accept, antidepressants for their symptoms when they do seek help.
Strengths and weaknesses of the study
It is possible that between 1995 and 1998 more people were being treated with antidepressants and their GHQ-12 scores may have improved. These improved scores would have been lost among the population as a whole. If they hadn't been treated with antidepressants, it is conceivable that the true level of GHQ-12 caseness in the population would have increased. It is impossible to know if this happened or the size of this effect. We know that, in the Scottish Health Survey of 1998, 11% of men and 18% of women were using drugs classified in a broad grouping of central nervous system drugs.5 We don't know what proportion of these were antidepressants and we can't estimate how effective these might have been in improving GHQ-12 scores. We would suggest, however, that any reduction in the percentage of the population with a GHQ-12 score of ≥4 due to this effect would be very small.
Some of the sources of data used in this study are more robust than others. Prescribing data are considered to be particularly robust because all prescriptions written by GPs, and dispensed by pharmacists in Scotland, are collected centrally so that the costs to pharmacists can be reimbursed. CMR data are less reliable because their collection depends on individual GP activity although a system of checks and quality control is in place to try to maintain their quality.7 Read codes may not be very stable due to the possibility of individual GP preferences for using particular codes changing over time. Although there were no official changes in Read codes during the period under study, it is possible that there were some minor changes in codes used by GPs in the participating practices. The prevalence figures for GHQ-12 ≥4 are estimates of the percentage of a possible psychiatric disorder at a particular point in time and are useful for making comparisons but they cannot be used for deducing the incidence of psychiatric disorder.6 However, the interrogation of multiple sources of data that all gave the same answers to the study questions suggests that the results are dependable.
Implications for clinical practice and further research
Hollinghurst and colleagues suggested that the recent rise in antidepressant prescribing is likely to be due to increased awareness of depression by patients and professionals; reduced side effects associated with newer antidepressants; and the broadening range of indications for which antidepressants are prescribed, for example, panic disorder.10 We could not find evidence for the first of these suggestions but we agree that it is possible that the threshold for prescribing antidepressants has lowered because newer antidepressants have been promoted as having fewer side effects. In this situation, antidepressant treatment would have been started more frequently although depression would not have been diagnosed more frequently. We also agree that it is likely that some of the increase in prescribing is due to the increased range of indications.
The suggestions discussed here need to be investigated further. There are likely to be multiple reasons for the increase in antidepressant prescribing by GPs and a range of sources of data and evidence need to be investigated. These sources include other routinely available data but we also suggest that further work that asks GPs what influences their prescribing is required. A recent report suggested that GPs who took part in an exploratory study were cautious in their decisions to prescribe antidepressants.13 The authors suggested, however, that their study was potentially limited both by the method used — focus groups — and by the subjects, who were self-selected. Face-to-face interviews with GPs selected on the basis of their level of antidepressant prescribing might help us to understand what is happening in this complex area.
Supplementary Material
Acknowledgments
We are grateful to Daniel Mackay for providing some of the data used in this paper.
Supplementary information
Supplementary information accompanies this paper at http://www.rcgp.org.uk/Default.aspx?page=2482
Funding body
This study was not separately funded, however Rosalia Munoz-Arroyo and Matt Sutton were funded by the Platform Project for some of the period during which this paper was written (SEHHD – CSO OOB/3/67). The Platform Project is a Scottish School of Primary Care collaborative venture between the Universities of Aberdeen, Dundee, Edinburgh and Glasgow, with ISDScotland and the Royal College of General Practitioners. The opinions expressed are those of the authors and not necessarily the funders
Ethics committee
Ethical approval was not required for this study as the data used are routinely available
Competing interests
The authors have stated that there are none
REFERENCES
- 1.Philp AV. Mental health in Scotland: information sources and selected insights. Edinburgh: NHS Scotland Information and Statistics Division; June 2002. http://www.isdscotland.org/isd/files/sources_insights2002.pdf.pdf (accessed 8 May 2006). [Google Scholar]
- 2.British Medical Association and Royal Pharmaceutical Society of Great Britain. British National Formulary. London: British Medical Association and Royal Pharmaceutical Society of Great Britain; 2005. [Google Scholar]
- 3.National Prescribing Centre. http://www.npc.co.uk/publications/prescribingTerms/frames.htm (accessed 12 May 2006)
- 4.Scottish Office Department of Health. The Scottish Health Survey 1995. www.show.scot.nhs.uk/SEHD/publications/sh5/sh5-00.htm (accessed 8 May 2006)
- 5.Scottish Office Department of Health. The Scottish Health Survey 1998. www.show.scot.nhs.uk/scottishhealthsurvey/sh8-00.htm(accessed 8 May 2006)
- 6.Goldberg D. A user's guide to the General Health Questionnaire. Windsor: NFER-NELSON; 1988. [Google Scholar]
- 7.Scottish Health Statistics. General practice — practice team information (PTI) http://www.isdscotland.org/isd/info3.jsp?pContentID=3728&p_applic=ccc&p_service=Contentshow (accessed 8 May 2006)
- 8.Graham L. Read code user guide. http://www.isdscotland.org/isd/files/ReadUserGuideLinked.doc(accessed 8 May 2006)
- 9.Pohlmeier W. An econometric model of the two-part decision making process in the demand for health care. J Hum Resour. 1995;30:339–361. [Google Scholar]
- 10.Hollinghurst S. Opportunity cost of antidepressant prescribing in England: analysis of routine data. BMJ. 2005;330:999–1000. doi: 10.1136/bmj.38377.715799.F7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Verhaak PFM. Mental health in the Dutch population and in general practice: 1987–2001. Br J Gen Pract. 2005;55:770–775. [PMC free article] [PubMed] [Google Scholar]
- 12.Kessler D. Screening for depression in primary care. Br J Gen Pract. 2005;55:659–660. [PMC free article] [PubMed] [Google Scholar]
- 13.Hyde J, et al. A qualitative study exploring how GPs decide to prescribe antidepressants. Br J Gen Pract. 2005;55:755–762. [PMC free article] [PubMed] [Google Scholar]


