Abstract
Background
Motivational interviewing has been shown to be broadly usable in a scientific setting in the management of behavioural problems and diseases. However, data concerning implementation and aspects regarding the use of motivational interviewing in general practice is missing.
Aim
To evaluate GPs' conception of motivational interviewing in terms of methods, adherence to and aspects of its use in general practice after a course.
Study design
In a randomised controlled trial concerning intensive treatment of newly diagnosed patients with type 2 diabetes detected by screening, the GPs were randomised to a course in motivational interviewing or not. The study also included a third group of GPs outside the randomised controlled trial, who had 2 years previously received a similar course in motivational interviewing.
Setting
General practice in Denmark.
Method
The intervention consisted of a 1.5-day residential course in motivational interviewing with 0.5-day follow-ups, twice during the first year. Questionnaire data from GPs were obtained.
Results
We obtained a 100% response-rate from the GPs in all three groups. The GPs trained in motivational interviewing adhered statistically significantly more to the methods than did the control group. More than 95 % of the GPs receiving the course stated that they had used the specific methods in general practice.
Conclusion
A course in motivational interviewing seems to influence GPs professional behaviour. Based on self-reported questionnaires, this study shows that the GPs after a course in motivational interviewing seemed to change their professional behaviour in daily practice using motivational interviewing compared with the control group. GPs evaluated motivational interviewing to be more effective than ‘traditional advice giving’. Furthermore, GPs stated that the method was not more time consuming than ‘traditional advice giving’.
Keywords: client counselling, diabetes, motivational interviewing, psychological interview
INTRODUCTION
The concept of ‘motivational interviewing’ evolved from experience with treatment of alcoholics and was described by Miller in 1983.1 The concept was developed into a coherent theory and a detailed description of the clinical procedures.2 Motivational interviewing has been shown to be broadly usable in a scientific setting in the management of behavioural problems and diseases.3 Hence, the method has been used and evaluated internationally especially in the last decade in relation to the following main areas: addiction (alcohol abuse and addiction to drugs); change in lifestyle (smoking cessation, weight-loss; physical activity; asthma and diabetes treatment), and; adherence (to treatment and to control, encounters of follow-up, counselling meetings).3 The technique has been deployed by various healthcare providers, including psychologists, doctors, nurses and midwives. Controlled trials in general practice have shown that it is an effective strategy in the treatment of different diseases.4–9 However, only very few studies have focused on how to implement and integrate motivational interviewing in professional behaviour in daily work in general practice10,11 and they have concluded that this strategy can be implemented in general practice. In the process of evaluating motivational interviewing on patients with type 2 diabetes, we found a need for evaluating whether the GPs educated and trained in motivational interviewing actually used and adhered to the methods in their clinical work.
The aim of this study was to evaluate how a 1.5-day course in motivational interviewing (including follow-up meetings) influenced GP's professional behaviour, and whether GPs, after a 1.5-day course, found the method to be useful in general practice.
How this fits in
Motivational interviewing has been used and evaluated internationally, especially in the last decade, in relation to the following areas: addiction, change in lifestyle, and adherence to treatment. Previous studies show significant effect of motivational interviewing in a broad area of diseases influenced by patient behaviour. Motivational interviewing can be effective in even brief encounters of 15 minutes and a course seems to influence GPs' professional behaviour towards use of the method for patient treatment. GPs evaluated that motivational interviewing was more effective than traditional advice giving, and that it improved the patient–doctor relationship. GPs stated that the method was not more time consuming than traditional advice-giving.
METHOD
Study group
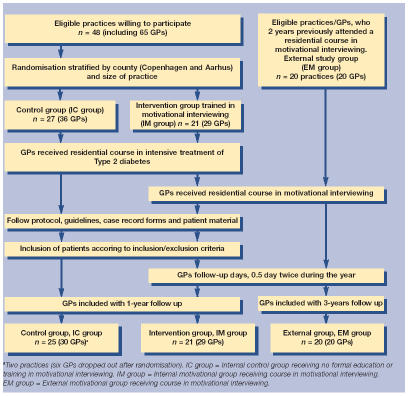
The randomised controlled trial study included two groups participating in the ADDITION study,12 which is a multicentre randomised controlled trial of a target-driven approach to intensive treatment of patients with type 2 diabetes detected by screening. On 1 January 2001, all practices registered at the County Health Insurance Registry in Aarhus County were invited to meetings about participation in the ADDITION study. No exclusion criteria for the GPs were applied and included GPs in the ADDITION study were randomised at practice level into a group giving standard care and an intervention group educated to intensive treatment including lifestyle intervention and poly-pharmacological treatment aiming for rigorous values of blood glucose, blood pressure and lipids in addition to anticoagulation treatment. Randomisation was done by drawing lots. The inclusion of GPs is shown in Figure 1. Randomisation within the ADDITION study was stratified by county (Copenhagen and Aarhus) and size of practices. GPs received education and training free of charge.
Figure 1.
Flowchart of included GPs and patients with type 2 diabetes.
This study included practices/GPs from the intervention group of the ADDITION study. These practices/GPs were sub-randomised into: a motivational group (M group) comprising GPs receiving a course with education and training in motivational interviewing; and a control group (C group) comprising GPs receiving no formal education or training in motivational interviewing.
The study also included a long-term motivational group (LM group). This group consisted of GPs (n = 20) who had attended the course in motivational interviewing 2 years prior to the start of the ADDITION study. This group was contacted externally to the ADDITION study and was asked to answer the same questionnaire as GPs within the ADDITION study, thus serving as a group of GPs with long-term knowledge of the use of motivational interviewing. GPs in this group attended the training and paid all expenses themselves.
Method of intervention
The courses in motivational interviewing for the GPs in the M and LM groups were conducted by a single trained teacher, who had conducted several of these courses successfully. The teacher is the first author of Motivational interviewing, a manual from the Danish Scientific Society of General Practitioners (2000).13 This manual and the book of Miller and Rollnick, Motivational interviewing, preparing people to change addictive behaviour14 (1991) constituted the theoretical part of the course curriculum. Each course included 6–12 GP participants. Each session started with a short introduction to the methods of motivational interviewing followed by group discussions and training the methods involving a high level of participation in workshops and role-plays. The principal rules of motivational interviewing in relation to the patient–doctor relationship14 were trained as was the use of the specific skills mentioned below. Detailed description of these skills can be found in the book Motivational interviewing14 and on the website: http://motivationalinterview.org/clinical/overview.html
Empowerment relies upon identifying and mobilising the client's intrinsic values and goals to stimulate behaviour change;14,15
Use of the ambivalence in motivational interviewing are designed to elicit, clarify, and resolve ambivalence to perceive benefits and costs associated with it;14
The decisional balance schedule and visual analogue scale are tools in which advantages and disadvantages with the behaviour to be changed and with the health behaviour to be obtained is enlighten. It is used in the process of eliciting and reinforcing the client's belief in ability to carry out and succeed in achieving a specific goal is essential;14
The ‘stage of change’ model clarifies the different stages toward changing behaviour. Readiness to change is not a client trait, but a fluctuating product of interpersonal interaction. Resistance and ‘denial’ is often a signal to modify motivational strategies. The stage of change model accommodates knowledge on how to clarify the patient's readiness to change behaviour and at what level to intervene on;14,16
Reflective listening is both a set of techniques and counselling style.14
The courses for the GPs in the M group consisted of 1.5-day training sessions with half a day follow-up twice during the first year.
Two years prior to the start of this study, the GPs in the LM group had participated in a course similar to that given the M group. None of the GPs in either three groups had previously participated in courses in motivational interviewing.
All GPs in the trial (M/C group) had participated in the same training courses in intensive treatment of type 2 diabetes patients detected by screening. The training course lasted half a day and follow up was performed as afternoon meetings twice every year. During these diabetes training sessions, it was stressed that GPs should act as counsellors for the patients, allowing treatment decisions to be based on a mutual understanding between the patient and the GP.
Measurements
No validated questionnaire was available for evaluating the courses in motivational interviewing and the GP's conception of the methods, adherence to the technique and their actual use of motivational interviewing. The construct of the questionnaire was therefore designed based on: the theoretical knowledge about motivational interviewing; the leading author's knowledge from attending the course; and knowledge from the teacher and head of the course. The content of the questionnaire was divided into themes: GPs reaction in specific patient cases; GPs preferred way of motivating change in patient behaviour; and practicability of motivational interviewing and aspects concerning the GP's use of the technique in their daily clinical work. The questionnaire was evaluated and pilot tested by GPs and lay people within and outside the Department of General Practice, University of Aarhus. The validation process included ensuring that questions were not to be misunderstood, that questions in total covered the themes while at the same time not overlaying each other and that answering categories was sufficient to discriminate between different answers. In order to evaluate the GPs' use of motivational interviewing, the four questions in Boxes 1 and 2 were asked.
Box 1. Questions 1–3: evaluating how GPs used motivational interviewing.
-
▸
Q1: What do you do, when the patient obviously does not follow your advice?
-
▸
Q2: What do you do, when you sense that the patient does not want to follow your advice?
-
▸
Q3: What do you do, when the patient's conception of good health and actual life style are inconsistent?
GPs had to respond on a 5-item Likert scale to each of the following possible reactions:
-
▸
Explain the plan of treatment and care once again
-
▸
Explore further the patient's abilities and possibilities for solving the problem
-
▸
Explain by arguments why it is important to follow the treatment once again
-
▸
Investigate if the patient believes that the treatment will help
-
▸
Make the patient tell about advantages and disadvantages of habits in relation to disease
-
▸
Inform further about the disease and treatment to pursuit the patient to a deal
-
▸
Tell further about the consequences if the treatment plan is not followed
-
▸
Make the patient summarise the agreed deal
-
▸
Ask about the patient's expectations to what you can do in the actual situation of disease
Five-item Likert scale: Fully agree = 1, partly agree = 2, not agree or disagree = 3, partly disagree = 4, totally disagree = 5.
Box 2. Question 4: evaluating how GPs used motivational interviewing.
-
▸
Q4: What do you do, when you aim at motivating change in patient behaviour?
GP's had to respond on a 5-item Likert scale to each of following possible reactions:
-
▸
Reflective listening
-
▸
Preparing the patient of different treatment options before choosing the one
-
▸
Using accurate arguments for change of lifestyle to emphasise the consequences of sustained lifestyle
-
▸
Clarifying the treatment strategy in relation to time
-
▸
Emphasising the patients resources
-
▸
Clarify what advantaged and disadvantages the patient sees in relation to disease and plan of treatment
-
▸
Showing patient empathy, support and respect
-
▸
Focusing on the positive sides of the patients habits in relation to the disease
Five-item Likert scale: always = 1, often = 2, on occasion = 3, seldom = 4, never = 5.
The possible reactions for Q1–4 were related to counselling style, using either motivational interviewing or ‘traditional advice giving’. Traditional advice giving is used as an expression for doctor-centred approach, that is the GP define the patients' problem from a biomedical perspective that usually does not include the patient perspective on the matter, thus giving advice accordingly.17,18
The sum-scores for questions 1–4 were calculated to evaluate whether or not the GPs used the methods of motivational interviewing or traditional advice giving. Questions 1–4 were based on the responses to each possible reaction in Boxes 1 and 2. The responses were first reversed in order to unify the direction of the response to each possible reaction. Then all the responses to the possible reactions to each question were added and divided by the number of items, thereby generating a mean response for each question. The method of sum-scoring questions has been used and validated in different settings.19–23
Questions 1–4 were given to all three groups of GPs, whereas the remaining questions regarding the practicability of motivational interviewing and aspects concerning the GPs' use of the technique in their daily clinical work (Table 2) were given to the GPs in the motivational groups (M/LM group). Questionnaires were mailed to all three groups either 1 year (M and C groups) or 3 years (LM group) after the courses. Reminders were mailed 2 weeks later.
Table 2.
GPs' use of specific methods of motivational interviewing 1 year (IM group) and 3 years (EM group) after a course in motivational interviewing.
| Group | IM group (n = 27) | EM group (n = 20) | IM group (n = 27) | EM group (n = 20) | |
|---|---|---|---|---|---|
| Methoda | GP has used the specific method (%) | GP has used the specific method (%) | GP agrees that method is usable, median (25%; 75% quartile) | GP agrees that method is usable, median (25%; 75% quartile) | P-value IM–EM |
| PEARLSb | 81 | 95 | 1 (1; 2) | 2 (1; 2) | ns |
| Reflective listening | 100 | 100 | 1 (1; 1) | 1 (1; 1) | ns |
| Visual analog scale | 92 | 84 | 2 (1; 2) | 2 (1.75; 3) | P<0.05 |
| Stage of change | 81 | 79 | 2 (1; 2) | 2 (1; 2) | ns |
| Balance schedule | 100 | 90 | 1 (1; 2) | 1.5 (1; 3) | P<0.05 |
| Showing and using the ambivalence | 85 | 79 | 1 (1; 2) | 1 (1; 3) | ns |
| Empowering | 96 | 100 | 1 (1; 1) | 1 (1; 2) | ns |
Questionnaire scaling: 1–5, 1 = Yes, fully agree and 5 = No, disagree.
Partnership-Empathy-Accept-Respect-Legitimate-Support (PEARLS). ns = non-statistical significant difference. IM group = internal motivational group receiving course in motivational interviewing. EM group = external motivational group receiving course in motivational interviewing.
Statistical method
The number of practices participating in this study was set by the main ADDITION study. Therefore, a post-hoc power calculation allowing for clustering was made concluding that the study would show effect (95% CI [confidence interval]) of motivational interviewing, if more than 40% of GPs in M-group compared to the C group stated using the method. Statistical analysis of data was conducted in SPSS (version 11.0). All single variables including Likert scale are shown as descriptive data and were analysed by a non-parametric Mann–Whitney test. All sum-score variables from questions 1–4 followed a normal distribution and consequently a t-test was performed showing results as mean with a 95% CI. A statistical significance level of 0.05 (two tailed) was used.
RESULTS
Study sample characteristics
A flowchart for participating practices and GPs is shown in Figure 1. In all, 48 practices with 65 GPs were included. Twenty-seven practices (36 GPs) were randomised into the M group and 21 practices (29 GPs) into the C group. Two practices, including 6 GPs (all in control group), dropped out just after randomisation. We obtained a 100% response rate to the questionnaire from the GPs in all three groups. All GPs in the M and LM group participated in the motivational interviewing courses, and less than 10% were absent from the 0.5-day follow-up meetings. The average age of the GPs was 53 years, 65% were male, and they had an average of 1533 patients (listed) in their practice. There were no significant differences between the study groups.
Study data and analyses
The motivational group seemed to adhere more to motivational interviewing than the control group as there were significant differences in terms of the GP's responses to different doctor–patient situations (Table 1). The responses from GPs in the control group to the possibilities raised in Boxes 2 and 3 showed that they used some elements from both strategies, motivational interviewing and traditional advice giving.
Table 1.
GPs' counselling according to the methods of motivational interviewing. Evaluation by mean sum-scores from the possible reactions to Q1–4 (see Boxes 1 and 2).
| IC group n = 31 Mean sum-score | IM group mean n = 27 Mean sum-score | EM group mean n = 20 Mean sum-score | P-value (95% CI) IC vs M | P-value (95% CI) IC vs EM | P-value (95% CI) M vs EM |
|---|---|---|---|---|---|
| 2.93 | 2.05 | 2.04 | 0.001 (0.56 to 1.21) | 0.001 (0.39 to 1.13) | 0.59 (−0.21 to 0.35) |
| 2.92 | 2.10 | 2.14 | 0.001 (0.49 to 1.15) | 0.001 (0.41 to 1.03) | 0.94 (−0.31 to 0.34) |
| 2.82 | 2.08 | 2.23 | 0.001 (0.40 to 1.06) | 0.022 (0.07 to 0.74) | 0.40 (−0.48 to 0.20) |
| 1.93 | 1.69 | 1.65 | 0.005 (0.09 to 0.44) | 0.026 (0.04 to 0.56) | 0.88 (−0.23 to 0.27) |
Questionnaire scaling: 1–5, 1 = acting according to the methods of motivational interviewing and 5 = acting according to ‘traditional advice giving’ (the doctor decides what is best for the patient). IC group = internal control group NOT receiving course in motivational interviewing. IM group = internal motivational group receiving course in motivational interviewing. EM group = external motivational group receiving course in motivational interviewing.
A majority of more than 81% of GPs in both motivational groups stated that they had used the different elements of motivational interviewing after the course, such as Partnership-Empathy-Accept-Respect-Legitimate-Support (PEARLS), visual analog scale, stage of change, balance schedule and empowering etc (Table 2).
Additional questions addressed the GPs' opinion of the course and aspects regarding actual use of the technique. On a questionnaire scale from 1–5, where 1 = fully agree and 5 = disagree, the GPs from both motivational groups agreed on the following questions (Table 3):
Are the methods of motivational interviewing realistic and usable in daily work? (median = 1 and 25%; 75% quartiles = 1, 2)
They are more effective than traditional advice giving (median = 1 and 25%; 75% quartiles = 1, 2)
Motivational interviewing is an improvement of my working-methods in the patient–doctor relationship (median = 1, 5 and 25%; 75% quartiles = 1, 2)
It is an advantage to change working-methods to motivational interviewing (median = 1, 5 and 25%, 75% quartiles = 1, 2)
Table 3.
GP questions: what is your opinion about the methods of motivational interviewing?
| Questions | IM group, n = 27 Median (25%; 75% quartiles) | EM group, n = 20 Median (25%; 75% quartiles) | IM versus EM group P-value |
|---|---|---|---|
| 1. Did you get the principal rules of motivational interviewing from the residential course? | 2 (1; 2) | 2 (1; 2) | ns |
| 2. Did you feel trained adequately to use motivational interviewing in daily work? | 2 (1; 2) | 2 (1; 2) | ns |
| 3. Are the methods of motivational interviewing realistic and usable in daily work? | 1 (1; 2) | 1 (1; 2) | ns |
| 4. They are very suitable for GPs | 2 (1; 2) | 2 (1; 2) | ns |
| 5. They are suitable for some patients | 3 (2; 5) | 4 (2.25; 4) | ns |
| 6. They are more effective than traditional advice giving | 1 (1; 2) | 1 (1; 2) | ns |
| 7. I have not yet had patients suitable for the motivational interview | 5 (4; 5) | 5 (4; 5) | ns |
| 8. Motivational interviewing is an improvement of my working methods in the patient–doctor relationship | 2 (1; 2) | 1.5 (1; 2) | ns |
| 9. I cannot change my working methods and habits by using motivational interviewing | 4 (2; 4) | 5 (4; 5) | P <0.05 |
| 10. It is an advantage to change working methods to motivational interviewing | 2 (1; 2) | 1 (1; 2) | ns |
| 11. The methods of motivational interviewing from the residential course helps me in my patient care and my patient–doctor relationship | 1 (1; 2) | 2 (1; 2) | ns |
| 12. The methods are time-consuming | 3 (2; 4) | 5 (3.25; 5) | P <0.05 |
| 13. Patients want the doctor to tell what must be done | 3 (2; 4) | 5 (4; 5) | P <0.05 |
| 14. It is difficult to change my ‘ways’ in the patient–doctor relationship | 2 (2; 3) | 4 (3; 5) | P <0.05 |
Questionnaire scaling: 1–5, 1 = Yes, fully agree and 5 = No, disagree. ns = non-statistical significant difference. IM group = internal motivational group receiving course in motivational interviewing. EM group = external motivational group receiving course in motivational interviewing.
Furthermore, the GPs from both motivational groups disagreed in the question; ‘I cannot change my working methods and habits by using motivational interviewing’, even though the LM group was more certain about this (median = 5 and 25%; 75% quartiles = 4; 5), than the M group (median = 4 and 25%; 75% quartiles = 3; 4). Finally the GPs in LM group were more certain (median = 5 and 25%; 75% quartiles = 3.25; 5) that the methods were not time-consuming than GPs in the M group (median = 3 and 25%; 75% quartiles = 2; 4).
DISCUSSION
Summary of main findings
Based on self-reported questionnaires, this study shows that, after a course in motivational interviewing, the GPs seemed to change their professional behaviour in daily practice using motivational interviewing compared with the control group. GPs evaluated motivational interviewing to be more effective than ‘traditional advice giving’.
Strength and limitations of the study
The main strengths of the study are that all GPs responded to the questionnaire, all GPs in the M group attended the motivational interviewing courses, and less than 10% GPs were absent from the follow-up meetings.
We used questionnaires as a method of measuring the effect of a course in motivational interviewing of GPs in general practice and obtained statistically significant changes between study groups. However, the sensitivity of the measuring method is not known, when focusing on the GPs' actual use and adherence to motivational interviewing. In order to enhance sensitivity of these aspects, external assessment was required, such as video-recordings. This was not possible in this study of 48 practices, and 65 GPs in two counties. We did not include the questions regarding specific methods and techniques of motivational interviewing in the questionnaire to the C group (the control group) for two reasons. In the pilot-testing process all GPs answered the questions, and GPs who had not previously attended a course in motivational interviewing were confused by the questions, which to them seemed irrelevant. Furthermore, we did not want to disclose the features and specific techniques of motivational interviewing to the control group, thus perhaps introducing a bias.
The GPs in the trial were randomised to either motivational interviewing or not, whereas GPs in the LM group had decided by themselves to participate in the course. Thus the GPs in the latter group were probably more motivated to obtain and use motivational interviewing than the former groups. However, both motivational groups (M/LM group) rated motivational interviewing the same way except that long-term group agreed more to the usefulness and the effect of motivational interviewing in general practice.
In spite of the relatively small number of GPs in each group (20–31), significant findings between the motivational group and control group were found. Previous studies on motivational interviewing in general practice have proven an effect.4–9 However, only few studies have focused on how to implement motivational interviewing in the daily clinical work in general practice in such a way that it is ascertained that the method is used after study closure.10,11 They concluded that despite barriers it was possible to implement the use motivational interviewing in general practice.10,11
The study suffers the limitation that GPs in the control group could have become familiar with motivational interviewing by personal initiative during the study period. Furthermore, GPs in the randomised controlled trial received training in intensive treatment of patients with type 2 diabetes. During these diabetes training sessions, it was stressed that GPs should act as counsellors giving patients advice about how to reduce the risk of late diabetic complications and allow treatment decisions to be based on mutual understanding between the patient and the GP. This may have influenced the GPs in the control group, who in their response to the possibilities in Boxes 2 and 3 indicated that they neither entirely used motivational interviewing or the ‘traditional advice giving’. However, some of their choices showed a tendency for adhering to motivational interviewing. Furthermore the M-group had to attend to two courses (intensive treatment of type 2 diabetes and motivational interviewing), thus the focus on the traditional intensive treatment may have weakened the focus on motivational interviewing. These circumstances tend to reduce the differences between GPs in the C and the M group. In spite of this, statistically significant differences were found.
The intervention consisted of a course in motivational interviewing conducted by one person. Outcome is therefore highly dependent on this person's teaching methods and capacity to train the GPs. If several teachers had conducted the courses, this problem would have been diminished. The use of more teachers on different courses, however, might have introduced differences in learning and training outcome. We chose to use one teacher only because only very few can teach motivational interviewing in Denmark and the teacher had previously conducted several of these courses and was the leading author to the course curriculum.
Detailed findings
The study showed that the GPs in the motivational group reported that they used the techniques of motivational interviewing significantly more than the control group. Furhtermore, even though GPs in the M group were recruited by randomisation, their responses mirrored those of the GPs who participated by own choice (LM group). The results after 3 years in the M group would probably be close to the present results of the LM group. This is further supported by the fact that both groups evaluated motivational interviewing as usable and suitable for general practice. In addition to this, more GPs in the LM group expressed that the method was not more time consuming than ‘traditional advice giving’. The time-consuming aspect of motivational interviewing has previously been investigated by Rollnick et al in relation to smoking cessation reporting that an average consultation encounter lasted 9–10 min, which was acceptable to the GPs.5
The motivational groups found that motivational interviewing improved the patient–doctor relationship and that it was more effective than ‘traditional advice giving’. Stott et al performed a study on how GPs would react to new technologies and methods showing that GPs did adopt, accept and use new methods when they facilitated solutions to problems in patient–doctor relationship.24 The difference between the motivational groups could indicate that it takes more than 1 year to integrate motivational interviewing into daily clinical practice.
Implications for future research
Doherty et al addressed the relevance of developing GPs' skills through motivational interviewing and the importance of acknowledging the difficulties of changing professional behaviour.25 This study has focused on the first step towards implementing motivational interviewing to change the way GPs are integrating motivational interviewing into their daily work. Further research into the precise use of motivational interviewing by GPs is required in order to identify which methods are most effective and why. Another aspect to be addressed is whether and how the use of motivational interviewing affects the patient's attitudes toward changing behaviour, such as lifestyle and adherence. Finally future research should explore potentially objective measures such as a change in patient risk profile. The ADDITION study12 is an ongoing randomised controlled trial, which among others aims to gather long-term effect measurements on these issues.
A motivational interviewing course seems to influence GPs' professional behaviour. Based on self-reported questionnaires, this study shows that the GPs after a course in motivational interviewing seemed to change their professional behaviour in daily practice using motivational interviewing compared with the control group. GPs evaluated motivational interviewing to be more effective than ‘traditional advice giving’. Furthermore, GPs stated that the method was not more time-consuming than ‘traditional advice giving’. Whether motivational interviewing results in a better prognosis for patients remains to be proved.
Acknowledgments
Thanks to all the GPs involved in the ADDITION study and to Professor Carl Erik Mabeck for sharing his profound knowledge on the area of motivational interviewing.
Funding body
We thank the Danish Research Foundation for General Practice, The Danish Medical Association Research Fund/The Lundbeck Funds Grant, The Diabetes Associations Foundation for Scientific Research and The Novo Nordic Research Foundation for financial support
Ethics committee
The study was approved by the Committee on Biomedical Research Ethics and by the Danish Data Protection Agency according to conducting the study within the rules of data safety and research ethics
Competing interests
The authors have stated that there are none
REFERENCES
- 1.Miller WR. Motivational interviewing with problem drinkers. Behavioural Psychotherapy. 1983;11:147–172. [Google Scholar]
- 2.Miller WR, Rollnick S. Motivational interviewing, preparing people to change addictive behavior. New York: The Guildford Press; 1991. [Google Scholar]
- 3.Rubak S, Christensen B, Sandbaek A, Lauritzen T. Motivational Interviewing: A systematic review and meta-analysis. Br J Gen Pract. 2005;55(513):305–512. [PMC free article] [PubMed] [Google Scholar]
- 4.Beresford SA, Curry SJ, Kristal AR, et al. A dietary intervention in primary care practice: the Eating Patterns Study. Am J Public Health. 1997;87:610–616. doi: 10.2105/ajph.87.4.610. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Harland J, White M, Drinkwater C, et al. The Newcastle exercise project: a randomised controlled trial of methods to promote physical activity in primary care. BMJ. 1999;319:828–832. doi: 10.1136/bmj.319.7213.828. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Rollnick S, Butler CC, Stott N. Helping smokers make decisions: the enhancement of brief intervention for general medical practice. Patient Educ Couns. 1997;31:191–203. doi: 10.1016/s0738-3991(97)01004-5. [DOI] [PubMed] [Google Scholar]
- 7.Woollard J, Beilin L, Lord T, et al. A controlled trial of nurse counselling on lifestyle change for hypertensives treated in general practice: preliminary results. Clin Exp Pharmacol Physiol. 1995;22:466–468. doi: 10.1111/j.1440-1681.1995.tb02046.x. [DOI] [PubMed] [Google Scholar]
- 8.Pill R, Stott NC, Rollnick SR, Rees M. A randomized controlled trial of an intervention designed to improve the care given in general practice to type II diabetic patients: patient outcomes and professional ability to change behaviour. Fam Pract. 1998;15:229–235. doi: 10.1093/fampra/15.3.229. [DOI] [PubMed] [Google Scholar]
- 9.Butler CC, Rollnick S, Cohen D, et al. Motivational consulting versus brief advice for smokers in general practice: a randomised trial. Br J Gen Pract. 1999;49:611–616. [Google Scholar]
- 10.Botelho RJ, Novak S. Dealing with substance misuse, abuse, and dependency. Prim Care. 1993;20:51–70. [PubMed] [Google Scholar]
- 11.Scales R, Miller JH. Motivational techniques for improving compliance with an exercise program: skills for primary care clinicians. Curr Sports Med Rep. 2003;2:166–172. doi: 10.1249/00149619-200306000-00010. [DOI] [PubMed] [Google Scholar]
- 12.Lauritzen T, Griffin S, Borch-Johnsen K, et al. The ADDITION study: proposed trial of the cost-effectiveness of an intensive multifactorial intervention on morbidity and mortality among people with type 2 diabetes detected by screening. Int J Obes Relat Metab Disord. 2000;24(Suppl 3):S6–S11. doi: 10.1038/sj.ijo.0801420. [DOI] [PubMed] [Google Scholar]
- 13.Mabeck CE, Kallerup H, Maunsbach M, DSAM . Copenhagen: The Danish Association of Doctors; 2001. Den motiverende samtale [Motivational interviewing] [Google Scholar]
- 14.Miller WR, Rollnick S. Motivational interviewing, preparing people to change addictive behavior. New York: The Guildford Press; 2002. [Google Scholar]
- 15.Feste C, Anderson RM. Empowerment: from philosophy to practice. Patient Educ Couns. 1995;26:139–144. doi: 10.1016/0738-3991(95)00730-n. [DOI] [PubMed] [Google Scholar]
- 16.Prochaska JO, DiClemente CC. Transtheoretical therapy: toward a more integrative model of change. Psychotherapy: theory, research and practice. 1982;19:276–288. [Google Scholar]
- 17.Mabeck CE. København: Munskgaard: Lægeforeningen; 1994. Lægen og patienten [The doctor and the patient] [Google Scholar]
- 18.Mabeck CE. Købehavn: Lægeforeningens forlag; 1999. Samtalen med patienten [The doctor and the patient] [Google Scholar]
- 19.Edgar KA, Skinner TC. Illness representations and coping as predictors of emotional well-being in adolescents with type 1 diabetes. J Pediatr Psychol. 2003;28:485–293. doi: 10.1093/jpepsy/jsg039. [DOI] [PubMed] [Google Scholar]
- 20.Skinner TC, Howells L, Greene S, et al. Development, reliability and validity of the Diabetes Illness Representations Questionnaire: four studies with adolescents. Diabet Med. 2003;20:283–289. doi: 10.1046/j.1464-5491.2003.00923.x. [DOI] [PubMed] [Google Scholar]
- 21.Skinner TC, Hampson SE, Fife-Schaw C. Personality, personal model beliefs, and self-care in adolescents and young adults with type 1 diabetes. Health Psychol. 2002;21:61–70. [PubMed] [Google Scholar]
- 22.Skinner TC, Hampson SE. Personal models of diabetes in relation to self-care, well-being, and glycemic control. A prospective study in adolescence. Diabetes Care. 2001;24:828–833. doi: 10.2337/diacare.24.5.828. [DOI] [PubMed] [Google Scholar]
- 23.McIver JP, Carmins EG. Unidimensional scaling. Beverly Hills, CA: Sage Publication; 1982. [Google Scholar]
- 24.Stott NC, Rees M, Rollnick S, et al. Professional responses to innovation in clinical method: diabetes care and negotiating skills. Patient Educ Couns. 1996;29:67–73. doi: 10.1016/0738-3991(96)00935-4. [DOI] [PubMed] [Google Scholar]
- 25.Doherty Y, Roberts S. Motivational interviewing in diabetes practice. Diabet Med. 2002;19(Suppl 3):1–6. doi: 10.1046/j.1464-5491.19.s3.2.x. [DOI] [PubMed] [Google Scholar]