Abstract
Beginning in 2004, the Indiana State Department of Health (ISDH) partnered with the Regenstrief Institute on a 4-year project to implement a statewide biosurveillance system incorporating more than 110 hospitals. This paper describes our evolving experience with the system including ongoing implementation challenges, how the system has helped to uncover events of public health significance, and future directions. The system currently receives emergency department visit data from 50 hospitals totaling nearly 5,000 visits per day, and is projected to have 65 hospitals connected by August 2006.
Introduction
Biosurveillance systems focus on the use of early disease indicators to identify outbreaks before definitive diagnoses are made. In the face of recent bioterrorism threats such as anthrax and current concerns about pandemic influenza, these systems are viewed as critical to the nation's health care infrastructure.1,2 Consequently, there are growing numbers of regional, state and federal biosurveillance initiatives underway.3,4,5,6 In order to be successful and sustainable, we believe that biosurveillance systems must provide value to both public health and healthcare delivery systems by integrating with existing health information systems. We previously described the Indiana biosurveillance project goals, technical architecture, and how it interoperates with and augments existing health information exchange.7 This paper describes our evolving experience with the system, including ongoing implementation challenges, preliminary operational results, and future directions.
In 2004, the Indiana State Department of Health (ISDH) partnered with the Regenstrief Institute to develop its biosurveillance system, the Public Health Emergency Surveillance System (PHESS). The goal of the project is to create a statewide, standards-based public health surveillance system connecting more than 110 of Indiana’s hospitals. Our four-year implementation strategy seeks to leverage data that is already commonly collected during routine health care delivery. Because the PHESS is built on a foundation of standardized HL7 messages, the infrastructure can readily incorporate additional clinical data flows beyond those used for traditional syndromic surveillance, including clinical messaging8 and electronic laboratory reporting.9 Further, because the PHESS uses a standards-based architecture, it is compatible with national initiatives including the CDC’s PHIN10 and BioSense projects.
Current Status
The PHESS implementation began in October, 2004. The system currently receives standards-based HL7 emergency department (ED) visit data (including free-text chief complaint) from 50 hospitals totaling nearly 5,000 ED visits per day. We are projected to have 65 hospitals connected by August 2006. The hospitals send data in real time using secure VPN connections consuming approximately 11 MB per day. Regenstrief processes these messages and securely delivers a batch dataset to the ISDH every three hours.
The Marion County Health Department (MCHD) is Indiana’s largest county health department and serves the Indianapolis metropolitan region (population 860,000). The MCHD receives Marion County ED visit data directly from the ISDH. Both the ISDH and the MCHD analyze PHESS data using ESSENCE, a biosurveillance monitoring application developed by Johns Hopkins University that provides tabular and geospatial statistical analyses capabilities.11 We monitor eight syndrome categories specified by ESSENCE, including respiratory, fever, gastrointestinal, neurological, hemorrhagic, botulinic, rash, and shock/coma. Any chief complaint that cannot be classified into one of these eight categories is placed into the category “other”.
Public Health Alert Review and Response
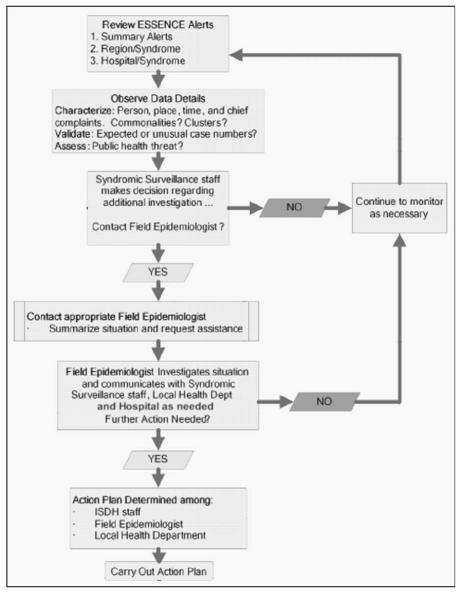
While many of the biosurveillance efforts have focused on data collection and accurate signal detection, a primary challenge for organizations using these systems is to formalize and streamline a response protocol. Because actual outbreaks are infrequent, surveillance systems produce more false signals than true signals. Thorough investigation of every signal would exhaust health department resources. At both the ISDH and the MCHD, an epidemiologist reviews ESSENCE output for unusual trends on a daily basis, and examines detailed data when an unusual signal occurs. If detailed data indicate a potential outbreak, disease specialists from the MCHD or one of the ISDH’s 10 district field epidemiologists are consulted, and local hospitals and/or local health departments may be contacted as a result. Hospital emergency department or infection control personnel then provide information that either concludes the inquiry or prompts a full field investigation.
If an outbreak is occurring, public health officials are contacted to provide increased investigative capacity, case management, and follow-up (Figure 1). The roles of the ISDH and local health departments vary based on local health department capacity and preferences. For Marion County, the ISDH plays primarily a supportive role by confirming unusual signals that the MCHD epidemiologists have noted, while the MCHD assumes the lead role. For other counties, the ISDH shares a more central leadership role in the investigation process in conjunction with local health officials. The MCHD requires less than 3 hours per week to review data and perform initial inquiries, and initiates less than one field investigation every three months. The ISDH actively optimizes monitoring and response protocols for the system, and so invests substantially more time.
Figure 1.
ISDH Public Health Alert Review and Response Process
Operational Lessons
Interfaces
One common implementation challenge we face is scheduling time with appropriate hospital personnel responsible for establishing outbound interfaces. Although most hospitals are pleased to participate in the PHESS, hospital IT staff are often overburdened and have little reserve time available for additional projects. Consequently, scheduling initial meetings and follow-up phone calls often can take weeks. An average of 84 days elapses for hospitals to establish real-time data transmission, while actual time required of hospital personnel is often less than one day.
Most hospital software vendors charge for additional outbound interfaces. As a result, a second challenge we face is hospitals that lack financial resources to make any needed modifications to their outbound data interface in order to connect to the PHESS. To address this, the ISDH encourages hospitals to use their state-allotted HRSA funds as a financial resource if such upgrades are necessary. Further, Regenstrief is very flexible about the messages hospitals transmit, allowing hospitals to use existing interfaces.
Monitoring Flows
Regenstrief monitors the status of real-time data flow from each hospital to ensure timely data delivery from all 50 hospitals. If the data transmission rate falls below a pre-specified threshold, automated processes first attempt to reset the connection. If transmission problems persist after all Regenstrief processes are operational and nominal, we work with the hospital to ensure that connectivity is established at their end and verify that their outbound interface (which is typically a commercial interface engine) is operational and transmitting data. Scheduled and unscheduled network outages lasting more than three hours generally occur less than five times per month for 50 hospitals. In the event of an outage, encountered data is buffered at the source system and transmitted once connectivity is re-established.
Public Health Events Detected
Although research demonstrates that data from emergency department encounters and hospital admissions can signal the onset and evolution of disease outbreaks earlier than traditional surveillance methods, there are few reports of active surveillance systems detecting real public health events.12,13 Below we present preliminary results for actual events of public health interest captured by the PHESS that likely would not have been reported.
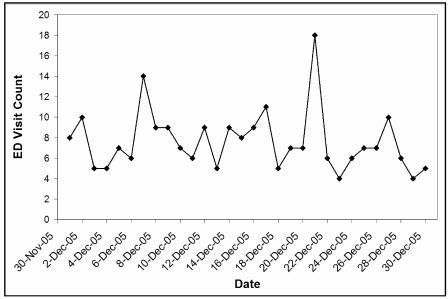
Carbon Monoxide
In December 2005, the ISDH noted an unusually high number of neurological cases in southern Indiana (Figure 2). The ISDH promptly contacted the field epidemiologist for that public-health preparedness district, and the hospital was subsequently contacted. The hospital confirmed that an entire family was evaluated in the emergency department for carbon monoxide exposure in the home. Identification of this event, which did not have major public health significance, provided clear evidence that Indiana's biosurveillance system could detect unusual trends representing real events. It also demonstrated the ability to detect small events, a single family in this example. Further, while public health has previously depended on passive reporting from source institutions, the PHESS’s active surveillance uncovered an event that the institution might not have otherwise reported.
Figure 2.
Neurological syndrome cases. Included in the 12/21/05 upsurge was a family exposed to carbon monoxide
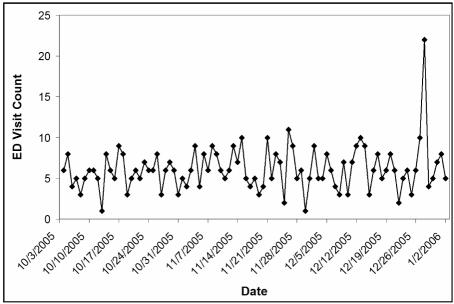
Gastroenteritis
Also in December 2005, the PHESS detected a higher-than-expected number of GI syndrome visits in central Indiana (Figure 3). Included in this upsurge was a cluster of patients who presented to the ED within minutes of one another. After noting the unusual event, the ISDH conferred with the MCHD epidemiologist. MCHD discovered that the increased number of cases resulted from an eight member family presenting with gastrointestinal symptoms. The family had recently consumed food from the same small grocery store. After a health inspection at the store, several food handling problems were corrected.
Figure 3.
A rise in gastrointestinal cases on 12/27/05 was partly due to a family who presented after eating the same food.
Although laboratory cultures of food samples revealed no causative agent, this event provided additional confirmation that the PHESS can help identify events requiring public-health follow-up, and in this case led to the redress of a public health problem.
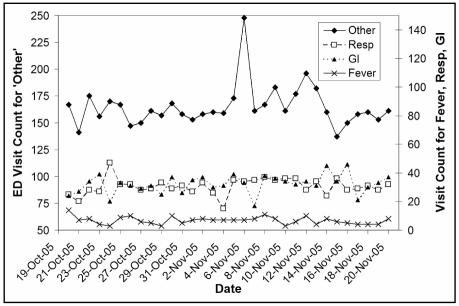
Natural Disaster
On November 6, 2005 the nation’s deadliest tornado of the year struck southwest Indiana, killing 24 people. Immediately following this event, total ED visit volume in the affected region increased noticeably. Figure 4 shows that the majority of excess patient visits were categorized as “other”, which is a catch-all category for visits not sorted into any of the eight pre-specified syndromes. As the ED visit volume climbed, no alerts were triggered for the eight ESSENCE categories. This suggests that the system has the ability to maintain specificity in the face of increased volume, and also indicates that monitoring the ratio of visits classified into syndromes of interest compared with visits classified as “other” may help to identify trends not captured in syndromes of interest.
Figure 4.
Visits categorized as “other” shows a clear spike of almost 100 visits within 24 hours of a deadly tornado striking the region.
Re-using the framework
The same standards-based technical components that underpin the PHESS (secure connectivity, real-time data transmission capabilities, and HL7 messaging) are also key components for other regional health information exchange activities. These include the Indiana Network for Patient Care (INPC), an operational, community-wide medical record system14, and DOCS4DOCS®, an electronic clinical results delivery service offered by the Indiana Health Information Exchange (IHIE) to providers across Indiana. This standards-based approach allows a hospital’s investment in interfaces to serve more than just the PHESS system. For example, the same technical infrastructure that delivers ED visit data can also deliver clinical results to physicians, and can deliver state-mandated reportable disease results to public health.
Hospitals appreciate the value of re-using data and technical infrastructure, and express interest in leveraging the framework implemented for the PHESS to participate in other health information exchange services including clinical messaging (DOCS4DOCS®), electronic health record services (INPC), and electronic laboratory reporting. In 2005 a PHESS hospital elected to join the INPC and DOCS4DOCS® as well.
Future Directions
The standards-based infrastructure created by the PHESS opens the door for additional public health information sharing initiatives. These include:
Additional biosurveillance data elements
Incorporating additional data types into the surveillance signal may help to improve detection accuracy.15 We are exploring including other timely surveillance data elements, including electronic vital signs, physician orders,16 and timely clinical results such as the complete blood count.
Ambulatory care sources
Currently the PHESS captures clinical data from emergency department visits. We are pursuing sources of ambulatory care encounter data as well to learn about the characteristics and value of this data source.
Resource monitoring
Data that accurately reflect the capacity of healthcare systems to deliver care is crucial for allocating resources in the event of a public health emergency. For example, one concrete measure that can help emergency preparedness planners is hospital census data, which reflects reserve bed capacity. We are evaluating the feasibility of collecting daily hospital bed counts for PHESS participants.
Clinical messaging
Clinical results are currently delivered to HIV counselors and ISDH HIV program administrators across the state of Indiana using DOCS4DOCS® clinical messaging, and plans are underway to expand to other program areas, including STD and newborn screening. Clinical messaging may also play an important role in providing feedback and additional clinical data to the healthcare delivery community during any unusual clinical trends. Emergency department physicians currently have access to community-wide INPC data. We are considering developing a notification icon that would alert the INPC users about any unusual public health activity during user login.
Electronic laboratory reporting
Seventeen hospitals in central Indiana currently send electronic laboratory reports (ELR) to local and state public health using the same messaging infrastructure as the PHESS. A recent analysis revealed that ELR captures up to four times as many cases as traditional reporting methods.17 We are currently working with hospitals and public health to develop a strategy to incorporate ELR into case identification and case management workflows where practical and feasible for public health.
Expanding access to ESSENCE
Access to ESSENCE data is currently limited to the ISDH, MCHD, and district field epidemiologists. PHESS hospitals and local health departments have requested access to their surveillance data. As a part of the public health feedback response, the ISDH and MCHD are exploring the feasibility of providing PHESS participants access to ESSENCE data.
Further exploration of chief complaint data
Chief complaint data is used almost exclusively for monitoring predefined syndromes.18 Ad-hoc analysis has revealed that certain keywords such as “exposure”, “meningitis”, and other chief complaints of interest may uncover trends previously undetected. We are exploring supplemental data mining techniques to uncover additional trends in the data.
Conclusion
Indiana's public health emergency surveillance system demonstrates the feasibility of developing a standards-based infrastructure that both augments and interoperates with existing health-care data exchanges. Since its inception 18 months ago, the system has demonstrated the ability to detect relatively small events. Further, it has accurately filtered cases during natural disasters, and has detected two relatively small events which would otherwise have gone unreported. By building an infrastructure that provides value to healthcare delivery and public health stakeholders, biosurveillance systems can maximize the likelihood for success and opportunities for sustainability.
Acknowledgements
We would like to acknowledge Senior Systems Engineer Shahid Khokar, PHESS Project Coordinator Jodi Trotter, MCHD epidemiologist Shandy Dearth, and the ISDH PHESS and field epidemiology staffs. Their talent, hard work, and dedication are crucial to the PHESS project’s success.
References
- 1.Das D, Weiss D, Mostashari F, et al. Enhanced drop-in syndromic surveillance in New York City following September 11, 2001. J Urban Health. 2003 Jun;80(2 Suppl 1):i76–88. doi: 10.1007/PL00022318. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Normile D. Avian influenza. Evidence points to migratory birds in H5N1 spread. Science. 2006 Mar 3;311(5765):1225. doi: 10.1126/science.311.5765.1225. [DOI] [PubMed] [Google Scholar]
- 3.Bradley CA, Rolka H, Walker D, Loonsk J. BioSense: implementation of a National Early Event Detection and Situational Awareness System. MMWR Morb Mortal Wkly Rep. 2005 Aug 26;54(Suppl):11–9. [PubMed] [Google Scholar]
- 4.Mandl KD. Infrastructure and methods to support real time biosurveillance. Proceedings of the National Science Foundation Next Generation Data Mining Workshop. 2002. http://www.cs.umbc.edu/ngdm02.
- 5.Lober WB, Trigg LJ, Karras BT, Bliss D, Ciliberti J, Stewart L, Duchin JS. Syndromic surveillance using automated collection of computerized discharge diagnoses. J Urban Health. 2003 Jun;80(2 Suppl 1):i97–106. doi: 10.1007/PL00022320. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Muscatello DJ, Churches T, Kaldor J, Zheng W, Chiu C, Correll P, Jorm L. An automated, broad-based, near real-time public health surveillance system using presentations to hospital Emergency Departments in New South Wales, Australia. BMC Public Health. 2005 Dec 22;5:141. doi: 10.1186/1471-2458-5-141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Grannis S, Biondich P, Mamlin B, et al. How Disease Surveillance Systems Can Serve as Practical Building Blocks for a Health Information Infrastructure: the Indiana Experience. Proc Symp American Medical Informatics Association. 2005 Fall; [PMC free article] [PubMed] [Google Scholar]
- 8.McGowan JJ, Overhage JM, Barnes M, McDonald CJ. Indianapolis I3: The third generation Integrated Advanced Information Management Systems. Med Libr Assoc. 2004 Apr;92(2):179–187. [PMC free article] [PubMed] [Google Scholar]
- 9.Overhage J, Suico J, McDonald C. Electronic laboratory reporting: barriers, solutions and findings. J Public Health Manag Pract. 2001;7(6):60–6. doi: 10.1097/00124784-200107060-00007. [DOI] [PubMed] [Google Scholar]
- 10.Loonsk JW, McGarvey SR, Conn LA, Johnson J. The Public Health Information Network (PHIN) Preparedness initiative. J Am Med Inform Assoc. 2006 Jan–Feb;13(1):1–4. doi: 10.1197/jamia.M1815. Epub 2005 Oct 12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Burkom HS, Elbert Y, Feldman A, Lin J. Centers for Disease Control and Prevention (CDC). Role of data aggregation in biosurveillance detection strategies with applications from ESSENCE. MMWR Morb Mortal Wkly Rep. 2004 Sep 24;53(Suppl):67–73. [PubMed] [Google Scholar]
- 12.Marx MA, Rodriguez CV, Greenko J, et al. Diarrheal illness detected through syndromic surveillance after a massive power outage: New York City, August 2003. Am J Public Health. 2006 Mar;96(3):547–53. doi: 10.2105/AJPH.2004.061358. Epub 2005 Dec 27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Hogan WR, Tsui FC, Ivanov O, Gesteland PH, Grannis S, Overhage JM, Mikanatha N, Robinson JM, Wagner M. Early Detection of Pediatric Respiratory and Diarrheal Outbreaks from Retail Sales of Electrolyte Products. JAMIA. 2003;10(6) doi: 10.1197/jamia.M1377. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Biondich P, Grannis S. Supplement to the J Pub Health Mgmt Prac: Integrating Child Health Information Systems. Nov, 2004. The Indianapolis Network for Patient Care (INPC): An Integrated Clinical Information System Informed by Over Thirty Years of Experience. [PubMed] [Google Scholar]
- 15.Chen JH, Schmit K, Chang H, Herlihy E, Miller J, Smith P. Use of Medicaid prescription data for syndromic surveillance--New York. MMWR Morb Mortal Wkly Rep. 2005 Aug 26;54(Suppl):31–4. [PubMed] [Google Scholar]
- 16.Ma H, Rolka H, Mandl K, Buckeridge D, Fleischauer A, Pavlin J. Implementation of laboratory order data in BioSense Early Event Detection and Situation Awareness System. MMWR Morb Mortal Wkly Rep. 2005 Aug 26;54(Suppl):27–30. [PubMed] [Google Scholar]
- 17.Overhage JM, Grannis S, McDonald CJ. Electronic Laboratory Reporting from Hospitals for Public Health: Validation Based on Operational Experience. unpublished manuscript. [Google Scholar]
- 18.Mikosz CA, Silva J, Black S, Gibbs G, Cardenas I. Centers for Disease Control and Prevention (CDC). Comparison of two major emergency department-based free-text chief-complaint coding systems. MMWR Morb Mortal Wkly Rep. 2004 Sep 24;53(Suppl):101–5. [PubMed] [Google Scholar]