Abstract
Utilizing advanced information technology, Intensive Care Unit (ICU) remote monitoring allows highly trained specialists to oversee a large number of patients at multiple sites on a continuous basis. In the current research, we conducted a time-motion study of registered nurses’ work in an ICU remote monitoring facility. Data were collected on seven nurses through 40 hours of observation. The results showed that nurses’ essential tasks were centered on three themes: monitoring patients, maintaining patients’ health records, and managing technology use. In monitoring patients, nurses spent 52% of the time assimilating information embedded in a clinical information system and 15% on monitoring live vitals. System-generated alerts frequently interrupted nurses in their task performance and redirected them to manage suddenly appearing events. These findings provide insight into nurses’ workflow in a new, technology-driven critical care setting and have important implications for system design, work engineering, and personnel selection and training.
INTRODUCTION
In the United States, intensive care units (ICUs) account for 10–20% of inpatient acute care beds and 20–30% of hospital budgets. Studies have shown that the use of intensivist-led multidisciplinary teams in ICUs have positive effects on preventing adverse events, improving healthcare quality, and optimizing resource utilization. Despite these findings, however, this intensivist-led care model is hampered, among other things, by a nationwide shortage of highly trained critical care specialists.1
The rapid advance of information technology has made it possible for specialists to monitor and manage ICU patient care remotely, thus providing a potential solution to the problems created by staffing shortage. In a typical ICU remote monitoring system, a team, staffed by intensivists, critical care registered nurses, and administrative personnel, oversees a large number of ICU patients at multiple hospital sites around-the-clock from a centralized location.2 As a result, ICU remote monitoring can leverage the limited number of intensive care specialists over more patients and many hospitals. A recent study on the clinical outcomes of such a remote monitoring program has shown that providing continuous proactive care and prompt interventions resulted in reductions in mortality, patient complications, length of stay, and costs.3
The enabling technology of ICU remote monitoring requires clinicians’ work to differ significantly from conventional patient care practices in regular ICUs, particularly for registered nurses. In a typical remote monitoring facility, nurses have access to a sophisticated clinical information system, can telecommunicate with remote ICU sites through video-conferencing, and are provided with various decision-support tools in their work. Correspondingly, their major responsibilities are centered on continuously monitoring patients’ physiologic signs, assimilating large amounts of information, and making prompt clinical decisions. In contrast to attending to two or three patients in a regular ICU, a nurse working in ICU remote monitoring typically has oversight of dozens of patients. These changes highlight the need to systematically investigate nurses’ workflow in this new critical care setting.
There are several reasons why in-depth, thorough examinations of clinicians’ work in ICU remote monitoring are in demand. First, the enabling technology of ICU remote monitoring substantially changes what clinicians do at work and largely determines the characteristics of their workflow. The reengineering of clinicians’ work has several ramifications. Within the remote monitoring system, physicians and nurses need to organize and synchronize their work processes as they are redefined by the technology. Outside, the clinicians’ presence as virtual doctors and nurses highlights the need to establish constructive collaboration with bedside caregivers and develop a positive relationship with remote patients. All these are major issues of clinicians’ daily work and have a direct impact on the performance as well as clinical outcomes of ICU remote monitoring.4 In a broader sense, these issues pertain to a wide range of technology-enabled programs in medical practice as well. Therefore, research of clinicians’ work in ICU remote monitoring will not only generate meaningful results regarding the specific technology involved but also shed light on how technological advances can affect medical practice in general.
Second, clinicians’ reliance on information technology such as the integrated clinical information system suggests that the effectiveness and efficiency of ICU remote monitoring hinge, to a certain extent, on how well the technological infrastructure is designed to support clinicians do their work. An information system with user-centered functionality and interface design facilitates clinicians’ task performance. In contrast, inappropriately designed or implemented technology can severely hinder clinicians’ performance. For example, a recent study on a general-purpose computerized physician order entry system used in an ICU has shown that improving the system’s user interface had a positive effect on clinicians’ work efficiency.5 In ICU remote monitoring, a fine-grained analysis of clinicians’ workflow can provide insight into clinicians’ interaction with technology in the work process and help identify ways to improve system design for better outcomes.
Third, as the nature of nurses’ work changes, so do the requirements on an individual’s knowledge, skills, and abilities. A nurse working in a remote monitoring capacity should possess not only domain expertise in critical care but also considerable technological skills and specific cognitive capabilities in order to accomplish new tasks entailed in remote patient monitoring. Thus, researching what nurses do in such a setting will help determine these individual characteristics, information that in turn can aid in personnel selection and training.
The current research was a time-motion study of registered nurses’ workflow in ICU remote monitoring. The purpose of the study was two-fold. The first was to survey nurses’ tasks in this new critical care setting. Secondly, we wanted to investigate the impact of the enabling technology on nurses’ workflow. The results from the current study will provide us with information regarding the performance outcomes of ICU remote monitoring.
METHODS
Setting
The study was conducted in an ICU remote monitoring facility affiliated with a large healthcare system located in the Gulf Coast region of the US. The facility had been using the eICU technology developed by VISICU for 21 months at the time of the study. It remotely monitored nine ICUs with a total of 132 beds in five of the healthcare system’s member hospitals. The patients were divided up and monitored by two teams, each consisting of one physician, two nurses, and one administrative personnel. The maximum workload for each nurse during a shift was 35 patients.
For each nurse, a computer workstation provided the platform for monitoring remote patients. Among other functions, the workstation allowed a nurse to access and manage patients’ health records, video-assess bedside care, monitor live vitals, and handle system-generated early warning signals. The workstation had five monitors, stacked in two rows and arranged semi-circularly with the nurse in the center, to display all the available clinical information.
Participants
Out of the 17 nurses who worked at the facility, seven were selected to participate based on their experience with ICU remote monitoring, which ranged from six to 21 months. All participants had had more than 10 years of critical care nursing experience prior to joining the facility.
Data collection
The study was conducted over a period of two weeks. Of the seven participants, four were observed during the second half of their regular day shift (12pm – 6pm), and the other three were observed during the first half of their regular night shift (6pm – 12am). Because nurses worked with physicians in teams and physician staffing in the facility was from noon to 7am, this time frame would allow us to observe the interactions between nurses and physicians during patient monitoring while at the same time avoid the possible negative effect of late night work. Overall, the observation time for all seven participants was 40.5 hours.
One of the authors (ZT) conducted all the observations using a data collection tool (described below). The observer had expertise in behavioral science and was experienced in workflow research in critical care settings. During each observation session, the study participant was first informed of the nature of the study and encouraged to carry out duties as she normally would. Then the observer observed from behind the participant and recorded relevant information using the tool. Although the participant would occasionally explain the ongoing activities, the observation was carried out in a way as to avoid interfering with the participant’s work as much as possible.
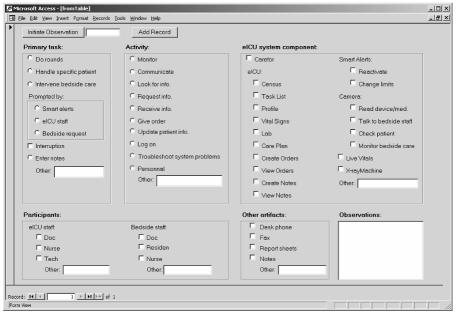
The construction of the data collection tool was based on findings from a preliminary study of nurses’ work in the same facility, and was implemented as a Microsoft Access Form application installed on a tablet PC (Figure 1). This tool allowed for structured data entry during observations. In designing the data collection tool, we used a two-level task hierarchy as the basic units of a nurse’s work: tasks and activities. A task was an event with a well-defined goal. An activity, on the other hand, was a concrete action taken towards achieving that goal. The preliminary study revealed the major types of tasks and activities nurses performed at work. While performing a task or activity, a nurse would need to use various components of the remote monitoring system and interact with individuals either in the same facility or in the remote ICUs. Accordingly, the data collection tool structured data entry into four categories: task, activity, artifacts, and participants. The observer collected information by selecting the appropriate options listed in each category on the Access form and, if needed, entering free-text notes in a data field to record additional information.
Figure 1.
Screenshot of the data collection tool used during observations
During each observation session, the observer initiated data collection by clicking a button on the form. The tool automatically recorded the system time as the start of the observation. The observer then determined the nature of the nurse’s work at this time, and recorded all relevant information on the form. As soon as the participant switched to a different task or activity, the observer clicked the “Add Record” button to conclude the current data entry and initiate a new record. The tool recorded the system time again as the end time for the just finished task as well as the start of the current task, and refreshed the form for the new entry.
Data Analysis
After data were collected from all seven participants, study-specific events such as nurses explaining to the observer or temporary suspensions of observation were discarded. This amounted to 1.7 hours or 4.2% of the overall duration. Therefore, the total valid observation time in the current study was 38.8 hours. Having examined all the remaining data, the observer slightly adjusted the 2-level task hierarchy initially defined and finalized the coding of each recorded data entry. In data analysis, the major variables of interest included the categorization of nurses’ tasks and activities, the times spent on different types of tasks and activities, and the frequency and duration of workflow interruptions. Data from all seven participants were pooled together to generate the final results.
RESULTS
Nurses’ major duties in the remote monitoring facility were to monitor patients, manage system-generated alerts, and update the clinical information system. Correspondingly, they performed a broad range of tasks at work. Overall, nurses’ tasks fell into five categories with distinctive goals.
The first category pertained to monitoring patients. The two primary tasks in this category were rounding and managing specific patients. In a rounding task, a nurse surveyed, in sequential order, the whole patient population under her watch, spending a short period of time on each patient. In managing specific patients, the nurse, prompted by certain alert signals, devoted attention to a single patient over a prolonged period of time. Managing specific patients required the nurse to assimilate clinical information from various sources, make a timely judgment, and determine what actions to take (e.g., to dismiss the alert, notify a physician, or communicate with bedside staff).
The second category was patient records maintenance, which included two tasks. The first was to transcribe patient’s admission and progress notes into the clinical information system. The second task was to fill out an information sheet for each patient for administrative purposes.
The third task category was staff collaboration. It consisted of two primary tasks. The first was shift handover, in which an outgoing nurse briefed an incoming nurse on important issues during shift change. The second task was consultation, in which a nurse, at another one’s request, gave advice regarding the other nurse’s patients.
The fourth category was specific to the use of information technology in remote monitoring. The primary tasks included setting up the workstation, logging on/off the remote monitoring system, and troubleshooting hardware or software problems.
The fifth, miscellaneous task category was of a managerial, social or personal nature. It included tasks and events such as scheduling shifts, discussing eICU-related topics, socializing with coworkers, and handling personal matters.
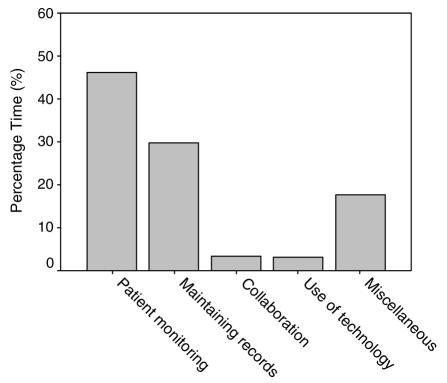
The times that the participants spent on different task categories are shown in Figure 2. As can be seen in Figure 2, nurses spent 46% of their time monitoring patients, 30% on maintaining patient records, 3% each on collaboration and technology-specific tasks, and the remaining 18% on miscellaneous tasks.
Figure 2.
Nurses’ time allocation on different task categories.
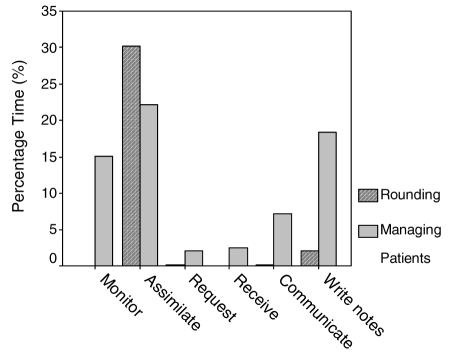
As rounding and managing specific patients were the two primary mechanisms through which nurses monitored remote patients, we further analyzed the activities nurses performed during these two tasks, focusing primarily on the information flow in the processes. The results showed that there were six major activities including: (1) Monitor remote patients’ live vitals; (2) Assimilate information embedded in various places in the clinical information system; (3) Request information not available in the system but necessary for making a clinical judgment; (4) Receive information from other staff; (5) Communicate with other clinicians about a patient’s condition; and, (6) Write notes about interactions with bedside staff in the clinical information system.
Figure 3 shows the percentage times nurses spent on the six information-centered activities in rounding and managing specific patients. The total duration of patient monitoring was 17.9 hours. As can be seen in Figure 3, the predominant activity in rounding was to assimilate information. It accounted for 30% of the total patient monitoring time as compared to just 2% that nurses spent writing notes in this process. On the other hand, when a patient’s condition warranted a thorough examination, managing that specific patient encompassed a broader range of activities. Overall, nurses spent 22% of the time assimilating information and 15% monitoring live vitals. The times they spent on communicating, requesting and receiving clinical information were 7%, 2%, and 3% of the total duration, respectively. Nurses spent another 18% of the time writing notes in the clinical information system to document how these specific situations were handled.
Figure 3.
Nurses’ time allocation on different activities while monitoring patients.
One of the most important characteristics of nurses’ workflow in remote patient monitoring was that they were frequently interrupted in the middle of tasks and activities. An interruption was defined as the suspension of a current task or activity due to managing an unexpected event. The results from the current study showed that each of the seven participants was interrupted 25 to 70 times over an observation period of approximately six hours. Overall, there were 296 interruptions during 38.8 hours of valid observation, resulting in an average of 7.6 interruptions per hour per nurse. The majority of the interruptions (87% of all) were triggered by the need to immediately attend to specific patients. Other sources of interruptions included requests to provide consultation to another nurse, shift scheduling, and handling personal matters. The time spent on managing an interruption ranged from a few seconds to over 10 minutes, with a median duration of approximately 20 seconds.
DISCUSSION
The current research aimed to investigate registered nurses’ work process in ICU remote monitoring, a relatively new, technology-driven critical care setting. Overall, the results show that nurses’ essential tasks revolved around three themes: monitoring patients, maintaining patients’ health records, and managing technology use. Nurses monitor remote patients either through rounding, in which they serve as a general monitoring mechanism for a large number of patients, or by selectively attending to specific patients. Monitoring patients requires nurses to use the enabling technology to assimilate, communicate, and upkeep large amounts of clinical information. These findings emphasize the information-centered nature of nurses’ work in this unique critical care setting.
The current results also show that nurses’ workflow is characterized by frequent interruptions. The majority of the interruptions were initiated when the remote monitoring system detected abnormality in a patient’s condition. By responding promptly (i.e., switching from an original task to managing the specific patient), nurses are able to address the issues at an early time. Therefore, nurses’ workflow redirection is necessary and important for delivering proactive care in ICU remote monitoring. Frequent interruptions, however, can have negative effects on clinicians’ task performance. Not only do interruptions postpone the completion of the original tasks, but more importantly the delays caused by handling interruptions significantly increase an individual’s cognitive load when returning to the previous tasks, thereby increasing the chance for errors.6 Given the fact that automatically generated alerts are a built-in component of the eICU remote monitoring mechanism, the current results thus highlight the need for improved system design to support nurses’ interruption-driven workflow.
Taken together, the results from the current study reveal nurses’ workflow in ICU remote monitoring as shaped by the enabling technology. Nurses’ need to assimilate large amounts of clinical information and frequently switch between tasks emphasize that the system should be well designed to support nurses perform their duties. In addition to this, the current results can also aid in a number of practical matters, including work design and standardization, personnel selection, and training.
Using advanced remote monitoring technology to bring highly trained specialists to a large number of patients in multiple ICUs is a relatively new approach to critical care. This approach is technology-driven and as a result brings about substantial changes to physicians’ and nurses’ medical practice. There is a great need to investigate the implications of these changes, not only in terms of clinical outcomes but also at behavioral, organizational, and societal levels. The current research is among the first to evaluate the performance outcomes of ICU remote monitoring, yet more work is needed in order for us to gain a comprehensive understanding of this new approach to critical care.
ACKNOWLEDGEMENTS
This project was supported in part by the Agency for Healthcare Research and Quality (AHRQ) grant 1RO1HS15234. The views expressed here are those of the authors and do not necessarily reflect the policy or position of the funding agency.
REFERENCES
- 1.Kelley MA, Angus D, Chalfin DB, Edward DC, Ingbar D, Johanson W, Medina J, Sessler CN, Vender JS. The Critical Care Crisis in the United States: A Report From the Profession. CHEST. 2004;125:1514–1527. doi: 10.1378/chest.125.4.1514. [DOI] [PubMed] [Google Scholar]
- 2.Celi LA, Hassan E, Marquardt C, Breslow M, Rosenfeld B. The eICU: It’s not just telemedicine. Crit Care Med. 2001;29(Suppl):N183–N189. doi: 10.1097/00003246-200108001-00007. [DOI] [PubMed] [Google Scholar]
- 3.Rosenfeld BA, Dorman T, Breslow MJ, et al. Crit Care Med. 2000;28:3925–3931. doi: 10.1097/00003246-200012000-00034. [DOI] [PubMed] [Google Scholar]
- 4.Peters SG, Farmer JC. Con: Is the tele-intensive care unit ready for prime time? Crit Care Med. 2004;32:288–290. doi: 10.1097/01.CCM.0000104927.48799.62. [DOI] [PubMed] [Google Scholar]
- 5.Ali NA, Mekhjian HS, Kuehn L, et al. Crit Care Med. 2005;33:110–114. doi: 10.1097/01.ccm.0000150266.58668.f9. [DOI] [PubMed] [Google Scholar]
- 6.Brixey JJ, Robinson DJ, Tang Z, Johnson TR, Turley JP, Zhang J. Interruptions in workflow for RNs in a level one trauma center. Proc AMIA Symp. 2005:86–90. [PMC free article] [PubMed] [Google Scholar]