Abstract
We have developed a system for real-time patient monitoring during large-scale disasters. Our system is designed with scalable algorithms to monitor large numbers of patients, an intuitive interface to support the overwhelmed responders, and ad-hoc mesh networking capabilities to maintain connectivity to patients in the chaotic settings. This paper describes an iterative approach to user-centered design adopted to guide development of our system. This system is a part of the Advanced Health and Disaster Aid Network (AID-N) architecture.
INTRODUCTION
Response to mass casualty incidents (MCIs) poses numerous challenges to the emergency medical services (EMS) community. Responders must care for an overwhelming number of patients with limited personnel and medical resources. EMS officers must coordinate transport for patients, often with insufficient information from responders in the field. In this chaotic environment, patients with minor injuries often depart the scene without notifying the response team; thus creating an organizational headache for EMS officers who are responsible for tracking the whereabouts of each patient.
Rapid and accurate triage of patients is a critical step in the response process. In three jurisdictions nearby the Washington DC metropolitan region, initial triage at the site of an incident involves attaching red, yellow, green or black colored paper tags to patients based upon assessed priority. Triaged patients wait at the scene until their designated ambulance arrives. With an understaffed response team, patients may wait for an extended period of time before transport. During this waiting period, patient conditions may deteriorate. Secondary injuries such as hypoxemia, hypotension, intracranial bleeding, and cardiac tamponade may become life-threatening if not treated immediately. To address these problems, current emergency response protocols require paramedics to periodically re-triage patients.1 To perform re-triage, medics need to measure patient vital signs to check for various cardiac and respiratory conditions. At the University of Maryland Baltimore County, medics are taught to re-triage every 5 minutes for red priority patients, every 10 minutes for yellow priority patients, every 15 minutes for green priority patients. In an MCI, however, this important protocol is often neglected by the overwhelmed responders.2
Technologies that monitor vital trends and detect the onset of fatal conditions may facilitate the timely treatment of patients in need. Unfortunately, there are systems available for mass casualty monitoring. Monitoring packs used by responders during routine ambulance runs can only track the vitals sign trends of a single patient.3 Bedside monitoring systems can track multiple patients, but require mainframe computing systems that are not suitable for field use.4
In collaboration with EMS in the DC region, we have developed a next-generation patient monitoring system to address the unsolved problems discussed above. This system incorporates electronic triage tags that continuously detect patient vital signs and location in indoor and outdoor environments.5 These electronic tags communicate over an ad-hoc wireless mesh network to a base station.6,7 The base station monitors and sorts patients, validates the accuracy of triage assignments, and signals critical changes. By allowing accurate and simultaneous monitoring of mass casualties, this system could greatly relieve responders’ workload, increase the quantity of patient care, identify those in need of rescue, and prioritize emergency care when resources are limited. Furthermore, this system may identify casualties who are physiologically unsavable and prevent the endangerment of responders during hazardous rescue conditions. The remainder of this paper describes the design considerations and preliminary evaluation of our patient monitoring system.
METHODLOGY
The following section describes methodology for two key aspects of our design: 1) vital signs monitoring and 2) usability engineering.
Vital signs monitoring
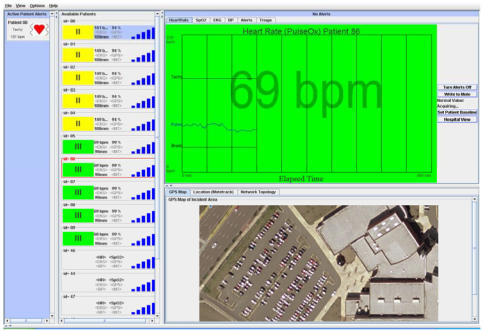
The design process was to select vital signs to be measured, assess sensor candidates, and design scalable algorithms for vital sign trends analysis. Based upon current protocols and discussions with paramedics, candidate vital signs are: 1) temperature, 2) pulse, 3) blood pressure, 4) respiratory rate, 5) oxygen saturation, 6) peripheral vascular perfusion, 7) mental status, and 8) electrocardiography. We narrowed this list of candidates based upon the performance of available sensors. To appraise sensor performance, we gathered a large list of noninvasive sensors and weighed each sensor upon the following criteria: 1) ease of use, 2) portability, 3) wearability, 4) ruggedness, 5) power consumption, and 6) capability of providing continuous vital sign data. Those that best fit these criteria were a blood pressure cuff, pulse oximeter, and a two-lead electrocardiogram. Next, we conducted an anonymous survey of six medics with over 90 years of combined exerience to assess the importance of the candidate vital signs to user needs. Respondents were asked to rank vital signs on a 7 point likert scale. Our results, as shown in Figure 1, indiated that pulse rate and oxygen saturation were rated to be the most important vital signs. Based upon this analysis, we decided to use pulse oximeter as the primary sensor for the electronic tag. We also implemented a wireless blood pressure cuff as a separate module that could be applied to patients who required the additonal level of monitoring.
Figure 1.
Importance of vital signs for patient monitoring
We developed vital signs analysis algorithms based upon published detection methods implemented by existing patient monitoring products.8–10 Paramedics and physicians were queried to determine which vital sign trends should be detected.11–13 To stimulate discussion, the interviewees were supplied with a list of the hypothetical cardiovascular and respiratory complications and asked them to review how they would detect these conditions using vital sign trends.
The detection algorithms were evaluated using manually-created scripts of vitals signs data. The ventricular tachycardia detection algorithm was tested with electrocardiogram recordings in the MIT-BIH arrhythmia database.14 We tested the use of our sensor under a range of conditions expected at an MCI.
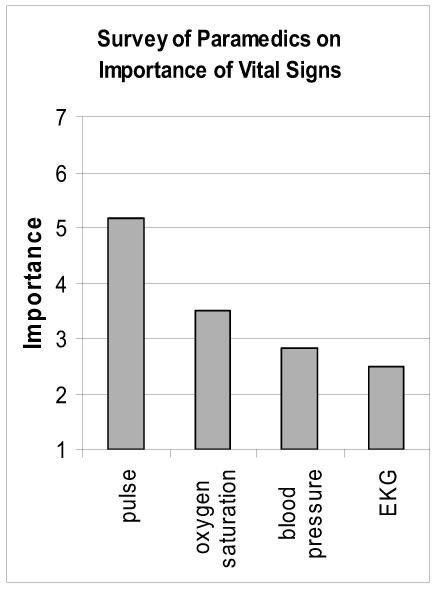
Usability Engineering
Our base station user interface, Figure 2, evolved through multiple iterations of rapid prototyping and user feedback. Initial iterations gathered input from a broad range of EMS personnel, technologists, and usability experts through cognitive walkthroughs, usability reviews, and round table discussions. Final rounds of iterations used interviews to focus on individual user needs. Each iteration and its implication on our design are described below.
Figure 2.
Graphical user interface of patient monitoring station
Upon completion of an initial prototype, we conducted cognitive walkthroughs with five technology exhibitors with paramedic experience at the 2005 Fire, Rescue, and EMS Expo.15 Feedback from these cognitive walkthroughs prompted implementation changes to the following:
Customize detection algorithms to each patient
Sort patients based upon priority levels and waiting times
Enable the ability to turn off alerts for any patient
In the second round of development, walkthroughs were conducted with two experienced user interface designers and two medical informaticians. We gathered feedback on the layout, font and image sizes, wording of components in the interface. Input from these sources led us to implement changes to:
Provide warnings to indicate alerts are turned off
Set icons and text to universally accessible colors schemes and provide customization options
Save text in files that can be easily modified or translated to specialized language in the future
In the third round of development, we presented our technology to two large group roundtable discussions involving paramedics from Baltimore/Washington International (BWI) Airport Fire and Rescue Department and Arlington County EMS. Feedback from these participants led us to modify features to:
Align status codes with commonly accepted color codes (pink =stable, blue=critical)
Provide warnings about changes in status codes instead of automatically triaging patients
In later rounds of development, we conducted one-on-one interviews with paramedics with disaster experience. Multiple iterations of user reviews allowed us to continuously improve our user interface to meet expressed needs. As a final evaluation, we conducted two anonymous surveys of experienced EMS personnel.
IMPLEMENTATION
When a patient is first triaged, a paramedic attaches the electronic tag to the patient’s neck or wrist, places the pulse oximeter on the patient’s ear or finger, and presses a button on the electronic tag to set the patient’s triage color. The electronic tag automatically starts transmitting data to a base station. The base station forwards the patient information in real time to a remote patient record database for storage and transmission to receiving hospitals. Base stations use Verizon EVDO wireless cards to attain high speed network connectivity for communication with the remote server. We integrated our system with a pre-hospital patient care software system currently used on all ambulances in Arlington County, VA. The following sections describe five areas of our implementation: 1) wearable devices, 2) vital sign analysis, 3) patient management, 3) reducing false alerts, and 4) usability engineering.
Wearable Devices
We developed the wearable electronic tag to provide five functionalities: vital sign monitoring, location tracking, medical record storage, triage color signaling, and alarm signaling. We integrated two types of location sensing capabilities – a GPS and an indoor tracking system to provide location in areas where GPS satellite signals cannot reach. The indoor location sensor, based on MoteTrack developed at Harvard University, requires installation of location beacons.16 In collaboration with Montgomery County Department of Homeland Security, we are installing location beacons at a designated indoor triage and treatment center near Washington DC.
Vital Sign Analysis
Table 1 shows a list of the monitored patient conditions.Our algorithm customizes to each patient using several novel techniques:
Table 1.
Alerts raised by vital sign analysis algorithms
| Alert Category | Alert |
|---|---|
| Cardiac | No pulse |
| Bradycardia | |
| Tachycardia | |
| Onset of change | |
| Stability | |
| Oxygen Saturation | Low oxygen saturation |
| Onset of change | |
| Blood Pressure | Systolic pressure |
| Diastolic pressure | |
| Widening pulse pressure | |
| Narrowing pulse pressure | |
| Mean arterial pressure | |
| Change |
If the patient has a medical record that has been previously entered, information from the medical record is used to adjust the alert detection thresholds.
Thresholds are customized based upon environmental factors including altitude and temperature.
Thresholds are programmatically adjusted based upon a patient’s current readings.
Paramedics can adjust thresholds on a patient by patient basis by selecting the “Alert Parameters” option and manually updating thresholds.
Each patient’s thresholds are transmitted to the remote patient record database for later retrieval. If there is no network connectivity to the remote server, the medic can choose to store thresholds patient tag by selecting the button “Write PCR to Mote.”
Patient Management
The user interface displays summary panels for all patients that contain the patient ID, triage color, wireless connection strength, and latest vital signs. All the patient summary panels are listed in one scrollable panel, sorted by priority and length of waiting time. When a paramedic clicks on a patient summary panel, that patient’s vital sign graphs are displayed in a graph area. This dashboard approach allows the user to maintain an overview of all patients while drilling down to the details of a single patient.
When an anomaly is detected in the patient vital signs, an alert appears on the user interface. All current alerts are listed inside a panel, making multiple alerts easy to manage. The paramedic can locate a patient in trouble by selecting a “Ring Patient Audio” feature, which will sound a buzzer and blink the lights on the patient’s electronic tag.
Reducing False Alerts
The default thresholds in the analysis algorithm cannot accurately analyze every person. Hence, our algorithm customizes its detection thresholds for each patient. A paramedic has additional options to deal with false alarms. The algorithm averages the data to supress single data points spikes caused by environmental noise or network glitches. A single data point over a threshold cannot set off an alarm. Finally, we allow users to override system alerts by turning off the alert detection for any patient. We warn paramedics of their action and add an “alerts off” icon to the corner of the patient summary panel.
Usability Engineering
User interfaces must be as simple and easy to use as possible. The inherent overload of information at a MCI, makes it challenging to select only the most important data to be displayed on a single screen. Table 2 summarizes the design principles we have discovered and implemented through our iterative design process.
Table 2.
User interface design principles for MCI patient monitoring systems
| Principle | Application to emergency medical response applications |
|---|---|
| Learnability | Provide guidance for tasks: Display descriptive text when cursor hovers over a button. |
| Provide visual feedback to users’ actions: Use a marker to indicated when a patient’s electronic tag is turned off | |
| Familiarity | Use familiar abbreviations such as triage symbols. |
| Match the system with current practices: Integrate systems to in non-disruptive ways to promote use during routine ambulance runs. | |
| Use common conventions for symbols and text: Label with roman numerals commonly printed on paper triage tags. | |
| Simplicity | Hide unnecessary functionality: Tabs and menus hide action buttons. |
| Provide non-redundant information: Deploy an overview pane that shows essential vital signs while hiding other details. | |
| Relieve user workload: Automatically customize monitoring algorithms for individual patients. | |
| Accessibility and Customizability | Enable customization of language, font, and font size. |
| Consider colorblind accessibility: Label red, yellow, green, and black triage colors with I, II, III, an IV symbols respectively. | |
| Provide multiple types of alarms: Incorporate alarms that can be displayed on the software, buzz on the patient’s device, blink on the patient’s device, or be turned off. | |
| Minimize Errors | Prevent user mistakes: Use a password button on the electronic tag to prevent patients from triaging themselves. |
| Minimize false alarms: Auto-adjust vital signs monitoring thresholds based on patient age and height. | |
| Recoverability | Plan for failures: Continuously save state of the system. If the computer crashes, users can restart from previously saved states. |
| Plan for unreliable networks: Incorporate ad-hoc wireless mesh networking capabilities. |
RESULTS
In order to ensure its applicability in the field, we have solicited evaluations of the proposed system design from actual EMS field personnel. Emergency Medical personnel at the Arlington Fire Department were surveyed for their opinions on different aspects of the AID-N system. The audience included captains, platoon chiefs, and paramedics with a cumulative 90 years of EMS experience. After conducting a demonstration to the personnel, a questionnaire was completed by each participant about the perceived utility and functionality of the different features. The overall system itself was received positively, and much of the input taken from the participants has already been implemented into the most recent design. Six paramedics at the Arlington Fire Department completed anonymous survey. Figure 3 show the average ratings from the surveys. Aspects of the system considered most useful were the feature allowing the patients to be listed by color and the ability to buzz electronic tags to locate patients in a crowd. The alarm monitor that provides alerts when vital signs fall out of a certain range was rated highly. The features that received highest ratings were those that facilitated triaging. The features that received the lowest ratings were those that helped to located patients. These results were not surprising, as paramedics typical monitor patients in relatively small cordoned areas, and the GPS would not allow them to discriminate between locations within such confines.
Figure 3.
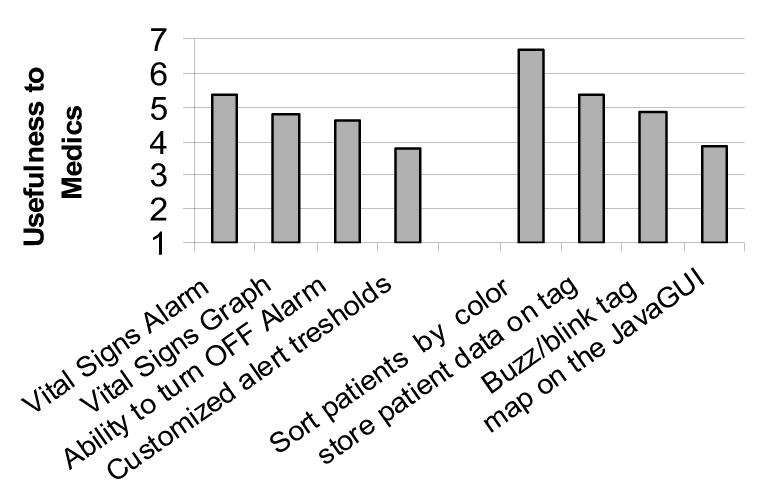
Results from survey of paramedics on the usefulness of various system
DISCUSSION
Our system offers many benefits over the current paper based system of triaging and tracking patients. While designing our system, our team collaborated extensively with medical professionals to identify their greatest needs. We acknowledge that our patient monitoring feature may not be useful in all situations. In an MCI when paramedics must triage many casualties quickly, they may not have time to respond to individual patient alerts until all patients have been triaged. The paramedics whom we interviewed predicted that our monitoring system would be most useful in situations where patients have been triaged and are waiting for ambulances. Our system could be used to prioritize patients who need to be transported by ambulance. The hardware and software prototypes we have developed hold promise for improving the efficiency of emergency response workflows.
Our system is currently being prepared for use in a simulated MCI exercise to take place in August 2006. This exercise will be conducted in partnership with Suburban Hospital, Johns Hopkins Hospital, and Montgomery County Fire and Rescue Service. During this exercise, comparisons between the effectiveness of current disaster response methodologies and our system shall be conducted.
ACKNOWLEDGEMENTS
This work was supported by the National Library of Medicine through grant N01-LM-3-3516. The authors would like to thank physicians at Suburban and Johns Hopkins for their medical expertise; EMS personnel in Baltimore and Montgomery County, MD and Arlington County VA for insight into first responders’ line of work; and the professors at University of Maryland Department of Emergency Health Services for guidance on EMS protocols and trends.
REFERENCES
- 1.FEMA Medical Team Training Manual. Available at http://www.fema.gov.
- 2.Interviews with Polk, D., MSW, NREMT-P, Paramedic Program Instructor at the University of Maryland Baltimore County Department of Emergency Health Services.
- 3.LifePak 12 Monitoring System; Medtronic Inc. Available at http://www.medtronic.com.
- 4.Visicu eICU Solutions, Visicu. http://www.visicu.com.
- 5.Gao T, Greenspan D, Welsh M. Vital Signs Monitoring and Patient Tracking Over a Wireless Network. Proc IEEE EMBS Annual International Conference. 2005 doi: 10.1109/IEMBS.2005.1616352. [DOI] [PubMed] [Google Scholar]
- 6.Lorincz K, Welsh M. Sensor Networks for Emergency Response: Challenges and Opportunities. IEEE Pervasive Computing. 2004 Oct–Dec;:16–23. [Google Scholar]
- 7.Hill J, Szewczyk R, Woo A, et al. System Architecture Directions for Networked Sensors. Proc. 9th Int’l Conf. Architectural Support for Programming Languages and Operating Systems. 2000:93–104. [Google Scholar]
- 8.Cardiac Arrest Associated With Trauma, Circulation. Circulation. 2005;112(24):IV 146–IV 149. [Google Scholar]
- 9.Schwartz GR. Principles and Practice of Emergency Medicine. King of Prussia, PA: Rittenhouse Book Distributors; 1999. [Google Scholar]
- 10.Behrman RE. Nelson Textbook of Pediatrics. Philadelphia, PA: W.B. Saunders Company; 2000. [Google Scholar]
- 11.Interviews with Lehmann H, MD, PhD, Associate Professor of Health Sciences Informatics, Johns Hopkins Medicine.
- 12.Interviews with Mitchell J, Paramedic Program Instructor at the University of Maryland Baltimore County Department of Emergency Health Services.
- 13.Interviews with Don Alves, MD, ER physician at University of Maryland Medical Center.
- 14.Goldberger AL, Amaral LAN, Glass L, et al. PhysioBank, PhysioToolkit, and PhysioNet: Components of a New Research Resource for Complex Physiologic Signals. Circulation. 101(23):e215–e220. doi: 10.1161/01.cir.101.23.e215. [DOI] [PubMed] [Google Scholar]
- 15.Firehouse Expo. Fire, Rescue, and EMS. Baltimore, MD: Jul–30. 2005. [Google Scholar]
- 16.Lorincz K, Welsh M. Divison of Eng and Applied Sciences. Harvard Univ; 2004. A Robust, Decentralized Approach to RF-Based Location Tracking, tech. report TR-19-04. [Google Scholar]