Abstract
The Emergency Department is a suitable but challenging environment to implement a sustainable pneumococcal vaccination program. To increase vaccination rates for patients ≥65 years old, we prospectively evaluated a closed-loop informatics approach over a 6-week study period. Among the 572 candidate patients, 284 were up-to-date with vaccination, 187 patients refused vaccination, 65 physicians declined to order the vaccine, and 28 patients received the vaccine during the ED visit. The informatics approach increased vaccination rate from a baseline of 49.8% to 54.9% (p < 0.01).
INTRODUCTION
Pneumococcal vaccination is recommended for patients ≥65 years old and patients <65 years with co-morbid illnesses. However, current vaccination rates remain far below the Healthy People 2010 target of >90%. The Emergency Department (ED) has been recommended as a suitable environment for vaccine administration. Computerized reminders have proven successful at increasing vaccination, but this has not been applied in the ED. We prospectively evaluated a “closed-loop,” informatics-based reminder system on vaccination rates in the ED. The system was embedded in the clinical workflow and included 4 different information systems: the electronic patient record (EMR), the computerized triage application, the computerized provider order entry (CPOE), and the order tracker application.
METHODS
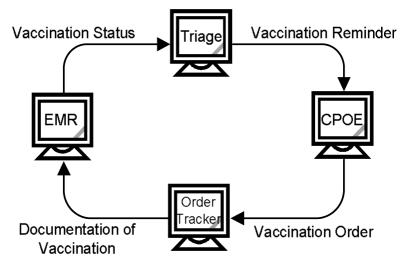
We included all patients ≥65 years old presenting to the adult ED during a 6-week study period (1/30/06-3/08/06). We excluded patients with the highest acuity level and patients without computerized triage documentation. The triage nurse documented current pneumococcal vaccination status based on information from the patient and the EMR problem list (Figure 1). The system determined eligibility based on vaccination status, age, and year of prior vaccination. For eligible, consenting patients the CPOE system prompted physicians for a vaccine order once at the end of the first ordering session. The nurse documented vaccination administration in the order tracker system, which was automatically added to the health maintenance section in the EMR. The system captured refusal reasons from patients or physicians. The study was approved by the IRB.
Figure 1:
Closed-loop information flow.
RESULTS
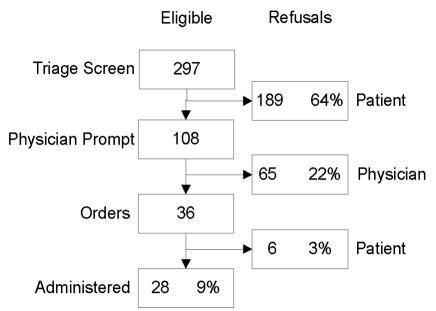
Among the 572 patients ≥65 years old, 284 (49.8%) were up-to-date and 288 (mean age 80.5±11 years, mean acuity level: 2.3±0.6) were eligible to receive the vaccine. Figure 2 displays the results. The most frequent patient refusal reasons were: “Vaccination is not necessary” (12.7%) and “I prefer my own primary care physician” (18.5%). The most frequent physician refusal reasons were: “Unable to verify eligibility” (30.8%) and “Not enough time” (9.23%).
Figure 2:
Eligible patients.
DISCUSSION
The closed-loop, informatics-based reminder system increased vaccination rates in the ED and created a sustainable, workflow-embedded, point-of-care infrastructure for a pneumococcal vaccination program in a challenging environment.
Acknowledgements
This study was supported by NLM T15 007450-03