Abstract
Introduction
“Infobuttons” have been proposed as a potential solution for lowering access barriers to on-line information resources at the point-of-care. The aim of this study is to describe the infobuttons infrastructure at Intermountain Healthcare and assess their use after 4 years of their initial release.
Methods
infobuttons are currently implemented in the problem list, laboratory results, and medication order entry modules of a web-based Clinical Information System. A software component called “E-resources Manager,” provides the infrastructure for the configuration of infobuttons without requiring any programming. A 4 year period of infobuttons use was analyzed using log data.
Results
in the past four years, infobuttons were used 53,127 times by 2,611 unique users. Usage has been constantly increasing and currently approximately 300 users access the infobuttons every month. Despite the high utilization, a small subset of users account for the majority of the infobutton sessions.
Conclusion
the continuous growth in use since the initial release confirms the usefulness of infobuttons. However, additional research and development is still needed before full benefits can be achieved.
Introduction
It has been well documented that physicians have a large number of information needs while taking care of their patients, and that most of these information needs are not met [1,2]. On-line health information resources (“e-resources”) are now widely available and have a great potential to solve part of these information needs. However, the use of e-resources at the point-of-care remains low, even with the ubiquity of the Internet, and most questions at the point-of-care are still left unanswered [2]. A possible explanation for such a low utilization is the fact that significant barriers still prevent the widespread use of e-resources at the point-of-care [2]. Candidate solutions for reducing these barriers should focus on the retrieval of relevant information in view of the context at which an information need occurs, without disrupting the care provider workflow.
Information retrieval tools called “infobuttons” have been developed in various institutions, with the intent of integrating Electronic Medical Records (EMR) with e-resources [3–5]. The term “infobutton” was first proposed by Cimino and it can be defined as information retrieval tools that automatically generate queries to e-resources using contextual information and patient data extracted from the EMR [3].
The infobutton icons are normally placed right next to clinical data elements commonly found in an EMR system (e.g., medication orders, laboratory results). When an infobutton is clicked, the user is presented with a list of questions about the data element of interest and a list of e-resources that cover the domain of the questions under consideration. When the user selects one of the questions, a search request is sent to the target e-resource, which can return a web page with search results or a specific document.
Background
Intermountain Healthcare (“Intermountain”) is a not-for-profit integrated delivery system of 21 hospitals, over 70 outpatient clinics, an employed physician group with over 500 physicians, and an insurance plan located in Utah and southeastern Idaho.
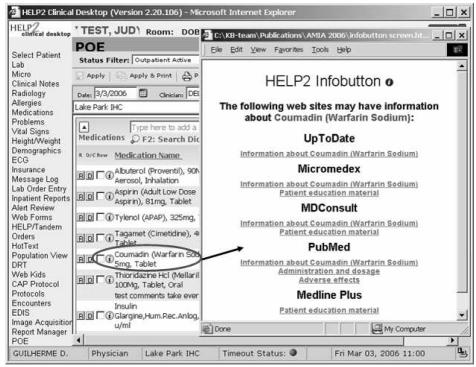
Clinicians at Intermountain have access to a web-based EMR called HELP2. HELP2 offers access to a wide variety of data and functions, including laboratory results, clinical notes, problem lists, and medication order entry [6]. Infobuttons were first released in HELP2 in September of 2001 in the medication ordering (outpatient), problem list, and laboratory results modules (Figure 1) [4].
Figure 1.
A HELP2 order entry screen, showing infobuttons (left) and the resulting page when the infobutton next to the medication “Coumadin (Warfarin)” is selected.
The HELP2 infobuttons use coded clinical data from the Intermountain clinical data repository (CDR) to generate search requests to e-resources. All CDR coded data values are maintained within a terminology server. Using services provided by the terminology server, each coded data value can be translated into suitable “free-text” search terms or codes from standard sources, such as ICD-9-CM, LOINC, and the National Drug Codes (NDC).
Examples of e-resources currently in use at Intermountain include MDConsult, Clin-eguide, Micromedex, UpToDate, and PubMed. These resources were selected as part of a corporate evaluation process conducted in 2002 by Intermountain librarians and the authors of this paper. In addition to infobuttons, these resources are also available at an “e-resources page,” which can be easily accessed from the HELP2 navigation menu.
Infobuttons infrastructure
The initial implementation of the HELP2 infobuttons had a number of limitations. The lack of an independent software component required each HELP2 module to have its own infobutton implementation. In addition, the infobuttons were not configurable, therefore modifications to e-resources required changes to each individual infobutton implementation in HELP2. These limitations restricted the number of e-resources that could be enabled to infobuttons.
In 2004, a software component called “E-resources Manager” (ERM) replaced the first infobutton implementation, resolving the limitations described. The ERM is conceptually similar to the Infobutton Manager proposed by Cimino et al. [7]. The ERM consists of 1 core component and 3 processes: “e-resource profiles,” “context matching,” “question generation,” and “query translation.”
The e-resource profiles are XML documents that identify the context in which an e-resource can provide applicable content and the query syntax that the resource uses to express these parameters. Context in the ERM can be expressed in terms of the task performed by the user in the EHR when the infobutton is clicked, gender, age groups, clinical concepts that the resource covers, and the discipline(s) that the resource focuses on.
With the release of the ERM we were able to configure infobutton links to resources that cover specific clinical domains (“domain-specific resources”). For example, in December 2005, we created profiles for two domain-specific resources: the National Library of Medicine’s Genetics Home Reference (GHR) and GeneTests, both offering content specific to genetic conditions [8, 9].
Other examples of domain-specific resources are content collections developed for internal use at health care organizations. As an example, we enabled problem list infobuttons links to Intermountain’s Care Process Models (CPMs), which provide guidance on the management of common conditions such as Diabetes, Asthma, and Depression.
Domain-specific resources are offered to the user only if the main concept of interest is covered by the resource. Domain-specific resources are always listed at the top of the infobutton page, with the assumption that a better answer will be more easily found on a more focused and specialized resource than on a generic one. Subsequent resources are ordered based on how often they are used within a specific context.
The e-resource profiles are stored in Intermountain’s Clinical Knowledge Repository (CKR), a corporate database used for managing knowledge assets that are relevant to applications such as HELP2. The profiles are created using a generic knowledge authoring tool that was developed to allow clinical experts to create knowledge content minimizing the dependencies on information technology personnel [10]. New profiles become instantly available to infobuttons, without requiring any changes to the ERM or HELP2.
When the ERM receives an HTTP request from HELP2 via its application program interface (API), the context matching process executes, using the profiles to identify the resources that match the context captured by the infobutton. Next, using the profiles of the selected resources, the question generation process creates the questions that each of the matching resources are able to handle, and presents these questions as hyperlinks in an HTML page. When the user selects one of the questions, a new request to the ERM is made, invoking the query translation process, which translates the parameters embedded in the selected question into the specific syntax of the target resource. Likewise, coded concepts are translated using the terminology server described in the previous section. Finally, an HTTP request is submitted to the target e-resource.
Infobuttons utilization
Infobutton utilization data from January 1st, 2002 to January 31st, 2006 were extracted from the CKR monitoring tables and then loaded into an MS Access database. All monitoring records associated with information technology personnel and fictitious patients used for testing or training purposes were systematically removed. The main unit of measurement was the “infobutton session,” defined as a click at an infobutton followed by the selection of one of the resources presented on the infobutton page.
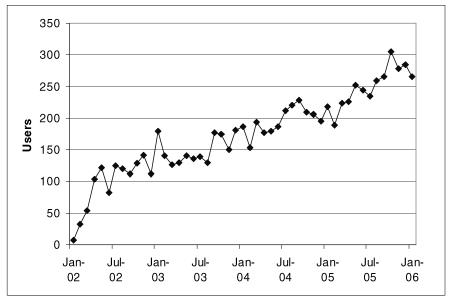
The monitoring data indicated that 2,611 users accessed the infobuttons, resulting on 53,127 infobutton sessions total. Figure 2 shows the number of unique users per month during the study period, indicating a steady growth in the use of infobuttons.
Figure 2.
number of unique infobutton users per month from January 2002 to January 2006.
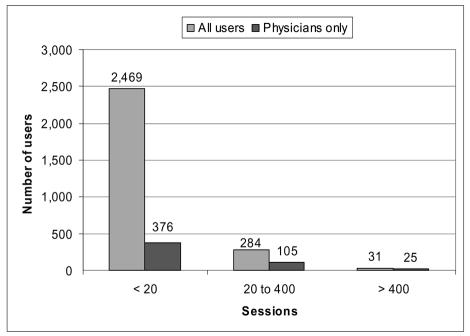
The average number of total sessions per user was 20.4, and the median was 2. The usage range was from 1 to 2,528 sessions per user, representing a very skewed distribution, apparently with 3 distinct types of usage pattern: daily users (more than 400 sessions), sporadic users (20 to 400 sessions), and “trial users,” i.e. users who tried infobuttons a few times and rarely used them again (less than 20 sessions). When looking only at physician users though, the average number of sessions per user was 66.9 and the median was 5, resulting on a less skewed distribution (Figure 3).
Figure 3.
distribution of total infobutton sessions per user (all users and physicians only) indicating 3 different types of usage pattern.
On average, 31 users clicked on an infobutton more than 10 times a month, but this number increased to 41 in the last 12 months. Regarding user discipline, physicians accounted for most of the sessions (69% of the sessions), followed by nurses (26%).
When grouped by the CIS module where the infobutton was located, 73% of the sessions came from the medication ordering module, 19% from laboratory results, and 8% from the problem list module. In 9% of the sessions, users looked for patient education handouts.
As far as e-resources, after obtaining the average number of sessions per month from each e-resource (some e-resources were not available during the entire period), Micromedex accounted for 44%, UpToDate for 23%, Clin-eguide for 18%, MDConsult for 11%, and PubMed for 2% of the sessions. Micromedex was the most common resource for medication ordering infobuttons (63% of the sessions), MDConsult the most common for problems (77%), and Clin-eguide the only option for laboratory results. More than half (55%) of the MDConsult sessions were conducted to obtain patient education handouts.
When looking at the main concept searched during an infobutton session, users looked up information on 3,247 medications, 487 lab tests, and 887 problems. Applying the 80/20 rule, 93 laboratory tests accounted for 80% of the laboratory infobutton sessions, 834 medications accounted for 80% of the medication ordering sessions, and 302 problems accounted for 80% of the problem list sessions. The 3 most frequent medications were Tramadol (3.7% of the medication ordering infobutton sessions), Escitalopram (2.9%), and Metmorfin (2.6%). The 3 most frequent laboratory tests were leukocytes count (3.7%), platelets count (2.9%), and BUN (2.6%). Finally, the 3 most frequent problems were Headache/Migraine (3.5%), Diabetes (3.1%), and Hypertension (2.2%).
Discussion
Different contexts in the healthcare workflow will lead to specific sets of information needs that are still not well understood, especially when information systems are an integral piece of the process [10]. In addition, a wide variety of specialized resources is normally required to answer each particular information need. This has been demonstrated by Ely et al., who found out that no single resource accounted for more than 7% of the answers to the questions that primary care physicians had in an outpatient setting [2]. Finally, each e-resource application program interface (API) adopts its own “dialect,” both in terms of syntax and terminology, complicating even further the integration between clinical systems, infobuttons, and e-resources. Given these factors, it is of great importance to have a software component that simplifies the implementation, configuration, and maintenance of infobuttons. Ultimately, this software component has to enable quick adaptations that result from additional knowledge about information needs and the increasing availability of new and specialized resources.
Other initiatives, such as the “infobutton communication standard” currently being developed by HL7, should also facilitate the implementation and maintenance of infobuttons [12]. The emerging standard should also help e-resources redefine their indexing strategies, search engines development, and content structures to more directly answer clinicians’ information needs at the point-of-care, a requirement that has been previously identified by Ely et al. [2].
By monitoring infobutton utilization, we have been able to understand the contexts in which infobuttons have been most successful in our institution, as well as to identify areas that need improvement. Our data are similar to other institutions in terms of users and sessions. Maviglia et al., for example, reported a total of 7,972 sessions and 359 users during the first year of infobutton use at Partners HealthCare [5]. Although we had 18,360 infobutton sessions and 1,311 users at Intermountain in 2005, the use of infobuttons during our first year is very similar (7,574 sessions).
Despite the large number of infobutton users in our institution, a small fraction of them use infobuttons consistently every day. These daily users apparently have incorporated infobuttons to their patient care workflow. Our frequency distribution of infobutton sessions per user is similar to the one reported by Maviglia et al., that is a small set of users have a very high utilization, while a larger group of users have only sporadic utilization patterns [5]. We intend to observe daily users more closely to understand how and why they use infobuttons more often than others. A preliminary analysis indicates that these users are typically primary care physicians, who work mostly in Intermountain outpatient clinics, and write medication orders, maintain a problem list, and access laboratory test results using HELP2.
We also intend to analyze sporadic and trial users to identify potential barriers for a more complete integration of infobuttons with their workflow. A potential explanation is that many HELP2 users do not keep patient records in the system, accessing HELP2 only to review data generated by others, such as previous notes, clinical reports, and laboratory results. These users would not have access to the infobuttons in the medications ordering module, for example. This is especially true for the inpatient setting, where users still use the HELP System (Intermountain’s legacy hospital information system), which does not have infobuttons, to enter patient data and obtain decision support. Another potential explanation is that nurses constitute an important portion of the sporadic and trial users and our infobuttons have not been specifically configured considering nurses’ information needs at this stage.
Most infobutton sessions originated from the medication ordering module. This finding confirms previous information needs studies, where medications are shown to be the most common topic in questions that physicians have at the point-of-care [13]. The fact that Micromedex (a drug information resource) was the preferred option among infobutton users also reinforces this conclusion. Another potential explanation is that infobuttons are easily available throughout the medication ordering module (e.g., medication search screen, favorite medications list, active medications list). The same is not true for the problem list and laboratory test results modules.
The utilization data showed a preference for resources that presented content primarily in summarized format, such as Micromedex, UpToDate, and Clin-eguide. Conversely, resources that provide access to the primary literature, such as MDConsult and PubMed, were not as important. The busy routine of practicing clinicians and the need for quick access to relevant information is a potential explanation for this finding. This is supported by previous studies that indicated “lack of time” as one of the main barriers to finding answers to questions at the point-of-care [1, 2].
MDConsult was the preferred resource when problem list infobuttons were used, but most often users were looking for patient handouts instead of information about the patient’s condition. This could be explained by the hypothesis that physicians probably access the problem list when a diagnosis is already established, minimizing the need for additional information on the patient’s condition. On the other hand, the presence of a diagnosis may match well with the healthcare workflow stage where patients are educated about their condition.
Users searched for information on a large number of concepts, especially medications, reflecting the variety of information needs that arise at the point-of-care and can be potentially fulfilled by infobuttons. The fact that most of the concepts associated with infobutton sessions were medications may be just a reflection of the complexity and dynamic nature of this domain. Even after applying the 80/20 rule, the number of concepts searched by users remains high, especially regarding problems and medications. The same is not true in the lab tests domain, where only 93 tests accounted for 80% of the infobutton sessions, indicating that an e-resource in this field could be reasonably comprehensive for point-of-care purposes without having to cover the whole spectrum of available lab tests.
The main limitation of our study is that the utilization monitoring data does not allow us to determine whether the user actually found the answer for her question. A potential solution for this shortcoming is the one employed by Maviglia et al., where users received an e-mail within 24 hours of an infobutton session, asking about their search experience [5]. Nevertheless, the continuous utilization growth within our institution provides an indirect indication of the usefulness of infobuttons, especially when associated with the medication ordering process.
Conclusion
During the four years that infobuttons have been available in our institution, we have been observing a constant increase in utilization, which provides good evidence of their usefulness. However, further research is necessary to increase the use of infobuttons. We are currently investigating 1) the factors associated with frequency of infobutton use; 2) the use of additional context attributes to improve the prediction of information needs and selection of resources (including a ranking mechanism); and 3) the use of previous usage patterns to automatically influence infobuttons behavior.
Acknowledgments
We would like to acknowledge James C. Reichert, MD, PhD, and Scott P. Narus, PhD for their effort on the initial implementation of HELP2 infobuttons at Intermountain Healthcare.
References
- 1.Covell DG, Uman GC, Manning PR. Information needs in office practice: are they being met? Ann Intern Med. 1985;103(4):596–9. doi: 10.7326/0003-4819-103-4-596. [DOI] [PubMed] [Google Scholar]
- 2.Ely JW, Osheroff JA, Chambliss ML, Ebell MH, Rosenbaum ME. Answering physicians’ clinical questions: obstacles and potential solutions. J Am Med Inform Assoc. 2005;12(2):217–24. doi: 10.1197/jamia.M1608. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Cimino JJ, Elhanan G, Zeng Q. Supporting Infobuttons with terminological knowledge. Proc AMIA Annu Fall Symp. 1997:528–32. [PMC free article] [PubMed] [Google Scholar]
- 4.Reichert JC, Glasgow M, Narus SP, Clayton PD. Using LOINC to link an EMR to the pertinent paragraph in a structured reference knowledge base. Proc AMIA Annu Fall Symp. 2002:652–6. [PMC free article] [PubMed] [Google Scholar]
- 5.Maviglia SM, Yoon CS, Bates DW, Kuperman G. KnowledgeLink: Impact of Context-Sensitive Information Retrieval on Clinicians’ Information Needs. J Am Med Inf Assoc. 2006;13:67–73. doi: 10.1197/jamia.M1861. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Clayton PD, Narus SP, Huff SM, et al. Building a comprehensive clinical information system from components. The approach at Intermountain Health Care. Methods Inf Med. 2003;42(1):1–7. [PubMed] [Google Scholar]
- 7.Cimino JJ, Li J, Bakken S, Patel VL. Theoretical, empirical and practical approaches to resolving the unmet information needs of clinical information system users. Proc AMIA Annu Fall Symp. 2002:170–4. [PMC free article] [PubMed] [Google Scholar]
- 8.Mitchell JA, Fun J, McCray AT. Design of Genetics Home Reference: a new NLM consumer health resource. J Am Med Inform Assoc. 2004;11(6):439–47. doi: 10.1197/jamia.M1549. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Tarczy-Hornoch P, Shannon P, Baskin P, Espeseth M, Pagon RA. GeneClinics: a hybrid text/data electronic publishing model using XML applied to clinical genetic testing. J Am Med Inform Assoc. 2000;7(3):267–76. doi: 10.1136/jamia.2000.0070267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Hulse NC, Rocha RA, Del Fiol G, Bradshaw RL, Hanna TP, Roemer LK. KAT: A Flexible XML-based Knowledge Authoring Environment. J Am Med Inform Assoc. 2005;12(4):418–30. doi: 10.1197/jamia.M1701. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Allen M, Currie LM, Graham M, Bakken S, Patel VL, Cimino JJ. The Classification of Clinicians’ Information Needs While Using a Clinical Information System. Proc AMIA Annu Fall Symp. 2003:26–30. [PMC free article] [PubMed] [Google Scholar]
- 12.Del Fiol G, Cimino JJ, Rocha RA. Infobutton Communication Standard (draft) [document on the Internet] Health Level 7. 2006. [cited 2006 Mar 3]. Available from: http://www.hl7.org/Library/Committees/dss/infobutton-proposal-2006-01-04.zip.
- 13.Ely JW, Osheroff JA, Ebell MH, et al. Analysis of questions asked by family doctors regarding patient care. BMJ. 1999;319(7206):358–61. doi: 10.1136/bmj.319.7206.358. [DOI] [PMC free article] [PubMed] [Google Scholar]