Abstract
As the Providence Health System is phasing in its Computerized Provider Order Entry (CPOE) system at the Providence Portland Medical Center, we conducted a study to demonstrate the effects of CPOE on medication turn-around time. Retrospectively, we tracked and compared medication orders that were placed via the existing paper-based system and the CPOE system. The results of this study coincide with, and confirm, previous research that has been performed at large academic medical centers.
INTRODUCTION
Like many, the Providence Health System (PHS) has begun its implementation of CPOE1. The flagship facility for their implementation is the Providence Portland Medical Center (PPMC). As part of its CPOE implementation, the PHS is looking to demonstrate some tangible benefits associated with CPOE. The PHS plans to do this by developing metrics that can be used to compare CPOE to traditional paper-based system. Therefore we conducted a study, which compared the differences between CPOE and the paper-based system with respect to medication turn-around time.
BACKGROUND
Benefits of CPOE
Since its conception, the benefits of CPOE have been widely documented, which include improved: documentation (improved date and time stamp compliance), legibility, and medication checks (drug-drug and drug-allergy) and medication turn-around time 2, 3, 4, 5, 6. Moreover, CPOE, despite recent findings, has been shown to reduce medical errors 5, 7. In addition, CPOE has been shown to positively affect the cost and quality of care 8.
Medication Turn-Around Time
Time-to-first-dose, or medication turn-around time, is considered the interval from the time a medication order was composed to the time the medication was delivered. Moreover, time-to-first dose can be broken down into two key phases: the time from when the order was composed to the time that pharmacy verifies the order, and the time from pharmacy verification to the time the medication was delivered 2.
The use of CPOE has been shown to reduce the overall medication turn-around time2, 3. Previous research has shown that significant time savings can be achieved in both phases of CPOE2. However, the most dramatic time savings are usually seen in the first phase.
Essentially, CPOE is an intervention that is designed to specifically affect the first phase of the medication turn-around time. CPOE drastically reduces the time it takes an order to be verified by the pharmacy, once it has been written. The reduced time in phase one is attributed to the fact that once an order has been written with CPOE, it is automatically routed to the appropriate department. In this case, the medication orders are routed directly to pharmacy.
Previous work has demonstrated time savings in the second phase as well2. However, this finding was unexpected.
Previous Research
Not much has been done in the way of measuring the effects of CPOE on medication turn-around times. However, the work that has been done shows promising results. Largely, these studies have demonstrated reductions in medication turn-around times in large academic medical centers 2, 3.
One study, by Mekhijan et al., at the Ohio State University found a statistically significant 70% reduction in their medication turn-around time 2. The most dramatic time savings were seen in the first phase, which was reduced to 33 minutes (0:33) from 3 hours and 57 minutes (3:57). In addition, the time associated with the second phase was reduced to 1 hour and 22 minutes (1:22) from 3 hours and 16 minutes (3:16). Overall, CPOE reduced the medication turnaround time from 5 hours and 28 minutes (5:28) to 1 hour and 51 minutes (1:51).
Another study, conducted by Lehman et al., at Rush, found similar results. This study also found a statistically significant reduction of their medication turn-around time. More specifically, they found that their medication turn-around times were reduced by roughly 64%. Prior to CPOE the average medication turn-around time was 3 hours and 49 minutes (3:49). CPOE, however, reduced this time to 1 hour and 23 minutes (1:23). Overall, the average medication turn-around time was reduced by 2 hours and 26 minutes (2:16) 3.
SETTING
Providence Portland Medical Center (PPMC)
PPMC is a large metropolitan hospital that is recognized for excellence in patient care and research in cancer, cardiac, orthopedics, women’s health, rehabilitation, and behavior health. PPMC contains 483 licensed beds and employs over 3, 300 people, nearly a third of which are medical staff.
Annually, PPMC admits over 21,000 patients and receives over 57,000 emergency department visits. On the average, PPMC has a daily patient census of 262 patients, and an average length of stay of 4.5 days.
4K
4K is a 21-bed Acute Rehabilitation Unit located on the 4th floor of PPMC. 4K specializes in treatment for patients who have suffered from:
Catastrophic illness
Congenital disorders/Stroke
Head and spinal cord injury
Multiple trauma
Neurological conditions
Orthopedic conditions
Generally, patients are referred to 4K by their primary care physician and evaluated by a staff physiatrist. Typically, patients that are admitted to this floor must have functional limitations in two or more of the following areas:
Cognitive-perceptual functions
Bowel and/or bladder continence
Pain management
Personal care activities
Mobility
The average length of stay is 9.5 days and the staff comprises several clinical specialties including physiatrists, rehabilitation nurses, physical, occupational and therapeutic recreation therapists, and social workers.
METHODS
Using the clinical information systems at PPMC we were able to retrospectively track medication orders that were written on 4K. This was done by reviewing the paper chart and the electronic order confirmation records for medication orders. Once the data was collected we then used SPSS to compare the overall mean medication turn-around times between CPOE and the paper-based system. In addition to the overall turn-around time, we compared the times of two key phases, the time from order composition to pharmacy verification and the time from pharmacy verification to delivery.
Data Collection
In order to review and track the key data points for medication turn-around time, we obtained two “dumps” of the medication orders (that were placed on 4K) before and after the introduction of CPOE. This was done by a PHS staff member who queried their clinical information system to obtain a data set of medication orders from 4K that were verified by the pharmacy from 8/15/05 – 10/7/05 and from 10/10/05 – 11/02/05.
Essentially, these data sets yielded a “snapshot” of the practice before and after the introduction of CPOE. The data sets consisted of a pharmacy tracking number, the drug name, a patient account number, the date and time the order was verified by the pharmacy, the date and time the order was started, and the route, frequency and dose for each medication.
Once the initial data sets were obtained, we established a protocol to include and exclude medication orders in this study. Ultimately, the protocol included medication orders that were composed, verified and administered on the same day. Therefore, PRN, or “as needed”, medication orders were excluded. In addition, routine and oral medication orders were included.
We began the study began by tracking the times for the medication orders that were placed via the paper-based system. The patient account number was used to search the PHS medical records for the record of when the medication was ordered. Once the correct record was found the medications from the data set and the medications in the record were matched. The medications were matched using the name, route, frequency, and dose. Once the medication was matched the appropriate date and time, which indicated when the order was composed, was recorded. The medication order was then classified according to the protocol. The medication orders were classified as valid* or surrogate†.
The focus then shifted to the orders that were placed via the CPOE system. Again, the medication orders that were placed via CPOE were tracked using the same methodology as the paper-based medication orders.
After both data sets were obtained, the elapsed time for each medication order was calculated. This was accomplished by calculating the difference from when the order was composed to when the order was delivered. In addition, we calculated the times for the individual phases. This was done by calculating the time from composition-to-verification, and from verification-to-delivery. These times were then entered and analyzed with statistical software package.
Analysis
Data analysis was performed using SPSS. The times were grouped, according to the data set from which the came. SPSS was used to obtain the descriptive statistics and to perform the appropriate statistical tests. After obtaining the descriptive statistics, a T-test (for unequal variances) was performed using the mean medication turn-around time, and the time from the first and second phase.
The mean, however, is a measure that can be highly influenced by outlying data points. Therefore, other descriptive statistics, such as the trimmed mean and median were also used to compare the differences of medication turn-around times between CPOE and the paper-based system.
RESULTS
We tracked a total of 199 medication orders from 4K. Of the 199 medication orders, 106 (53%) were placed via the paper-based system and 93 (47%) were placed via the CPOE system.
The 106 medication orders from the paper-based system consisted of 77 valid orders and 29 surrogate orders. Of the 77 valid orders, 39 were telephone/voice orders placed by nurses or pharmacy personnel, and 38 were medication orders placed by physicians.
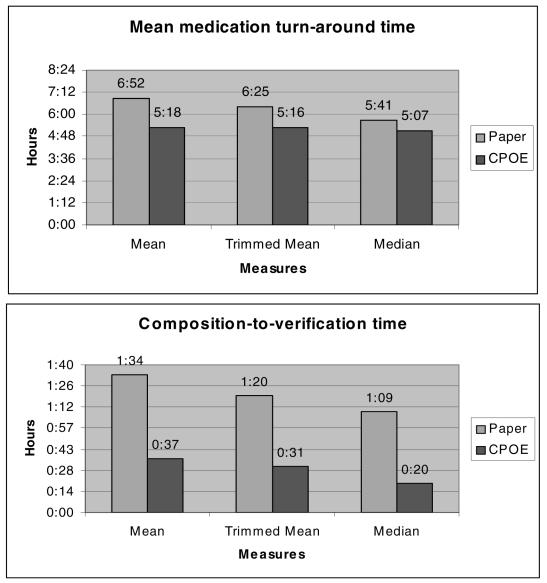
Overall, we found statistically significant differences (p=.008) between the means from the paper-based and CPOE systems. The mean medication turn-around time was reduced from 6 hours and 52 minutes (6:52) to 5 hours and 18 minutes (5:18), a reduction of 23%. The paper-based system yielded a trimmed mean time of 6 hours and 25 minutes (6:25), and a median time of 5 hours and 41 minutes (5:41). For the medication orders that were placed via CPOE, all were valid according to our protocol. The CPOE system, on the other hand, yielded a trimmed mean time of 5hours and 16 minutes (5:16), and a median time of 5 hours and 7 minutes (5:07).
When we looked at each phase separately we found that CPOE only affected the first phase. Therefore, the overall reduction in time was due to a dramatic time savings in the first phase. Again, we found statistically significant differences (p<.001) between the mean time from the paper-based and CPOE systems. For this phase, (the time from order composition to pharmacy verification) we found that the paper-based system yielded a mean time of 1 hour and 34 minutes (1:34), a trimmed mean time of 1 hour and 20 minutes (1:20), and a median time of 1 hour and 9 minutes (1:09). The CPOE system, on the other hand, yielded a mean time of 37 minutes (0:37), a trimmed mean time of 31 minutes (0:31), and a median time of 20 minutes (0:20).
DISCUSSION
Study Results
The results of this study are promising. We were able to demonstrate a statistically significant reduction of the overall medication turn-around time. We found a substantial time savings in the composition-to-verification phase. This is largely attributed to the fact that CPOE eliminates several time consuming steps during the process of carrying out a medication order.
However, we did not achieve the magnitude of results that were found at Ohio State University by Mekhijan et al. Specifically, our study did not produce the time savings in the latter phase of the medication turn-around time, the time from pharmacy verification to delivery. Nevertheless, our results are positive and show that CPOE allows for more efficient patient care in a clinical setting.
There could be several differences that account for the lack of time savings in the latter half of the medication turn-around time. Two reasons are more apparent and therefore will be discussed. First, the rehab setting may lessen the impact of our results. Most of the previous work has been performed in large academic medical centers, on time sensitive units. Second, the use of “surrogate” times, for the paper-based medication orders, definitely lessens the impact of CPOE.
The setting itself could very well influence the outcome pertaining to the latter half of the medication turn-around time. Being that 4K is a rehab unit, many of the medications that are delivered on this floor are routine and/or oral. The study at Ohio State University, however, was conducted in a surgical transplant unit. Moreover, the Ohio State study limited its orders to intravenous medications, which in turn excluded routine and oral medications.
Lastly, during the data collection period, we noticed a large percentage of orders that were collected did not have the proper date and time stamp. As previously reported, nearly 30% of the orders did not have a valid date and time stamp; and of the 77 orders that had valid time stamps 50% were telephone/voice orders that were actually placed by nurses or pharmacists. After noticing this trend, and in the interest of time, we decided to keep these orders. We felt that the data would have administrative implications and give us insight into the ordering practices of the physicians on 4K. However, we realize that by doing so, we were essentially “washing out”, or lessening the impact of the results from our study. Nevertheless, we have a worst-case scenario of the improvement that CPOE provided when carrying out medication orders.
CONCLUSION
The results of this research study have both organizational and scientific applications. On an organizational level, the results of this study can be used to build and strengthen internal administrative and/or physician support. Moreover, organizationally speaking, these results validate the efforts put forth at PPMC.
In addition, this study demonstrates that CPOE allows for more efficient patient care within the organization. However, in this study, CPOE was only shown to affect a certain portion of the medication turn-around time. But nevertheless, CPOE was shown to reduce the overall medication turn-around time.
Also, from this study, we were able to obtain information about physician ordering practices, such as date and time stamp compliance. Again, as previously reported, only 70% of the paper-based orders contained the proper date and time stamp; compared to 100% compliance from the CPOE system. Although it was not the focus of the study, this information could be quite useful to administrative personnel within the organization.
Scientifically, the results of this study confirm findings from previous studies at large academic medical centers2, 3. Although we did not find nearly the reduction in overall time, we did see a significant improvement. But more importantly, the results of this study demonstrate that the benefits of CPOE can extend from academic medical centers to community-based medical centers.
ACKNOWLEDGEMENTS
I would like to thank Richard Gibson for allowing me to take part in his endeavors at PPMC, and Joan Ash for her guidance.
Footnotes
Valid orders are medication orders that contain a date and time of when they were composed.
Surrogate orders are medication orders that have a date, but lack the time. Therefore, the time the order is observed, or “taken off”, by the unit coordinator or nurse is considered the surrogate time.
REFERENCES
- 1.Kuperman GJ, Gibson RF. Computer physician order entry: benefits, costs, and issues. Ann Intern Med. 2003;139:31–9. doi: 10.7326/0003-4819-139-1-200307010-00010. [DOI] [PubMed] [Google Scholar]
- 2.Mekhjian HS, Kumar RR, Kuehn L, Bentley TD, Teater P, et al. Immediate benefits realized following implementation of physician order entry at an academic medical center. J Am Med Inform Assoc. 2002;9:529–539. doi: 10.1197/jamia.M1038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Lehman ML, Brill JH, Skarulis PC, Keller D, Lee C. Physician Order Entry impact on drug turn-around times. Proc AMIA Symp. 2001:359–63. [PMC free article] [PubMed] [Google Scholar]
- 4.McDonald JC, Brill JH, Johnson K, et al. Implementing a physician order entry system: perspectives from five physicians. Session 18: HIMMS Proc. 1996 [Google Scholar]
- 5.Bates DW, Kuperman G, Teich JM. Computerized physician order entry and quality of care. Qual Manag Health Care. 1994;2(4):18–27. [PubMed] [Google Scholar]
- 6.Bates DW, Teich J, Lee J, Seger D, Kuperman GJ, Boyle D, et al. The impact of computerized physician order entry on medication error prevention. J Am Med Informatics Assoc. 1999;6:313–321. doi: 10.1136/jamia.1999.00660313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Koppel R, Metlay JP, Cohen A, et al. Role of computerized physician order entry systems in facilitating medication errors. JAMA. 2005;293:1197–1203. doi: 10.1001/jama.293.10.1197. [DOI] [PubMed] [Google Scholar]
- 8.Schroeder CG, Pierpaoli PG. Direct order entry by physicians in a computerized hospital information system. Am J Hosp Pharm. 1986;43:355–9. [PubMed] [Google Scholar]