Abstract
In the French DocPatient project, we work on documentary functionalities to improve the use of the electronic medical record. We suggest that integration of specific uses for paper medical documents in the design of the electronic medical record will improve its utility, use and acceptance. We propose in this paper to add a functionality of annotations in the electronic medical record to reinforce collaboration, coordination and awareness.
Introduction
Traditionally, health professionals use a paper medical record. From now on, this record shows its limits, in particular to share medical knowledge between all the health professionals in an hospital, in a care network... The electronic medical record must be equivalent to the paper one. It must support the practices necessary to the collaboration of the practitioners. However, recent studies on their practices with the electronic medical record [1,2] reveal important gaps between its objectives and the ways health professionals use it. Systems have failed in a wide variety of medical organisations (medical offices, hospitals…). Actually, most of the health professionals use both a paper and an electronic medical record because they are obliged by the medical authorities to use the electronic one and because they still prefer to use the paper one to collaborate. We can doubt that the electronic medical record, as it is actually presented to the health professionals, matches with their practices.
How can we explain this series of failures? Designers are confronted with the scale of the medical organisations. For example, the hospitals are particular organisations, offering services (the care) and managing knowledge thanks to the medical record. The number of stakeholders [3] whose work is based on the medical record is very important: in the medical units, in the technical units such as pharmacy, laboratories…, in the research departments... Those actors use it for varied tasks: medical activities such as diagnoses, therapeutic decisions... or others activities such as control, planning, education... The medical record must represent varied knowledge such as weight, hospitalisation reports, images... on varied mediums such as paper or electronic documents, images, databases... The medical record, its users and its managers are distributed in heterogeneous places. To conclude, it is very difficult to build an electronic medical record. The technical methods are now available, but the designers do not succeed in providing health professionals tool adapted to the scale of the organisation and to their intercorrelation of practices. Health professionals are still waiting for an electronic medical record as efficient as the paper medical record.
In this paper, we present the results of a multidisciplinary study dealing with a functionality of annotations for improving collaboration in the electronic medical record. After having briefly presented the material and methods, we show why the electronic annotations allow coordination and awareness in the paper medical record and for which reasons they must be transposed in the electronic settings. To finish, we present our tool of annotations and the tests carried out with the potential users.
1. Material and Methods
Since 2002, we were part of the French DocPatient project which is financed by the region of Picardie. It gathers a multi-field team composed of sciences for engineer (data-processing) and social sciences (law and management). We work in collaboration with a pilot site1 and an industrial partner2. We develop a functionality of annotation, making easier the manipulations of the electronic documents and the collaboration between health professionals.
The study of the paper and the electronic medical record used in our pilot site allow us to understand how they use the documents and why they annotate them. Annotations are a relevant support for the collaboration, coordination and awareness which are not provided by the standardised documents we find in most of the electronic settings. This assessment is coherent with the studies carried out in the field of the Computer Supported Collaborative Work. Hartswood and Gennari [2,4] have underlined the difficulties encountered by the health professionals when they work with the electronic documents and the interest of annotating them for collaborating. We studied the literature concerning this activity [5,6] in others fields. We built a tool to annotate an electronic medical record and to reuse these annotations. We tested this tool in our pilot site with the potential users. This work allows us to notice improvements for our tool and to supplement our analysis of the health professionals’ practices of annotations.
2. Annotations a support for collaboration
Among all the practices of the practitioners, we focussed our attention on the annotations because we thought that they are a relevant support for their collaboration. We propose the following definition:
An annotation is a particular note linked to a target. The target can be a collection of documents, a document, a segment of document (a paragraph, a group of words, an image, and a part of image …), and another annotation. Each annotation has a content, materialised by an inscription. It is a trace of the mental representation elaborated by the annotator about the target. The content of the annotation can be interpreted by another reader. The anchor links the annotation to the target (a line, a surrounded sentence …).
Annotations, a support for coordination
In an hospital, work is distributed between the health professionals who are relatively independent and autonomous to carry out their tasks. The nurse and the physician can organise their own tasks as they want as long as their activities merge to care the patient. However, health professionals are also “mutually dependent” [7]. The nurse cannot begin the administration of a drug if the physician did not write the regulation. Consequently, they need coordination to manage this interdependence of the tasks. For example, they need to allot a task to the most competent health professional, to prevent two health professionals from doing the same activity, to build the schedules... For that, they need a form of agreement called by De Terssac [8] the Common Frame of Reference COFOR (representation of the common task, objectives and partners). Most of the time, the COFOR is supported by the direct interactions. For example, the physician does not have the same concerns than the pharmacist but, during their direct interactions (often by phone), they use the COFOR as well as their own competences to disambiguate the communication.
These direct interactions are not sufficient and the practitioners need shared artefacts to maintain the COFOR. For that, they developed a significant culture of writing words. In order to keep most of the traces of their exchanges and of their acts, they transcribe them on a perpetual medium, on the paper or on the electronic documents of the medical record. Considering the number and the complexity of the situations of interactions, the hospital units have organised a real process of “documentarisation” [9]. The heads of department have designed the architecture of the record and the documents organisation. The management of the documents is easier: in the paper record, we know where to retrieve the surgical report and their physical manipulations are easier: thanks to the predefined outline of the patient discharge summary, a writer knows where to look for the paragraph he wants to fill in and a reader knows where to retrieve the paragraph he want to read. These predefined types of documents fix the rules of reading and writing, which allow readings in distant contexts in time and space from the creation. Berg et al. [10] affirm that this way of using and reusing the paper medical record is linked to the contextual nature of the medical knowledge. Finally, the documents of the record allow to build the COFOR necessary for practitioners’ coordination.
In spite of the “documentarisation” effort of the medical authorities to simplify the writing and the reading of the medical documents, these ones are not sufficient to allow the practitioners to really work on all the knowledge they create. Health professionals encounter some difficulties relative to the type of the documents which are too rigid and standardised for writers’ writing and relative to the unpredictability of medical knowledge. Where can they consign the knowledge not envisaged by the designers when the documents are too structured? On paper, even if the designer leaves textual fields for non foreseeable knowledge, they annotate the rigid forms. With a graphical way (an arrow, an underlined part), they connect the comment and the part of the document having caused the comment. A posteriori, the readers can also leave traces of their comprehension in annotations. These ones allow to contextualise the knowledge not envisaged by the designer, produced during the writing and the reading. The reader can re-appropriate the document, rewrite it according to the desired use. Currently, this knowledge is annotated on paper and not written in the electronic documents because there is no means to extend them. Consequently, annotations are a relevant support for the practitioners’ coordination when the too standardised medical documents show their limits.
Annotations, a support for awareness
For a successful collaboration, practitioners must be aware of the others’ activities. A lot of studies have shown that coordination increases when people know what happens around them (synchronous mode) or what has happened (asynchronous mode) [11,4]. Without awareness, a worker can repeat an action carried out by another worker. He can look for information although his colleague knows it. He can hamper the work of another actor because he is not aware of his presence in the environment… When people work in a synchronous way, face-to-face, awareness is provided by their direct interactions and their mutual observations. The nurse is aware of the physician when they collaborate in the patient’s room. During an asynchronous work, awareness needs a support and the documents of the medical record are used for that. Reddy et al. [12] showed “that users often were not looking for information about the patient per se, but rather for information about the activities of other health-care workers regarding that patient”.
If the documents of the medical record offer a certain level of awareness, there are not sufficient. Most of the knowledge used to support awareness is transitory, partial, incremental.... Health professionals do not want to consign it in the documents. These ones are too much “public” (all the practitioners working with the patient consult the documents) and too much “formal” (the practitioners consign knowledge according to writing rules' fixed by the documents designers). Therefore, annotations are a relevant support, less “official” for all their interactions. Practitioners know that annotations will be read as incomplete and subject to revision, contrary to the predefined documents of the record. They can use them to write all they need for informal interactions.
Synthesis: a person annotates because:
She cannot, without annotations, add her semiotic production to the document because the data capture does not allow the writer to enter the desired data. It is the case of the too rigid medical forms. Therefore, an annotation is an escape clause if there is no current method to extend forms.
She does not want to add her semiotic production to the document because this one is written with an intention of communication different from the initial intention of the annotated document. In so doing, the annotator is adding an information about the document rather than information that belongs in the document itself. It is the case when a reader annotates to keep traces of his reading, when several practitioners collaborate by taking as support the documents they annotate. Consequently, an annotation is also an escape clause if there is no means to code the comments about the documents.
The use of annotations during collaborative activities depends on the role of the reader in the organisation. A physician writes « blood gas in 2 hours ». A nurse reads this message, she detects the interference with her own care (she has to delay the child’s bath) and she understands that she must prepare the child for the blood gas. A fellow analyses this comment from another point of view and consequently, this note induces others collaborative activities.
All these examples show how the practitioners use annotations to act: either to enrich the annotated document or to be the transitory support of knowledge used to create new knowledge (recorded or not in a document). Therefore, annotating is already an action which enables health professionals to store knowledge but also to maintain a certain level of coordination and awareness.
3. An annotations dedicated to the medical record
Designers of new electronic medical record are likely to think of these added functionalities which will help practitioners to maintain collaboration. Providing a functionality which allows to comment the documents can be used for that. But we can go further. In our tool, we have exploited these annotations to improve the use of the electronic record.
Health professionals need functionalities of hypertextual navigation because they have readings problem in the electronic medical record such as cognitive overload, no global vision… As we find in annotations traces of their readings, we can reuse these annotations to build documents of navigation. It is a new document added to the record, which allows to retrieve the initial documents of this record (as a summary, index). Such a document of navigation contrived from annotations corresponds to a list of items leading to annotations, selected by the user according to one or more criteria (annotator’s name, date, topic…). From these annotations, a reader retrieves the annotated documents. So, we offer him new reading roads. We can also use annotations to have particular point of view on the document. During the creation of an annotation, the annotator can specify the recipients of his annotation with access rights: himself, a group of users, all the readers. During the consultation of the record, there is an automatic filtering. Consequently, a reader visualises only the annotations he has the right to see. In addition, this reader can filter manually the annotations and visualise only a collection of annotations selected according to criteria. These three functionalities help the readers to build their own vision of the electronic record and the COFOR.
Health professionals need aids to build synthesis used for collaboration in particular for exchanging the most important knowledge they need during the care. We propose to use annotations in order to produce these syntheses. For example, a practitioner writes the patient discharge summary. He reads the record, selects and comments some parts. Gathering all these annotations in a new document gives him a base to write this report. Then, he can rewrite the generated document, add knowledge and a page setting. The reader becomes a “reader-writer”.
Health professionals need aids to exchange information for maintaining coordination and awareness. For that, a user can send an annotation to one or more recipients (as an email). The message can have content (a comment) or not and can be produced in connection with an element of a record, or a record taken as a whole or in response to another message. When the recipient receives a message in a reception box, he retrieves the source of the message (the document, the record or the previous message).
We built a first tool in collaboration with our industrial partner according to these specifications. On the Figure 1, a user annotates a document. He highlights a part of the document and attaches a comment and a link up to another document of the record (a thorax radiograph).
Figure 1.
Our tool of annotations
4. Utilisability tests and results
We undertook a semi-realistic utilisability study of our tool to check with the potential users the interest of annotating in the electronic medical record. We have chosen 20 users representative of the end-users: 5 senior physicians, 5 fellows, 5 nurses and 5 administrative agents. At the beginning of the test, we invite the user to fill in a pre-evaluation form to collect his profile, his data-processing competences and his current use of paper annotations. Then, we ask him to carry out some tasks. The head of department helped us to build scenarios adapted to the 4 professional categories. In so doing, the user handles the various functionalities as he could do for his work. During the manipulations, we note the information he gives us orally and his mimicries. At the end, the user fills in a post-evaluation form to collect his point of view about the relevance and the user-friendliness of all the functionalities.
The practitioners’ comments were very positive. 100% of the health professionals said that they use annotations on paper and would use annotations on the electronic settings. They like to retrieve the paper practices of annotations (to draw the attention on parts of the documents, to communicate in an asynchronous way, to aid the appropriation of the medical record….). They enjoy the new functionalities and they think these ones can reinforce their collaboration particularly the messages. We detailed these observations and the analyses of the two forms in [13]. We add here a collaborative perspective with the table 2 which summarises the reasons they evoked for explaining us why the proposed functionalities match with their current collaborative activities.
Table 2.
Impact of our functionalities on coordination and awareness practices
| Functionalities | Impact on coordination | Impact on awareness |
|---|---|---|
| Annotation Writing | To add knowledge relative to the coordination of the activities (planning, order…) when they cannot or they do not want write it in the documents | To add knowledge to allow the partners to be aware of his own activities (report of action…) when they cannot or they do not want to write it in the documents |
| Annotation Reading | To read annotations which impact on their own activities | To read annotations which allow to be aware of the annotator’s interest point (the annotated part). |
| Synthesis | To make easier the writing of synthesis which are the main documents used for coordination | To make easier the writing of synthesis, the main documents used to be aware of what have been done for the patient |
| Manual filtering | To visualise the annotations dealing with the things to do for a patient, in the context of a document. | To visualise only the annotations of a person to be aware of his way of thinking the patient in the context of a document. |
| Document for navigation | To visualise the annotations dealing with the things to do for a patient, in the context of his record. | To visualise only the annotations of a person to be aware of his way of thinking the patient, in the context of his record. |
| Automatic filtering | To target the recipients of an annotation (by choosing limited access right) | Danger! Some information can be hiding! |
| Message | To communicate in an asynchronous way in the context of the documents | To diffuse knowledge to a wide audience |
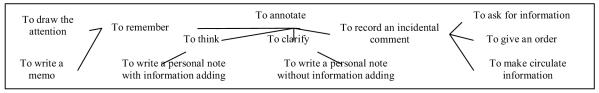
From these tests and our readings [5,6], we built two models: one for annotations acts (cf. figure 3), which enables us to describe the annotator’s intention of communication and one for the annotation object, seen as the result of the annotation act. With this second model, we describe how the annotator chooses elements from his environment to transmit his message: anchor, target, location of the content and speeches acts to transmit his message. We can infer on this second model to deduce elements of the first model. Generally, a physician underlines passages of the laboratory results to draw the attention of his fellows. We thus deduce rules to adapt the interface of our application according to the user, the annotated document and the annotations. For example, the previous annotations of the physician will be in full view in the context of the document to draw the attention of the fellows.
Figure 3.
Model of the acts of annotations
To conclude, these first results justify the presence of annotations in the electronic medical record to support collaborative practices. The criticisms are mainly related to the way we present the functionalities and not to their interest. We will take them into account to refine our tool and we will implement the rules elaborated thanks to our models.
5. Conclusions and Prospects
The documents of the medical record play a key role for the storage of the medical knowledge and for the health professionals’ collaboration (coordination and awareness). In most of the electronic settings, we do not find sufficient functionalities to support these mechanisms. Consequently, these tools are often perceived as organisational and cultural obstacles. Health professionals are frustrated because they find no sufficient benefits for using the electronic medical record rather than the paper one. Indeed, there is a contradiction between the medical authorities’ needs (they want electronic standardised data for their activities of management, research…) and the health professionals’ needs (they want a relevant support to collaborate). In most of the electronic medical record, the documents are standardised to answer the medical institutions’ needs. The practitioners who tend to adjust the categories of the medical record to answer their needs of collaboration cannot do it any more.
Designers must create added functionalities which will help practitioners to maintain collaboration, coordination and awareness. We propose the integration of a documentary functionality: annotations. Indeed, the tools of annotation are common. Moreover, practitioners already annotate the documents of the paper medical record. Consequently, such functionality in the electronic record seems natural. The originality of our work comes from the way we exploit these annotations to make easier the handlings of the electronic documents and the communications. The tests realised with the practitioners on our tool validate our assumption that an annotation tool is useful for them. About the theoretical prospects, we foresee to generalise our definitions with contexts broader than the medical record because experts use annotations in many others fields as genetics, architecture... We also need to study more precisely the impact of the change of medium on this practice, by considering the fact that it is possible to make non-linguistic annotations (diagrams, video, audio…) in multimedia documents.
Footnotes
The hospital ward of paediatric intensive care and neonatal medicine of Amiens
The company UNI-MEDICINE http://www.uni-medecine.com/
References
- 1.Pratt W, Reddy MC, McDonald DW, Tarczy-Hornoch P, Gennari JH. Incorporating ideas from computer-supported cooperative work. Journal of Biomedical Informatics. 2004;37:128–137. doi: 10.1016/j.jbi.2004.04.001. [DOI] [PubMed] [Google Scholar]
- 2.Hartswood M, Procter R, Rouncefield M, Slack R. Making a Case in Medical Work: Implications for Electronic Medical Record. Computer Supported Cooperative Work. 2003;12:241–266. [Google Scholar]
- 3.Dieng-Kuntz R, Corby O, Gandon F, Giboin A, Golebiowska J, Matta N, Ribière M. Méthodes et outils pour la gestion des connaissances : une approche pluridisciplinaire du Knowledge Management. 2001. [Google Scholar]
- 4.Gennari JH, Weng C, Benedetti J, McDonald DW. Asynchronous communication among clinical researchers: A study for systems design. International Journal of Medical Informatics. 2005;74:797–807. doi: 10.1016/j.ijmedinf.2005.03.019. [DOI] [PubMed] [Google Scholar]
- 5.Marshall CC. The Future of Annotation in a Digital (Paper) World. In: Harum, Twidale, editors. Successes and Failures of Digital Library. 2000. [Google Scholar]
- 6.Ovsiannikov IA, Arbib MA, McNeil TH. Annotation technology. International Journal of Human-Computer Studies. 1999;50:329–362. [Google Scholar]
- 7.Hoc JM. Towards a cognitive approach to human-machine cooperation in dynamic situations. International Journal of Human-Computer Studies. 2001;54:509–540. [Google Scholar]
- 8.De Terssac G, Chabaud C. Référentiel opératif commun et fiabilité. In: Leplat J, de Terssac G, editors. Les Facteurs Humains de la Fiabilité Dans les Systèmes Complexes. 1990. [Google Scholar]
- 9.Zacklad M. Proc. Workshop Distributed Collective Practice: Building new Directions for Infrastructural Studies, 2004 CSCW. Nov–Oct Documents for Action (DofA): infrastructures for Distributed Collective Practices. [Google Scholar]
- 10.Berg M, Goorman E. The contextual nature of medical information. International Journal of Medical Informatics. 1999;56:51–60. doi: 10.1016/s1386-5056(99)00041-6. [DOI] [PubMed] [Google Scholar]
- 11.Reddy M, Pratt W, Dourish P, Shabot M. Socio-technical requirements analysis for clinical system methods. Methods of Information in Medicine. 2003;42:437–444. [PubMed] [Google Scholar]
- 12.Reddy M, Dourish P, Pratt W. Coordinating Heterogeneous Work: Information and Representation in Medical Care. Proc. 2001 ECSCW. :239–58. [Google Scholar]
- 13.Bringay S, Barry C, Charlet J. Workshop KM&OM, IJCAI-2005. Jul–Aug Annotations for managing knowledge in the Electronic Health Record. [Google Scholar]