Abstract
Hospitals transitioning from paper to electronic information systems often find that inadequate fit of newly implemented technology to work environment is causing delays, inefficient use of resources, and may be introducing a new kind of errors attributable to the complexity of human interaction with computer systems. The purpose of this study is to characterize workflow, decision making and cognitive processes of clinicians in the emergency department of a large hospital, and to suggest optimal technological interventions for observed problems. The analysis of collected data identified fifteen tasks and areas that either slowed the process of care by unnecessary work duplication or created opportunities for medical error. We have made several suggestions for replacing suboptimal processes by technology or for refining current configurations of information and communication devices to become more appropriate to the cognitive and workflow demands of specific tasks and defined within the larger context of emergency clinical work.
INTRODUCTION
An increasingly large population of patients is using emergency departments (ED) of large hospitals as their gateway to medical care. A recent study reports that more than 90% of EDs operate either “at” or “over” capacity.1 Endemic patient overcrowding in urgent care facilities creates a highly dynamic and charged working environment in which the quality of care may be compromised by the extraneous demand on time and attention of care providers. Clinicians have to simultaneously attend to newly arriving patients as well as to those waiting for treatment, tests, procedures or for available beds.2 Despite the proficiency and experience of the ED staff, medical errors are often the result of difficulties associated with complex patient tracking and information processing systems.3 Exacerbating conditions such as congested waiting and treatment areas, suboptimal workflow and inadequate communication systems are contributing factors in a process producing high-risk environments detrimental to patient safety.4
Health Information Technology (HIT) has a prominent role in managing care by monitoring clinical events, providing real-time decision support and feedback on entered data, and by generating alerts and reminders. Many hospitals invest in HIT to improve workflow, reduce long-term operating costs and to minimize medical error.5
Technology also transforms the reasoning and cognitive behavior of individual clinicians and the way teams collaborate in providing care to a patient. Information systems and other electronic devices do not merely accelerate or augment function but may qualitatively restructure the performance of a task.6 The mediating role of technology in healthcare has been demonstrated in several domains of application, such as electronic medical record systems7 or patient-controlled analgesic devices.
An optimally designed information system may for example automate routine tasks so that they only require staff supervision. Interruptive communication patterns, such as face-to-face or telephone contacts can be reduced to include only necessary encounters or be replaced by less obtrusive asynchronous messaging. The system may also reorder task priority queues and manage their flow as conditions change.
The critical aspect of transition from paper-based management to electronic information systems is selecting the most appropriate technology for the established workflow without adding unnecessary complexity or increasing the cognitive effort of clinicians required for device interaction. A truly informed choice requires detailed knowledge of the existing work environment, its complexities, inherent risks and opportunities for error in the process of care. Consequences to workflow and cognitive behavior of users, intended as well as unintended, need to be carefully examined before the newly configured system is operational.
The purpose of this study is to characterize the workflow, decision making and cognitive processing of clinicians in the emergency department of a large urban hospital and to suggest possible technological interventions for identified problems. Findings were used to recommend the best technology for patient tracking and workflow management, communication among providers and for a clinical information system to replace the current paper-based system.
The methods we used include ethnographic data collection, observations, surveys, questionnaires and cognitive task analysis that are applicable to a wide variety of clinical environments transitioning from paper to electronic information technology.
METHODS
Current research of perception and cognition in the context of humans working with complex technology suggests that errors are neither solely attributable to lapses in performance or to defects in technology but arise as a product of their interaction.8
Some health information systems may ironically foster cognitive errors rather than reduce the likelihood of medical errors9 if their interface or workplace integration is not designed to fit the task and specific environment. Informatics research and cognitive science can help to characterize the nature of such errors and inform the design and implementation processes to prevent unintended consequences.10
For example, cognitive task analysis (CTA), a core methodology used in cognitive science to study human performance in both laboratory and real-world settings11 was used in this study to characterize the process of triage. Performance of individuals can be studied by examining the information-processing demands of a task, the required domain-specific knowledge and the effectiveness of available technology-based support.12 We can characterize sets of generic clinical tasks that impose similar cognitive demands, such as diagnostic reasoning or patient monitoring and management. A generic task has a common underlying structure that requires similar kinds of reasoning and patterns of inference and can therefore be generalizable to populations of clinicians across clinical settings.6
The selection of relevant data that are necessary to make a decision or to carry out a task and their appropriate representation at the most optimal time can affect the speed and accuracy of clinical decisions. For example, an observational study of 36 triage nurses13 found that decision making is not dependent on the amount of available physiological data and that urgency categorization is of often based on subjective data and expertise. However, triage time decreased if the nurse was aware of the patient’s case prior to arrival. Such findings can inform the design of triage decision support that may, for example, generate a patient record summary at the time of the patient’s identification upon arrival.
A comprehensive methodology used in this analysis comprises several techniques that collect information on different aspects of the triage process and combine them into a rich, detailed description of events that characterize the process and its failures. Similar approach has been used to analyze a serious medication error in a case study of an overdose following a failure in interaction between humans and a computer-based provider order entry system related to the ordering of potassium chloride.14
Study design
We have conducted a qualitative, descriptive study of triage decision making and workflow management in a large urban adult emergency department. Ethnographic observational methods such as shadowing, structured interviews and task observation were used to collect field data.
Methods of analysis
A thematic coding scheme was developed using a grounded theory approach in which the primary investigator reviewed a subset of protocols for emergent common themes related to difficulties in communication and in technology interaction. Each category was further specified according to difficulties related to personal, computer, device, or policy issues. Communications were coded for the role of involved providers (e.g., pre-triage, triage or district nurse) and mode (e.g., personal, electronic, written).
Shadowing
Thirteen triage nurses were observed at different times of day. The type of events, actions, their time and duration were noted. For example, consultations with clinicians were audio recorded. Collected data were segmented by patient case, temporally ordered and coded for analysis.
Interviews
Seven nurses were asked eleven questions in short interviews (about 15 minutes) to elicit perceptions of their role in triage. They were asked to describe a typical workday, list closest collaborators and their most commonly used mode of communication. They were also asked a series of open-ended questions about the convenience of information access, their opinion on potential improvements of the triage process, and asked to recall and describe an adverse event they had observed. In the last part of the interview, the nurses were asked to rate the frequency of guideline use and their perceived utility, and to rate how the usefulness of current information technology. Lastly, we asked them to describe what improvements in technology they would like to see implemented.
Semantic networks
A workflow model was constructed by mapping the representations of observed actions of individual patient cases. An analysis of the network can identify points of difficulties in communication and decision making at every stage of triage. Time stamps allowed duration estimates of each event and their temporal distribution. Semantic networks represent well the dynamic triage environment and make possible the identification of areas where clinicians need support tools. The findings allowed us to suggest technological interventions and their most optimal way of implementation.
Decision making
Urgency classification as explained by nurses in interviews has been analyzed.
RESULTS
The results of workflow and semantic analyses were combined with observational data and the most important findings and recommendations are summarized in Table 1.
Table 1.
Findings and recommendations following a task analysis
| No | Task | Prov | Tm | Com | IT | Findings - Problems | Recommendations |
|---|---|---|---|---|---|---|---|
| Pre-triage | |||||||
| 1 | ID patient | Pre-Triage Nurse | 1–2 minutes | Per | N | Privacy concerns; misspelled names may cause multiple entries in EMR | Separate from waiting room; electronic entry of pt. names |
| 2 | Urgency | N | No decision support; patient history and practice guidelines not accessible | Integrated tracking and EMR systems for immediate recall | |||
| 3 | Patient Destination | Per | N | Waiting room activity not monitored; no direct communication with fast-track | Pts may be given bracelets; alerts to fast-track personnel | ||
| 4 | Paper form | Wrt | N | Legibility; single copy for all clinicians | Replace by electronic system | ||
| Triage | |||||||
| 5 | Assessment | Triage Nurse | 12 minutes | Per
Wrt |
N | Interpreter inaccessible; EMR with visit history unavailable; no guidelines | Communication via PC or intercom; electronic guideline |
| 6 | Vitals | Wrt | N | Done by nurse if technician unavailable | |||
| 7 | Triage category | Wrt
Per |
N | No decision support available; patient EMR history, allergies unavailable | EMR may be ready from pre-traige stage for overview | ||
| 8 | Tests | Wrt | N | Paper ordering in place; execution of quick tests like blood sugar level | Replace by computer-based ordering system | ||
| 9 | Tracking | Elc | Y | Duplication of data from paper; manual updates of state not always accurate | Integrated system with EMR; automatic updates via RFID | ||
| 10 | Workload estimate | Per
Elc |
Y | Cognitively difficult; requires calls when tracking system is not updated | Tracking can automate this with algorithms and updates | ||
| 11 | Patient Destination | Per
Elc |
Y | Awareness of current overall workload of district nurses required | Tracking system to allocate patients to appropriate area | ||
| ED Transfer | |||||||
| 12 | Find a bed | Triage Nurse | 3 minutes | Per | N | Often unavailable, patients crowded around main desk area on chairs | Electronic tracking to signal availability of beds sooner |
| 13 | Find district nurse | Per | N | Nurses have workload of 10–15 pts and can be at many locations | Personal RFID tracking and reporting, wireless alerts | ||
| 14 | Present patient | Per | N | When the patient case explained, chart is often not available (at registration) | Integrated tracking and EMR available in real time to all | ||
| Registration | |||||||
| 15 | Copy form to EMR | Clerk | ? | Elc
Wrt |
Y | Second manual copying of pt data; transcript errors; duplication of records | Electronic chart updated anytime during the visit |
Legend: Prov-Provider; Tm-Duration; Com-Communication; IT-Comp. support available; Per-Personal; Wrt-Written; Elc-Electronic;
Process and task description
The triage process involved 15 discrete tasks (columns One and Two of Table 1) that were completed in sequence and can be defined as parts of four work segments: pre-triage, triage, the transfer of a patient to a specific treatment area, and registration. There were care providers in four roles: A pre-triage nurse, triage nurse, a district (area) nurse, and an emergency room technician. District nurses are assigned to four treatment areas (A–D) and each attends to 10–15 patients at a time. Walk-in patients first give their reason for the visit to the pre-triage nurse positioned at the entrance who then initiates tracking by writing down their name, date of birth and the chief complaint on a printed form (1). The nurse assigns level of urgency (2) and sends the patients either directly to fast-track treatment or to the waiting room (3). As charts accumulate, the nurse sorts them by urgency and places them to a bin inside the triage room (4). Patients arriving by ambulance bypass the pre-triage and the waiting room. Clinical triage evaluation of a patient starts with the triage nurse taking the top chart from the bin and locating the patient in the waiting room. An interpreter may be called for Spanish speaking patients who make up a significant portion of the ED population. The nurse examines the patient (5) and charts findings on the paper form. Vital signs are recorded (6) and the patient is assigned an urgency category (7). Diagnostic tests such as blood sugar, hemoglobin, or EKG may be ordered if indicated (8). After the evaluation, most of the charted data is entered into a computer-based patient tracking system (9), the nurse estimates the current workload of district nurses in each of the four treatment areas (10), and after verbal confirmation with other triage nurses to avoid sending two patients to the same area, decides on the treatment location of the patient inside the ED (11). The destination area and the assigned district nurse are noted on the chart and the patient is either taken inside the ED or told to wait in the waiting room (12). The triage nurse typically escorts the patient and searches for the district nurse (13) and verbally presents the case report (14). The chart is handed to the registration clerk who enters the data into the electronic patient record.
Findings and recommendations
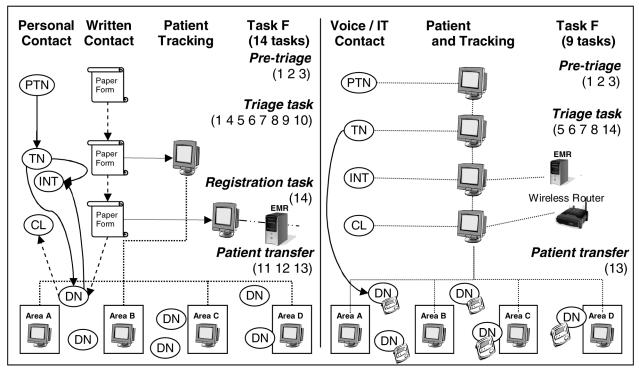
The construction and interpretation of the semantic network analysis was crucial for the identification of communication flow, bottlenecks and repetitive tasks. A graphical representation of the observed task flow, communication patterns and patient tracking is shown in the left side of Figure 1, and the proposed changes on the right. Pre-triage station is located near the entrance to the usually full waiting room, creating a concern for patients whose private conversation with the nurse can be easily overheard by others. The immediate area could be shielded by a physical barrier. Patients are asked to present identification from which personal data are hand-copied on a paper form. The pre-triage nurse should instead have a workstation networked to the hospital EMR and initiate integrated paperless charting and tracking by searching for an existing record so that returning patients would have history, allergies and other pertinent data ready for the triage nurse in the next step. Patients should be issued at this point a bracelet with name and encoded basic data (e.g., an RFID tag) for quick identification later in the process. During the triage proper, the nurse needs to enter the data on a chart and also copy them into a tracking system not currently connected to the hospital EMR. The implementation of a single, integrated electronic system that would populate automatically most known fields that now have to be filled in would save entry time and allow for a better task division between pre-triage and triage nurses. For example, there is usually a long waiting time between the two steps so the shorter pre-triage could be expanded to prepare more data for the subsequent providers without creating an overall delay in patient processing. Real-time decision support on urgency levels, based in part on data stored in the EMR and on newly entered information, may help to avoid medical errors that ensue from a failure to treat certain conditions within a recommended period of time. The triage nurse then has to assign the patient to a district nurse according to current patient load and urgency level. This task involves a cognitively difficult estimate of the total number of patients in each area while paying particular attention to urgency level distribution and factoring in the number of available physicians. To ensure that the chosen district nurse’s availability has not changed since the last nurse list update, each triage nurse has to communicate with others before making a final decision and then verbally announce it. The nurses are forced to keep a mental record of the patients they have recently assigned as the tracking record is often not updated quickly enough. A system automating updates in real time, for example by tracking patients movement through RFID tagging, can eliminate this step entirely while balancing patient assignment load according to a pre-determined algorithm. Similar wireless locating technology can be used to find the district nurse in shorter time and to send alerts to her mobile device (see Figure 1) about a new incoming patient. The registration task could also be eliminated as the tracking and EMR systems would be integrated, and some electronic entry tasks currently performed by the nurses easily reassigned to a clerk. Communication patterns that currently rely mostly on verbal or personal contact could be changed by using asynchronous, less interruptive means, differentiated by urgency priority. For example, implementing instant messaging on workstations and wireless devices or using voice-over-IT for interpreting services or consultations may diminish unnecessary disruptions of workflow.
Figure 1.
Communication and workflow diagram - current and proposed configurations
Legend: PTN-Pre-triage nurse; TN-Triage nurse; INT-Interpreter; CL-Clerk; DN-District nurse
CONCLUSIONS
We found that the cause of many delays, inefficiencies and opportunities for error were the product of failures in interaction among human and system agents. Information technology was either not implemented or was not integrated well into the workflow, often resulting in task duplication or suboptimal task division. Our comprehensive method of data collection and analysis has allowed us to characterize the current process of emergency care and its failures based on observations of real interactions and communications during the actual work process carried out by clinicians the field. We could not have made appropriate recommendations for the improvement of the process without such a multifaceted and detailed analysis.
The errors and problems we described are likely to occur within similar systems at other institutions. Increasingly complex systems of care delivery require comprehensive analyses of human actions and errors for design changes that emphasize clarity of communication and the implementation of technology that supports specific user tasks.
REFERENCES
- 1.Lewin Group T. The results of the American Hospital Association Survey of emergency Department (ED) and hospital capacity. Falls Church, VA: American Hospital Association; 2002. Apr, Emergency department overload: A growing crisis. [Google Scholar]
- 2.Trzeciak S, Rivers EP. Emergency department overcrowding in the United States: An emerging threat to patient safety and public health. Emerg Med J. 2003;20(5):402–5. doi: 10.1136/emj.20.5.402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.McNutt RA, Abrams R, Arons DC. Patient safety efforts should focus on medical errors. J Am Med Assoc. 2002 Apr 17;287(15):1997–2001. doi: 10.1001/jama.287.15.1997. [DOI] [PubMed] [Google Scholar]
- 4.Gordon JA, Billings J, Asplin BR, Rhodes KV. Safety net research in emergency medicine: proceedings of the Academic Emergency Medicine Consensus Conference on "The Unraveling Safety Net". Acad Emerg Med. 2001;8(11):1024–9. doi: 10.1111/j.1553-2712.2001.tb01110.x. [DOI] [PubMed] [Google Scholar]
- 5.Bates DW, Ebell M, Gotlieb E, Zapp J, Mullins HC. A proposal for electronic medical records in U.S. primary care. J Am Med Inform Assoc. 2003 Jan–Feb;10(1):1–10. doi: 10.1197/jamia.M1097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Patel VL, Kaufman DR, Arocha JF. Emerging paradigms of cognition in medical decision-making. J Biomed Inform 2002. 2002;35:52–75. doi: 10.1016/s1532-0464(02)00009-6. [DOI] [PubMed] [Google Scholar]
- 7.Kushniruk AW, Kaufman DR, Patel VL, Levesque Y, Lottin P. Assessment of a computerized patient record system: a cognitive approach to evaluating medical technology. MD Comput. 1996 Sep–Oct;13(5):406–15. [PubMed] [Google Scholar]
- 8.Woods DD, Roth EM. Cognitive engineering: Human problem solving with tools. Hum Factors. 1988;30(4):415–30. [Google Scholar]
- 9.Bates DW, Cohen M, Leape LL, Overhage JM, Shabot MM, Sheridan T. Reducing the frequency of errors in medicine using information technology. J Am Med Inform Assoc. 2001 Jul–Aug;8(4):299–308. doi: 10.1136/jamia.2001.0080299. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Ash JS, Berg M, Coiera EW. Some unintended consequences of information technology in health care: The nature of patient care information system-related errors. JAMIA. 2004;11(2):104–12. doi: 10.1197/jamia.M1471. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Schraagen JM, Chipman SF, Shute VJ. State-of-the-art review of cognitive task analysis techniques. In: Schraagen JM, Chipman SF, editors. Cognitive task analysis. Mahwah, NJ: Lawrence Erlbaum Associates, Inc; 2000. pp. 467–87. [Google Scholar]
- 12.Patel VL, Arocha JF, Kaufman DR. A primer on aspects of cognition for medical informatics. JAMIA. 2001 Jul;8(4):324–43. doi: 10.1136/jamia.2001.0080324. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Gerdtz MF, Bucknall TK. Triage nurses' clinical decision making. An observational study of urgency assessment. J Adv Nurs. 2001;35(4):550–61. doi: 10.1046/j.1365-2648.2001.01871.x. [DOI] [PubMed] [Google Scholar]
- 14.Horsky J, Kuperman GJ, Patel VL. Comprehensive analysis of a medication dosing error related to CPOE. JAMIA. 2005;12(4):377–82. doi: 10.1197/jamia.M1740. [DOI] [PMC free article] [PubMed] [Google Scholar]