Abstract
Factors contributing to low adherence to clinical guidelines by clinicians are not well understood. The user interface of ATHENA-HTN, a guideline-based decision support system (DSS) for hypertension, presents a novel opportunity to collect clinician feedback on recommendations displayed at the point of care. We analyzed feedback from 46 clinicians who received ATHENA advisories as part of a 15-month randomized trial to identify potential reasons clinicians may not intensify hypertension therapy when it is recommended. Among the 368 visits for which feedback was provided, clinicians commonly reported they did not follow recommendations because: recorded blood pressure was not representative of the patient’s typical blood pressure; hypertension was not a clinical priority for the visit; or patients were nonadherent to medications. For many visits, current quality-assurance algorithms may incorrectly identify clinically appropriate decisions as guideline nonadherent due to incomplete capture of relevant information. We present recommendations for how automated DSSs may help identify “apparent” barriers and better target decision support.
Introduction
Adherence to hypertension guidelines remains low despite evidence that adequate blood pressure (BP) control significantly reduces the risk for cardiovascular events.1 Numerous strategies to improve clinician adherence have yielded modest improvements.2 A better understanding is needed of the factors that impede or facilitate incorporation of recommended best practices into clinicians’ daily practice.
Surveys3–5 and focus groups6,7 are typical methods used to investigate barriers to guideline adherence. However, these approaches often engage clinicians when they are temporally remote from the specific clinical scenarios in which medical decisions are made, increasing the likelihood that physicians will have a biased recall of specific management decisions.
Collecting feedback at the point of care during clinical practice offers several distinct advantages to data collection methods such as surveys. First, when integrated with the presentation of decision support, a point-of-care feedback interface facilitates real-time submission of clinician feedback in the context of decision-making and can reduce recall biases present in clinician surveys. Second, clinician feedback is automatically linked to the specific patient scenario and/or specific displayed drug recommendation about which the clinician is commenting. Finally, submitted comments are automatically logged by the DSS, eliminating the need for respondents to return surveys as required with paper-based data collection methods.
ATHENA-HTN
The ATHENA DSS (Assessment and Treatment of Hypertension: Evidence-based Automation Decision Support System, now known as ATHENA-HTN) is an automated guideline-based DSS for the management of hypertension.8–10 ATHENA-HTN delivers advisories with patient-specific recommendations to clinicians in primary care clinics at the point of care via an interface to the Veterans Affairs (VA) Computerized Patient Record System (CPRS).
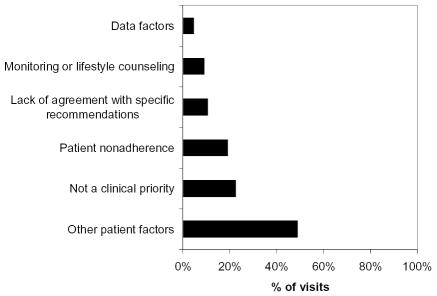
The ATHENA-HTN user interface, which describes all clinician comments as “optional and welcome”, has three features designed to collect feedback during point-of-care use of the system. First, clinicians can report that hypertension is not the focus of the specific patient visit and opt out of the ATHENA advisory by clicking on a button noting “not a clinical priority”. Second, in response to specific displayed drug recommendations, clinicians may select up to eight options from a “checklist” of possible explanations for not pursuing the recommended action (Figure 1). Third, clinician can enter free-text comments into a feedback box. A previous study illustrated how point-of-care clinician comments collected via the ATHENA-HTN free-text feedback box feature may be used in post-fielding surveillance of the DSS after deployment.11
Figure 1.
Checklist of reasons for not adhering to a displayed drug recommendation
Patients with elevated BPs represent the most pressing cases in hypertension management because of their increased risk for cardiovascular events.12 Surveys linking physician-reported barriers with specific patient visits suggest that physicians may decide not to follow guidelines to intensify antihypertensive drug therapy because they are satisfied with the patient’s BP4 or improvement in BP over time,5 believe that more time is needed to observe a drug effect,5 or consider home BP measurements to be satisfactory.5 In this paper, we analyze clinician comments provided at the point of care via an automated DSS for hypertension management (ATHENA-HTN) in order to identify potential barriers to guideline adherence.
Material and Methods
This is a qualitative analysis of point-of-care clinician feedback collected via ATHENA-HTN to identify potential barriers to clinician guideline-concordant intensification of antihypertensive drug therapy.
Collection and classification of feedback
As part of a randomized trial to assess the overall effect of ATHENA-HTN on guideline concordance and BP, recommendations were generated daily for 15 months at nine geographically-dispersed clinical sites within the Durham VA, Palo Alto VA, and San Francisco VA Health Care Systems.11 Ninety-one out of 173 primary care clinicians (i.e., attending physicians, registered nurse practitioners, physician assistants, and residents) participating in the randomized trial were assigned to the experimental arm. These clinicians received the ATHENA advisory and had the opportunity to provide point-of-care feedback. Feedback was logged into a Microsoft SQL database.
Two ATHENA-HTN team members (SBM, ASC) reviewed free-text comments for intellectual content and to identify common themes. They compared their classifications for consistency. When they found discrepancies, they attempted to reach consensus through discussion. Final decisions were adjudicated by a third team member (MKG).
Subsequent classification of data from all feedback sources into barriers-related concepts was guided by a framework for guideline adherence developed by Cabana et al.13 Categories based on the Cabana et al. framework included: patient non-adherence (e.g., “patient nonadherent with meds”); other patient factors (e.g., “patient refuses to increase current medications”, “BP doing well by home readings”, “multiple side effects to multiple different antihypertensives”); lack of agreement with specific recommendations (e.g., “can’t add an ACEI”, “no need to change meds”); and need for more monitoring or lifestyle counseling (e.g., “will follow for now”). Patient non-adherence was considered distinct from other patient factors because it potentially influences clinician attitudes towards the expected benefit of intensification of therapy (described as “lack of outcome expectancy” by Cabana et al.). In contrast, other patient factors such as adverse drug effects or patient preference are not expected to affect clinician attitudes about expected benefit, but may affect whether the displayed drug recommendation is clinically appropriate for the specific patient scenario (described as “external barriers” by Cabana et al.). Two additional categories were created by team members for feedback that fell outside the Cabana et al. framework: (1) not a clinical priority and (2) data factors (e.g., “patient does not have diabetes”).
The ATHENA advisory was displayed to 91 clinicians at 13,942 visits. At 57% of these visits (7,978/13,942), the patient had a recorded BP above target. Of the high-BP visits, antihypertensive therapy was not intensified 66% of the time (5,241/7,978). Forty-six clinicians provided barriers-related feedback at 7% of high-BP visits where therapy was not intensified (368/5,241). Among the 46 clinicians who gave any barriers-related feedback, the median response was four comments per clinician (range: 1, 48; interquartile range: 1, 12).
Analytic approach
For the 368 visits at which clinicians provided barriers-related feedback, we calculated the overall percent of visits at which each type of potential barrier was reported. Because multiple barriers could be reported for a given visit, we also calculated the frequency of specific visit-level patterns of reported barriers as a percent of all visits. Preliminary analyses identified two clinicians who provided a substantially greater number of comments compared to others in the sample. We therefore repeated our analysis after removing these outliers. The frequency of reported barriers did not differ significantly using the two approaches, so we present only results based on the complete sample of visits. Analyses were performed using SAS software, Version 9.1 of the SAS System for Windows (SAS Institute, Cary, NC).
Results
Patients had moderately or significantly elevated BPs at 76.1% of the visits in our sample (Table 1). At 63.9% of visits, patients were already being managed with two or more antihypertensive medications; and for over three-quarters of visits, BP remained uncontrolled from the previous office visit.
Table 1.
Characteristics of high-BP visits without treatment intensification for which barriers-related feedback was provided (n=368)
| Characteristic | |
|---|---|
| Patient age at visit, mean years (sd) | 68 (12) |
| Male, % | 95.9 |
| Race/Ethnicity | |
| White, non-Hispanic, % | 40.5 |
| Black, non-Hispanic, % | 16.6 |
| Other, % | 2.4 |
| Unknown, % | 40.5 |
| BP level above target*† | |
| Slightly elevated, % | 23.9 |
| Moderately elevated, % | 53.8 |
| Significantly elevated, % | 22.3 |
| Number of active antihypertensive medications‡ | |
| None, % | 12.5 |
| 1 drug, % | 23.6 |
| 2 drugs, % | 37.8 |
| 3 drugs, % | 19.8 |
| 4 drugs, % | 6.3 |
| Visits occurring <30 days after previous visit, %§ | 14.4 |
| Elevated BP at previous visit, %§ | 78.3 |
For patients with a diagnosis of heart failure, diabetes, or renal failure, target BP is defined as systolic BP (SBP)<130 mm Hg and diastolic BP (DBP)<85 mm Hg. For all other patients, target BP is defined as SBP<140 mm Hg and DBP<90 mm Hg.
“Slightly elevated”: SBP or DBP <5 mm Hg above target. “Moderately elevated”: BP>5 mm Hg above target and (SBP<160 and DBP<100). “Significantly elevated”: SBP>160 or DBP>100.
Visits at which patients were on >4 antihypertensive drugs were ineligible for ATHENA-HTN.
Two visits were missing BP for the previous visit.
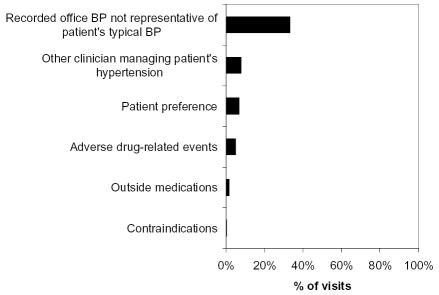
Overall, “other patient factors” was the most frequently reported barrier to intensifying therapy (49%), followed by clinician perceptions that hypertension was not a clinical priority for that visit (23%), and patient non-adherence (19%) (Figure 2). The need to continue monitoring and/or to provide lifestyle counseling was less frequently reported, but was described in nearly 1 in 10 visits.
Figure 2.
Frequency of potential barriers to guideline adherence, among high-BP visits with barriers-related feedback and no intensification of therapy (n=368)*
*Multiple responses were allowed. Percentages do not sum to 100%.
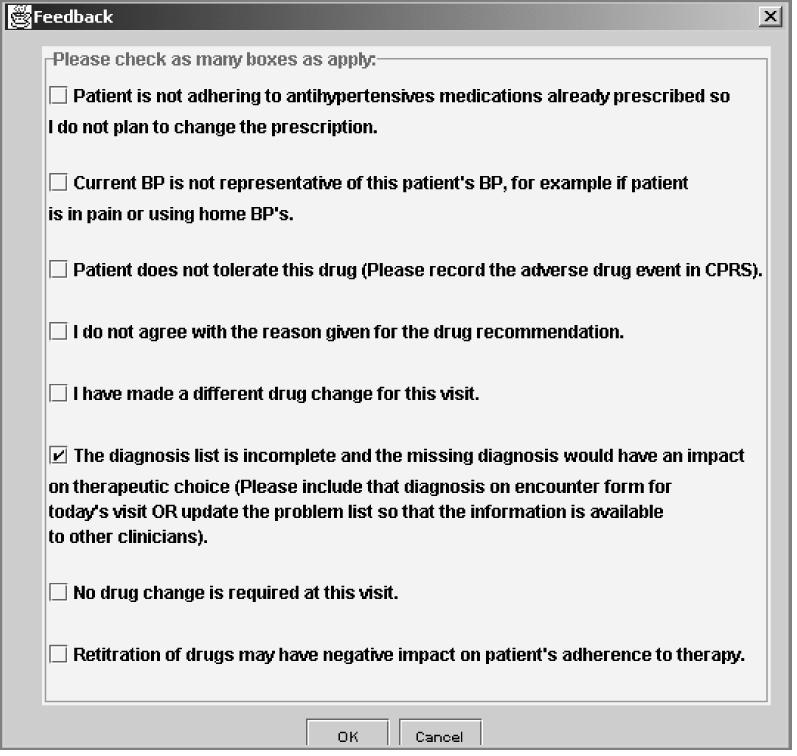
When assessed by the specific pattern of barriers reported at a given visit, two or more types of barriers were reported in 14.4% of visits (Figure 3). Among visits for which only one type of barrier was reported, the relative frequencies of the different barrier types remained unchanged.
Figure 3.
Frequency of specific patterns of potential barriers, among high-BP visits with barriers-related feedback and no intensification of therapy (n=368)
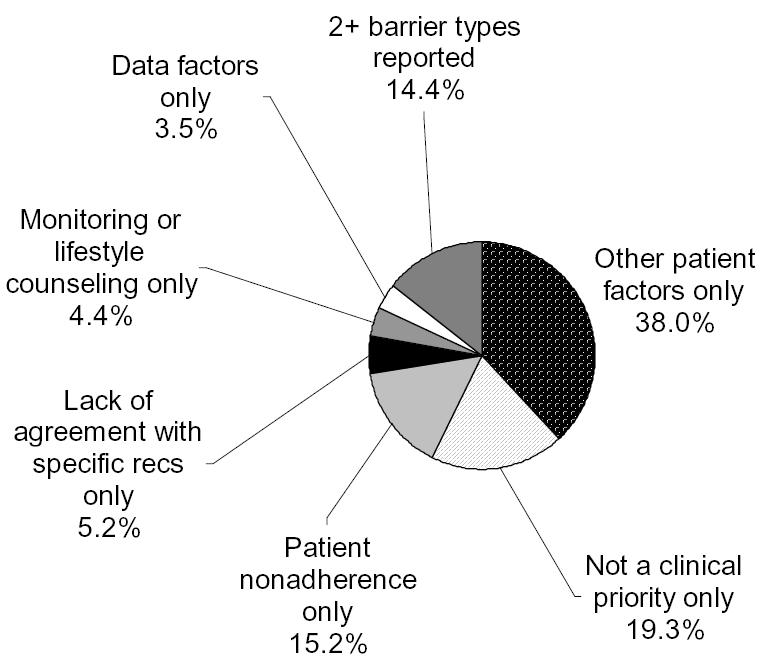
An exploration of themes comprising the “other patient factors” category found that clinicians believed the office BP was not representative of the patient’s typical BP at 122 visits (e.g., home BPs below target, patient currently experiencing pain), or 68% of the 180 visits with reported “other patient factors” barriers and 33% of visits overall (Figure 4). At 8% of visits overall, clinicians who received the ATHENA advisory noted that another clinician was responsible for managing the patient’s hypertension. Other themes included patient preference (7%) and medication-related issues (i.e., adverse drug events, outside medications, contraindications) (7%).
Figure 4.
Frequency of “other patient factors” themes, among high BP-visits with barriers-related feedback and no intensification of therapy (n=368)*
*Multiple responses were allowed. Percentages do not sum to 100%.
Discussion
We have developed an automated, practical approach to collecting point-of-care information from clinicians via ATHENA-HTN. Analysis of this feedback revealed a variety of patient-, clinician-, and data-related reasons for why clinicians did not follow guidelines to intensify treatment. For many visits, we found that clinician feedback described influential patient and data factors that were not systematically captured by the electronic medical record (EMR) data available to the DSS. This suggests that many decisions currently identified by the DSS as guideline nonadherent may in fact represent clinically appropriate decisions.
Our findings shed light on several specific areas where automated decision support systems for hypertension management may be improved. Compared with human review of medical records, computer-aided review can produce different judgments about whether a clinician behavior is guideline nonadherent. This is due in part to the presence of clinically relevant information in the EMR that is entered in non-standardized formats (e.g., free-text comments).14 In a randomized trial comparing office-BP-driven hypertension treatment decisions with home-BP-driven decisions, reliance on home BPs (i.e., information often captured only in free-text in medical records) led to less intensive drug treatment.15 Our finding that clinicians frequently did not consider the recorded office BP to be representative of the patient’s typical BP is consistent with that of Ferrari et al., who found that satisfactory patient self-measured BPs were a main reason clinicians reported for not intensifying therapy.5 Standardized collection and coding of data on home BPs may improve the usefulness and applicability of displayed recommendations in facilitating optimal hypertension management. Analysis of point-of-care feedback also identified instances where the primary care clinician was not responsible for managing the patient’s hypertension. Approaches to identify the correct clinician decision-maker are needed to ensure effective guideline implementation and to appropriately target decision support.
Other factors identified in our study, such as clinician reports that hypertension was not a clinical priority or that more monitoring was needed, have been reported in previous studies.3–5 These factors may describe appropriate clinician guideline non-adherence in certain patient scenarios. However, Oliveria et al. found that clinicians often deferred intensification even when uncontrolled hypertension had been documented for at least six months preceding the patient’s most recent visit.4
Our study has several limitations. Given the extra work required to offer optional comments, it may be expected that busy clinicians would do so infrequently. Clinicians voluntarily provided feedback at 7% of visits. Many barriers may be under-reported. While provision of feedback was not associated with patient demographic characteristics or the number of active antihypertensive medications, clinicians in our study were more likely to provide feedback at visits where the patient had a significantly elevated BP and/or an elevated BP at their previous visit (data not shown). It is possible that clinicians selectively offered comments for scenarios they encountered repeatedly or for scenarios they believed required justification. We are not able to confirm this using our data. For these reasons, our findings may not be generalizable beyond our study sample. Nevertheless, these spontaneously offered comments, provided during actual patient encounters, offer additional insight into the various factors and challenges clinicians consider at the time of the medical decision.
In summary, point-of-care feedback collected from clinicians via ATHENA-HTN provides a rich source of information about perceived barriers and other factors related to adherence to guidelines. Integration of a variety of feedback features into ATHENA-HTN offered clinicians the opportunity to provide holistic impressions of the applicability of hypertension management guidelines to specific patient scenarios, as well as responses to specific drug recommendations. This ability to link data available in the EMR with computer-generated advice and clinician responses allowed us to identify several important clinician, patient, and data barriers to guideline-concordant intensification of therapy. Our study suggests that clinicians’ failure to intensify therapy may reflect valid concerns about whether this action is appropriate for many patients.
Acknowledgements
This work was supported in part by VA HSR&D CPG-97-006, CPI-275, and IIR 20-034, and NIH LM05708. Dr. Lin’s effort was supported by AHRQ NRSA HS000028-19. The authors thank the staff of VA medical centers in Durham, Palo Alto, and San Francisco. The views expressed are those of the authors and not necessarily those of the Dept. Veterans Affairs or other affiliated organizations.
References
- 1.Hajjar I, Kotchen TA. Trends in prevalence, awareness, treatment, and control of hypertension in the United States, 1988–2000. JAMA. 2003;290:199–206. doi: 10.1001/jama.290.2.199. [DOI] [PubMed] [Google Scholar]
- 2.Walsh J, McDonald KM, Shojania KG, et al. Hypertension care. Closing the quality gap: a critical analysis of quality improvement strategies. In: Shojania KG, McDonald KM, et al., editors. Vol. 3. Rockville, MD: AHRQ; 2005. #04-0051-3. [PubMed] [Google Scholar]
- 3.Mottur-Pilson C, Snow V, Bartlett K. Physician explanations for failing to comply with "best practices". Eff Clin Pract. 2001;4:207–13. [PubMed] [Google Scholar]
- 4.Oliveria SA, Lapuerta P, McCarthy BD, et al. Physician-related barriers to the effective management of uncontrolled hypertension. Arch Intern Med. 2002;162:413–20. doi: 10.1001/archinte.162.4.413. [DOI] [PubMed] [Google Scholar]
- 5.Ferrari P, Hess L, Pechere-Bertschi A, Muggli F, Burnier M. Reasons for not intensifying antihypertensive treatment (RIAT): a primary care antihypertensive intervention study. J Hypertens. 2004;22:1221–9. doi: 10.1097/00004872-200406000-00024. [DOI] [PubMed] [Google Scholar]
- 6.Cranney M, Warren E, Barton S, Gardner K, Walley T. Why do GPs not implement evidence-based guidelines? A descriptive study. Fam Pract. 2001;18:359–63. doi: 10.1093/fampra/18.4.359. [DOI] [PubMed] [Google Scholar]
- 7.Powell-Cope GM, Luther S, Neugaard B, Vara J, Nelson A. Provider-perceived barriers and facilitators for ischaemic heart disease (IHD) guideline adherence. J Eval Clin Pract. 2004;10:227–39. doi: 10.1111/j.1365-2753.2003.00450.x. [DOI] [PubMed] [Google Scholar]
- 8.Goldstein MK, Coleman RW, Tu SW, et al. Translating research into practice: organizational issues in implementing automated decision support for hypertension. JAMIA. 2004;11:368–76. doi: 10.1197/jamia.M1534. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Goldstein MK, Hoffman BB, Coleman RW, et al. Patient safety in guideline-based decision support for hypertension management: ATHENA DSS. JAMIA. 2002;9:S11–16. [PMC free article] [PubMed] [Google Scholar]
- 10.Goldstein MK, Hoffman BB, Coleman RW, et al. Implementing clinical practice guidelines while taking account of changing evidence: ATHENA DSS, an easily modifiable decision-support system for managing hypertension in primary care. Proc AMIA Symp. 2000:300–4. [PMC free article] [PubMed] [Google Scholar]
- 11.Chan A, Martins S, Coleman R, et al. Post fielding surveillance of a guideline-based decision support system. Advances in patient safety: from research to implementation. In: Henriksen K, Battles J, et al., editors. Vol. 1. Rockville, MD: AHRQ; 2005. #05-0021-1. [PubMed] [Google Scholar]
- 12.Chobanian AV, Bakris GL, Black HR, et al. Seventh report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure. Hypertension. 2003;42:1206–52. doi: 10.1161/01.HYP.0000107251.49515.c2. [DOI] [PubMed] [Google Scholar]
- 13.Cabana MD, Rand CS, Powe NR, et al. Why don't physicians follow clinical practice guidelines? A framework for improvement. JAMA. 1999;282:1458–65. doi: 10.1001/jama.282.15.1458. [DOI] [PubMed] [Google Scholar]
- 14.van der Lei J, Musen MA, van der Does E, Man in 't Veld AJ, van Bemmel JH. Comparison of computer-aided and human review of general practitioners' management of hypertension. Lancet. 1991;338:1504–8. doi: 10.1016/0140-6736(91)92311-o. [DOI] [PubMed] [Google Scholar]
- 15.Staessen JA, Den Hond E, Celis H, et al. Antihypertensive treatment based on blood pressure measurement at home or in the physician's office: a randomized controlled trial. JAMA. 2004;291:955–64. doi: 10.1001/jama.291.8.955. [DOI] [PubMed] [Google Scholar]