Abstract
Objective
To present the diagnostic features of lateral epicondylosis and response to treatment by Active Release Technique® (ART), a promising treatment for lateral epicondylosis.
Clinical Features
The most important feature is pain at the lateral epicondyle of the humerus, most notably in actively extending or passively flexing the wrist.
Intervention and Outcome
Treatment involves eliminating any inflammation, reducing muscular pain and hypertonicity, correcting biomechanical dysfunction, and restricting/modifying the offending activity. ART® was successfully utilized in an attempt to remove adhesions and promote restoration of normal tissue texture. A sports specific rehabilitation protocol was employed to re-establish wrist extensor strength and interferential current and ice were used to control pain and residual inflammation.
Conclusion
A combination of soft tissue therapy, rehabilitation, and therapeutic modalities is a protocol that may be used by both allopathic and chiropractic practitioners alike, and allow for the athletic patient to return to play as quickly as possible.
Keywords: tennis elbow, lateral epicondylosis, tendonitis, extensor carpi radialis brevis, ART®, rehabilitation
Abstract
Objectif
Pour présenter les manifestations cliniques au traitement par la méthode Active Release Technique® (ART) de l’épicondyle latérale, un traitement prometteur pour cette affection.
Caractéristiques cliniques
La principale manifestation se présente sous forme de douleur à l’épicondyle latérale de l’humérus, plus particulièrement en déployant activement le poignet et en faisant des exercices passifs de souplesse.
Intervention et résultats
Le traitement consiste à éliminer toute inflammation, à atténuer la douleur musculaire et l’hypertonie, à corriger la dysfonction biochimique et à restreindre et à modifier l’activité à la source du problème. ART® a été utilisé avec succès quand on a tenté de retirer les adhérences et de favoriser le rétablissement de la texture normale des tissus. On a eu recours à un protocole de réadaptation spécifique inspiré de la médecine sportive pour rétablir la force de l’extenseur du poignet et le courant interférentiel et la glace pour contrôler la douleur et l’inflammation résiduelle.
Conclusion
Une conjugaison de traitements des tissus, de réadaptation et de modalités thérapeutiques forme un protocole pouvant être utilisé tant par la médecine générale que les chiropraticiens, permettant ainsi aux patients de retourner au jeu le plus rapidement possible.
Introduction
Lateral epicondylitis/lateral epicondylalgia, or tennis elbow is a common pathology of both athletes and non-athletes, affecting 1 to 3 % of the population at large.1,2 This condition is most often associated with overuse or a repetitive stress, as opposed to an acute inflammatory reaction. The lack of pathological evidence of inflammation in these types of injuries has lead most authors to now refer to this condition as an epicondylosis, abandoning the mislabeled “itis”.3–6
However, the choice of treatment options for this condition is even more controversial. There are many treatment options available to the clinician, but their use is often based on anecdotal evidence. Various treatments ranging from conservative to more invasive measures have been described with varying degrees of success, with no conclusive scientific evidence to support any particular treatment protocol.
Although many treatment modalities may be used, few of them rest on scientific evidence and none have really been proven to be more effective than the others. The paucity of evidence on treatments for lateral epicondylosis may stem from several sources, including the self-limiting nature of the condition, the lack of pathophysiological data, the methodological shortcomings of the current studies, and the existence of multiple factors which may influence the outcome.1,7
This paper will highlight the course of lateral epicondylosis in one patient, and examine the anatomy, pathology and treatment options in a review of the literature.
Case Report
A 51-year-old male, right hand dominant recreational tennis player suffered from right elbow pain that had lasted three months. The pain, which had progressively worsened in the previous two weeks was characterized as stiff, achy, and sometimes throbbing and was rated as an 8/10 in intensity on a numeric pain rating (zero being no pain and 10 being the worst pain ever). The patient was no longer able to play tennis. The pain began insidiously after playing in a weekend tournament. Initially he sought out physical therapy care, which included therapeutic ultrasound, ice and an elbow strap. The patient attended eight or nine sessions over one month without improvement to his condition, and he was referred to an orthopedic surgeon for a corticosteroid injection. The injection relieved his symptoms for approximately one month, in which he continued to play tennis with the elbow strap. In the last month his symptoms returned, and in the last two weeks his pain was described to be the worst it had ever been. The pain was noted to be at its worst in the morning, and was aggravated by extending the wrist to brush his teeth, open doors, and carry groceries. Ice and Advil were reported to be minimally relieving. The patient discarded his elbow strap considering it to be of no benefit. No numbness, tingling or weakness was noted in the hand. The patient denied previous trauma to his right elbow, but did recall a similar pain in his left elbow a few years earlier that resolved on its own with rest.
Upon inspection, there was no ecchymosis and the lateral epicondyle and common extensor origin did not appear to be inflamed (no redness or swelling) when compared to the opposite side. All active ranges of motion of the elbow joints were full, while flexion and extension in the right wrist were limited due to pain. Passive range of motion, was also limited by patient discomfort particularly at the end range of right wrist flexion, and was able to reproduce the patient’s chief complaint at the right elbow. Resisted wrist extension and grip strength were very painful and the patient declined to provide much effort as this reproduced a sharp pain at the lateral epicondyle. Motion palpation of the radial head proved unremarkable and was not pain provoking. The common extensor origin was tender to direct palpation, as was the extensor carpi radialis brevis, which was noted to be leathery and lumpy. Orthopedically, Cozen’s test (resisted wrist flexion from a flexed elbow and pronated/extended wrist position) was positive. Mill’s test, (passive extension of the elbow from a flexed elbow, pronated forearm and flexed wrist/finger position) was inconclusive in that it was uncomfortable but did not produce pain at the lateral epicondyle.
The patient was diagnosed with lateral epicondylosis with a myofasciopathy of the extensor carpi radialis brevis. He was treated six times over two weeks with Active Release Technique® (ART) to the affected muscles at the common origin (namely- extensor carpi radialis brevis/longus, and supinator). In addition to the soft tissue treatment, a rehabilitation program was performed (see Table 1), which was followed by 20 minutes of interferential current and 10 minutes of ice. After the first treatment the patient reported to feel 80% better, and at the time of discharge there was complete resolution of his symptoms (VAS 0/10 with no pain provocation on examination). The patient returned to playing tennis and at one and two month follow-ups he denied any exacerbation, playing tennis 2–3 times per week. Consultation with the patient’s racquet club tennis professional also prompted the patient to purchase a light, non-vibrational racquet with moderate string tension, in addition to improving his stroke technique, to prevent any recurrences.
Table 1.
– Rehab Program
| Exercise | Instructions |
|---|---|
| General Stretching – shoulder, elbow, wrist | Active isolated stretching – dynamic
5 minute warm-up |
| Wrist Flexion/Extension | 3 sets of 10 with surgical tubing of increasing difficulty |
| Elbow Flexion/Extension | As above |
| Finger Extension/Flexion | For 1 minute with hand webs of increasing difficulty |
| Forearm Pronation/Supination | 3 sets of 10 with a 5 lb weighted hammer |
| Radial/Ulnar Deviation | 3 sets of 10 with a 3 lb. weighted racquet |
| Eccentric loading of wrist extensors | 1 set of 10 with a 25 lb. dumbbell |
| Plyometric, purse drop (extend from full flexion) | 1 set of 10 with 5 lbs of weight |
| Simulated tennis swings – forehand, backhand, and serve | 3 lb. weighted tennis racquet to Cable cross – 1 set of 20 for each with 5–10 lbs of resistance |
Discussion
Competitive and recreational athletes sustain a wide variety of soft tissue, bone, ligament, tendon and nerve damage to their upper extremities. Most such injuries are related to direct trauma or repetitive stress, and account for a significant amount of “down time” for the athlete in sports where the arm is utilized for throwing, catching, or swinging. Tennis elbow is a painful ailment about the elbow that is common in tennis players. Tennis elbow occurs most commonly in people aged 40 to 50 years with an equal distribution between men and women.3,8,9 The dominant arm is involved in 75% of patients, and the incidence most directly relates to playing time in amateur players.3 It has been reported that nearly 50% of all tennis players over 35 years old and 60% of players over 50 years old suffer from tennis elbow at some point in their career.3
Elbow biomechanics play a very important role in many overhead sporting activities including tennis. The amount of tension and the location of the stress within the elbow joint is dependent on the stroke used and the mechanics of each stroke.10 Electromyographic (EMG) studies of elbow function in tennis have shown that the serving motion creates a larger demand on the elbow than does the ground stroke.10 That being said, it is well known amongst tennis players that improper backhand mechanics is one of the main causes for elbow injuries. In fact, the incidence of lateral epicondylitis has been clinically linked to a one-handed backhand, and greater wrist extension and pronation activity.10 Some tennis instructors teach a double-hand backstroke, a stroke which minimizes wrist pronation, and/or a stroke that avoids leading with the elbow to minimize the potential for improper mechanics.
Traditionally the term tennis elbow has been synonymous with lateral epicondylitis. However, the term epicondylitis suggests an inflammatory process, and as Boyer has pointed out – there is no evidence of acute or chronic inflammation in the publications examining the pathological specimens of patients who were operated on for this condition.11 Repetitive muscle contraction will produce tensile forces within a tendon of an involved muscle, potentially causing microtrauma. If the natural healing process fails, pathological alteration of tissue results in a fibroblastic and vascular response called angiofibroblastic degeneration.3,4,5,6 The pathology of tennis elbow is thus most likely to be angiofibroblastic degeneration at the origin of the wrist extensors, and more suitably referred to as lateral epicondylosis.3,4,5,6
The current understanding of this condition places the specific pathology at the extensor carpi radialis brevis.3,4,12,13 The origin of the extensor carpi radialis brevis is covered by the extensor carpi radialis longus and the extensor communis origin. In fact, the common extensor origin consists of the fused tendons of extensor carpi radialis brevis, extensor digitorum, extensor digiti minimi, and extensor carpi ulnaris. Biomechanical studies of tensile force at the lateral epicondyle further indicate that stretching extensor carpi radialis brevis, extensor digitorum communis and the superficial head of the supinator produce large increases in tensile force at the epicondyle.14 Obviously a thorough understanding of the anatomical arrangement of these muscles and their specific actions is necessary to make a correct diagnosis. Additionally, it is important to rule out other differential diagnoses such as capitellum fracture, lateral collateral ligament injury, osteochondritis dessicans, posterior interosseus nerve syndrome, radial head fracture and synovitis.12
Radiographic analysis of lateral epicondylitis may reveal calcification along the lateral epicondyle however, radiographs as an initial step in diagnosing lateral epicondylosis is not necessary.15 On the other hand a diagnostic ultrasound of the common extensor origin can be used to confirm lateral epicondylitis in patients with elbow pain and add additional information in regards to the severity.16
Most authors suggest that over 90% of patients will respond to conservative care, which may include rest, bracing, strengthening, therapeutic modalities, and steroid injections3,17,18,19,20 Additionally, it has been reported in cases where surgery was required that over 90% of patients responded well.21
The attempted meta-analysis in 1992 by Labelle et al. reviewed 185 articles on the subject of tennis elbow treatment, however only a single paper was considered to be of a good quality design for controlled therapeutic trials. They concluded that there was insufficient evidence to support any single current method of treatment.22 This conclusion was reiterated even more recently in the meta-analysis by Bisset et al. who identified 28 randomised controlled trials which met their minimum criteria.7 These authors suggested that there was a lack of evidence for the long-term benefit of physical interventions in general.7
There have been a number of studies comparing therapeutic modalities with placebo for the treatment of soft tissue injuries such as lateral epicondylosis. There is insufficient evidence to support the use of most physiotherapy interventions and only weak evidence for the efficacy of therapeutic ultrasound in the treatment of tennis elbow.7,22,23,24 Basford et al. assessed patients for pain, tenderness to palpation, grip strength, medication usage, and subjective perception of pain after a double masked, placebo controlled, randomized trial utilizing a low intensity laser. The results of this study showed that there were no significant differences, and they concluded that there was no demonstrable beneficial effect of laser therapy.25
The 2004 systematic review for the efficacy of splinting for lateral epicondylitis identified early positive, but not conclusive evidence supporting the effectiveness of splinting.26 Similarly, there have been conflicting results on the use of braces and orthotic devices, which may be useful in the initial stages of therapy.27,28, 29
The ability to control the pain associated with lateral epicondylagia may be achieved through acupuncture. A recent systematic review suggested that acupuncture was effective in the short-term relief of lateral epicondyle pain.30 The Fink et al. randomized controlled trial for chronic epicondylitis also showed that real acupuncture points showed a reduction of pain and an improvement of function at early follow-up.31 More long-term follow-up would be useful to assess whether acupuncture has a greater role than simply pain modulation.
In addition to the acupuncture findings, manipulations and/or mobilizations have been suggested to have a hypoalgesic effect. The works of Strujis et al. and Paungmali et al. have shown that manipulation of the wrist and mobilization of the elbow may play a role in the management of the pain associated with lateral epicondylitis.32,33 The preliminary evidence does suggest that manipulations and mobilizations may have some positive effects in the reduction of pain and improvement of function.23
Historically, a popular choice for treating tendonitis had been deep friction massages. However as evidenced by the 2002 Cochrane review there is simply not a large enough sample size to draw any conclusions in regards to control of pain or improvement in function.34 The concepts of cross-friction techniques have since evolved into an augmented soft tissue mobilization, more commonly known as the “Graston Technique Instrument-Assisted Soft Tissue Mobilization” or simply Graston.35 The Graston protocol for epicondylosis uses specifically designed stainless steel instruments which are moved with multidirectional strokes around the bony prominence of the elbow. Preliminary studies utilizing this Graston technique have shown promising results when compared to a traditional physiotherapy protocol in the treatment of lateral epicondylitis.36
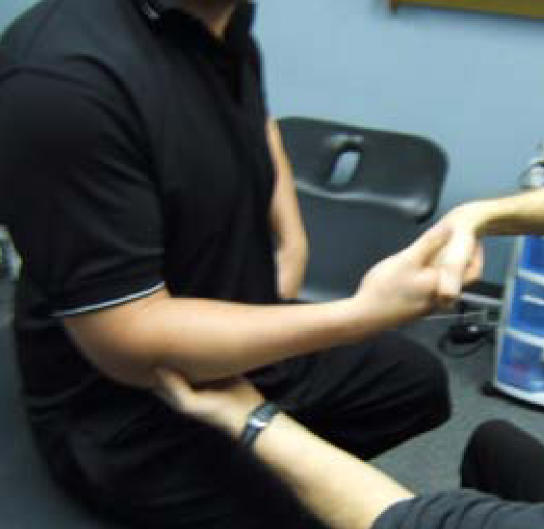
Perhaps the most popular of soft tissue techniques to gain recent notoriety is Active Release Technique or ART®. This therapy is based on the observation that the anatomy of the forearm has traversing tissues situated at oblique angles to one another that are prone to reactive changes producing adhesions, fibrosis and local edema and thus pain and tenderness.37,38 During active release therapy, the clinician applies a combination of deep digital tension at the area of tenderness and the patient actively moves the tissue through the adhesion site from a shortened to a lengthened position.37,38 For example, in order to treat extensor carpi radialis brevis, the clinician applies proximal tension distal to the lateral epicondyle while the patient extends the elbow and pronates and flexes the wrist.37 A preliminary report on the use of ART® for a variety of upper extremity overuse syndromes found a 71% efficacy rate.38 (See Figure 1). Unfortunately, clinical trials on this technique are lacking and at this point, the popularity of ART® is based largely on anecdotal evidence.
Figure 1.
Palpation of extensor carpi radialis longus and brevis with proximal traction to perform an ART pass.
Despite a lack of scientific evidence to show benefit from steroid injection, its use in general practice is common. The 1999 randomized controlled trial by Hay et al. showed a significant improvement in the injection group compared to the naproxen and placebo group at four weeks. However, at one year, all three groups had responded well and there was no significant difference between them.39 Local injections of steroid appear to provide a short-term benefit, but have little long-term benefit and the recurrence rate is high.18,22,39,40,41,42 Considering the known side effects associated with steroids, the usefulness of this treatment is questionable.
On the basis of observational trials for resistant lateral epicondylosis there is a growing trend to recommend extracorporeal shock wave therapy as an alternative treatment for chronic epicondyle pain. Despite the numerous conflicting studies published in the recent years, shock wave therapy appears to be safe and may be effective in pain control.43 Still, there appears to be a significant placebo effect and the literature does not show that shock wave therapy consistently performs better than a sham treatment or standard physiotherapy based treatments.43,44,45,46,47,48,49,50 In fact in the recent systematic review and meta-analysis on physical interventions for lateral epicondylalgia, the authors conclude that shock wave therapy is not beneficial in the treatment of tennis elbow.7
Most conservative treatment plans call for the incorporation of an active rehabilitation program to align collagen fibres and improve tensile strength. Rehab focusing on strength and flexibility exercises for wrist extensors and flexors is considered standard care. Theoretically, if an athlete increases the strength of their wrist extensors, the muscles should be stiffer and able to absorb a greater force and thus transfer less force to the elbow. In addition, appropriate stretching of these muscles (stretch induced hypertrophy) would reduce force transferred to the elbow; and strong posterior shoulder muscles would allow for a quicker movement of the arm and wrist through the zone of impaction with the ball, thereby decreasing the time of tensile load on the elbow. A recent pilot study by Svernlov showed that an eccentric training regime can considerably reduce symptoms of lateral epicondylosis regardless of duration and may be superior to conventional stretching.51 Although rehabilitative exercises are considered the mainstay of successful treatment/prevention of lateral epicondylosis and included with most plans of management, the literature does not specifically substantiate the effectiveness to be greater than the previously described conservative treatments.23
The vast majority of tennis elbow patients respond to non-operative forms of treatment, and only selected cases may benefit from more invasive operative treatments. The percutaneous release of the common extensor origin has been to shown to provide excellent results and appears to be a commendable treatment in patients who do not respond to conservative care.52 Similarly, surgical interventions which identify and remove the pathological tissue that represents angiofibroblastic degeneration have favorable preliminary scientific evidence.5,6,21,53,54 Still, there are no published controlled trials of surgery for lateral elbow pain, and without a control group it is not possible to draw any conclusions about the value of this intervention.55
Conclusions
Lateral epicondylosis is a common ailment, especially amongst athletes who participate in racquet sports. While the healing process is sometimes long and arduous, early recognition and institution of conservative care will allow the majority of patients to recover and return to play. Diagnosis is usually straightforward and can often be attributed to overuse or as a response to a stress overload.
Lateral epicondylosis is certainly a challenging musculoskeletal condition to treat and this is largely due to the lack of definitive evidence for the clinical efficacy of the myriad of treatment approaches seen within the literature.56
Successful treatment involves measures to relieve pain and reduce stress in surrounding tissues while addressing the underlying pathology of angiofibroblastic degeneration and the resulting physical impairments.
To date, despite the large number of studies on lateral epicondylosis/itis there is insufficient evidence to support any single conservative method of treatment due to contradicting results, insufficient subjects per study and the low number of studies per intervention. The utilization of a previously undocumented specific soft tissue treatment – ART® which is intended to remove adhesions and restore normal tissue texture appears to have resolved lateral epicondylosis rapidly in this case. The use of ART® in conjunction with a specifically aimed rehabilitation program in the treatment of tendonopathies warrants further investigations with a larger sample size and a control.
References
- 1.Hong QN, Durand MJ, Loisel P. Treatment of lateral epicondylitis: where is the evidence? Joint Bone Spine. 2004;71(5):369–373. doi: 10.1016/j.jbspin.2003.05.002. [DOI] [PubMed] [Google Scholar]
- 2.Walker-Bone K, Palmer KT, Reading I, Coggon D, Cooper C. Prevalence and impact of musculoskeletal disorders of the upper limb in the general population. Arthritis Rheum. 2004;51(4):642–651. doi: 10.1002/art.20535. [DOI] [PubMed] [Google Scholar]
- 3.Ollivere CO, Nirschl RP. Tennis elbow:current concepts and rehabilitation. Sports Med. 1996;22(2):133–139. doi: 10.2165/00007256-199622020-00006. [DOI] [PubMed] [Google Scholar]
- 4.Regan W, Wold LE, Conrad R, Morrey BF. Microscopic histopathology of chronic refractory lateral epicondylitis. Am J Sports Med. 1992;20:746. doi: 10.1177/036354659202000618. [DOI] [PubMed] [Google Scholar]
- 5.Kraushaar BS, Nirschl RP. Tendonosis of the elbow (Tennis Elbow). Clinical features and finding of histological, immunohistochemical, and electron microscopy studies. J Bone Joint Surg Am. 1999;81:259–278. [PubMed] [Google Scholar]
- 6.Nirschl RP. Elbow tendonosis/tennis elbow. Clin Sports Med. 1992;11:851–870. [PubMed] [Google Scholar]
- 7.Bisset L, Paungmali A, Vincenzino B, Beller E. A systematic review and meta-analysis of clinical trials on physical interventions for lateral epicondylalgia. Br J Sports Med. 2005;39:411–422. doi: 10.1136/bjsm.2004.016170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Terry S. ed. Campbell’s Operative Orthopaedics, 9th ed. St. Louis, USA: Mosby-Year Book; 1998.
- 9.Frostick SP, Mohammad M, Ritchie DA. Sports Injuries of the Elbow. Br J Sports Med. 1999;33:301–311. doi: 10.1136/bjsm.33.5.301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Loftice J, Fleisig GS, Zheng N, Andrews JR. Biomechanics of the elbow in sports. Clin Sports Med. 2004;23(4):519–530. doi: 10.1016/j.csm.2004.06.003. [DOI] [PubMed] [Google Scholar]
- 11.Boyer MI, Hastings H. Lateral tennis elbow: “Is there any science out there? J Shoulder Elbow Surg. 1999;8(5):481–491. doi: 10.1016/s1058-2746(99)90081-2. [DOI] [PubMed] [Google Scholar]
- 12.Conway JE. Clinical evaluation of elbow injuries in the athlete. J Musculoskeletal Med. 1998;15(10):43–52. [Google Scholar]
- 13.Rettig AC. Elbow, forearm, and wrist injuries in the athlete. Sports Med. 1998;25(2):115–130. doi: 10.2165/00007256-199825020-00004. [DOI] [PubMed] [Google Scholar]
- 14.Erak S, Day R, Wang A. The role of the supinator in the pathogenesis of chronic lateral elbow pain: a biomechanical study. J Hand Surg (Br) 2004;29(5):461–464. doi: 10.1016/j.jhsb.2004.06.001. [DOI] [PubMed] [Google Scholar]
- 15.Pomerance J. Radiographic analysis of lateral epicondylitis. J Shoulder Elbow Surg. 2002;11(2):156–157. doi: 10.1067/mpn.2002.121147. [DOI] [PubMed] [Google Scholar]
- 16.Connell D, Burke F, Combes P, McNealy S, Freeman D, Pryde D, Hoy G. Sonographic examination of lateral epicondylitis. AJR Am J Roentgenol. 2001;176(3):777–782. doi: 10.2214/ajr.176.3.1760777. [DOI] [PubMed] [Google Scholar]
- 17.Grundberg AB, Dobson JF. Percutaneous release of the common extensor origin for tennis elbow. Clin Orthop. 2000;376:137–140. doi: 10.1097/00003086-200007000-00019. [DOI] [PubMed] [Google Scholar]
- 18.Servier TL, Wilson JK. Treating lateral epicondylitis. Sports Med. 1999;28:375–380. doi: 10.2165/00007256-199928050-00006. [DOI] [PubMed] [Google Scholar]
- 19.Thomas DR, Plancher KD, Hawkins RJ. Prevention and rehabilitation of overuse injuries of the elbow. Clin Sports Med. 1995;14(2):459–477. [PubMed] [Google Scholar]
- 20.Brown M. The older athlete with tennis elbow : rehabilitation considerations. Clin Sports Med. 1995;14(1):267–273. [PubMed] [Google Scholar]
- 21.Nirschl RP, Pettrone FA. Tennis Elbow: the surgical treatment of lateral epicondylitis. J Bone Joint Surg Am. 1979;61:832–839. [PubMed] [Google Scholar]
- 22.Labelle H, Guibert R, Joncas J, Newman N, Fallaha M, Rivard CH. Lack of scientific evidence for the treatment of lateral epicondylitis of the elbow. J Bone Joint Surg Br. 1992;74:646–651. doi: 10.1302/0301-620X.74B5.1388172. [DOI] [PubMed] [Google Scholar]
- 23.Trudel D, Duley J, Zastrow I, Kerr EW, Davidson R, MacDermid JC. Rehabilitation for patients with lateral epicondylitis: a systematic revie. J Hand Ther. 2004;17(2):243–266. doi: 10.1197/j.jht.2004.02.011. [DOI] [PubMed] [Google Scholar]
- 24.Smidt N, Assendeft WJ, Arola H, Malmivaara A, Greens S, Buchbinder R, van der Windt DA, Bouter LM. Effectiveness of physiotherapy for lateral epicondylitis: a systematic review. Ann Med. 2003;35(1):51–62. doi: 10.1080/07853890310004138. [DOI] [PubMed] [Google Scholar]
- 25.Basford JR, Sheffield CG, Cieslak KR. Laser Therapy: A randomized, controlled trial of the effects of low intensity Nd: YAG irradiation of lateral epicondylitis. Arch Phys Med Rehabil. 2000;81:1504–1510. doi: 10.1053/apmr.2000.17812. [DOI] [PubMed] [Google Scholar]
- 26.Borkholder CD, Hill VA, Fess EE. The efficacy of splinting for lateral epicondylitis: a systematic review. J Hand Ther. 2004;17(2):181–199. doi: 10.1197/j.jht.2004.02.007. [DOI] [PubMed] [Google Scholar]
- 27.Strujis PA, Kerkhoffs GM, Assendelft WJ, Dijk CN. Conservative treatment of lateral epicondylitis: brace versus physical therapy or a combination of both – a randomized clinical trial. Am J Sports Med. 2004;32(2):462–469. doi: 10.1177/0095399703258714. [DOI] [PubMed] [Google Scholar]
- 28.Strujis PA, Smidt N, Arola H, van Dijk CN, Buchbinder R, Assendelft WJ. Orthotic devices for tennis elbow: a systematic review. Br J Gen Pract. 2001;51(472):924–929. [PMC free article] [PubMed] [Google Scholar]
- 29.Strujis PA, Smidt N, Arola H, van Dijk CN, Buchbinder R, Assendelft WJ. Orthotic devices for tennis elbow. Cochrane Database Syst Rev. 2001;(2) doi: 10.1002/14651858.CD001821. [DOI] [PubMed] [Google Scholar]
- 30.Trinh KV, Phillips SD, Ho E, Damsma K. Acupuncture for the alleviation of lateral epicondyle pain: a systematic review. Rheumatology. 2004;43(9):1085–1090. doi: 10.1093/rheumatology/keh247. [DOI] [PubMed] [Google Scholar]
- 31.Fink M, Wolenstein E, Karst M, Gehrke A. Acupuncture in chronic lateral epicondylitis: a randomized controlled trial. Rheumatology. 2002;41(2):205–209. doi: 10.1093/rheumatology/41.2.205. [DOI] [PubMed] [Google Scholar]
- 32.Strujis PA, Damen PJ, Bakker EW, Blakenbvoort L, Assendelft WJ, van Dijk CN. Manipulation of the wrist for management of lateral epicondylitis: a randomized pilot study. Phys Ther. 2003;83(7):608–616. [PubMed] [Google Scholar]
- 33.Paungmali A, O'Leary S, Souvlis T, Vincenzino B. Hypoalgesic and sympathoexcitatory effects of mobilization with movement for lateral epicondylagia. Phys Ther. 2003;83(4):374–383. [PubMed] [Google Scholar]
- 34.Brosseau L, Casimiro L, Milne S, Robinson V, Shea B, Tugwell P, Wells G. Deep transverse friction massage for treating tendinitis. Cochrane Database Syst Rev. 2002;(4) doi: 10.1002/14651858.CD003528. [DOI] [PubMed] [Google Scholar]
- 35.Sevier TL, Wilson JK. Treating lateral epicondylitis. Sports Med. 1999;28(5):375–380. doi: 10.2165/00007256-199928050-00006. [DOI] [PubMed] [Google Scholar]
- 36.Sevier TL. Traditional physical therapy vs. graston technique augmented soft tissue mobilization in treatment of lateral epicondylitis. J Am College Sports Med. 1995;27(5) [Google Scholar]
- 37.Mooney V. Overuse syndromes of the upper extremity: rational and effective treatment. J Musculoskeletal Med. 1998;15(8):11–18. [Google Scholar]
- 38.Schiottz-Christensen B, Mooney V, Azxad S, Selstad D, Gulick J, Bracker M. The role of active release manual therapy for upper extremity overuse syndromes – a preliminary report. J Occup Rehab. 1999;9(3):201–211. [Google Scholar]
- 39.Hay EM, Paterson SM, Lewis M, Hosie G, Croft P. Pragmatic randomized controlled trial of local corticosteroid injection and naproxen for treatment of lateral epicondylitis of elbow in primary care. BMJ. 1999;319:964–968. doi: 10.1136/bmj.319.7215.964. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Newcomer KL, Laskowski ER, Idank DM, McLean TJ, Egan KS. Corticosteroid injection in early treatment of lateral epicondylitis. Clin J Sport Med. 2001;11(4):214–222. doi: 10.1097/00042752-200110000-00002. [DOI] [PubMed] [Google Scholar]
- 41.Bowen RE, Dorey FJ, Shapiro MS. Efficacy of nonoperative treatment for lateral epicondylitis. Am J Orthop. 2001;30(8):642–646. [PubMed] [Google Scholar]
- 42.Smidt N, Assendelft WJ, van der Windt DA, Hay EM, Buchbinder R, Bouter LM. Corticosteroid injections for lateral epicondylitis: a systematic review. Pain. 2002;96(1–2):23–40. doi: 10.1016/s0304-3959(01)00388-8. [DOI] [PubMed] [Google Scholar]
- 43.Wang CJ, Chen HS. Shock wave therapy for patients with lateral epicondylitis of the elbow: a one to two year follow up study. Am J Sports Med. 2002;3093:422–425. doi: 10.1177/03635465020300031901. [DOI] [PubMed] [Google Scholar]
- 44.Chung B, Wiley JP. Effectiveness of extracorporeal shock wave therapy in the treatment of previously untreated lateral epicondylitis: a randomized controlled trial. Am J Sports Med. 2004;32(7):1660–1667. doi: 10.1177/0363546503262806. [DOI] [PubMed] [Google Scholar]
- 45.Rompe JD, Decking J, Schoellner C, Theis C. Repetitive low-energy shock wave treatment for chronic lateral epicondylitis in tennis players. Am J Sports Med. 2004;32(3):734–743. doi: 10.1177/0363546503261697. [DOI] [PubMed] [Google Scholar]
- 46.Trinh K. Extracorporeal shock wave therapy for lateral epicondylitis. Clin J Sport Med. 2004;14(2):105–106. doi: 10.1097/00042752-200403000-00013. [DOI] [PubMed] [Google Scholar]
- 47.Somogyi D. Extracorporeal shock wave therapy for lateral epicondylitis. Clin J Sport Med. 2003;13(5):325–326. doi: 10.1097/00042752-200309000-00011. [DOI] [PubMed] [Google Scholar]
- 48.Haake M, Konig IR, Decker T, Reidel C, Buch M, Muller HH. Extracorporeal shock wave therapy in the treatment of lateral epicondylitis: a randomized multicenter trial. J Bone Joint Surg Am. 2002;84A(11):1982–1991. doi: 10.2106/00004623-200211000-00012. [DOI] [PubMed] [Google Scholar]
- 49.Speed CA, Nichols D, Richards C, Humphreys H, Wies JT, Burnet S, Hazleman BL. Extracorporeal shock wave therapy for lateral epicondylitis – a double blind randomized controlled study. J Orthop Res. 2002;20(5):895–898. doi: 10.1016/S0736-0266(02)00013-X. [DOI] [PubMed] [Google Scholar]
- 50.Ko JY, Chen HS, Chen LM. Treatment of lateral epicondylitis of the elbow with shock waves. Clin Orthop. 2001;(387):60–7. doi: 10.1097/00003086-200106000-00008. [DOI] [PubMed] [Google Scholar]
- 51.Svernlov B, Adolfsson L. Non-operative treatment regime including eccentric training for lateral humeral epicondylagia. Scand J Med Sci Sports. 2001;11(6):328–334. doi: 10.1034/j.1600-0838.2001.110603.x. [DOI] [PubMed] [Google Scholar]
- 52.Kaleli T, Ozturk C, Temiz A, Tirelioglu O. Surgical treatment of tennis elbow: percutaneous release of the common extensor origin. Acta Orthop Belg. 2004;70(2):131–133. [PubMed] [Google Scholar]
- 53.Verharr J. Lateral extensor release for tennis elbow. J Bone Joint Surg Am. 1993;75:1034–1043. doi: 10.2106/00004623-199307000-00010. [DOI] [PubMed] [Google Scholar]
- 54.Rosenberg N, Henderson I. Surgical treatment of resistant lateral epicondylitis. Follow-up study of 19 patients after excision, release and repair of proximal common extensor tendon origin. Arch Orthop Trauma Surg. 2002;122(9–10):514–517. doi: 10.1007/s00402-002-0421-8. [DOI] [PubMed] [Google Scholar]
- 55.Buchbinder R, Green S, Bell S, Barnsley L, Smidt N, Assendelft WJ. Surgery for lateral elbow pain. Cochrane Database Syst Rev. 2002;(1) doi: 10.1002/14651858.CD003525. [DOI] [PubMed] [Google Scholar]
- 56.Vincenzino B. Lateral epicondylagia: a musculoskeletal physiotherapy perspective. Man Ther. 2003;8(2):66–79. doi: 10.1016/s1356-689x(02)00157-1. [DOI] [PubMed] [Google Scholar]