Abstract
BACKGROUND
Although practice protocols exist for SMT and functional rehabilitation, no practice protocols exist for structural rehabilitation. Traditional chiropractic practice guidelines have been limited to acute and chronic pain treatment, with limited inclusion of functional and exclusion of structural rehabilitation procedures.
OBJECTIVE
(1) To derive an evidence-based practice protocol for structural rehabilitation from publications on Clinical Biomechanics of Posture (CBP®) methods, and (2) to compare the evidence for Diversified, SMT, and CBP®.
METHODS
Clinical control trials utilizing CBP® methods and spinal manipulative therapy (SMT) were obtained from searches in Mantis, CINAHL, and Index Medicus. Using data from SMT review articles, evidence for Diversified Technique (as taught in chiropractic colleges), SMT, and CBP® were rated and compared.
RESULTS
From the evidence from Clinical Control Trials on SMT and CBP®, there is very little evidence support for Diversified (our rating = 18), as taught in chiropractic colleges, for the treatment of pain subjects, while CBP® (our rating = 46) and SMT for neck pain (rating = 58) and low back pain (our rating = 202) have evidence-based support.
CONCLUSIONS
While CBP® Technique has approximately as much evidence-based support as SMT for neck pain, CBP® has more evidence to support its methods than the Diversified technique taught in chiropractic colleges, but not as much as SMT for low back pain. The evolution of chiropractic specialization has occurred, and doctors providing structural-based chiropractic care require protocol guidelines for patient quality assurance and standardization. A structural rehabilitation protocol was developed based on evidence from CBP® publications.
Keywords: chiropractic, spinal manipulation, rehabilitation
Abstract
ANTÉCÉDENTS
Quoi qu’il y ait des protocoles d’exercice établis pour la manipulation vertébrale et la réadaptation fonctionnelle, il n’existe aucun protocole pour la réadaptation structurale. Les directives d’exercices chiropratiques traditionnels se limitent à des traitements pour la douleur aigue et chronique avec une inclusion limitée des procédures de réadaptation fonctionnelle et une exclusion des procédures de réadaptation stucturale.
OBJECTIF
(1) Faire dévier des publications sur les procédures biomécaniques cliniques de la posture (BCP) un protocole d’exercice, avec preuve à l’appui, pour la réadaptation structurale, et (2) Comparer la preuve pour la techniques diversifiée, la manipulation vertébrale et la procédure biomécanique de la posture (BCP).
PROCÉDURES
Des essais de contrôle clinique avec l’utilisation des procédures biomécaniques cliniques et la manipulation vertébrale ont été obtenus, suite à des recherches dans Mantis, CINAHL et Index Medicus. En utilisant, les données des rapports de synthèse sur la manipulation vertébrale pour la technique diversifiée (tel qu’enseigné dans les collèges de chiropractie), la manipulation vertébrale et les procédures BCP ont été évaluées et comparées.
RÉSULTATS
Fondés sur la preuve des essais de contrôle clinique sur la manipulation vertébrale et les procédures BCP, il existe peu de preuve pour soutenir la technique diversifiée (notre taux = 18), tel qu’enseigné dans les collèges de chiropractie, pour le traitement de la douleur des sujets, contrairement aux procédures BCP (notre taux = 46) et la manipulation vertébrale pour la cervicalgie (taux = 58) et le lumbago (notre taux = 202) qui sont soutenues par la preuve.
CONCLUSION
Tandis que la procédure BCP possède approximativement, autant de preuve à l’appui que la manipulation vertébrale pour la cervicalgie, la méthode BCP possède davantage de preuves à l’appui, pour soutenir ses procédures que la méthode diversifiée, enseignée dans les collèges de chiropractie, mais pas autant que la manipulation vertébrale pour le lumbago. L’évolution de la spécialisation de la chiropractie est devenue une réalité et les médecins qui fournissent des soins de chiropractie, à base structurale, nécessitent des directives de protocole pour offrir aux patients une assurance de la qualité des soins et une normalisation. Un protocole de réadaptation structurale a été élaboré, fondé sur la preuve des publications, reliées aux procédures BCP.
Introduction
Recently, the buzzwords “evidence-based,” “evidence-based medicine” (EBM), and “evidence-based practice” (EBP) have appeared in clinical practice protocols. EBP is defined as clinical decision-making based on (1), sound external research evidence combined with individual clinical expertise and (2), the needs of the individual patient.1,2 EBP protocols have recently been written for several conditions.2–9
The goal of EBP is to improve patient outcomes, quality of care, and provide some standardization of treatment. Systematic reviews of available published evidence are required. The value of these literature reviews, however, depends on the quality of the review (selection bias by those doing the review) and the quality of the publications.10 To have “evidence” on aspects of all treatment methods is nearly impossible in any healthcare discipline, including medicine11 and chiropractic.12
The highest form of “evidence” would seem to be reliability studies, validity studies, and randomized clinical control trials (RCTs). Critics of a certain healthcare method often condemn that method if RCTs have not been published. This might seem unreasonable as there may be more agreement amongst researchers for other types of evidence. There are other types of clinical (non-randomized clinical trial, cohort, case report, etc.) and basic scientific studies that can provide “evidence” that a certain type or method of care might be reasonable, sufficient, or standard. In fact, the RCT may not be the best source of evidence for the clinical practice of chiropractic.1,13,14
The exact question being debated is “what does and what does not provide evidence in EBM.15–17 In 2001, Bolton1 discussed the reliance on RCTs in EBP protocols. Although the first few published RCTs on spinal manipulative therapy (SMT) were important for the chiropractic profession, RCTs are so narrow in methodology as to not often be useful in clinical chiropractic practice.1,14 Although the RCT is unarguably the best research design, “randomization and controlled conditions play no part in everyday clinical practice”1 and thus, evidence for effectiveness in that arena cannot be collected by RCTs. The strengths and limitations of the RCT have been discussed elsewhere.18
Given the limitations of the RCT in evaluating chiropractic treatment,14 it has been stated that it does not make sense to exclusively pursue the RCT in the future.13 Other research designs such as qualitative and outcomes research are now being recognized as very meaningful ways of providing the evidence in EBP.1 Additionally, it is known today that well-done case studies most often demonstrate findings consistent with that of the RCT.19,20
Since 1975, the chiropractic profession has enjoyed improved political support in a number of countries due to some published analyses favorable to chiropractic care.21–25 Unfortunately, because early evidence (RCTs) for manipulation had been on the effectiveness for treating acute and chronic pain complaints (i.e. LBP), the ensuing guidelines have primarily been based on acute/ chronic pain care. Consequently, in North America, chiropractic’s inclusion in government health insurance and private insurance programs has coincided with restrictions in frequency and duration of the care permitted. In response, some chiropractic organizations have written their own guidelines in an attempt to obtain fairness in these systems.26–28
Chiropractic treatment protocols could ideally be categorized into either: (a) Acute pain care, (b) Chronic pain care, (c) Functional rehabilitation care, or (d) Structural rehabilitation care. Recently, the profession has shown renewed interest in structural rehabilitative care. In a survey of 108 participating North American practices, Hawk et al.29 (their Table 10, page 167) reported Clinical Biomechanics of Posture (CBP®) technique to be the 7th most utilized technique in chiropractic practices. Problematically, there is only one manuscript detailing proposed guidelines for structural rehabilitation of the spine; this was based on a few preliminary studies.30
Our objectives are two-fold: (1) Compare the evidence for Diversified, General Spinal Manipulative Therapy (SMT), and CBP® for reduction in neck and low back pain intensity; (2) Derive an evidence-based practice protocol for structural rehabilitation from publications on Clinical Biomechanics of Posture (CBP®) methods. We will use some of Bolton’s1 ideas of evidence for EBP guidelines when discussing recent published research concerning CBP® structural rehabilitation procedures. To insure communication with the reader, a table of definitions is presented31–35 (Table 1).
Table 1.
Definitions of terms used in this manuscript
| Term | Operational Definition |
|---|---|
| Functional Rehabilitation | Rehabilitation with a purpose of treating/preventing deconditioning syndrome and abnormal illness behaviors via: relaxing/stretching overactive/tight muscles, mobilizing/adjusting stiff joints, facilitating/strengthening weak muscles, re-educating movement patterns (Liebenson, 1996).31 |
| Structural Rehabilitation | Rehabilitation with a purpose to normalize both posture and spine alignment primarily via mirror image exercises, mirror image adjusting, mirror image/extension traction. |
| Weak Muscle | Muscles that result in loss of movement if that muscle cannot contract sufficiently to move a body part through its partial or complete range of motion (Kendall et al. 1993).32 |
| Shortened Muscle | Muscles with a degree of shortness that results in slight to moderate loss of range of motion (Kendall et al. 1993).32 |
| SMT (Spinal Manipulative Therapy) | Spinal Manipulative Therapy defined as application of high-velocity, low-amplitude manual thrusts to the spinal joints slightly beyond the passive range of joint motion (Haldeman & Phillips, 1991).33 |
| Diversified Technique | Specific Spinal Manipulation Technique with the following steps:
|
| Acute pain | Pain less than 6 weeks duration. |
| Subacute pain* | Pain of 6 weeks to 3 months duration. |
| Chronic Pain* | Pain of greater than 3 months or of multiple occurrences (Carr, 2004).34 |
| MMI (Maximum Medical Improvement) | Term often used interchangeably with Maximum Chiropractic Improvement (MCI) or Maximum Therapeutic Benefit (MTB) indicating that further recovery and restoration of function can no longer be anticipated to a reasonable degree of medical/therapeutic certainty (Bryans, 2000).35 |
Bronfort et al.36 defined chronic pain as greater than 6 weeks and did not use the subacute category.
Methods
In order to compare the evidence for Diversified, SMT, and CBP®, literature searches were conducted in Mantis, CINAHL, and Index Medicus for Clinical Control Trials on SMT, Diversified, and CBP® methods.
We identified 73 RCTs on SMT, including only two clinical control trials on Diversified technique (as defined in Table 1), and 6 non-randomized clinical control trials on CBP® technique methods. In 2004, Bronfort et al.36 had identified 69 of the RCTs on SMT and performed a meta-analysis. This manuscript will adapt the Bronfort et al.36 analysis of the 69 RCTs identified before February 2003, and apply this analysis to two additional RCTs located since February 2003.37–38 Additionally, there have been two other review articles discussing SMT.39–40
In these RCT papers’ methods, we were looking for (1) any pain scales, (2) any disability scores, (3) the number of subjects, (4) whether SMT was actually used or only PT Mobilization, (5) if Diversified technique was used (as defined in Table 1), and (6) if DCs, MDs, or PTs performed the treatment, and (7) the number of treatments (visits).
Bronfort et al.36 deleted RCTs with 10 subjects or less, while in this manuscript, we deleted any RCTs if (1) there were 11 subjects or less (there were 3 such RCTs) and (2) if instead of SMT, authors utilized Physical Therapist’s mobilization (MOB) techniques. Table 2 provides our adapted analysis from Bronfort et al.,36 who categorized RCTs into acute pain, chronic pain, and mixed pain in each of the neck and low back regions, and our number of RCTs excluded and included for analysis. In 2004, two additional RCTs were published.70–71 While Hurwitz et al.’s 2004 study71 is a re-look at previous 2002 data,59 the 2004 Haas et al. study70 had less than 10 subjects in the treatment groups. We compared pain scale data in the 29 remaining RCTs41–69 and the two RCTs published since February 200337–38 to the CBP® published clinical control trials.72–77
Table 2.
RCT studies using SMT as the treatment
| Health conditioned studied in RCT | RCTs identified by Bronfort36 | Number excluded by Bronfort36 | Number excluded if MOB & not SMT utilized | Number excluded for ≤ 11 patients | Number used as evidence in this manuscript |
|---|---|---|---|---|---|
| Acute LBP | 15 | 9 | 1 | 0 | 540–44 |
| Chronic LBP | 15 | 4 | 4 | 1 | 645–50 |
| Mix LBP | 16 | 2 | 0 | 2 | 1251–62 |
| Acute NP | 5 | 3 | 1 | 0 | 163 |
| Chronic NP | 7 | 2 | 2 | 0 | 364–66 |
| Mix NP | 11 | 6 | 2 | 0 | 367–69 |
MOB = Physical Therapy Mobilization without SMT cavitation.
Acute = Pain for a duration of less than 6 weeks.
Chronic = Pain greater than 6 weeks duration, as defined by Bronfort et al.36
LBP = Low Back Pain.
NP = Neck Pain.
RCT = Randomized Clinical Control Trial.
SMT = Spinal Manipulative Therapy.
Table 3 provides the authors’ rating scale for Clinical Control Trials used in this manuscript. This rating scale is based on four parameters including: indexing data base of manuscript publication, type of clinical trial (RCT vs. non-RCT), the number of subjects, and use of pain scales, at minimum, either a numerical rating scale (NRS) or visual analogue scale (VAS). Outcome tools construction is rather a difficult procedure and, although simple and intuitively obvious, our new rating tool (Table 3) has not been tested.
Table 3.
Rating scale for clinical control trials used in this manuscript
| Rating* for Index where published | |||
|---|---|---|---|
| Controlled Trial | Mantis | CINAHL | Index Medicus |
| RCT with greater than 29 patients | 6 | 8 | 10 |
| RCT with less than 30 patients | 4 | 6 | 8 |
| Non-RCT with greater than 29 patients | 4 | 6 | 8 |
| Non-RCT with less than 30 patients | 3 | 5 | 7 |
If the RCT methods do not provide pain scales, which negates analysis of pain improvement, then 2 additional points are subtracted from the ratings above.
In order to derive an evidence-based practice protocol for structural rehabilitation from publications on Clinical Biomechanics of Posture (CBP®) methods, data from the six identified clinical trials on CBP® technique were extrapolated to estimate durations of care necessary to correct varying postural displacements. The extrapolations are reasonable as the CBP® controlled trial data is not linear (i.e. multiple pairs of data points, xi,yi, that make a line when plotted), but are average improvements for 36 treatments in a sample of more than 30 subjects, over a long time period (36 treatments over 3 months), and is exactly the kind of average data that can be extrapolated to another time period.
Results
Overall, there is a considerable amount of evidence supporting the use of SMT for low back (our rating = 202) and neck pain (our rating = 58), as well as support for CBP® technique for pain (our rating = 46). Surprisingly, there is little data existing on Diversified technique (as defined in Table 1) for either low back (our rating = 18) or neck pain (our rating = 0). Tables 4–6 summarize this data.
Table 4.
Rating and analysis of 25 RCTs for low back pain using general SMT and Diversified
| Low Back Pain RCT | # Treated patients | # visits | Pain score VAS/NRS pre/post | Treatment DC, MD, DO, PT? | Diversified used? | General SMT used? | Rating |
|---|---|---|---|---|---|---|---|
| *Glover et al, 197441 | 43 | 1 | NR | PT | no | yes | 8 |
| *Godfrey et al, 198442 | 22, 22 | 1 | NR | MD/DC | no | yes | 6 |
| Hadler et al, 198743 | 26 | 1 | NR | MD | no | yes | 6 |
| *MacDonald et al, 199044 | 49 | 5 | NR | DO | no | yes | 8 |
| Mathews et al, 198745 | 165 | <10 | NR | PT | no | yes | 8 |
| *Bronfort et al, 199646 | 71, 51 | 10 | 5.4 / 3.7 | DC | yes | no | 10 |
| Burton et al, 200047 | 20 | 6–18 | NR | DO | no | yes | 6 |
| *Coxhead et al, 198148 | 8G of 16 | 5–10 | NR | PT | no | yes | 6 |
| Herzog et al, 199149 | 16 | 10 | 3.2 / 1.8** | DC | no | yes | 8 |
| Pope et al, 199450 | 69 | 9 | Improved 2.4 | DC | no | yes | 10 |
| Triano et al, 199551 | 47 | 12 | 3.8 / 1.3 | DC | no | yes | 10 |
| *Anderson et al, 199952 | 83 | 12 | 4.9 / 3.2 | DO | no | yes | 10 |
| Cherkin et al, 199853 | 133 | 6.9 | 5.5 / 2.0 | DC | no | yes | 10 |
| Doran et al, 197554 | 116 | 6 | NR | MD | no | yes | 8 |
| Evans et al, 197855 | 15, 17 | 9 | NR | MD | no | yes | 6 |
| Giles et al, 199956 | 23 | 6 | 5.0 / 2.5 | DC | NR | NR | 8 |
| Hoehler et al, 198157 | 56 | 2–8 | NR | MD | no | yes | 8 |
| Hsieh et al, 200258 | 49 | 9 | NR | DC | yes | no | 8 |
| *Hurwitz et al, 200259 | 171 | NR | 4.7 / 2.5** | DC | NR | yes | 10 |
| Meade et al, 199060 | 384 | 9 | NR | DC | NR | ? | 8 |
| Postacchini et al, 198861 | 87 | 16–22 | NR | DC | no | yes | 8 |
| Skargren et al, 199762 | 138 | 7 | NR | DC | NR | NR | 8 |
| *Wreje et al, 199263 | 18 | 1 | 4.0 / 4.0 | MD | no | yes | 8 |
| Williams et al, 200337 | 72 | 3 | NR | DO | no | yes | 8 |
| Licciardone et al, 200338 | 91 | 7 | NR | DO | no | yes | 8 |
| Totals (Pain & Rating) | Mean 4.6/2.6 | 202 |
Methods include additional treatments besides just SMT.
Interpreted from graphs.
NR = Not Reported.
Table 6.
| CBP® Clinical Control Trials | # Treated patients | # visits | Chronic Pain: NRS Pre/post | Treatment by DC, MD, DO, PT? | Diversified Technique Used? | General SMT used? | Rating |
|---|---|---|---|---|---|---|---|
| Harrison et al, 199472 | 35 | 60 | NR | DC | no | yes | 6 |
| Harrison et al, 200273 | 30 | 35 | 4.3 / 1.6 | DC | no | yes, 0–3 wk | 8 |
| Harrison et al, 200274 | 30 | 38 | 4.1 / 1.1 | DC | no | yes, 0–3 wk | 8 |
| Harrison et al, 200375 | 48 | 38 | 4.4 / 0.6 | DC | no | yes, 0–3 wk | 8 |
| Harrison et al, 200476 | 51 | 37 | 4.0 / 0.7 | DC | no | no | 8 |
| Harrison et al, 200477 | 63 | 36 | 3.0 / 0.8 | DC | no | yes, sporadic | 8 |
| Totals (Pain & Rating) | Mean 4.0/1.0 | 46 |
NRS = Numerical Rating Scale for pain (0 = no pain, 1, 2, ..., 8, 9, 10 = severe disabling pain).
Diversified = a specific conglomeration of SMT maneuvers that requires specific listing, patient position, doctor position, and thrust opposite the listing (see definition Appendix 1).
NR = Not Reported.
0–3 wk = SMT given only in first 3 weeks of care out of 12 weeks of care.
sporadic = only a few subjects received an SMT, in only 0–3 weeks of care.
Using reported VAS (divided by 10) or NRS scores in Tables 4–6, an average pain reduction can be computed for the clinical control trials for low back pain using SMT techniques, neck pain SMT techniques, and CBP® methods. This comparison shows that the average reported numerical rating of initial (I) and follow-up (F) pain for Neck SMT studies is I/F = 4.8 / 2.5, the average for Low Back SMT studies is 4.6 / 2.6, while the average for CBP® studies is 4.0 /1.0. Thus, while the average pain reduction (NRS) in SMT studies is approximately 48%, the average for CBP® studies is 75%.
Using only the papers that reported numerical pain data in Tables 4–6, ending clinical pain can be assessed. Simple pain outcome data (i.e. NRS, VAS) comparing pre-to-post treatment results indicate that, although partial reductions in pain levels are achieved for SMT trials, post-treatment pain levels are reported to be at significant clinical levels, e.g., an average of ending NRS = 2.6 in Table 4 and ending NRS = 2.5 in Table 5. The same pain data comparison found for the CBP® clinical trials indicate minimal-to-negligible pain levels in the post-treatment groups (average ending NRS = 1.0 in Table 6).
Table 5.
Rating and analysis of seven SMT RCTs for neck pain
| Neck Pain RCT | # Treated patients | # visits | Pain: VAS/NRS Pre/post | Treatment by DC, MD, DO, PT? | Diversified Used? | General SMT used? | Rating |
|---|---|---|---|---|---|---|---|
| *Howe et al, 198364 | 26 | 1–3 | NR | MD | no | yes | 6 |
| *Bronfort et al, 200165 | 64 | 24 | 5.7 / 3.7 | DC | no | yes | 8 |
| Jordan et al, 199866 | 33 | 12 | 4.3 / 2.0 | DC | NR | NR | 10 |
| *Sloop et al, 198267 | 21 | 1 | Improved 1.8 | MD | no | yes | 6 |
| Giles et al, 199956 | 23 | 6 | 4.5 / 1.5 | DC | no | yes | 8 |
| Hurwitz et al, 200268 | 171 | 1 | 4.8 / 2.6 | DC | no | yes | 10 |
| Skargren et al, 199769 | 41 | 7 | 4.6 / 2.5 | DC | no | yes | 10 |
| Totals (Pain & Rating) | Mean 4.8/2.5 | 58 |
Methods include additional treatments besides just SMT.
NR = Not Reported.
A similar analysis to numerical pain using disability scores (not shown) from the RCTs in Tables 4 and 5 indicates that treatment subjects, on average, have significant disability at follow-up in these SMT studies (using those papers which report disability with NDI, SF-36, Roland-Morris, and/or Oswestry). For example, the reader is referred to the recent study by Leboeuf-Yde.78
Extrapolated CBP® clinical trial average data (Table 7) could be easily interpreted to estimate hypothetical treatment durations based on the magnitude of postural deviations (millimeters/degrees) as starting points in patient care (see Table 8).
Table 7.
| CBP®Study | Traction Minutes | Number of Visits | Number Months | Initial ARA | Post ARA | Average Improvement |
|---|---|---|---|---|---|---|
| Sagittal Cervical: | ||||||
| Compression-Extension72 | 10 | 60 | 3.0 | −14.5° | −27.7° | 13.2° |
| 2-way73 | 20 | 35 | 3.0 | −12.4° | −26.6° | 14.2° |
| Combined 2-way & Comp-Extension74 | 20 | 38 | 3.4 | −4.2° | −22.1° | 17.9° |
| Sagittal Lumbar: | ||||||
| APM&R 200275 | 20 | 38 | 3.0 | −22.4° | −33.7° | 11.3° |
| AP Cervical: | ||||||
| Lateral Translation76 | 20 | 37 | 3.0 | 13.7 mm | 6.8 mm | 6.9 mm |
| AP Lumbar: | ||||||
| Lateral Translation77 | 20 | 36 | 3.0 | 15 mm | 7.3 mm | 7.7 mm |
Note: The only CBP® non-randomized clinical control trial to not have pain data is Ref #72.
Table 8.
| CBP®Study | Example Initial ARAs or Tx | Normal ARA150,153or Tx150 | Expected Average Improvement in 3 months | Number of 3 Months Programs needed | Number of Visits Suggested |
|---|---|---|---|---|---|
| Cervical: | |||||
| JMPT 199472 | −27.7° | −43° | 13.2° | 1 | 60 |
| Comp-Ext | −14.5° | −43° | 13.2° | 2 | 120 |
| −1° | −43° | 13.2° | 3 | 180 | |
| APM&R 200273 | −26.6° | −43° | 14.2° | 1 | 35 |
| 2-way | −12.4° | −43° | 14.2° | 2 | 70 |
| +2° | −43° | 14.2° | 3 | 105 | |
| JMPT 200274 | −22.1° | −43° | 17.9° | 1 | 38 |
| Combined 2-way | −4.2° | −43° | 17.9° | 2 | 76 |
| & Comp-Ext | +14° | −43° | 17.9° | 3 | 114 |
| JRRD 200376 | 7 mm | 0 | 6.9 mm | 1 | 37 |
| Lateral Translation | 14 mm | 0 | 6.9 mm | 2 | 74 |
| 21 mm | 0 | 6.9 mm | 3 | 111 | |
| Lumbar: | |||||
| APM&R 200275 | −33° | −40° | 11.3° | 1 | 38 |
| Extension | −22.4° | −40° | 11.3° | 2 | 76 |
| −11.1° | −40° | 11.3° | 3 | 114 | |
| Eur Spine J 200377 | 7 mm | 0 | 7.7 mm | 1 | 36 |
| Lateral Translation | 15 mm | 0 | 7.7 mm | 2 | 72 |
| 22 mm | 0 | 7.7 mm | 3 | 108 |
ARA = absolute rotation angle.
Tx = translation on the x-axis.
Discussion
From the analysis presented on RCTs with the treatment of SMT in Tables 4–6, there is considerable evidence for the treatment of general spinal manipulation to be utilized for neck pain (our rating = 58) and back pain (our rating = 202). However, there is very little evidence for Diversified Technique, as defined in Table 1 (rating = 18). Thus, there is more evidence for CBP methods (our rating = 46) than for the Diversified technique (rating = 18), which is the technique method mandated by the Council on Chiropractic Education (CCE-USA and CCE-Canada) to be taught in all Chiropractic College curricula in the USA and Canada.
According to our review of studies on SMT and reduction in chronic pain intensity, it is readily apparent that the average neck pain subject is left with a NRS/VAS = 2.5 and the average for low back pain subject is left with a NRS/VAS = 2.6 (review Table 5). We note, the definition of a 2 = Constant Minimal to Intermittent Slight Pain and a 3 = Constant Slight Pain with some handicap. In contrast, the same pain data comparison found for the CBP® clinical trials indicate an ending value of NRS/ VAS = 1 = Minimal Pain or annoyance (Table 6). Therefore, it is obvious that while short-term usage of SMT reduces chronic pain intensity, it does not relieve it and in fact these subjects would not be described as MMI. The recent studies by Haas et al.71 and Leboeuf-Yde et al.78 are good examples of this. Thus, practice protocols based on pain in SMT studies are incomplete. Also, such practice protocols must include more visits than 12 because treated subjects, in published RCTs, were left in chronic pain (NRS = 2.6) after up to 12 treatments of SMT.
In a pilot RCT with a small number of subjects (n = 8 in each group), Haas et al.71 found that an increased number of treatments, up to 12, was associated with greater improvement of headache pain. However, even in the 12 treatment group, the headache pain was still less than 50% improved.71 Likewise, in a recent large multi-center trial, after 4 treatments of SMT for lower back pain, Leboeuf-Yde et al. found that subjects were left with a NRS of 2.6 (12 month follow up data). Leboeuf-Yde et al.78 also reported that these subjects still had significant levels of disability on the Oswestry scale (35-Moderate Disability down to 22.2-Moderate Disability).
Recent publications have found that health related quality of life and functional disability measures (Short Form-36, Oswestry, Neck Disability questionnaires, etc. ...) are more sensitive and important than simple pain intensity outcomes.79 It is of interest that recent publications have found strong correlations between altered sagittal spinal alignment (specifically loss of the distal lumbar lordosis), health quality of life, and physical function as measured with the Short Form-36 questionnaire.80 Therefore, we recommend that clinicians utilize health status and disability questionnaires at all initial and follow-up examinations. In this manner, strong evidence can be used to support the need and outcome effects of CBP® treatment methods (or any other chiropractic care) past the 8–12 visit “bench mark” of traditional SMT based studies.
Thus, CBP® multi-modal methods can be utilized to achieve health and disability improvements. But improvements in structural alignment are the primary intervention goal. Before deriving a protocol for structural rehabilitation from CBP® publications, a brief review is given for an appreciation of the clinical relevance of structural rehabilitation of the spine and posture.
Clinical relevance for structural rehabilitation
It is known that spinal function is directly related to spinal structure, as has been proven for the cervical and lumbar spinal regions.80–84 With mal-alignment in neutral posture, static and especially dynamic function from this mal-alignment dictates altered stress/strain relationships of associated spinal structures, including the bones,85–87 intervertebral discs,88–91 facet joints,92 musculotendinous tissues,93 ligamentous tissues,94 and neural elements.95–100
Postural alterations are known to be associated with a plethora of human afflictions from general pain syndromes,101–109 to problems with specific joints such as the hip110–111 and the knee,112 to problems with specific spinal regions such as the flat-back syndrome,113 and cervical kyphosis,109 to local organ ailments such as uterine prolapse,114–115 gastric herniation,116 and respiratory function,117–119 to thinking,118,120 and even to morbidity and mortality.121–125 Improved posture alignment has been one of the most sought-after goals in the treatment of human ailments for ages; this continues today in all medical arenas, such as dentistry, physiotherapy, physiatry, surgery, and chiropractic.126–134
Since traditional SMT has not been found to be associated with routine improvement in spinal alignment, its therapeutic effects are thought to be in reducing pain and facilitating increased spinal motion.135 Of interest, however, many monotherapies, have been found to have either limited effectiveness or complete lack of success in treating chronic low back pain. Bogduk136 has discussed that these monotherapies include analgesics, NSAIDs, muscle relaxants, antidepressants, physiotherapy, surgery, and manipulative therapy. In contrast, Gross et al.137 have reported that the multi-modal care of exercise combined with cervical manipulation provides better results than either procedure used alone. The criticism of monotherapies is taken into consideration by CBP® technique as it uses a multi-modality care regimen of SMT as well as mirror image® exercises, mirror image® adjusting and mirror image®/extension spinal traction procedures, other stretching procedures, and ergonomic counseling.
Limitations
Limitations of using data from RCTs on SMT and CBP® Clinical Control Trials in this review study are the same as those expressed by Bronfort et al.36 The interested reader is referred to page 350 of their study.
Goals in structural rehabilitation
If we categorize chiropractic treatment into: (a) acute pain care, (b) chronic pain care, (c) functional rehabilitation care, and (d) structural rehabilitation care, the goals of care in structural rehabilitation may encompass the first two (acute and chronic pain care). Considering the relationship between spinal function and structure,80–84 it is probable that functional rehab and structural rehab are attempts to treat the same patient dysfunction; albeit with different approaches.
For example, a patient presenting with acute or chronic neck pain with 50 mm of anterior head translation, initially would be treated with a trial of traditional SMT including any ancillary procedures (heat, ice, massage, stretching, etc. ...) for about 2–4 weeks to attempt to improve pain levels and spinal motion. Following this, functional rehabilitation would seek to improve strength in weakened muscles and flexibility in shortened or tightened muscles; muscle dysfunction is considered to be the cause of the displacement.32 In the case of anterior head translation it has been found that the neck flexors have decreased endurance and maximal isometric contraction strength.138
In contrast, structural rehabilitation procedures would seek to improve the postural abnormality by exercising the head in the exact opposite displacement (i.e., posterior head translation). Posterior head translation causes contraction of the upper neck flexors and stretches the upper neck extensors.139 Therefore, it is apparent the two approaches (functional vs. structural) are attempting to treat the same disorder by different means.
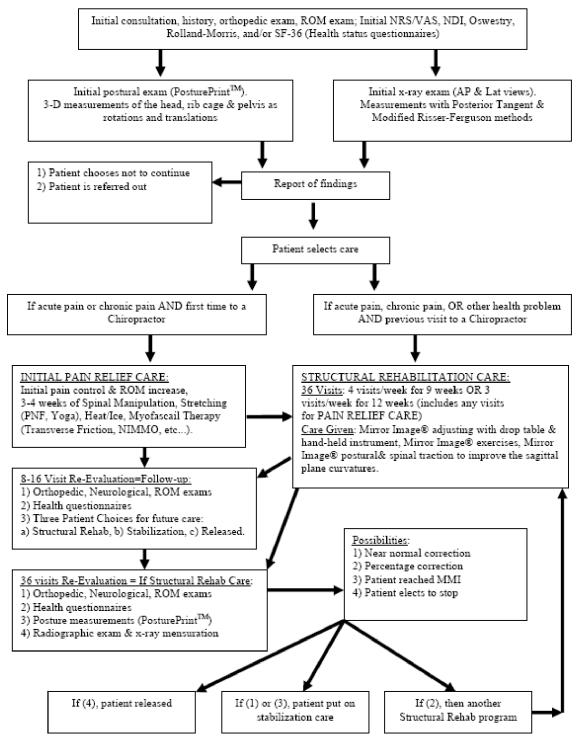
Figure 1 provides an algorithm that outlines the protocols, procedures, and time frames for a structural rehabilitation program of chiropractic care. This structural rehabilitation algorithm will be first supported and then detailed in the duration of the manuscript. The uniqueness of structural rehabilitation is the goal of normalizing both posture and spine alignment to evidence based values. This goal requires (1) a precise definition of normal posture; (2) reliability and validity of postural measurement; (3) a precise definition (model) of the normal spine; and (4) reliability and validity of spinal measurements.
Figure 1.
Algorithm for Structural Rehabilitation
Overview of CBP® Procedures
1) Radiographic Procedures
Radiographic line drawing analysis has been shown to be one of the most reliable tools in clinical practice.134 The Harrison posterior tangent method for measurement of sagittal spinal curves and the modified Riser-Ferguson method for measurement of frontal plane spinal displacements have both been studied for reliability. These two methods have been found to have good to excellent inter and intra-examiner reliability with small mean absolute values of observer differences for both angles and distances.140–143
The validity of radiographic analysis is supported by knowledge of posture and coupling, termed main motion (posture) and coupled motion (spinal segmental movements) in the literature.144–148 The radiographic spinal alignment (spinal coupling) can be compared to the initial posture of the patient (main motion) to determine if the coupling patterns are the same as published movements in the literature. This is valid, however, only if the clinician utilizes the same radiographic positioning methods as that used in the published studies;149 in fact, the CBP® standardized x-ray positioning procedures have been studied for their repeatability. Harrison et al.149 presented data on pre-post lateral and AP spinal x-rays ascertained in six different control groups and compared their results to twenty other manuscripts in the literature. Their149 results were similar to previous investigators, namely that x-ray positioning is highly repeatable even when taken by different examiners.
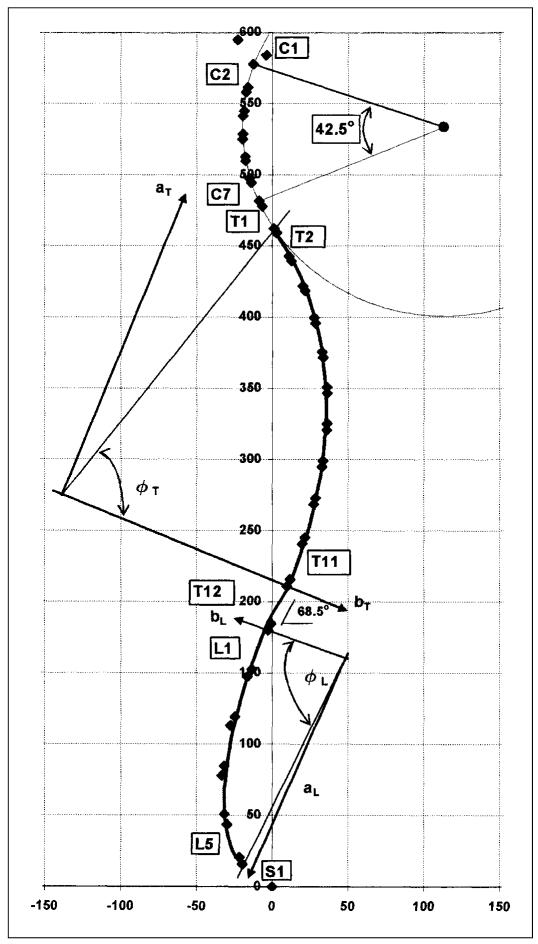
2) Ideal and Average Spinal Model
To determine abnormality of radiographic spinal alignment, the radiographic measurements are compared to a published normal spinal model that provides ideal and average alignment values (Figure 2). This normal spinal model is based, in part, on average values from normal subjects and has been published in orthopedic and chiropractic journals.150–156 Normal values have been published for each sagittal vertebral segmental angle (RRA = relative rotation angle, e.g., T8–T9) and for sagittal regional global angles (ARA = absolute rotation angle, e.g., C2–C7, T3–T10, and L1–L5). This model is “evidence-based.” In fact, the CBP® sagittal lumbar model153 and the sagittal cervical model156 were found to have discriminative validity in as much as they can distinguish between normal subjects, acute pain subjects, and chronic pain subjects.153,156
Figure 2.
The CBP® Full-spine Normal Model is the path of the posterior longitudinal ligament through the posterior body margins. It is composed of separate ellipses in the different spinal regions (cervicals, thoracics, & lumbars). It has near perfect sagittal balance of vertical alignment of C1-T1-T12-S1. This model provides normal sagittal plane curves and normal values for all segmental angles and global angles. The sagittal curves have points of inflection (mathematic term for change in direction from concavity to convexity) at inferior of T1 and inferior of T12. Reprinted with permission from Harrison DE et al. Spinal Biomechanics for Clinicians. Vol. I. Evanston, WY: Harrison CBP® Seminars, Inc., 2003.
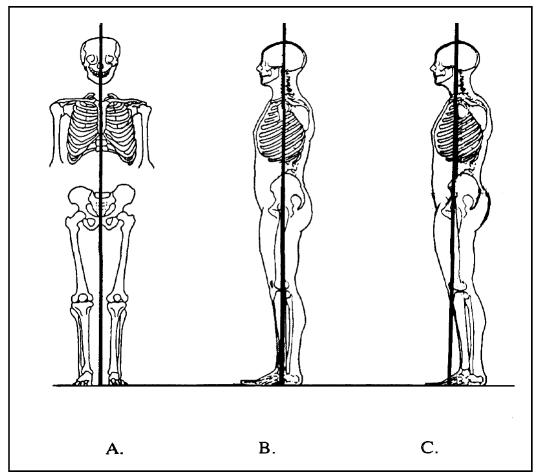
Further validity for an optimum upright spinal position comes from an analysis of loads and stresses based on minimum energy expenditure.89,121,157–159 Also, statistical analyses have derived an average normal spine.160,161 A biomechanical analysis of spinal loads dictates a vertical spine in the antero-posterior view (see AP view in Figure 3A), while more work must be done to derive a normal postural position in the sagittal view. Both ideal and average sagittal human postural alignments have been discussed.134,160–163 Figures 3B and 3C illustrate the ideal and average sagittal postures, respectively. The average sagittal posture in Figure 3C has a forward head posture and poor sagittal balance of C1, T1, T12, and S1; recent publications negate this position as normal due to increased muscle and disc loads, and tissue stresses.89,109,121,128,158,163,164
Figure 3.
In A, normal AP postural alignment is depicted. In B and C, ideal sagittal and average sagittal alignment are illustrated, respectively. Since the average human sagittal alignment (C) has forward head posture and poor C1, T1, T12, and S1 sagittal balance, it is not considered normal. Adapted with permission from Harrison DE et al. Spinal Biomechanics for Clinicians. Vol. I. Evanston, WY: Harrison CBP® Seminars, Inc., 2003.
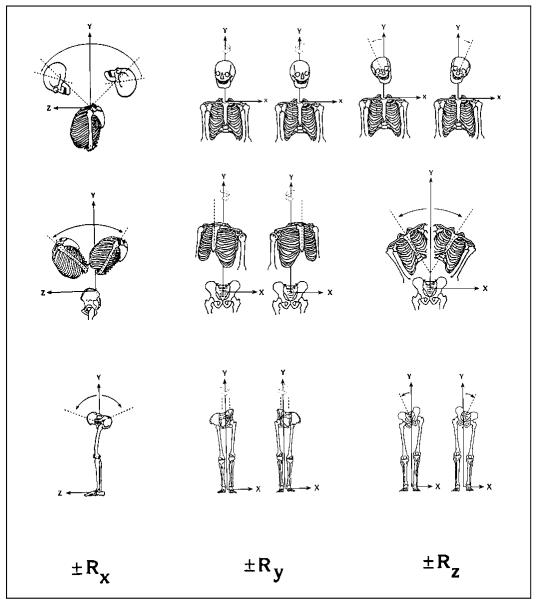
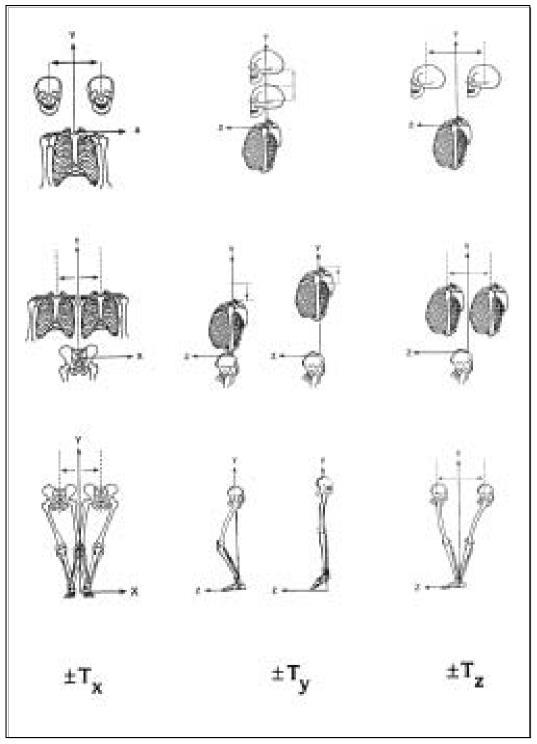
With normal posture precisely described (Figures 3A and B), abnormal posture can be determined. Using biomechanical concepts, abnormal posture has been described as rotations and translations of the head, rib cage, and pelvis from normal position in a 3-dimensional coordinate system (Figures 4 and 5).165,166 The last item necessary to complete the goals of structural rehabilitation protocols is the measurement of standing human posture. There are several computerized systems offered by various companies (e.g., Biotonix, PosturePro, ChiroVision) that use digital images of a patient to analyze their posture. Only one, however, can determine abnormal posture as numerical data of rotations (in degrees) and translations (in millimeters) for each displacement of the head, thorax, and pelvis (Biotonix’s new module: Posture-PrintTM).167–168
Figure 4.
Abnormal Postural Rotations. Rotations of the head relative to the thorax; thorax relative to the pelvis; and pelvis relative to the feet are depicted from the top to bottom rows, respectively. Regional rotations about the x, y, and z-axes are depicted from the left to right columns, respectively. Reprinted with permission from Harrison DE et al. Spinal Biomechanics for Clinicians. Vol. I. Evanston, WY: Harrison CBP® Seminars, Inc., 2003.
Figure 5.
Abnormal Postural Translations. Translations of the head relative to the thorax; thorax relative to the pelvis; and pelvis relative to the feet are depicted from the top to bottom rows, respectively. Regional translations along the x, y, and z-axes are depicted from the left to right columns, respectively. Reprinted with permission from Harrison DE et al. Spinal Biomechanics for Clinicians. Vol. I. Evanston, WY: Harrison CBP® Seminars, Inc., 2003.
As with measures of pain intensity, range of motion, and quality of life, periodic assessment of structural alignment is important to evaluate progress and determine when maximum medical improvement has been reached (Figure 1). Posture analysis via digital photography is non-invasive. While use of multiple follow-up radiographs are deemed necessary for use in surgical treatment by orthopedic surgeons,169 some chiropractors have condemned the use of post-radiographs to collect alignment data.170–175 Importantly, these condemnations170–175 can be considered expert opinion evidence only, without supporting data. In contrast, there is data to show that the use of medical x-rays constitutes a very minor health risk.176–185 In fact, Cohen (University of Pittsburg) has written extensively on the over-exaggeration of exposure from medical x-rays.171,181–184 The following section will review the relative health risks of spinal radiography.
Health Risks of Radiography in Structural Rehabilitation
In structural rehabilitation care, it is necessary that the Doctor obtain initial and follow-up posture and radiographic measurements. The frequency suggested for radiography is an initial examination, with follow-up measurements at 36 visit intervals, which could be 4 visits per week for 9 weeks or 3 visits per week for 12 weeks.186–187 Data from CBP’s® 6 clinical control trials72–77 indicate that the average chronic pain patient needs 6 months of intensive care to achieve a near normal spinal and postural alignment. This would mean, on average, one initial set of x-rays and single plane follow-up x-rays depending on the part of the spine being treated.
The structural rehabilitation algorithm for x-ray imaging frequency is minimal, compared to that of orthopedic surgeons, who often take initial pre-operative, immediate post-operative, one month, 6–12 months, and long-term follow-up radiographs (total of 5 sets of x-rays) for surgery cases.169 In fact, according to Fischgrund (2005, pp 1017 and 1023), “Routine cervical spine radiographs taken for the evaluation of degenerative disc disease and cervical radiculopathy include lateral, anteroposterior, and oblique views.”169 “Typical follow-up of these patients includes an office visit at 1 week, with routine anteroposterior and lateral radiographs. By 6 weeks, lateral flexion and extension views usually show that the fusion construct is stable ...”.169 Fischgrund further stated that follow-ups are ascertained at 1 year, 2 years, or 5 or more years depending upon the specific study. Therefore, according to Fischgrund, surgery patients receive initial, 1-week post op, 6-week post op, and 1, 2, or 5 year follow ups.169
As orthopedists use radiographs to evaluate and monitor structural spinal changes, so too do doctors utilizing CBP® structural rehabilitation protocols.
From Maurer:178 “Authorities agree that while no radiation dose level is risk-free, the level used in diagnostic radiology provides low-dose risk and is considered as acceptable to the average individual.” The 1949 National Council on Radiation Protection and Measurements (NCRP) defines permissible dose as: “the dose of ionizing radiation that, in light of present knowledge, is not expected to cause appreciable bodily injury to a person at any time during his lifetime.” Since this NCRP statement, the trend in science has been away from the “permissible or acceptable” dose concept to the current “risk” concept. In either approach, the end result is similar: “for the information gained with diagnostic radiology, the radiation risk is minimal.”
To educate the reader to the minimal risks of medical x-rays, some equivalent risks are provided from the literature. Medical x-rays are of very minimal health risk compared to the risks associated with environmental factors such as air travel (in Table 9, exposure equivalent relates to life expectancy). From Butler,179 for example, one can calculate the routine exposure of airplane passengers and crew; based on 0.60 mSv (0.6 x 0.1 rem) per 100 block hours (the mean for a flight between New York City and Athens, Greece), a pilot flying 700 block hours per year would receive an annual occupational exposure of 4.2 mSv (0.42 rem). In contrast, a pilot flying 700 block hours on a Chicago-to-San Francisco route (0.41 mSv/100 block hours) would receive an annual dose of approximately 2.8 mSv (0.28 rem).
Table 9.
Relative Risks of Different Environmental Exposures176,178,179,184 (These values relate to equivalence of reduced life expectancy)
| Environmental Item | Exposure Equivalent | Exposure Equivalent |
|---|---|---|
| Pilot Flying: New York City-Athens | 4200 microSv/yr | 420 mrem/yr |
| Pilot Flying: Chicago-San Francisco | 2800 microSv/yr | 280 mrem/yr |
| Chest x-ray | 100 microSv | 10 mrem |
| Extremity x-ray | 10 microSv | 1 mrem |
| Dental x-ray | 100 microSv | 10 mrem |
| Head/neck x-ray | 200 microSv | 20 mrem |
| Cervical Spine x-ray | 220 microSv | 22 mrem |
| Lumbar spinal x-rays | 1300 microSv | 130 mrem |
| Smoking a Cigarette | 70 microSv | 7 mrem |
| Fat Person Eating Pie-a-la-mode | 350 microSv | 35 mrem |
This Chicago-San Francisco dose is 0.28 rem/yr = 280 mrem/yr = 5.4 mrem/wk. For comparison, according to Cohen and Lee,176 “smoking a cigarette has the risk equivalent of 7 mrem of radiation, and an overweight person eating a pie a-la-mode runs a risk equal to that of 35 mrem.” Equating absorbed dose and dose equivalent, 1 rem = 0.01 J/kg = 1 rad, Table 9 provides the minimal dose equivalent for medical x-rays. However, it is noted that current high-frequency machines and use of filtration systems (i.e. Nolan filters) allow human exposures to be reduced very significantly (50%) as compared to earlier equipment.188
It now becomes obvious why Federal Governments and airplane companies do not tell pilots to stop flying after one year. By simply reducing rich desserts, cigarettes, or soft-drinks, a pilot can cancel out his equivalent radiation risks! The government website states that a flight from LA to NY and back is approximately worth one chest x-ray due to being in the upper atmosphere. Thus, pilots who fly two round trips from LA to NY per week, get the dose equivalent of two chest x-rays per week or about 100 per year! After 10 years, for example, an airline pilot could accumulate an equivalent of 1,000 chest x-rays!
Cohen and Lee176 and Cohen184 provided a look at radiation risk levels, along with other examples of risks associated with various activities and how they translate into equivalence in loss of life expectancy. It provides the likely results of both general patterns of behavior and one-time occurrences. According to their study, the drinking of one diet soft drink per day reduces life expectancy by two days; ingesting 100 calories per day by drinking regular soft drinks increases body weight by 7 pounds and reduces life expectancy by 210 days. If you are 30 percent overweight you lose 1,300 days; 20 percent overweight 900 days; unmarried males lose 3,500 days; smokers lose 2,250 days.176 These studies and many others point out that risks are associated with nearly all activities of daily living.
While DACBRs’ (chiropractic radiologists) opinions, with minimal supporting data, condemned the use of initial and post-radiographs to collect alignment measurements,170–175 data actually exists that indicates medical x-ray exposure may have a health benefit.191 However, minimal risk is inherent in everything we do as part of the human experience. While we must constantly work towards the reduction of health risks in all endeavors, we may be led to accept a minimal level as normal. While there is no data indicating diagnostic radiology has a present risk, any radiation dose must be compared to the benefits of useful information gained. The necessity for appropriate treatment selection is indeed an acceptable trade-off when put into perspective. The need for x-ray imaging is especially clear when one considers that radiographic imaging is the only valid method for attaining spinal alignment values; whereas surface contour methods (e.g., flexible ruler) are invalid and unreliable.192–196
Radiation Hormesis
Radiation hormesis is the stimulatory or beneficial effect of low doses of ionizing radiation. While an actual benefit from radiation exposure may seem outrageous, there is much scientific evidence for this phenomenon. This topic is in direct conflict with the “Linear No-Threshold Hypothesis” (LNT), which has been assumed to be true for more than 50 years. This LNT model comes from estimating the risks at lower doses of radiation, in the absence of data, by extrapolating in a linear model from large doses of radiation from atomic bombs dropped on Japan in the 1940s.
This LNT model has been used to set limits of radiation exposure by all official and governmental associations.185 Recently in 2003, Kauffman180 reiterated that authors critical of exposure from diagnostic radiation always use the LNT model. This use of the LNT model includes the recent 2005 report by the USA National Research Council.197 This report stated, “there will be some risk, even at low doses (100 mSv or less), although the risk is small” and “there is no direct evidence of increased risk of non-cancer diseases at low doses.”197 This 2005 report ignored and contradicted an earlier 2003 review by Kant et al.198
For a comparison of exposures, USA citizens are exposed to an average annual natural background radiation level of 3 mSv, while exposure from a chest x-ray is approximately 0.1 mSv and exposure from a whole body computerized tomography (CT) scan is approximately 10 mSv.197 Also it is noted that 10mSv = 1,000mrem, which equates to about 46 cervical series or 8 lumbar series (see Table 9).
The LNT model has been questioned for its application to low levels of exposure by many researchers.183,189,199–202 Actually, below a certain level of exposure, there are beneficial health effects, (termed radiation hormesis), which do not follow from extrapolation of the high-dose portion of the curve.182,189–191,203–217
Structural Rehabilitation Protocols
While other methods may provide evidence for structural rehabilitation, we discuss only recent research outcomes in CBP® Technique. CBP® is unique in chiropractic, in that it utilizes a “mirror image®” concept applied to human posture; this basic tenet has a sound foundation in Linear Algebra, an area of study common to both engineering and mathematics.218 CBP® multi-modal care consists of three primary procedures: mirror image® exercises, mirror image® adjustments, and mirror image®/ extension traction. These mirror image® posture positions are the rotation and translation pairs in or about each coordinate axis (Figures 4 and 5).
The reason for postural mirror image® exercises, adjustments, and traction procedures is to address all the tissues involved in spine and posture alignment. Although strength and conditioning exercise has not proven to correct posture,219 mirror image® exercises have shown initial promise in the reduction of posture and spinal displacements.220–224 These exercises are performed to stretch shortened muscles and to strengthen those muscles that have weakened in areas where postural muscles have adapted to asymmetric or ill-positioned postures.
Postural adjustments as performed with drop table, hand-held instrument, or even mirror image® manipulation procedures, are performed for resetting the nervous system regulation of postural muscle balance.225,226 Postural mirror image® extension traction provides sustained loading periods of 10–20 minutes and is necessary to cause visco-elastic deformation to the resting length of the spinal muscles, ligaments, and discs.227
From 1994–2004, CBP® has completed seven case studies,228–234 and has completed six non-randomized clinical control trials.72–77 While case studies are ranked as the lowest level of clinical studies evidence on the traditional scientific evidence hierarchy, non-randomized control trials are the 2nd highest type of evidence; ranked second only to the RCT.1,14 Recalling that RCTs are inadequate for evaluating multi modal chiropractic care regimens,1 these seven CBP® case studies228–234 and six CBP® control trials72–77 provide a growing clinical evidence base to support the need for CBP® structural care programs of sufficient durations to provide as near normal as possible posture and spine structural rehabilitation/re-alignment. From CBP’s® six clinical control trials, 72–77 Table 7 presents the average total number of visits, frequency, duration of care, and the amount of spinal alignment improvement found for the cervical and lumbar lordoses and cervical/lumbar frontal plane alignments, respectively.
Table 8 presents actual and extrapolated data estimating durations of care necessary for correcting hypothetical sagittal plane displacements; we note that a negative sign means lordotic curvature and a positive sign indicates kyphotic curvature for measurements in the cervical and lumbar regions.140–142 Table 8 also gives average and extrapolated data estimating the duration of care necessary to reduce/correct a head and trunk list (side shift posture) in the AP cervico-thoracic and lumbar radiographs as measured appropriately (i.e. measured as a horizontal displacement of: 1) Mid-C2 dens compared to vertical line up from estimated center of mass (CM) of Thoracic #4 in an AP cervico-thoracic analysis;144 2) Estimated CM of T12 compared to a vertical line up from the S2 tubercle in an AP lumbar analysis.143,235
From Table 8 one can estimate structural care durations based on extrapolations from the CBP® clinical trials. It should be mentioned that these are merely averages; and are in fact extrapolations from the current clinical trial data. Therefore, individual patients may change in shorter or longer times; thus, follow-up radiological exams provide the clinician with valuable insight into individual patient response to treatment. The following provide examples of estimating average durations of care hypothetically necessary to restore a patient’s spine to ideal spinal alignment:
If a patient had a kyphotic cervical curve ARA (C2 to C7) measuring +12°, then 3 programs (treatment blocks of 38 sessions) of 2-way extension-compression traction would hypothetically correct the misalignment. That is, three increments of average improvement of −17.9°, results in an extrapolated average correction of 3x(−17.9) +12° = −41.7°, which approximates the ideal cervical lordosis of −43°.150
If a patient had a hypolordotic cervical ARA (C2 to C7) measuring −29°, then one program of 35 visits of CBP® 2-way traction would be expected to correct the misalignment: −29° + 1x(−14.2°) = −43.2° (ideal normal).150
If a patient had a hypolordotic lumbar curve ARA (L1 to L5) of −18°, then two programs of CBP® lumbar extension traction of 38 visits would hypothetically correct the misalignment. That is, two increments of average improvement of −11.3°, results in an extrapolated correction of 2x(−11.3°) + −18° = −40.6°, which approximates the average/ideal normal lumbar lordosis value of −40°153 (see Table 8).
Criticisms of CBP Methods
In the past, criticisms of CBP® methods and x-ray protocols have been based on the 1999 Commentary by Haas et al.170 These criticisms often neglect to provide the Harrison rebuttal written in 2000,134 which reported that Haas et al.170 misrepresented references, misinterpreted references, misquoted references, and performed a selective literature review.134 In fact, this Harrison-Haas debate was a series of three publications.134,170,236 Additionally, the uniformed often state that the extension position in CBP® cervical traction methods are dangerous.
Numerous articles from the literature lead to the conclusion that this is definitely not the case. In fact, in a 1999 thorough review of the literature on varying positions of the head associated with vertebral and basilar artery blood flow and dissection, Haldeman et al.237 concluded that “examination of the data fails to show a consistent position or movement of the neck that could be considered particularly dangerous.”
In addition, Thiel et al.238 found no occlusion of vertebral artery blood flow during various head and neck positioning tests on the patient, including head extension.
Inaccurate personal opinions about the dangers of extension come from “Beauty Parlor Stroke.” There has been anecdotal criticism of the hyper-extension head position at Beauty Parlors. Much of this criticism seems to be based on several letters to editors and case reports in the Index Medicus literature concerning “beauty parlor stroke.”239–243 The positions referred to were prolonged (1-hour or more) hyper-extension combined with axial rotation,239–243 although Endo et al.243 did not discuss any rotation of the head. In 1992 and 1993, Weintraub239–241 reported on seven cases of “Beauty Parlor Stroke” in which clients at beauty parlors had symptoms of nystagmus, ataxia, slurred speech, facial weakness, nausea, vomiting, vertigo, and dysarthria after having their hair shampooed. Six of these seven individuals were older than 75 years and one was 54-years-old. The 54-year-old subject had been left in a position of cervical hyper-extension over the edge of a shampoo bowl in excess of two hours. In 1995, Stratigos242 reported on the condition of his mother after a trip to a beauty parlor.
All four of these articles discussed in detail that the mechanism of vertebrobasilar injury is associated with cervical axial rotation while in hyper-extension. In 2000, Endo et al.243 reported a single case of a woman aged 62 who suffered a “beauty parlor stroke.” There was no mention of the duration of shampoo treatment or a detailed explanation of the position of the head.
Unlike beauty parlor employees, individuals employing CBP® spinal traction methods are trained physicians, who do screening examinations on patients for tolerance to head extension. Using our cervical traction protocol, patients are screened and then monitored while traction time periods are increased at only a few minutes per visit, starting at 3–5 minutes, over a period of many visits to a maximum of 20 minutes. These traction methods are also not used or modified for those of advanced age and do not involve axial rotation in the extended position. While any induced stroke symptoms would be unacceptable, these “beauty parlor strokes” should not be applied to CBP® cervical extension traction methods, when used by trained physicians.
Conclusions
Besides the RCT, other forms of scientific evidence, if existing, may be more than adequate to create goal-oriented clinical guidelines.1,13,14,244 CBP® studies provide the typical type of chiropractic care, as several procedures are provided to the patient on each visit. At present, there is evidence for SMT for neck and low back pain. From published research for the treatment of chronic neck and back pain at this time, CBP® Technique has more supporting evidence than Diversified Technique, as taught in all Chiropractic Colleges.
This paper has presented guidelines as a clinical tool for the practice of structural rehabilitation by CBP® technique methods. CBP® is unique, in that, unlike most chiropractic techniques,245 CBP® has laid a solid foundation of basic science research (spine modeling, x-ray line drawing reliability, x-ray positioning repeatability, posture reliability, biomechanical stress analysis), clinical research (case studies, clinical trials), and educational research (reviews, position papers).
Because traditional practice protocols in chiropractic have considered only acute and chronic pain conditions, limited inclusion of functional rehabilitation, and a total neglect of structural rehabilitation, there is a need to have published protocols for structural rehabilitation of the spine and posture. This manuscript has proposed structural protocol guidelines based on clinical evidence from a significant quantity and quality of CBP® technique publications. Tables 6–8 are based on CBP® mirror image® methods. The use of multiple clinical methodologies in these CBP® studies is consistent with Bolton’s ideas13 of clinical applications in EBP. Because of the focused literature herein, this guideline serves as a tool only for the doctor practicing structural rehabilitation utilizing CBP® mirror image® exercise, adjusting, and traction procedures.
Acknowledgement
The authors acknowledge the assistance of Dr. Dennis Mizel DC with this manuscript.
References
- 1.Bolton JE. The evidence in evidence-based practice: what counts and what doesn’t count? J Manipulative Physiol Ther. 2001;24:362–366. doi: 10.1067/mmt.2001.115259. [DOI] [PubMed] [Google Scholar]
- 2.Sackett DL, Richardson WS, Rosenberg W, Haynes RB. Evidence-based medicine: How to practice and teach EBM. New York: Churchill-Livingstone, 1997.
- 3.Lipman G. Evidence-based pain management and palliative care. J Pain Palliat Care Pharmacother. 2002;16:1–3. [PubMed] [Google Scholar]
- 4.Fishbain DA, Cutler RB, Rosomoff HL, Rosomoff RS. Can patients taking opioids drive safely? A structured evidence-based review. J Pain Palliat Care Pharmacother. 2002;16:9–28. [PubMed] [Google Scholar]
- 5.Caramanica L, Cousino JA, Peterson S. Four elements of a successful quality program. alignment, collaboration, evidence-based practice, and excellence. Nurs Adm Q. 2003;27:336–343. doi: 10.1097/00006216-200310000-00012. [DOI] [PubMed] [Google Scholar]
- 6.Jordan KM, Arden NK, Doherty M, et al. EULAR recommendations 2003: an evidenced based approach to the management of knee osteoarthritis: Report of a task force of the standing committee for the International Clinical Studies Including Therapeutic Trials. Ann Rheum Dis. 2003;62:1145–1155. doi: 10.1136/ard.2003.011742. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Wassem RA, Stillion-Allen KA. Evidence-based management of the fibromyalgia patient. In search of optimal functioning. Adv Nurs Prac. 2003;11:34–38. 41–43. [PubMed] [Google Scholar]
- 8.Hasenfeld R, Shekelle PG. Is the methodological quality of guidelines declining in the US? Comparison of the quality of US Agency for Health Care Policy and Research (AHCPR) guidelines with those published subsequently. Qual Saf Health Care. 2003;12:428–434. doi: 10.1136/qhc.12.6.428. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Sackett DL. Evidence-based medicine [editorial] Spine. 1998;23:1085–1086. doi: 10.1097/00007632-199805150-00001. [DOI] [PubMed] [Google Scholar]
- 10.Davidson KW, Goldstein M, Kaplan RM. Evidence-based behavioral medicine: What is it and how do we achieve it? Ann Behav Med. 2003;26:161–171. doi: 10.1207/S15324796ABM2603_01. [DOI] [PubMed] [Google Scholar]
- 11.Smith R.Where is the wisdom ...? The poverty of medical evidence Br Med J 1991303798–799.1932964 [Google Scholar]
- 12.Brouwers M, Charette M. Evaluation of clinical practice guidelines in chiropractic care: A comparison of North American guideline reports. J Can Chiropr Asso. 2001;45:141–153. [Google Scholar]
- 13.Bolton JE. Whence the evidence from evidence-based practice? Br J Chiropr. 2000;4:2–3. [Google Scholar]
- 14.Hawk C. Chiropractic clinic research: where are we looking for the key? J Neuromusculoskeletal System. 1999;7:150–155. [Google Scholar]
- 15.Miles A, Polychronis A, Grey J. Evidence-based medicine: Why all the fuss? This is why. J Eval Clin Pract. 1997;3:83–86. doi: 10.1046/j.1365-2753.1997.00103.x. [DOI] [PubMed] [Google Scholar]
- 16.Fahey T. Applying the results of clinical trials to patients in general practice: perceived problems, strengths, assumptions, and challenges for the future. Br J Gen Pract. 1998;1:1173–1178. [PMC free article] [PubMed] [Google Scholar]
- 17.McKee M, Britton A, Black N, et al. Interpreting the evidence: choosing between randomized and non-randomized studies. Br Med J. 1999;319:312–315. doi: 10.1136/bmj.319.7205.312. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Rosenfeld RM. Meaningful outcomes research. In: Isenberg SF, ed. Managed care, outcomes and quality. New York: Thieme, 1998:99–115.
- 19.Venning GR. Validity of anecdotal reports of suspected adverse drug reactions: The problem of false alarms. BMJ. 1982;284:249–252. doi: 10.1136/bmj.284.6311.249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Benson K, Hartz AJ. A comparison of observational studies and randomized controlled trials. N Engl J Med. 2000;342:1878–1886. doi: 10.1056/NEJM200006223422506. [DOI] [PubMed] [Google Scholar]
- 21.Chiropractic in New Zealand: report of the commission of inquiry. Wellington, NZ:P.D. Hasselberg, Government Printer, 1979.
- 22.Manga P, Angus D, Papadopoulos C, Swan W. The effectiveness and cost-effectiveness of chiropractic management of low back pain. Ottawa:Kenilworth Publishing, 1993.
- 23.Meade TW, Dyer S, Browne W, Frank AO. Randomized comparison of chiropractic and hospital outpatient management for low back pain: results from extended follow up. Br Med J. 1995;311:349–351. doi: 10.1136/bmj.311.7001.349. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Shekelle, P. G., Adams, A. H., Chassin, M. R., Hurwitz, E. L., Phillips, R. B., and Brook, R. H. The appropriateness of spinal manipulation for low back pain. Project overview and literature review. Santa Monica, CA, RAND, 1991.
- 25.Bigos S, Bowyer O, Braen G, et al. Acute low back pain problems in adults. Clinical practice guideline No. 14. AHCPR Publication No. 95–0642. Rockville, MD: Dept. of Health and Human Services (US), Agency for Health Care Policy and Research, Public Health Service:1994.
- 26.Michigan Chiropractic Society. Chiropractic Care and Utilization Review Guidelines. Lansing, MI:MCS, 1991.
- 27.Standards of Practice. Minnesota Chiropractic Association. MN:MCA, 1991.
- 28.Ohio State Chiropractic Association. The chiropractic manual for insurance claims personnel. Columbus, OH:OSCA, 1990.
- 29.Hawk C, Long CR, Boulanger KT. Prevalence of non-musculoskeletal complaints in chiropractic: report from a practice-based research program. J Manipulative Physiol Thera. 2001;24:157–169. [PubMed] [Google Scholar]
- 30.Troyanovich SJ, Harrison DE, Harrison DD. Structural rehabilitation of the spine and posture: Rationale for treatment beyond the resolution of symptoms. J Manipulative Physiol Ther. 1998;21:37–50. [PubMed] [Google Scholar]
- 31.Liebenson C. Rehabilitation of the spine: a practicioner’s manual. New York: Lippincott Williams & Wilkins, 1996.
- 32.Kendall FP, McCreary EK, Provance PG. Muscles Testing and Function. (4th ed.). Baltimore: Williams & Wilkins, 1993.
- 33.Haldeman S, Phillips RB. Spinal manipulative therapy in the management of low back pain. In: Frymoyer, J.W., Ducker, T.B., Hadler, N.M., Kostuik, J.P., Weinstein, J.N., Whitecloud, T.S. editors. The adult spine: principles and practice. New York: Raven Press, Ltd. 1991:1581–1605.
- 34.Carr DB, Goudas LC, Denman WT, Brookoff D, Staats PS, Brennen L, Green G, Albin R, Hamilton D, Rogers MC, Firestone L, Lavin PT, Mermelstein Safety and efficacy of intranasal ketamine for the treatment of breakthrough pain in patients with chronic pain: a randomized, double-blind, placebo-controlled, crossover study. Pain. 2004;108(1–2):17–27. doi: 10.1016/j.pain.2003.07.001. [DOI] [PubMed] [Google Scholar]
- 35.Bryans R. (editor). Whiplash: A practitioner’s guide to understanding Whiplash Associated Disorders (WAD). Canadian Chiropractic Association, 2000.
- 36.Bronfort G, Haas M, Evans R, Bouter LM. Efficacy of spinal manipulation and mobilization for low back pain and neck pain: a systematic review and best evidence synthesis. Spine J. 2004;4:335–356. doi: 10.1016/j.spinee.2003.06.002. [DOI] [PubMed] [Google Scholar]
- 37.Williams NH, Wilkinson C, Russell I, Edwards RT, Hibbs R, Linck P, et al. Randomized osteopathic manipulation study (ROMANS): pragmatic trial for spinal pain in primary care. Fam Pract. 2003;20:662–669. doi: 10.1093/fampra/cmg607. [DOI] [PubMed] [Google Scholar]
- 38.Licciardone JC, Stoll ST, Fulda KG, Russo DP, Siu J, Winn W, et al. Osteopathic manipulative treatment for chronic low back pain: a randomized controlled trial. Spine. 2003;28:1355–1362. doi: 10.1097/01.BRS.0000067110.61471.7D. [DOI] [PubMed] [Google Scholar]
- 39.Assendelft WJ, Morton SC, Yu EI, Suttorp MJ, Shekelle PG. Spinal manipulative therapy for low back pain. Cochrane database Syst Rev. 2004;(4):CD000447. doi: 10.1002/14651858.CD000447.pub2. [DOI] [PubMed] [Google Scholar]
- 40.Cherkin DC, Sherman KJ, Deyo RA, Shekelle PG. A review of the evidence for the effectiveness, safety, and cost of acupuncture, massage therapy, and spinal manipulation for low back pain. Ann Intern Med. 2003;138:898–906. doi: 10.7326/0003-4819-138-11-200306030-00011. [DOI] [PubMed] [Google Scholar]
- 41.Glover JR, Morris JG, Khosla T. Back pain: a controlled clinical trial of rotational manipulation of the trunk. Br J Industr Med. 1974;31:59–64. doi: 10.1136/oem.31.1.59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Godfrey CM, Morgan PP, Schatzker J. A randomized trial of manipulation for low-back pain in a medical setting. Spine. 1984;9:301–304. doi: 10.1097/00007632-198404000-00015. [DOI] [PubMed] [Google Scholar]
- 43.Hadler NM, Curtis P, Gillings DB, Stinnet S. A benefit of spinal manipulation as adjunctive therapy for acute low-back pain: a stratified controlled trial. Spine. 1987;12:703–706. [PubMed] [Google Scholar]
- 44.MacDonald RS, Bell CMJ. An open controlled assessment of osteopathic manipulation in nonspecific low-back pain. Spine. 1990;15:364–370. doi: 10.1097/00007632-199005000-00005. [DOI] [PubMed] [Google Scholar]
- 45.Mathews JA, Mills SB, Jenkins VM, et al. Back pain and sciatica: controlled trials of manipulation, traction, sclerosant and epidural injections. Br J Rheumatol. 1987;26:416–423. doi: 10.1093/rheumatology/26.6.416. [DOI] [PubMed] [Google Scholar]
- 46.Bronfort G, Goldsmith CH, Nelson CF, Boline PD, Anderson AV. Trunk exercise combined with spinal manipulation or NSAID therapy for chronic low back pain: a randomized, observer-blinded clinical trial. J Manipulative Physiol Ther. 1996;19:570–582. [PubMed] [Google Scholar]
- 47.Burton AK, Tillotson KM, Cleary J. Single-blind randomized controlled trial of chemonucleolysis and manipulation in the treatment of symptomatic lumbar disc herniation. Eur Spine J. 2000;9:202–207. doi: 10.1007/s005869900113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Coxhead CE, Inskip H, Meade TW, North WR, Troop JD. Multicentre trial of physiotherapy in the management of sciatic symptoms. Lancet. 1981;1:1065–1068. doi: 10.1016/s0140-6736(81)92238-8. [DOI] [PubMed] [Google Scholar]
- 49.Herzog W, Conway PJ, Wilcox BJ. Effects of different treatment modalities on gait symmetry and clinical measures for sacroiliac joint patients. J Manipulative Physiol Ther. 1991;14:104–109. [PubMed] [Google Scholar]
- 50.Pope MH, Phillips RB, Haugh LD, Hsich CY, MacDonald L, Haldeman S. A prospective randomized three-week trial of spinal manipulation, transcutaneous muscle stimulation, massage and corset in the treatment of subacute low back pain. Spine. 1994;19:2571–2577. doi: 10.1097/00007632-199411001-00013. [DOI] [PubMed] [Google Scholar]
- 51.Triano JJ, McGregor M, Hondras MA, Brennen PC. Manipulative therapy versus education programs in chronic low back pain. Spine. 1995;20:948–955. doi: 10.1097/00007632-199504150-00013. [DOI] [PubMed] [Google Scholar]
- 52.Anderson GB, Lucente T, Davis AM, Kappler RE, Lipton JA, Leurgans S. A comparison of osteopathic spinal manipulation with standard care for patients with low back pain. N Engl J Med. 1999;341:1426–1431. doi: 10.1056/NEJM199911043411903. [DOI] [PubMed] [Google Scholar]
- 53.Cherkin DC, Deyo RA, Battie M, Street J, Barlow W. A comparison of physical therapy, chiropractic manipulation, and provision of an educational booklet for the treatment of patients with low back pain. N Engl J Med. 1998;339:1021–1029. doi: 10.1056/NEJM199810083391502. [DOI] [PubMed] [Google Scholar]
- 54.Doran DM, Newell DJ. Manipulation in treatment of low back pain: a multicentre study. BMJ. 1975;2:161–164. doi: 10.1136/bmj.2.5964.161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Evans DP, Burke MS, Lloyd KN, Roberts EE, Roberts GM. Lumbar spinal manipulation on trials. Part I: Clinical Assessment Rheumatol Rehabil. 1978;17:46–53. doi: 10.1093/rheumatology/17.1.46. [DOI] [PubMed] [Google Scholar]
- 56.Giles LGF, Muller R. Chronic spinal pain syndromes : a clinical pilot trial comparing acupuncture, a nonsteroidal anti-inflammatory drug, and spinal manipulation. J Manipulative Physiol Ther. 1999;22:376–381. doi: 10.1016/s0161-4754(99)70082-5. [DOI] [PubMed] [Google Scholar]
- 57.Hoehler FK, Tobis JS, Buerger AA. Spinal manipulation for low back pain. JAMA. 1981;245:1835–1838. [PubMed] [Google Scholar]
- 58.Hsieh CY, Adams AH, Tobis J, et al. Effectiveness of four conservative treatments for subacute low back pain: a randomized clinical trial. Spine. 2002;27:1142–1148. doi: 10.1097/00007632-200206010-00003. [DOI] [PubMed] [Google Scholar]
- 59.Hurwitz EL, Morgenstern H, Harper P, et al. A randomized trial of medical care with and without physical therapy and chiropractic care with and without physical modalities for patients with low back pain: 6-month follow-up outcomes from the UCLA low back pain study. Spine. 2002;27:2193–2204. doi: 10.1097/00007632-200210150-00002. [DOI] [PubMed] [Google Scholar]
- 60.Meade TW, Dyer S, Browne W, Townsend J, Frank AQ. Low back pain of mechanical origin: randomized comparison of chiropractic and hospital outpatient treatments. BMJ. 1990;300:1431–1437. doi: 10.1136/bmj.300.6737.1431. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Postacchini F, Facchini M, Palieri P. Efficacy of various forms of conservative treatment in low back pain. A comparative study. Neuro Orthop. 1988;6:28–35. [Google Scholar]
- 62.Skargren EI, Oberg BE, Carlsson PG, Gade M. Cost and effectiveness analysis of Chiropractic and physiotherapy treatment for low back and neck pain. Six-months follow-up. Spine. 1997;22:2167–2177. doi: 10.1097/00007632-199709150-00015. [DOI] [PubMed] [Google Scholar]
- 63.Wreje U, Nordgren B, Aberg H. Treatment of pelvic joint dysfunction in primary care- a controlled study. Scand J Prim Health Care. 1992;10:310–315. doi: 10.3109/02813439209014080. [DOI] [PubMed] [Google Scholar]
- 64.Howe DH, Newcombe RG, Wade MT. Manipulation of the cervical spine. A pilot study. J R Coll Gen Pract. 1983;33:574–579. [PMC free article] [PubMed] [Google Scholar]
- 65.Bronfort G, Evans R, Nelson B, Aker P, Goldsmith C, Vernon H. A randomized clinical trial of exercise and spinal manipulation for patients with chronic neck pain. Spine. 2001;26:788–799. doi: 10.1097/00007632-200104010-00020. [DOI] [PubMed] [Google Scholar]
- 66.Jordan A, Bendix T, Nielsen H, Hansen FR, Host D, Winkel A. Intensive training, physical therapy, or manipulation for patients with chronic neck pain. A prospective single-blinded randomized clinical trial. Spine. 1998;23:311–319. doi: 10.1097/00007632-199802010-00005. [DOI] [PubMed] [Google Scholar]
- 67.Sloop PR, Smith DS, Goldberg E, Dore C. Manipulation for chronic neck pain. A double-blinded controlled trial. Spine. 1982;7:532–535. doi: 10.1097/00007632-198211000-00003. [DOI] [PubMed] [Google Scholar]
- 68.Hurwitz EL, Morgenstern H, Harber P, Kominski GF, Yu F, Adams AH. A randomized trial of chiropractic manipulation and mobilization for patients with neck pain: clinical outcomes from the UCLA neck-pain study. Am J Public Health. 2002;92:1634–1641. doi: 10.2105/ajph.92.10.1634. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Skargren EI, Oberg BE, Carlsson PG, Gade M. Cost and effectiveness analysis of Chiropractic and physiotherapy treatment for low back and neck pain. Six-months follow-up. Spine. 1997;22:2167–2177. doi: 10.1097/00007632-199709150-00015. [DOI] [PubMed] [Google Scholar]
- 70.Hurwitz EL, Morgenstern H, Vassilaki M, Chiang LM. Adverse reactions to chiropractic treatment and their effects on satisfaction and clinical outcomes among patients enrolled in the UCLA Neck Pain Study. J Manipulative Physiol Ther. 2004;27:16–25. doi: 10.1016/j.jmpt.2003.11.002. [DOI] [PubMed] [Google Scholar]
- 71.Haas M, Groupp E, Aicki M, Fairweather A, Ganger B, Attwood M, Cummins C, Baffes L. Dose response for chiropractic care of chronic cervicogenic headache and asssociated neck pain: a randomized pilot study. J Manipulative Physiol Ther. 2004;27(9):547–553. doi: 10.1016/j.jmpt.2004.10.007. [DOI] [PubMed] [Google Scholar]
- 72.Harrison DD, Jackson BL, Troyanovich SJ, Robertson G, De George D, Barker WF. The efficacy of cervical extension-compression traction combined with diversified manipulation and drop table adjustments in the rehabilitation of cervical lordosis: a pilot study. J Manipulative Physiol Ther. 1994;17:454–464. [PubMed] [Google Scholar]
- 73.Harrison DE, Cailliet R, Harrison DD, Janik TJ, Holland B. A new 3-point bending traction method for restoring cervical lordosis and cervical manipulation: A nonrandomized clinical controlled trial. Arch Phys Med Rehab. 2002;83:447–453. doi: 10.1053/apmr.2002.30916. [DOI] [PubMed] [Google Scholar]
- 74.Harrison DE, Harrison DD, Betz J, Colloca CJ, Janik TJ, Holland B. Increasing the cervical lordosis with seated combined extension-compression and transverse load cervical traction with cervical manipulation: Nonrandomized clinical control trial. J Manipulative Physiol Ther. 2003;26:139–151. doi: 10.1016/S0161-4754(02)54106-3. [DOI] [PubMed] [Google Scholar]
- 75.Harrison DE, Cailliet R, Harrison DD, Janik TJ, Holland B. Changes in sagittal lumbar configurations with a new method of extension traction: Nonrandomized clinical controlled trial. Arch Phys Med Rehab. 2002;83:1585–1591. doi: 10.1053/apmr.2002.35485. [DOI] [PubMed] [Google Scholar]
- 76.Harrison DE, Cailliet R, Betz J, et al. Conservative methods for reducing lateral translation postures of the head: A non-randomized clinical control trial. J Rehab Res Dev. 2004;41(4):631–640. doi: 10.1682/jrrd.2003.05.0070. [DOI] [PubMed] [Google Scholar]
- 77.Harrison DE, Cailliet R, Betz JW, Harrison DD, Haas JW, Janik TJ, Holland B. A non-randomized clinical control trial of Harrison mirror image methods for correcting trunk list (lateral translations of the thoracic cage) in patients with chronic low back pain. Eur Spine J. 2005;14(2):155–162. doi: 10.1007/s00586-004-0796-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Leboeuf-Yde C, Gronstvedt A, Borge JA, Lothe J, Magnesen E, Nilsson O, Rosok G, Stig LC, Larsen K. The Nordic back pain subpopulation program: A 1-year prospective multicenter study of outcomes of persistent low-back pain in chiropractic patients. J Manipulative Physiol Ther. 2005;28(2):90–96. doi: 10.1016/j.jmpt.2005.01.010. [DOI] [PubMed] [Google Scholar]
- 79.Horng YS, Hwang YH, Wu HC, Liang HW, Jang Y, Twu FC, Wang JD. Predicting health-related quality of life in patients with low back pain. Spine. 2005;30:551–555. doi: 10.1097/01.brs.0000154623.20778.f0. [DOI] [PubMed] [Google Scholar]
- 80.Korovessis P, Dimas A, Lambiris E. The significance of correlation of radiographic variables and MOS short-form health survey for clinical decision in symptomatic low back pain patients. Stud Health Technol Inform. 2002;91:325–331. [PubMed] [Google Scholar]
- 81.Walmsley RP, Kimber P, Culham E. The effect of initial head position on active cervical axial rotation range of motion in two age populations. Spine. 1996;21:2435–2442. doi: 10.1097/00007632-199611010-00005. [DOI] [PubMed] [Google Scholar]
- 82.Takeshima T, Omokawa S, Takaoka T, Araki M, Ueda Y, Takakura Y. Sagittal alignment of cervical flexion and extension: Lateral radiographic analysis. Spine. 2002;27:E348–355. doi: 10.1097/00007632-200208010-00014. [DOI] [PubMed] [Google Scholar]
- 83.Hirose D, Ishida K, Nagano Y, Takahashi T, Yamamoto H. Posture of the trunk in the sagittal plane is associated with gait in community-dwelling elderly population. Clin Biomech. 2004;19(1):57–63. doi: 10.1016/j.clinbiomech.2003.08.005. [DOI] [PubMed] [Google Scholar]
- 84.Edmondston SJ, Henne SE, Loh W, Ostvoid E. Influence of cranio-cervical posture on three-dimensional motion of the cervical spine. Man Ther. 2005;10(1):44–51. doi: 10.1016/j.math.2004.07.004. [DOI] [PubMed] [Google Scholar]
- 85.Stokes I, Spence H, Aronsson D, Kilmer N. Mechanical modulation of vertebral body growth: implications for scoliosis progression. Spine. 1996;21:1162–1167. doi: 10.1097/00007632-199605150-00007. [DOI] [PubMed] [Google Scholar]
- 86.Bowman SM, Keaveny TM, Gibson LJ, Hayes WC, McMahon TA. Compressive creep behavior of bovine trabecular bone. J Biomechanics. 1994;27:301–310. doi: 10.1016/0021-9290(94)90006-x. [DOI] [PubMed] [Google Scholar]
- 87.Mente PL, Aronsson DD, Stokes IAF, Iatridis JC. Mechanical modulation of growth for the correction of vertebral wedge deformities. J Orthop Res. 1999;17:518–524. doi: 10.1002/jor.1100170409. [DOI] [PubMed] [Google Scholar]
- 88.Brickley-Parsons D, Glimcher MJ. Is the chemistry of collagen in intervertebral discs an expression of Wolff’s Law? A study of the human lumbar spine. Spine. 1983;9:148–163. doi: 10.1097/00007632-198403000-00005. [DOI] [PubMed] [Google Scholar]
- 89.Harrison DE, Colloca CJ, Harrison DD, Janik TJ, Haas JW, Keller TS. Anterior thoracic posture increases thoracolumbar disc loading. Eur Spine J. 2005;14(3):234–242. doi: 10.1007/s00586-004-0734-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Kaigle A, Ekstrom L, Holm S, Rostedt M, Hansson T. In vivo dynamic stiffness of the porcine lumbar spine exposed to cyclic loading: influence of load and degeneration. J Spinal Disord. 1998;11:65–70. [PubMed] [Google Scholar]
- 91.Lotz JC, Chin JR. Intervertebral disc cell death is dependant on the magnitude and duration of spinal loading. Spine. 2000;25:1477–1483. doi: 10.1097/00007632-200006150-00005. [DOI] [PubMed] [Google Scholar]
- 92.Frechede B, et al. Risk of injury of the human neck during impact: role of geometrical and mechanical parameters. Euro CSRS, Porto, Portugal, May 30–June 5 , Paper A29, 2004.
- 93.Mayoux-Benhamou MA, et al. Influence of head position on dorsal neck muscle efficiency. Electromyogr Clin Neurophysiol. 1993;33:161–166. [PubMed] [Google Scholar]
- 94.Kumaresan S, Yoganandan N, Pintar FA. Finite element analysis of the cervical spine: A material property sensitivity study. Clinical Biomechanics. 1999;14:41–53. doi: 10.1016/s0268-0033(98)00036-9. [DOI] [PubMed] [Google Scholar]
- 95.Smith CG. Changes in length and position of the segments of the spinal cord with changes in posture in the monkey. Radiology. 1956;66:259–265. doi: 10.1148/66.2.259. [DOI] [PubMed] [Google Scholar]
- 96.Reid JD. Effects of flexion-extension movements of the head and spine upon the spinal cord and nerve roots. J Neurol Neurosurg Psychiatry. 1960;23:214–221. doi: 10.1136/jnnp.23.3.214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Adams CBT, Logue V. Studies in cervical spondylotic myelopathy I: Movement of the cervical roots, dura and cord, and their relationship to the course of the extrathecal roots. Brain. 1971;94:557–568. doi: 10.1093/brain/94.3.557. [DOI] [PubMed] [Google Scholar]
- 98.Breig A. Pathological stress in the pons-cord tissue tract and its alleviation by neurosurgical means. In: Congress of Neurological Surgeons, ed. Clinical neurosurgery. Baltimore: Williams & Wilkins, 1973:87–94. [DOI] [PubMed]
- 99.Breig A, Marions O. Biomechanics of the lumbosacral nerve roots. Acta Radiologica Diagnosis. 1963;1:1141–1160. doi: 10.1177/028418516300100603. [DOI] [PubMed] [Google Scholar]
- 100.Breig A. Adverse mechanical tension in the central nervous system: An analysis of cause and effect: Relief by functional neurosurgery. Stockholm: Almqvist and Wiksell International, 1978.
- 101.Cailliet R. Low back pain syndrome. Philadelphia: F.A. Davis, 1981.
- 102.Harber P, Bloswick D, Beck J, Pena L, Baker D, Lee J. Supermarket checker motions and cumulative trauma risk. J Occup Med. 1993;35:805–811. doi: 10.1097/00043764-199308000-00018. [DOI] [PubMed] [Google Scholar]
- 103.Genaidy AM, Karwowski W. The effects of neural posture deviations on perceived joint discomfort ratings in sitting and standing postures. Ergonomics. 1993;36:785–792. doi: 10.1080/00140139308967942. [DOI] [PubMed] [Google Scholar]
- 104.Rys M, Konz S. Standing. Ergonomics. 1994;37:677–687. doi: 10.1080/00140139408963682. [DOI] [PubMed] [Google Scholar]
- 105.Powers C, Maffucci R, Hampton S. Rear foot posture in subjects with patello-femoral pain. J Orthop Sports Phys Ther. 1995;22:155–160. doi: 10.2519/jospt.1995.22.4.155. [DOI] [PubMed] [Google Scholar]
- 106.Eklund J, Odenrick P, Zettergren S, Johansson H. Head posture measurements among work vehicle drivers and implications for work and workplace design. Ergonomics. 1994;37:623–639. doi: 10.1080/00140139408963678. [DOI] [PubMed] [Google Scholar]
- 107.Watson A. Sports injuries in footballers related to defects of posture and body mechanics. J Sports Med Phys Fitness. 1995;35:289–294. [PubMed] [Google Scholar]
- 108.Beaman DN, Graziano GP, Glover RA, Wojtys EM, Chang V. Substance P innervation of lumbar spine facet joints. Spine. 1993;18:1044–1049. doi: 10.1097/00007632-199306150-00014. [DOI] [PubMed] [Google Scholar]
- 109.Ganju A, Ondra SL, Shaffrey CI. Cervical kyphosis. Techniques in Orthopaedics. 2003;17:345–354. [Google Scholar]
- 110.Davies JW. Man’s assumption of the erect posture: Its effect on the position of the pelvis. Am J Obstet Gynecol. 1955;70:1012–1020. doi: 10.1016/0002-9378(55)90008-9. [DOI] [PubMed] [Google Scholar]
- 111.Offierski CM, Macnab I. Hip-spine syndrome. Spine. 1983;8:316–321. doi: 10.1097/00007632-198304000-00014. [DOI] [PubMed] [Google Scholar]
- 112.Tsuji T, Matsuyama Y, Goto M, et al. Knee-spine syndrome: correlation between sacral inclination and patello-femoral joint pain. J Orthop Sci. 2002:519–523. doi: 10.1007/s007760200092. [DOI] [PubMed] [Google Scholar]
- 113.Lee CS, Lee CK, Kim YT, Hong YM, Yoo JH. Dynamic sagittal imbalance of the spine in degenerative flat back. significance of pelvic tilt in surgical treatment. Spine. 2001;26:2029–2035. doi: 10.1097/00007632-200109150-00017. [DOI] [PubMed] [Google Scholar]
- 114.Lind LR, Lucente V, Kohn N. Thoracic kyphosis and the prevalence of advanced uterine prolapse. Obstet Gynecol. 1996;87:605–609. doi: 10.1016/0029-7844(95)00477-7. [DOI] [PubMed] [Google Scholar]
- 115.Mattox TF, Lucente V, McIntyre P, Miklos JR, Tomezsko J. Abnormal spinal curvature and its relationship to pelvic organ prolapse. Am J Obstet Gynecol. 2000;183:1381–1384. doi: 10.1067/mob.2000.111489. [DOI] [PubMed] [Google Scholar]
- 116.Winans HM. Anemia in the aged (Syndrome of kyphosis, gastric hernia, and anemia) Texas J Med. 1938;34:422–423. [Google Scholar]
- 117.Hansson KG. Body mechanics in geriatrics. J Am Geriatrics Soc. 1954;2:429–433. doi: 10.1111/j.1532-5415.1954.tb02134.x. [DOI] [PubMed] [Google Scholar]
- 118.Lennon J, Shealy N, Cady RK, Matta W, Cox R, Simpson WF. Postural and respiratory modulation of autonomic function, pain, and health. Am J Pain Manag. 1994;4:36–39. [Google Scholar]
- 119.Weiss HR. The effect of an exercise program on vital capacity and rib mobility in patients with idiopathic scoliosis. Spine. 1991;16:88–93. doi: 10.1097/00007632-199101000-00016. [DOI] [PubMed] [Google Scholar]
- 120.Riskind J, Gotay C. Physical posture: Could it have regulatory of feedback effects on motivation and emotion? Motivation Emotion. 1982;6:273–298. [Google Scholar]
- 121.Keller TS, Harrison DE, Colloca CJ, Harrison DD, Janik TJ. Prediction of osteoporotic spinal deformity. Spine. 2003;28:455–462. doi: 10.1097/01.BRS.0000048651.92777.30. [DOI] [PubMed] [Google Scholar]
- 122.Freeman JT. Posture in the aging and aged body. JAMA. 1957;165:843–846. doi: 10.1001/jama.1957.72980250013020. [DOI] [PubMed] [Google Scholar]
- 123.Milne JS, Williamson J. A longitudinal study of kyphosis in older people. Age Ageing. 1983;12:225–233. doi: 10.1093/ageing/12.3.225. [DOI] [PubMed] [Google Scholar]
- 124.Cutler WB, Friedmann E, Genovese-Stone E. Prevalence of kyphosis in a healthy sample of pre- and postmenopausal women. Am J Phys Med Rehab. 1993;72:219–225. doi: 10.1097/00002060-199308000-00009. [DOI] [PubMed] [Google Scholar]
- 125.Anderson F, Cowan NR. Survival of healthy older people. Br J Prev Soc Med. 1976;30:231–232. doi: 10.1136/jech.30.4.231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Festa F, Tecco S, Dolci M, Ciufolo F, et al. Relationship between cervical lordosis and facial morphology in Caucasian women with a skeletal class II malocclusion: a cross-sectional study. Cranio. 2003;21:121–129. doi: 10.1080/08869634.2003.11746240. [DOI] [PubMed] [Google Scholar]
- 127.Garrett TR, Youdas JW, Madson TJ. Reliability of measuring forward head posture in a clinical setting. JOSPT. 1993;17:155–160. doi: 10.2519/jospt.1993.17.3.155. [DOI] [PubMed] [Google Scholar]
- 128.Hanten WP, Lucio RM, Russell JL, Brunt D. Assessment of total head excursion and resting head posture. Arch Phys Med Rehab. 1991;72:877–880. doi: 10.1016/0003-9993(91)90003-2. [DOI] [PubMed] [Google Scholar]
- 129.Carr EK, Kenney FD, Wilson-Barnett J, et al. Inter-rater reliability of postural observation after stroke. Clin Rehabil. 1999;13:229–242. doi: 10.1177/026921559901300307. [DOI] [PubMed] [Google Scholar]
- 130.Muto T, Takeda S, Kanazawa M, Yamazaki A, Fujiwara Y, Mizoguchi I. The effect of head posture on the pharyngeal airway space (PAS) Int J Oral Maxillofac Surg. 2002;31:579–583. doi: 10.1054/ijom.2002.0279. [DOI] [PubMed] [Google Scholar]
- 131.Taylor AR. The mechanism of injury to the spinal cord in the neck without damage to the vertebral column. J Bone Joint Surg. 1951;33B:543–547. doi: 10.1302/0301-620X.33B4.543. [DOI] [PubMed] [Google Scholar]
- 132.Lazennec J-Y, Ramare S, Arafati N, Laudet CG, et al. Sagittal alignment in lumbosacral fusion: relations between radiological parameters and pain. Euro Spine J. 2000;9:47–55. doi: 10.1007/s005860050008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133.Akumaru T, Kawahara N, Yoon T, Minamide A, et al. Adjacent segment motion after a simulated lumbar fusion in different sagittal alignments. Spine. 2003;28:1560–1566. [PubMed] [Google Scholar]
- 134.Harrison DE, Harrison DD, Troyanovich SJ, Harmon S. A normal spinal position: It’s time to accept the evidence. J Manipulative Physiol Ther. 2000;23:623–644. doi: 10.1067/mmt.2000.110941. [DOI] [PubMed] [Google Scholar]
- 135.Hurwitz EL, Aker PD, Adams AH, Meeker WC, Shekelle PG. Manipulation and mobilization of the cervical spine: a systematic review of the literature. Spine. 1996;21:1746–1759. doi: 10.1097/00007632-199608010-00007. [DOI] [PubMed] [Google Scholar]
- 136.Bogduk N. Management of chronic low back pain. Med J Aust. 2004;180:79–83. doi: 10.5694/j.1326-5377.2004.tb05805.x. [DOI] [PubMed] [Google Scholar]
- 137.Gross AR, Kay TM, Kennedy C, et al. Clinical practice guideline on the use of manipulation or mobilization in the treatment of adults with mechanical neck disorders. Man Ther. 2002;7:193–205. doi: 10.1054/math.2002.0477. [DOI] [PubMed] [Google Scholar]
- 138.Watson DH, Trott PH. Cervical headache: An investigation of natural head posture and upper cervical flexor muscle performance. Cephalgia. 1993;13:272–284. doi: 10.1046/j.1468-2982.1993.1304272.x. [DOI] [PubMed] [Google Scholar]
- 139.Ordway NR, Seymour R, Donelson RG, Hojnowski L, Lee E, Edwards WT. Cervical sagittal range-of-motion analysis using three methods. cervical range-of-motion device, 3space, and radiograph. Spine. 1997;22:501–508. doi: 10.1097/00007632-199703010-00007. [DOI] [PubMed] [Google Scholar]
- 140.Harrison DE, Harrison DD, Cailliet R. Cobb method or Harrison posterior tangent method: which to choose for lateral cervical radiographic analysis. Spine. 2000;25:2072–2078. doi: 10.1097/00007632-200008150-00011. [DOI] [PubMed] [Google Scholar]
- 141.Harrison DE, Cailliet R, Harrison DD, Janik TJ, Holland B. Reliability of Centroid, Cobb, and Harrison Posterior Tangent Methods: Which to choose for analysis of thoracic kyphosis. Spine. 2001;26:E227–E234. doi: 10.1097/00007632-200106010-00002. [DOI] [PubMed] [Google Scholar]
- 142.Harrison DE, Harrison DD, Cailliet R, Janik TJ, Holland B. Radiographic analysis of lumbar lordosis: Centroid, Cobb, TRALL, and Harrison Posterior Tangent Methods. Spine. 2001;26:E235–E242. doi: 10.1097/00007632-200106010-00003. [DOI] [PubMed] [Google Scholar]
- 143.Harrison DE, Holland B, Harrison DD, Janik TJ. Further reliability analysis of the Harrison radiographic line drawing methods: Crossed ICCs for lateral posterior tangents and AP Modified-Riser Ferguson. J Manipulative Physiol Ther. 2002;25:93–98. doi: 10.1067/mmt.2002.121411. [DOI] [PubMed] [Google Scholar]
- 144.Harrison DE, Harrison DD, Troyanovich SJ. Three-dimensional spinal coupling mechanics: part I. a review of the literature. J Manipulative Physiol Ther. 1998;21:101–113. [PubMed] [Google Scholar]
- 145.Harrison DE, Harrison DD, Troyanovich SJ. Three-dimensional spinal coupling mechanics: Part II. Implications for chiropractic theories and practice. J Manipulative Physiol Ther. 1998;21:177–186. [PubMed] [Google Scholar]
- 146.Harrison DE, Cailliet R, Harrison DD, Janik TJ, Troyanovich SJ, Coleman RR. Lumbar coupling during lateral translation of the thoracic cage relative to a fixed pelvis. Clin Biomech. 1999;14:704–709. doi: 10.1016/s0268-0033(99)00030-3. [DOI] [PubMed] [Google Scholar]
- 147.Harrison DE, Harrison DD, Cailliet R, Janik TJ, Troyanovich SJ. Cervical coupling during lateral head translation creates an S-configuration. Clin Biomech. 2000;15:436–440. doi: 10.1016/s0268-0033(99)00098-4. [DOI] [PubMed] [Google Scholar]
- 148.Harrison DE, Cailliet R, Harrison DD, Janik TJ. How do anterior/posterior translations of the thoracic cage affect the sagittal lumbar spine, pelvic tilt, and thoracic kyphosis? Euro Spine J. 2001;11:287–293. doi: 10.1007/s00586-001-0350-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 149.Harrison DE, Harrison DD, Colloca CJ, Betz J, Janik TJ, Holland B. Repeatability over time of posture, radiograph positioning, and radiograph line drawing: An analysis of six control groups. J Manipulative Physiol Ther. 2003;26:87–98. doi: 10.1067/mmt.2003.15. [DOI] [PubMed] [Google Scholar]
- 150.Harrison DD, Janik TJ, Troyanovich SJ, Holland B. Comparisons of lordotic cervical spine curvatures to a theoretical ideal model of the static sagittal cervical spine. Spine. 1996;21:667–675. doi: 10.1097/00007632-199603150-00002. [DOI] [PubMed] [Google Scholar]
- 151.Harrison DD, Janik TJ, Troyanovich SJ, Harrison DE, Colloca CJ. Evaluation of the assumptions used to derive an ideal normal cervical spinal model. J Manipulative Physiol Ther. 1997;20:246–256. [PubMed] [Google Scholar]
- 152.Janik TJ, Harrison DD, Cailliet R, Troyanovich SJ, Harrison DE. Can the sagittal lumbar curvature be closely approximated by an ellipse? J Orthop Res. 1998;16:766–770. doi: 10.1002/jor.1100160620. [DOI] [PubMed] [Google Scholar]
- 153.Harrison DD, Cailliet R, Janik TJ, Troyanovich SJ, Harrison DE, Holland B. Elliptical modeling of the sagittal lumbar lordosis and segmental rotation angles as a method to discriminate between normal and low back pain subjects. J Spinal Disord. 1998;11:430–439. [PubMed] [Google Scholar]
- 154.Harrison DE, Janik TJ, Harrison DD, Cailliet R, Harmon S. Can the thoracic kyphosis be modeled with a simple geometric shape? The results of circular and elliptical modeling in 80 asymptomatic patients. J Spinal Disord Tech. 2002;15:213–220. doi: 10.1097/00024720-200206000-00008. [DOI] [PubMed] [Google Scholar]
- 155.Harrison DD, Harrison DE, Janik TJ, Cailliet R, Hass JW. Do alterations in vertebral and disc dimensions affect an elliptical model of thoracic kyphosis? Spine. 2003;28:463–469. doi: 10.1097/01.BRS.0000048648.73805.98. [DOI] [PubMed] [Google Scholar]
- 156.Harrison DD, Harrison DE, Janik TJ, et al. Modeling of the sagittal cervical spine as a method to discriminate hypolordosis: results of elliptical and circular modeling in 72 asymptomatic subjects, 52 acute neck pain subjects, and 70 chronic neck pain subjects. Spine. 2004;29(22):2485–2492. doi: 10.1097/01.brs.0000144449.90741.7c. [DOI] [PubMed] [Google Scholar]
- 157.Farfan HF. Form and function of the musculoskeletal system as revealed by mathematical analysis of the lumbar spine. Spine. 1995;20:1462–1474. doi: 10.1097/00007632-199507000-00004. [DOI] [PubMed] [Google Scholar]
- 158.Harrison DE, Harrison DD, Janik TJ, Jones EW, Cailliet R, Normand M. Comparison of axial flexural stresses in lordosis and three buckled configurations of the cervical spine. Clin Biomech. 2001;16:276–284. doi: 10.1016/s0268-0033(01)00006-7. [DOI] [PubMed] [Google Scholar]
- 159.Harrison DE, Jones EW, Janik TJ, Harrison DD. Evaluation of axial and flexural stresses in the vertebral body cortex and trabecular bone in lordosis and two sagittal cervical translation configurations with an elliptical shell model. J Manipulative Physiol Ther. 2002;26:391–401. doi: 10.1067/mmt.2002.126128. [DOI] [PubMed] [Google Scholar]
- 160.Beck A, Killus J. Normal posture of spine determined by mathematical and statistical methods. Aerospace Medicine. 1973;44:1277–1281. [PubMed] [Google Scholar]
- 161.Beck A, Killus J. Analyse par conputer de la statique du rachis [Computer analysis of spinal measurements] J Radiol Electrol Med Nucl. 1975;56:402–403. [PubMed] [Google Scholar]
- 162.Kuchera M. Gravitational stress, musculoligamentous strain, and postural alignment. Spine: State of the Art Reviews. 1995;9:463–489. [Google Scholar]
- 163.Jackson RP, McManus AC. Radiographic analysis of sagittal plane alignment and balance in standing volunteers and patients with low back pain matched for age, sex, and size. Spine. 1994;19:1611–1618. doi: 10.1097/00007632-199407001-00010. [DOI] [PubMed] [Google Scholar]
- 164.Kiefer A, Shirazi-Adl A, Parnianpour M. Synergy of the human spine in neutral postures. Euro Spine J. 1998;7:471–479. doi: 10.1007/s005860050110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 165.Harrison DD. CBP Technique: The physics of spinal correction. National Library of Medicine #WE 725 4318C, 1982–1997, 1982.
- 166.Harrison DD. Abnormal postural permutations calculated as rotations and translations from an ideal normal upright static spine. In: Sweere JJ, ed. Chiropractic Family Practice. Gaithersburg: Aspen Publishers, 1992:1–22.
- 167.Harrison DE, Janik TJ, Cailliet R, Harrison DD, Normand MC, Black P, Perron DL. Validation of an algorithm to estimate 3-D rotations and translations of the rib cage in upright posture from three 2-D digital images. 8th Biennial Congress of the World Federation of Chiropractic, International Conference on Chiropractic Research, Sydney, Australia, June 16–18, 2005:328–329.
- 168.Harrison DE, Janik TJ, Cailliet R, Harrison DD, Normand MC, Black P, Perron DL. Validation of an algorithm to estimate 3-D rotations and translations of the head in upright posture from three 2-D images. 8th Biennial Congress of the World Federation of Chiropractic, International Conference on Chiropractic Research, Sydney, Australia, June 16–18, 2005:332–333.
- 169.Fischgrund JS. Surgical Management of Cervical Radiculopathy: Anterior Procedures. Part A. Anterior Cervical Discectomy and Fusion. Ch. 75. In: The Cervical Spine. 4th ed. Clark CR editor. Lippincott Williams and Wilkins, Philadelphia, 2005. page 1017,1023.
- 170.Haas M, Taylor JAM, Gillette RG. The routine use of radiographic spinal displacement analysis: a dissent. J Manipulative Physiol Ther. 1999;22:254–259. doi: 10.1016/s0161-4754(99)70053-9. [DOI] [PubMed] [Google Scholar]
- 171.Taylor JAM. The use of radiography in evaluating subluxation. In: Gatterman MI, ed. Foundations of chiropractic subluxation. St. Louis: Mosby, 1995:68–85.
- 172.Hariman DG. Letter to Editor [Harrison et al. The efficacy of cervical extension-compression traction combined with diversified manipulation and drop table adjustments in the rehabilitation of cervical lordosis] J Manipulative Physiol Ther. 1995;18:42–44. [PubMed] [Google Scholar]
- 173.Schultz GD, Bassano JM. Is radiography appropriate for detecting subluxations? Topics in Clinical Chiro. 1997;4:1–8. [Google Scholar]
- 174.Phillips RB. Plain film radiography in chiropractic. J Manipulative Physiol Ther. 1992;15:47–50. [PubMed] [Google Scholar]
- 175.Taylor JAM. Full-spine radiography: a review. J Manipulative Physiol Ther. 1993;16:460–474. [PubMed] [Google Scholar]
- 176.Cohen BL, Lee IS. A catalog of risks. Health Physics. 1979;36:707–722. doi: 10.1097/00004032-197906000-00007. [DOI] [PubMed] [Google Scholar]
- 177.International Atomic Energy Agency. Facts about low-level radiation. American Nuclear Society, 1982.
- 178.Maurer EL. Risk perspective. Dynamic Chiropractic 1990 (http://www.chiroweb.com/archives/08-14/11.html).
- 179.Butler G. Inflight occupational exposures to cosmic radiation and magnetic fields. Air Line Pilot. 2000;1:30+. [Google Scholar]
- 180.Kauffman JM. Diagnostic Radiation: Are the risks exaggerated? J Amer Phys Surg. 2003;8(2):54–55. [Google Scholar]
- 181.Cohen BL. Test of the linear-no threshold theory of radiation carcinogenesis for inhaled radon decay products. Health Physics. 1995;68(2):157–174. doi: 10.1097/00004032-199502000-00002. [DOI] [PubMed] [Google Scholar]
- 182.Cohen BL. The cancer risk from low level radiation: a review of recent evidence. Med Sent. 2000;5:128–131. [Google Scholar]
- 183.Cohen BL. Cancer risk from low-level radiation. AJR. 2002;179(5):1137–43. doi: 10.2214/ajr.179.5.1791137. [DOI] [PubMed] [Google Scholar]
- 184.Cohen BL. Catalog of risks extended and updated. Health Physics. 1991;61(3):317–335. doi: 10.1097/00004032-199109000-00002. [DOI] [PubMed] [Google Scholar]
- 185.Walker JS. Permissible dose: A history of radiation protection in the 20th century. Berkeley, Calif: University of California Press, Berkeley, 2000.
- 186.Harrison DE, Harrison DD, Hass JW. Structural rehabilitation of the cervical spine. Evanston, WY: Harrison CBP® Seminars, Inc., 2002.
- 187.Harrison DE, Harrison DD, Haas JW, Betz J, Oakley PA. CBP® structural rehabilitation of the lumbar spine. Evanston, WY: Harrison CBP® Seminars, Inc., 2005.
- 188.Regano LJ, Sutton RA. Radiation dose reduction in diagnostic X-ray procedures. Phys Med Biol. 1992;37(9):1773–1788. doi: 10.1088/0031-9155/37/9/004. [DOI] [PubMed] [Google Scholar]
- 189.Luckey TD. Radiation Hormesis. Boca Raton: CRC Press. 1991;5:228–230. [Google Scholar]
- 190.Luckey TD. Nurture with ionizing radiation: a provocative hypothesis. Nutrition Cancer. 1999;34(1):1–11. doi: 10.1207/S15327914NC340101. [DOI] [PubMed] [Google Scholar]
- 191.Sherwood T. 100 years’ observation of risks from radiation for British male radiologists. Lancet. 2001;358:604. doi: 10.1016/S0140-6736(01)05818-4. [DOI] [PubMed] [Google Scholar]
- 192.Stokes IAF, Bevins TM, Lunn RA. Back surface curvature and measurement of lumbar spinal motion. Spine. 1987;12:355–361. doi: 10.1097/00007632-198705000-00009. [DOI] [PubMed] [Google Scholar]
- 193.Johnson GM. The correlation between surface measurement of head and neck posture and the anatomic position of the upper cervical vertebrae. Spine. 1998;23:921–927. doi: 10.1097/00007632-199804150-00015. [DOI] [PubMed] [Google Scholar]
- 194.Refshauge KM, Goodsell M, Lee M. The relationship between surface contour and vertebral body measures of upper spine curvature. Spine. 1994;19:2180–2185. doi: 10.1097/00007632-199410000-00010. [DOI] [PubMed] [Google Scholar]
- 195.Mosner EA, Bryan JM, Stull MA, Shippee R. A comparison of actual and apparent lumbar lordosis in black and white adult females. Spine. 1989;14:310–331. doi: 10.1097/00007632-198903000-00011. [DOI] [PubMed] [Google Scholar]
- 196.Harrison DE, Haas JW, Cailliet R, Harrison DD, Holland B, Janik TJ. Concurrent validity of the flexicurve instrument measurements: sagittal skin contour of the cervical spine compared to lateral cervical radiographic measurements. J Manipulative Physiol Ther 2005; in Press. [DOI] [PubMed]
- 197.Committee to Assess Heath Risks from Exposure to Low Levels of Ionizing Radiation. Health risks from exposure to low levels of ionizing radiation: BEIR VII Phase 2. National Research Council. Washington DC: National Academies Press, 2005. [PubMed]
- 198.Kant K, Chauhan RP, Sharma GS, Chakarvarti SK. Hormesis in animals exposed to low-level ionizing radiation. Inter J Low Rad. 2003;1(1):76–87. [Google Scholar]
- 199.Feinendegen LE. Evidence for beneficial low level radiation effects and radiation hormesis. Br J Radiol. 2005;78:3–7. doi: 10.1259/bjr/63353075. [DOI] [PubMed] [Google Scholar]
- 200.Parsons PA. Hormesis: an adaptive expectation with emphasis on ionizing radiation. J Appl Tox. 2000;20:103–112. doi: 10.1002/(sici)1099-1263(200003/04)20:2<103::aid-jat639>3.0.co;2-o. [DOI] [PubMed] [Google Scholar]
- 201.Pollycove M. The issue of the decade: hormesis. Eur J Nucl Med. 1995;22:399–401. doi: 10.1007/BF00839052. [DOI] [PubMed] [Google Scholar]
- 202.Pollycove M. Nonlinearity of radiation health effects. Env Health Persp. 1998;106:363–368. doi: 10.1289/ehp.98106s1363. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 203.Luckey TD. Hormesis with Ionizing Radiation. CRC Press, Boca Raton, FL, 1980:
- 204.Cohen BL. Problems in the radon vs. lung cancer test of the linear no-threshold theory and a procedure for resolving them. Health Phys. 1997;72:623–628. doi: 10.1097/00004032-199704000-00015. [DOI] [PubMed] [Google Scholar]
- 205.Cohen BL. Updates and extensions to tests of the linear no-threshold theory. Technology. 2000;7:657–672. [Google Scholar]
- 206.Frigerio NA, Eckerman KF, Stowe RS. Carcinogenic hazard from low-level, low-rate radiation, Part I. Rep.ANL/ES-26.Argonne Nat.Lab 1973.
- 207.Jagger J. Natural background radiation and cancer death rate in Rocky Mountain and Gulf Coast States. Health Phys. 1998;75:428–434. doi: 10.1097/00004032-199810000-00012. [DOI] [PubMed] [Google Scholar]
- 208.Kostyuchenko VA, Krestina L. Long-term irradiation effects in the population evacuated from the east-Urals radioactive trace area. Sci Total Environ. 1994;142:119–125. doi: 10.1016/0048-9697(94)90080-9. [DOI] [PubMed] [Google Scholar]
- 209.Matanoski, G. M. Health effect of low level radiation in shipyard workers: final report. report no. DOE DE-AC02–79 EV10095. 1991. Washington, DC, US Dept of Energy.
- 210.Hickey RJ, Bowers EJ, Clelland RC. Radiation hormesis, public health, and public policy: a commentary. Health Phys. 1983;44:207–219. doi: 10.1097/00004032-198303000-00001. [DOI] [PubMed] [Google Scholar]
- 211.Tubiana M. The carcinogenic effect of low doses: the validity of the linear no-threshold relationship. Int J Low Rad. 2003;1:1–33. [Google Scholar]
- 212.Cameron JR. Moderate doae rate ionizing radiation increases longevity. Br J Radiol. 2005;78:11–13. doi: 10.1259/bjr/62063624. [DOI] [PubMed] [Google Scholar]
- 213.Cameron JR. Radiation increased the longevity of British radiologists. Br J Radiol. 2002;75:637–640. doi: 10.1259/bjr.75.895.750637. [DOI] [PubMed] [Google Scholar]
- 214.Cameron JR. Longevity is the most appropriate measure of health effects of radiation. Radiol. 2003;229:14–15. doi: 10.1148/radiol.2291030291. [DOI] [PubMed] [Google Scholar]
- 215.Cameron JR. Is radiation an essential trace energy? Physics and Society 2001; Oct:http://www.aps.org/units/fps/newsletters/2001/october/a50ct01.html
- 216.Parsons PA. Radiation hormesis: an ecological and energetic perspective. Med Hypoth. 2000;57:277–279. doi: 10.1054/mehy.2000.1240. [DOI] [PubMed] [Google Scholar]
- 217.Luckey TD. Radiation hormesis in cancer mortality. Chi Med J. 1994;107:627–630. [PubMed] [Google Scholar]
- 218.Harrison DD, Janik TJ, Harrison GR, Troyanovich SJ, Harrison DE, Harrison SO. Chiropractic biophysics technique: A linear algebra approach to posture in chiropractic. J Manipulative Physiol Ther. 1996;19:525–535. [PubMed] [Google Scholar]
- 219.Hrysomallis C, Goodman C. A review of resistance exercise and posture realignment. J Strength Cond Res. 2001;15:385–390. [PubMed] [Google Scholar]
- 220.Den Boer WA, Anderson PG, Limbeek JV, Kooijman MA. Treatment of idiopathic scoliosis with side shift therapy. an initial comparison with a brace treatment historical cohort. Euro Spine J. 1999;8:406–410. doi: 10.1007/s005860050195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 221.Weiss HR. Influence of an in-patient exercise program on scoliotic curve. Italian Journal of Orthopaedics & Traumatology. 1992;18:395–406. [PubMed] [Google Scholar]
- 222.Weiss HR, Lohschmidt K, el-Obeich N, Verres C. Preliminary results and worst-case analysis of inpatient scoliosis rehabilitation. Pediatr Rehabil. 1997;1:35–40. doi: 10.3109/17518429709060940. [DOI] [PubMed] [Google Scholar]
- 223.Weiss HR. The Schroth scoliosis-specific back school-Initial results of a prospective follow-up study. Orthop Ihre Grenzgeb. 1995;133:114–117. doi: 10.1055/s-2008-1039421. [DOI] [PubMed] [Google Scholar]
- 224.Pearson ND, Walmsley RP. Trial into the effects of repeated neck retractions in normal subjects. Spine. 1995;20:1245–1251. doi: 10.1097/00007632-199506000-00006. [DOI] [PubMed] [Google Scholar]
- 225.DeVocht JW, Pickar JG, Wilder DG. EMG activity levels of paraspinal muscles during spinal manipulation. Proceedings of International Society for the Study of the Lumbar Spine, Cleveland, Ohio, May 14–18, 2002.
- 226.Harrison DD. Spinal Biomechanics: A Chiropractic Perspective. National Library of Medicine #WE 725 4318C, 1982–1997.
- 227.Oliver MJ, Twomey LT. Extension creep in the lumbar spine. Clin Biomech. 1995;10:363–368. doi: 10.1016/0268-0033(95)00001-2. [DOI] [PubMed] [Google Scholar]
- 228.Paulk GP, Bennett DL, Harrison DE.Management of a chronic lumbar disk herniation with CBP methods following failed chiropractic manipulative intervention J Manipulative Physiol Ther2004279579e1–579e7. [DOI] [PubMed] [Google Scholar]
- 229.Bastecki A, Harrison DE, Haas JW. ADHD: A CBP case study. J Manipulative Physiol Ther. 2004;27(8):525e1–525e5. doi: 10.1016/j.jmpt.2004.08.007. [DOI] [PubMed] [Google Scholar]
- 230.Ferrantelli JR, Harrison DE, Harrison DD, Steward D. Conservative management of previously unresponsive whiplash associated disorders with CBP methods: a case report. J Manipulative Physiol Ther. 2005;28(3):205e1–205e8. doi: 10.1016/j.jmpt.2005.02.006. [DOI] [PubMed] [Google Scholar]
- 231.Haas JW, Harrison DE, Harrison DD, Bymers B. Conservative treatment of a patient with syringomyelia using chiropractic biophysics protocols. J Manipulative Physiol Ther. 2005;28(6):452e1–452e7. doi: 10.1016/j.jmpt.2005.06.005. [DOI] [PubMed] [Google Scholar]
- 232.Berry RH, Oakley PA, Harrison DE. A structural approach to the post-surgical laminectomy. J Chiropractic Education. 2005;19(1):44. [Google Scholar]
- 233.Harrison DE, Bula JB, Harrison DD. Non-operative correction of flat back using lumbar extension traction: A case study of three. J Chiropractic Education. 2003;17(1):13–14. [Google Scholar]
- 234.Oakley PA, Harrison DE. Use of Clinical Biomechanics of Posture (CBP®) protocol in a postsurgical C4–C7 total fusion patient: A case study. J Chiropractic Education. 2005;19(1):66. [Google Scholar]
- 235.Troyanovich SJ, Harrison SO, Harrison DD, et al. Chiropractic Biophysics digitized radiographic mensuration analysis of the anteroposterior lumbar view: A reliability study. Journal of Manipulative and Physiological Therapeutics. 1999;22:309–315. doi: 10.1016/s0161-4754(99)70063-1. [DOI] [PubMed] [Google Scholar]
- 236.Harrison DE, Harrison DD, Troyanovich SJ. Reliability of spinal displacement analysis on plane x-rays: A review of commonly accepted facts and fallacies with implications for chiropractic education and technique. J Manipulative Physiol Ther. 1998;21(4):252–66. [PubMed] [Google Scholar]
- 237.Haldeman S, Kohlbeck FJ, Mcgregor M. Risk factors and precipitating neck movements causing vertebrobasilar artery dissection after trauma and spinal manipulation. Spine. 1999;24:785–794. doi: 10.1097/00007632-199904150-00010. [DOI] [PubMed] [Google Scholar]
- 238.Thiel H, Wallace K, Donat J, Yong-Hing K. Effect of various head and neck positions on vertebral artery blood flow. Clin Biomech. 1994;9:105–110. doi: 10.1016/0268-0033(94)90032-9. [DOI] [PubMed] [Google Scholar]
- 239.Weintraub M. Beauty parlor stroke syndrome: a report of two cases. Neurology. 1992;42 (suppl):340. [Google Scholar]
- 240.Weintraub M. Beauty parlor stroke syndrome: a report of five cases. [Letter to editor] JAMA. 1993;269:2085–2086. doi: 10.1001/jama.1993.03500160051022. [DOI] [PubMed] [Google Scholar]
- 241.Weintraub M. Beauty parlor stroke: When a beautician becomes a physician. [Reply to Letter to Editor] JAMA. 1993;270:1198–1199. doi: 10.1001/jama.270.10.1198b. [DOI] [PubMed] [Google Scholar]
- 242.Stratigos J. Vertebrobasilar disease and beauty parlor stroke syndrome. Am Family Phys. 1995;52:1287–1290. [PubMed] [Google Scholar]
- 243.Endo K, Ichimaru K, Shimura H, Imakiire A. Cervical vertigo after hair shampoo treatment at a hairdressing salon: a case report. Spine. 2000;25(5):632–634. doi: 10.1097/00007632-200003010-00017. [DOI] [PubMed] [Google Scholar]
- 244.Kaptchuk TJ. The double-blind, randomized, placebo-controlled trial: gold standard or golden calf? J Clin Epidemiol. 2001;54:541–549. doi: 10.1016/s0895-4356(00)00347-4. [DOI] [PubMed] [Google Scholar]
- 245.Keating JC., Jr Several pathways in the evolution of chiropractic manipulation. J Manipulative Physiol Ther. 2003;26:300–321. doi: 10.1016/S0161-4754(02)54125-7. [DOI] [PubMed] [Google Scholar]