Abstract
Objective
To determine the effects of a semi-customized experimental cervical pillow on symptomatic adults with chronic neck pain (with and without headache) during a four week study.
Design
A randomized controlled trial.
Sample size
Thirty-six adults were recruited for the trial, and randomly assigned to experimental or non-experimental groups of 17 and 19 participants respectively.
Subjects
Adults with chronic biomechanical neck pain who were recruited from the Canadian Memorial Chiropractic College (CMCC) Walk-in Clinic.
Outcome measures
Subjective findings were assessed using a mail-in self-report daily pain diary, and the CMCC Neck Disability Index (NDI).
Statistical analysis
Using repeated measure analysis of variance weekly NDI scores, average weekly AM and PM pain scores between the experimental and non-experimental groups were compared throughout the study.
Results
The experimental group had statistically significant lower NDI scores (p < 0.05) than the non-experimental group. The average weekly AM scores were lower and statistically significant (p < 0.05) in the experimental group. The PM scores in the experimental group were lower but not statistically significant than the other group.
Conclusions
The study results show that compared to conventional pillows, this experimental semi-customized cervical pillow was effective in reducing low-level neck pain intensity, especially in the morning following its use in a 4 week long study.
Keywords: pillow, neck pain
Abstract
Objectif
Déterminer les effets d’un oreiller cervical semi-personnalisé à l’essai sur des adultes qui manifestent des symptômes de douleur cervicale chronique (avec ou sans maux de tête) durant la période d’étude de quatre semaines.
Étude
Un essai randomisé contrôlé
Échantillonnage
Pour l’essai, trente-six adultes ont été recrutés et divisés au hasard en deux groupes : un groupe expérimental de 17 participants et un groupe non expérimental de 19 participants.
Sujets
Les adultes ayant des douleurs cervicales biomécaniques chroniques ont été recrutés à la clinique sans rendezvous du Canadian Memorial Chiropractic College (CMCC).
Mesures d’impact
Des déclarations subjectives ont été recueillies à l’aide d’un journal quotidien d’auto-évaluation de la douleur que les participants devaient poster et grâce à l’Index d’invalidité cervicale (Neck Disability Index (NDI) du CMCC.
Analyse statistique
La moyenne hebdomadaire des résultats de la douleur ressentie en avant-midi et en après-midi des groupes expérimental et non expérimental a été comparée pendant toute la durée de l’étude à l’aide de l’analyse de variance hebdomadaire par mesure répétée des résultats de l’Index d’invalidité cervicale (NDI).
Résultats
Les résultats de l’Index d’invalidité cervicale (NDI) du groupe expérimental étaient, de façon statistiquement significative (p < 0,05), inférieurs à ceux du groupe non expérimental. La moyenne hebdomadaire des résultats de l’avant-midi du groupe expérimental était inférieure et statistiquement significative (p < 0,05). Les résultats de l’après-midi du groupe expérimental étaient inférieurs, mais non statistiquement significatifs, à ceux de l’autre groupe.
Conclusions
Les résultats de l’étude démontrent que l’oreiller cervical semi-personnalisé à l’essai, comparé à un oreiller conventionnel, est efficace pour réduire l’intensité de la douleur à la base du cou, spécialement le matin, dans les heures suivant son utilisation, durant les quatre semaines de l’étude.
Introduction
This is the third in a series of pilot studies involving the pre-testing of an experimental prototype cervical pillow. The first two studies were published in recent issues of JCCA,1,2 where the literature is discussed in detail.
Neck pain, both chronic and acute, affects a considerable percentage of people at any given time. It has an overall point prevalence of 9–14% and lifetime prevalence of 33% in the North American adult population.3–4 Point prevalence is highest in the 50–59 year-old age category. More females are affected than males, with lifetime prevalence at about 30% and 15% respectively.5–7
Since an estimated one-third of a person’s life is spent sleeping, acute and chronic cervical pain may benefit from management strategies which include modalities such as cervical pillows.8 With the growing interest in the role of cervical pillows, an increasing number of studies have recently been published.8–15 The results of our literature search thorough MEDLINE, Index to Chiropractic Literature and MANTIS are briefly summarized below.
Review of the Literature
The lordotic cervical curve has long been recognized as necessary for maintaining human bipedal posture.16 Gray’s Anatomy17 states that the cervical curve is a secondary curve which first appears in intrauterine life and “is further accentuated when the child is able to hold up its head (at three to four months), and to sit upright (about nine months)”. Recognizing this, Leach18 radiographically evaluated the cervical curve depths (CCD) of 35 patients who presented with cervical hypolordosis or kyphosis (CH/K). Of these, one group of 20 patients who received only chiropractic manipulative therapy (CMT) gained a mean improvement of 4.55 degrees while the second group of 9 patients who received both CMT and orthopaedic cervical pillow therapy improved 2.22 degrees (p < 0.01). The control group of 6 patients had a mean improvement of 0.83 degrees. The importance of this finding is clouded by the fact that the author had no way of knowing if the patients assigned to the cervical pillow used it properly. Proper usage is likely very important in achieving clinically important benefit.2
A case series by Smythe19 involving 91 prior Fibromyalgia patients and 60 non-prior Fibromyalgia patients, all with neck pain, found that after 18 months of using a cervical pillow, 63% and 84% respectively, achieved clinically important relief. This bodes well for further controlled study, but the Smythe design is by no means a confirmatory one.
Jackson,20 in a study using lateral radiographs of the cervical spine with and without exposure to regular and roll-shaped pillows, concluded that the roll-shaped pillow restores the cervical lordosis (while supporting the head and neck), and decreases neck pain and discomfort while sleeping. However, with regard to the alleviation of symptoms, not enough is revealed about how the data were collected.
Hagino et al.21 evaluated the effectiveness of the Align-Right Cylindrical cervical pillow in reducing chronic neck pain severity. Twenty-eight subjects participated in this Before-After trial, for a period of 6 weeks (including a 2-wk baseline). The investigators concluded that the data suggest that clinically important benefits can be expected from a similar chronic neck pain population. Because a Before-After study is not a confirmatory design, the investigators also recommended further study using the RCT design to compare the Align-Right Cylindrical pillow to other commonly used cervical pillows.
Lavin et al.7 studied 41 subjects with benign cervical pain in a randomized crossover trial comparing 3 pillows (the subjects’ usual pillow, a roll pillow and a water-based pillow) with regard to pain intensity, pain relief, quality of sleep, disability, and overall satisfaction. All the subjects were diagnosed with benign cervical pain syndromes and were selected from outpatient neurology and physiatry clinics. The investigators concluded that proper selection of a pillow significantly reduces pain and improves quality of sleep, but does not significantly affect disability outcomes as measured by the Sickness Impact Profile (SIP). In this study there is no mention of a “washout period” between pillow administrations (to bring the subjects back to their base-line levels); without this, it is unclear whether there were any carryover effects between different pillows. Furthermore, the analysis appears to have utilized the mean of each post-treatment period, rather than pre-post treatment period changes, so it is not clear whether the cross-over data may not largely be the post-treatment data of the previous pillow.
Person and Mortiz22 tested 6 different pillows on neck pain and quality of sleep. 55 subjects (37 hospital employees and 18 neck patients) tested all of the pillows in random order over the course of 3 weeks (3 consecutive nights per pillow). The authors concluded that pillows with firm support for the cervical lordosis could be recommended for the management of neck pain. However, this study suffers from several problems which limit its usefulness as a confirmatory study. Since the subjects used each pillow for only three nights, no conclusion with respect to the long-term effects of these pillows could be made. Furthermore, for this particular complaint, three nights may be too short to obtain clinically meaningful physiological and subsequent symptom changes to occur. Finally, there was no washout period (bringing the subjects back to their baseline levels) between administrations of the six pillows, thereby possibly resulting in clinically important carryover effects.
Hayland23 reviewed the above three studies (Hagino et al., Lavin et al., and Person et al.) and concluded that a pillow, which supplies a choice of sides, is more likely to be helpful to a broad range of clients. He also stated that prescribing a good cervical support pillow is an important adjunctive therapy in the chiropractic management of neck pain.
Palazzi et al.24 assessed the effects of two types of pillows on bilateral sternocleidomastoid muscles EMG activity in healthy subjects and in patients with myogenic craio-cervical-mandibular dysfunction. The study was performed on 15 patients with myogenic cranio-cervical-mandibular dysfunction (CMD) subjects and 15 healthy subjects. EMG recordings at rest and during swallowing of saliva and maximal voluntary clenching were performed by placing surface electrodes on the right and left sternocleidomastoid muscles. EMG activity was recorded in the supine position and in the lateral decubitus position with the head supported by: 1. A Sleep Easy Pillow (interwood Marketing Groups, Concord, Ontario, Canada) and 2. A Standard Pillow (INDUVET). In the lateral decubitus position a significantly higher contralateral than ipsilateral EMG activity at rest in the sternocleidomastoid muscles was observed with both types of pillows in healthy subjects as well as in patients with myogenic CMD (ANOVA and Duncan’s Multiple-Range Test). The authors suggested that if the lateral decubitus posture is prolonged, it could be important in the genesis of sternocleidomastoid hyperactivity.
Santander et al.25 also assessed the effects of head and neck inclination on bilateral sternoleidomastoid EMG activity in healthy subjects and in patients with myogenic cranio-cervical-mandibular dysfunction. The study was performed on 16 electromyographic cranio-cervical-mandibular dysfunction (CMD) and 16 healthy subjects. EMG recordings at rest and during swallowing of saliva and maximal voluntary clenching were performed by placing surface electrodes on the right and left sternocleidomastoid muscles. EMG activity was recorded in the left lateral decubitus position, under the following experimental conditions: 1. Head, neck and body horizontally aligned, 2. Head and neck upwardly inclined with respect to the body, simulating the effect of a thick pillow, 3. Head and neck downwardly inclined with respect to body, simulating the effect of a thin pillow. A significantly higher contralateral EMG activity and a more asymmetric EMG activity were observed in the CMD group than in the healthy subjects (Kruskal-Wallis Test). The results suggested a different behavior of bilateral sternocleidomastoid EMG activity in CMD patients than in healthy subjects depending on the positioning of the head and neck.
Erfanian et al.1 assessed whether external measurements of the subject’s neck are predictive of the preferred thickness of cervical pillow, given a choice of four different contour thicknesses. This study utilized a preliminary correlational design. A total of 105 subjects were assessed using measurements of the cervical spine from:
the external occipital protuberance (EOP) to the seventh cervical spinous process posteriorly,
from the mastoid to the acromioclavicular joint laterally, and
the neck girth measured at the fourth cervical vertebra.
After being given about 10 minutes to test the pillow, subjects were asked to select the most comfortable of the four thicknesses. This study found neither statistically significant nor clinically important correlation between neck dimensions and pillow size preference.
Erfanian et al.2 subsequently tested for any adverse effects of a semi-customized (variable thickness) cervical pillow prototype on 23 asymptomatic adults. In this Before-After study, the subjects used the cervical pillow for one week, and were monitored on a daily basis via a daily diary type of self-report questionnaire. The questionnaire included the outcome measures of pain severity, sleep quality, and pillow comfort. None of the analyses yielded clinically important or statistically significant differences between the pre and post-pillow measures, and the majority (91%) of subjects did not experience any painful adverse effects. From this, the authors concluded that the cervical pillow prototype is ethically safe to test further on a demographically similar symptomatic population.
The objective of the present study is therefore to determine the effects of this cervical pillow prototype on adults with chronic biomechanical neck pain, with and without headache. Adverse effects, pain relief, and activities of daily living during four weeks of test-pillow usage were assessed.
Methods and materials
Design architecture
A randomized controlled trial design of four weeks duration was used.
The experimental intervention
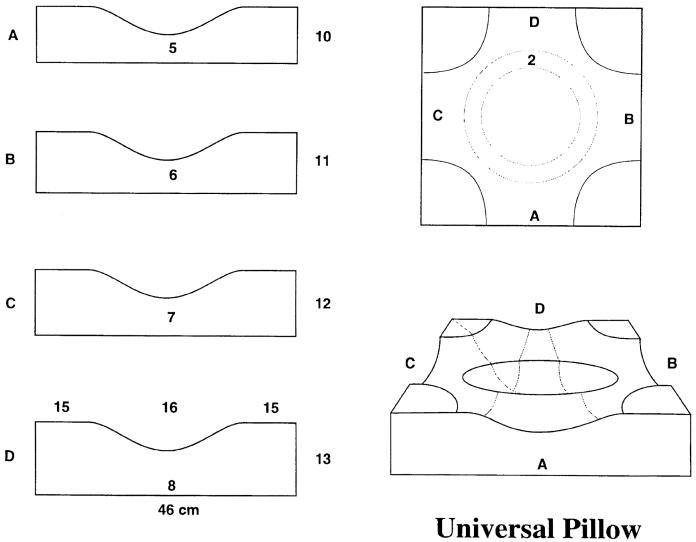
A cervical pillow prototype with foam quadrants of increasing height was administered to the experimental group. Although this pillow is not fully customized for each user, it offers the user the option of choosing between four heights (Figure 1). Due to the variability in human neck thickness and shoulder width, a different height of pillow may be required when someone is lying on his/her back as opposed to side. This potential problem is addressed by this semi-customized pillow in that a shorter height throughout the middle curved area for supine sleeping, and a higher height on the either sides of the curved area for lateral recumbent sleep posture is provided.
Figure 1.
The test (semi-customized) pillow Universal Pillow
Objectives
To determine the effects of a semi-customized experimental cervical pillow on symptomatic adults with chronic neck pain (with and without headache) during a four week study.
Sample profile
Study participants consisted of adults (> 25 years of age) who presented to the CMCC Herbert K. Lee Walk-in Outpatient Clinic with chronic biomechanical neck pain with and without headache. For the purposes of this study, chronic neck pain is defined as neck pain with onset at least 3 months prior to the participant’s enrolment in the study.8 Chronic pain participants were targeted for this study since neck-pain sufferer are presumed to be most likely spending money on devices to help correct the problem; in effect, the chronic pain sufferer is likely to comprise a sizable proportion of the market for such devices.
Exclusion criteria consisted of: any trauma (such as a motor vehicle accident) experienced within the last year, migraine headache, and known organic pathology within or referring to the cervical spine. These exclusions allowed us to limit the eligible subjects to chronic biomechanical neck pain patients. Subjects normally using no pillow or anything other than a conventional pillow were also excluded.
With regard to the headache aspect, since Vernon et al.26 found that the neck plays an important role in the manifestation of adult benign headaches, participants concurrently suffering from benign headaches were not excluded.
All eligible and participating patients provided written, informed consent prior to enrolment in the study.
Sample size
A sample size estimate was performed using the SPSS Sample Power Version 2.0 program. At the 5% level of significance, a power level of 80%, a clinically important mean between-groups change of 1 unit on the 11-point Numerical Rating Pain Scale (NRS), and with a pooled standard deviation of 1 unit, the sample size estimate revealed that a minimum of 17 participants per group would be necessary. Therefore, a sample of 36 participants was recruited for this trial. This sample was randomly allocated to the experimental and control groups, resulting in 17 and 19 subjects in each group, respectively.
Outcome measures
A one-week daily diary type of self-report questionnaire (Appendix 1) which incorporated an 11-point Numerical Rating Pain Scale (NRS) to collect the primary outcome measures of pre- and post-sleep neck pain was used. The NRS has been shown to be a valid and reliable pain-intensity assessment scale.27 Participants also completed the CMCC Neck Disability Index (NDI) once per week for the duration of study.
Protocol
Participants were randomly allocated to the non-experimental and experimental groups. In the former, the participant continued using his/her usual generic pillow, while in the latter, the participant used the experimental cervical pillow prototype. The participants were asked to use their assigned pillows every night for the next four consecutive weeks. They were instructed to fill in their diary questionnaires on a daily basis, and complete the NDI form once at the beginning of each new week. Participants were also instructed to mail each weeks set of questionnaires back to CMCC in the pre-addressed and stamped envelopes provided.
Subjects were asked to continue their regular activities of daily living during the study period, and to the degree possible, to refrain from taking pain medications and other therapies for their neck pain.
Statistical analysis
Daily PM and AM NRS as well as weekly NDI scores of the participants in each group were compared using repeated measure analysis of variance. Assumptions of compound symmetry were tested using the Muchly’s test of sphericity.31
Differences in pain scores were analyzed using independent sample t-tests procedures comparing Week 4 with Week 1 (study’s end and starting point respectively).
Results
Of the 36 subjects who consented to participate; six failed to complete all the required questionnaires and were not included in the analysis; four experienced unexpected problems such as stress at work, death in the family and sports injuries, and hence could not complete the study; one found the pillow uncomfortable and withdrew from the study during the second week.
Demographic profile of the participants is presented in Table 1. The mean (Sd) neck pain duration values for each of the experimental and non-experimental groups were 6.4 (5.1) years and 7.9 (10.3) years, respectively, with a minimum of 3 months to a maximum of 38 years.
Table 1.
Demographic Profile of the Participants
| Experimental Group (n, %) | Non-Experimental Group (n, %) | |
|---|---|---|
| Gender | Males (2, 14.3) | Males (6, 54.4) |
| Females (12, 85.7) | Females (5, 45.5) | |
| Age (SD) | 34.1 (9.5) | 30.2 (7.7) |
The mean NDI Scores for weeks 1 to 4 are presented in Table 2. As seen the experimental group showed lower and statistically significant (F = 3.51, p < 0.05) mean NDI scores than the non-experimental group.
Table 2.
Weekly NDI Scores
| Experimental Group mean (SD) | Non-Experimental Group mean (SD) | ||
|---|---|---|---|
| Weekly NDI Score | Week 1 | 14.18 (7.77) | 11.21 (6.42) |
| Week 2 | 14.00 (7.10) | 12.79 (16.33) | |
| Week 3 | 11.09 (5.54) | 13.21 (16.28) | |
| Week 4 | 9.27 (6.02) | 15.64 (14.96) |
F (Greenhouse-Geisser32 = 3.51), P = 0.04
Weekly AM and PM pain-NRS scores showed lower scores for the experimental group with the AM scores being statistically significant (F = 3.23, p < 0.05) (Table 3).
Table 3.
Weekly AM and PM NRS Scores
| Experimental Group mean (SD) | Non-Experimental Group mean (SD) | ||
|---|---|---|---|
| F = 1.86, P = 0.14 | |||
| Weekly PM Scores | Week 1 | 3.08 (2.34) | 1.39 (0.79) |
| Week 2 | 2.56 (2.16) | 1.29 (1.32) | |
| Week 3 | 2.47 (1.80) | 1.49 (1.28) | |
| Week 4 | 2.37 (1.47) | 1.81 (1.32) | |
| Experimental Group mean (SD) | Non-Experimental Group mean (SD) | ||
|---|---|---|---|
| F (Greenhouse-Geisser = 3.23), P = 0.04 | |||
| Weekly AM Scores | Week 1 | 2.29 (2.13) | 1.32 (1.24) |
| Week 2 | 1.98 (1.87) | 1.13 (1.36) | |
| Week 3 | 1.82 (1.71) | 1.22 (1.27) | |
| Week 4 | 1.56 (1.45) | 1.49 (1.49) | |
Differences in the average AM reported pain scores between week 4 and 1 were statistically different in the experimental group (t-test = 2.53, p < 0.05) (Table 4).
Table 4.
Difference in AM and PM Pain Scores (Week 4–1)
| Experimental Group mean (SD) | Non-Experimental Group mean (SD) | ||
|---|---|---|---|
| t-test = 2.53, P = 0.03 | |||
| Difference in AM Pain | −0.72 (1.15) | 0.17 (0.21) | |
| Experimental Group mean (SD) | Non-Experimental Group mean (SD) | ||
|---|---|---|---|
| t-test = 1.88, P = 0.07 | |||
| Difference in PM Pain | −0.71 (1.48) | 0.42 (1.50) | |
Discussion
Reasons for dropping out of the study were not due to adverse effects of using the pillow except in one case. Despite a large drop out the study results remained statistically significant in the NDI and weekly AM pain-NRS scores.
Although the study included subjects with mild pain levels, the effects of the experimental pillow use were still evident.
Problems with this study
Although the NRS and NDI are considered reliable and responsive instruments,28 chronic pain clients tend to be relatively more desensitized to their pain levels than their acute and subacute counterparts.29,30 Tait et al.29 found that pain duration correlated negatively with the level of disability. They suggest that people generally accommodate to pain when it persists over time.
Participants may have not used the pillow as prescribed. Although this pillow is not fully customized, it offers the user the option of choosing between four heights as well as different positioning arrangement for supine or lateral recumbent sleep posture. Proper usage is likely very important in achieving clinically important benefits.2
Recommendations
Subjects with more severe neck-pain to be tested.
A larger sample of a minimum of 17 subjects per intervention group to be recruited.
The follow-up period to be several weeks longer to assess long-term effects.
Conclusion
This study suggests that compared to conventional pillows, the experimental semi-customized cervical pillow in this study proved to be effective in reducing daily AM neck pain and weekly NDI scores in a group of chronic neck pain sufferers.
Acknowledgments
Contribution of Dr. Jacqueline Roberts in preparation of this article is greatly acknowledged.
Appendix #1 ONE WEEK DAILY DIARY
| Subject #: | ||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Week #: | ||||||||||||||||
| Day # | 1 | 2 | 3 | 4 | 5 | 6 | 7 | |||||||||
| Which Side of pillow did you sleep on last night? | ||||||||||||||||
| A, B, C or D | ||||||||||||||||
| Rate the pain that you experienced at bedtime. | ||||||||||||||||
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | |||||||
| none | moderate | worse ever | ||||||||||||||
| Rate the pain that you experienced waking in the morning. | ||||||||||||||||
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | |||||||
| none | moderate | worse ever | ||||||||||||||
| The pillow promoted sleeping on your: | ||||||||||||||||
| back = 1 | ||||||||||||||||
| Side = 2 | ||||||||||||||||
| Stomach = 3 | ||||||||||||||||
| Rate the comfort level offered by the pillow: | ||||||||||||||||
| Very comfortable = 1 | ||||||||||||||||
| Somewhat comfortable = 2 | ||||||||||||||||
| Somewhat uncomfortable = 3 | ||||||||||||||||
| Uncomfortable = 4 | ||||||||||||||||
| How did your neck pain affect your activity today? | ||||||||||||||||
| No effect = 0 | ||||||||||||||||
| Minimal effect = 1 | ||||||||||||||||
| Interference with work/leisure = 2 | ||||||||||||||||
| Absent from work/school = 3 | ||||||||||||||||
| Has anything unusual happened today that may have affected your neck pain? Y/N If so, what? (use the space at the bottom if necessary). | ||||||||||||||||
| Did you take a painkiller for your neck pain today? | ||||||||||||||||
| How many? | ||||||||||||||||
References
- 1.Erfanian P, Hagino C, Guerriero R. Pilot study: An investigation on the relationship between external cervical measurements and the preference of cervical pillow thickness. JCCA. 1998;42(2):83–89. [Google Scholar]
- 2.Erfanian P, Hagino C, Guerriero R. A preliminary study assessing adverse effects of a semi-customized cervical pillow on asymptomatic adults. JCCA. 1998;42(3):156–162. [Google Scholar]
- 3.Bland JH. Disorders of the cervical spine. Philadelphia: Saunders, 1987: 1–8.
- 4.Shekelle PG, Brook RH. A community-based study of the use of chiropractic services. Am J Pub Health. 1991;81(4):439–442. doi: 10.2105/ajph.81.4.439. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Van der Donk J, Schouten JSA, Passchier J, Van Roumunde LKJ, Valkenburg HA. The associations of neck pain with radiological abnormalities of the cervical spine and personality traits in a general population. J Rheumatol. 1991;18(12):1884–1889. [PubMed] [Google Scholar]
- 6.Brussieres A. A review of functional outcome measures for cervical spine disorders: literature review. JCCA. 1994;38(1):32–40. [Google Scholar]
- 7.Lavin RA, Pappagallo M, Kuhlemeier KV. Cervical pain: a comparison of three pillows. Arch Phys Med Rehabil. 1997;78(2):193–198. doi: 10.1016/s0003-9993(97)90263-x. [DOI] [PubMed] [Google Scholar]
- 8.Curl DD. Head/neck pain: the need to identify the patient with acute vs. chronic pain. Chiropractic Technique. 1989;1(3):101–105. [Google Scholar]
- 9.Radford W. The development of posture support devices. Dig Chiro Econ. 1987;4:81. [Google Scholar]
- 10.Summer J. Pillows and posture. Dig Chiro Econ. 1990;2:70–73. [Google Scholar]
- 11.Hyland JK. Postural cervical support. Dig Chiro Econ. 1993;2:30–31. [Google Scholar]
- 12.Hamilton RA. Recliner chairs and the cervical spine. Dig Chiro Econ. 1989;2:68–70. [Google Scholar]
- 13.Stierwalt DD. Five-year follow-up study on waterbed effect on backaches and stiffness. Dig Chiro Econ. 1987;5:70–71. [Google Scholar]
- 14.Huston GJ. Everyday aids and appliances, collars and corsets. BMJ. 1988;296(6617):276. doi: 10.1136/bmj.296.6617.276. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Chiropractix: New orthopaedic pillow offers unprecedented adjustability. The American Chiropractor. 1990; 45–46.
- 16.Hinwood JA, Richardson P. Architecture of the cervical spine: measurement of certain characteristics. Chiro J Aust. 1991;2(2):47–52. [Google Scholar]
- 17.Warwick R, Williams PL. (eds) Gray’s anatomy, 35th ed, London: Longman, 1973: 284.
- 18.Leach RA. An evaluation of the effect of chiropractic manipulative therapy on hypolordosis of the cervical spine. JMPT. 1983;6(1):17–23. [PubMed] [Google Scholar]
- 19.Smythe HA. The C6–7 syndrome: Clinical features and treatment response. J Rheumatol. 1994;21(8):1520–1526. [PubMed] [Google Scholar]
- 20.Jackson R. The Cervical Syndrome. 4th ed IL: Charles C, 1987.
- 21.Hagino C, Boscariol J, Dover L, Letendre R, Wicks M. Before/after study to determine the effectiveness of the Aligh-Right cylindrical pillow in reducing chronic neck pain severity. JMPT. 1998;21(2):89–93. [PubMed] [Google Scholar]
- 22.Persson L, Moritz U. Neck support pillows: A comparative study. JMPT. 1998;21(4):237–240. [PubMed] [Google Scholar]
- 23.Hyland JK. Cervical support pillows: useless or helpful? Canadian Chiropractic. 1999;2(3):54–56. [Google Scholar]
- 24.Palazzi C, Miralles R, Miranda C, Valenzuela S, Casassus R, Santander H, et al. Effects of two types of pillows on bilateral sternocleidomastoid EMG activity in healthy subjects and in patients with myogenic cranio-cervical-mandibular dysfunction. Cranio. 1999;17(3):202–212. doi: 10.1080/08869634.1999.11746096. [DOI] [PubMed] [Google Scholar]
- 25.Santander H, Miralles R, Perez J, Valenzuela S, Ravera MJ, Ormeno G, et al. Effects of head and neck inclination on bilateral sternocleidomastoid EMG activity in healthy subjects and in patients with myogenic cranio-cervial-mandibular dysfunction. Cranio. 2000;18(3):181–191. doi: 10.1080/08869634.2000.11746131. [DOI] [PubMed] [Google Scholar]
- 26.Vernon H, Steiman I, Hagino C. Cervicogenic dysfunction in muscle contraction headache and migraine: a descriptive study. JMPT. 1992;15(7):418–429. [PubMed] [Google Scholar]
- 27.Jensen MP, Karoly P, Braver S. The measurement of clinical pain intensity: a comparison of six methods. Pain. 1986;27(1):117–126. doi: 10.1016/0304-3959(86)90228-9. [DOI] [PubMed] [Google Scholar]
- 28.Vernon H, Mior S. The Neck Disability Index: a study of reliability and validity. JMPT. 1991;14(7):409–415. [PubMed] [Google Scholar]
- 29.Tait RC, Pollard CA, Margolis RB, Duckro PN, Krause SJ. The Pain Disability Index: psychometric and validity data. Arch Phys Med Rehabil. 1987;68(7):438–441. [PubMed] [Google Scholar]
- 30.Tibbles AC, Waalen JK, Hains F. Response set bias, internal consistency and construct validity of the Oswestry Low Back Pain Disability Questionnaire. JCCA. 1998;42(3):141–149. [Google Scholar]
- 31.Muchly JW. Significance test for sphericity of a normal n-variate distribution. Annals of Mathematical Statistics. 1940;11:204–209. [Google Scholar]
- 32.Girden ER. ANOVA Repeated Measures. Thousand Oaks, CA: Sage Publications 1992. Quantitative Applications in the Social Sciences series no. 84.