Abstract
Recent papers, including a review conducted by van Tulder et al., have suggested that there is paucity of information as to the efficacy of acupuncture treatment. However, there has been a significant increase in the use of acupuncture therapy for treatment of various ailments, including lower back pain. Chiropractors, along with other health care professionals, are using acupuncture as an adjunct to their main therapeutic intervention as demonstrated by a recent survey by the Canadian Chiropractic Protective Association (CCPA). However, like many other interventions, including NSAIDs and spinal manipulations, signs of side effects should be monitored when acupuncture treatments are considered. Recent papers have noted such complications as pneumothorax and hepatitis following acupuncture treatments. A case is presented in which a patient, who received previous acupuncture treatments, presented to a chiropractic clinic complaining of low back and leg pain. Early recognition of potential complications after acupuncture treatment may minimize significant impairments and disability.
Keywords: chiropractic, low back pain, discitis, infection, acupuncture
Abstract
Des travaux récents, dont une étude menée par van Tulder et al., donnent à penser qu'il existe une pénurie d’information en ce qui concerne les traitements d’acupuncture. Cependant, on assiste à une hausse marquée de l’usage de l’acupuncture dans le traitement de différents malaises, y compris les douleurs lombaires. Selon un sondage effectué dernièrement par l’Association de protection chiropratique canadienne (APCC), les chiropraticiens ainsi que les autres professionnels de la santé utilisent l’acupuncture en guise de traitement d’appoint à leur intervention thérapeutique principale. Cependant, comme dans le cas de beaucoup d’autres interventions, dont l’utilisation des AINS et les manipulations vertébrales, les signes d’effets secondaires doivent être surveillés lorsque des traitements d’acupuncture sont envisagés. Des documents récents ont noté que des complications telles que le pneumothorax et l’hépatite sont survenues après des traitements d’acupuncture. Dans le cas exposé, un patient qui a déjà reçu des traitements d’acupuncture s’est présenté à une clinique de chiropratique en se plaignant de douleurs dans la région lombaire et dans les jambes. Il est possible de minimiser les risques de déficience et de handicap en détectant au plus tôt les complications potentielles à la suite d’un traitement d’acupuncture.
Case report
A 50-year-old male presented to a chiropractic clinic complaining of lower back and right leg pain after lifting a heavy box. He stated that this pain started approximately six weeks ago and had been steady since the onset. He also reported experiencing some coldness in his right foot.
Initially, he attended and was examined in the emergency department at a local hospital. He stated that initial x-rays were taken, but due to the lack of any significant objective findings, he was discharged with analgesics. He received on-going physiotherapy and more recently started to receive needle acupuncture treatments from a ‘traditionally-trained’ acupuncturist. He was also taking NSAIDs for seven to eight weeks with equivocal result. Approximately two weeks prior to presenting to the chiropractic clinic, the patient reported receiving a longer than usual acupuncture needle, placed in his lower back region. He started to experience more discomfort in the last 2 days, and although he found resting in a supine position to be somewhat relieving, he would awake several times during the night, due to lower back discomfort.
On his presentation to the chiropractic clinic, he complained of significant pain localized to the lumbosacral region. He walked in with a cane. The active lumbar range of motion was significantly limited in all directions by lower back and right leg pain. Neurological examination of the lower limbs demonstrated diminished sensation along the right lateral calf, to the dorsum of the foot. Supine straight leg raise was limited to 50° on the right by leg pain, while left was limited to 60° by right-sided lower back and leg pain. Passive hip mobility was symmetrical, although it was associated with lower back pain. He denied having any bowel or bladder dysfunction, or weight loss, but did feel that he had localized sweating over the lumbosacral region. He attributed the sweating to the heat pad he was using to alleviate his lower back pain. Walking aggravated the pain in the lower back and he also felt more pain and weakness in the right leg. He did not complain of any other constitutional symptoms and reported that he was in good general health prior to this episode.
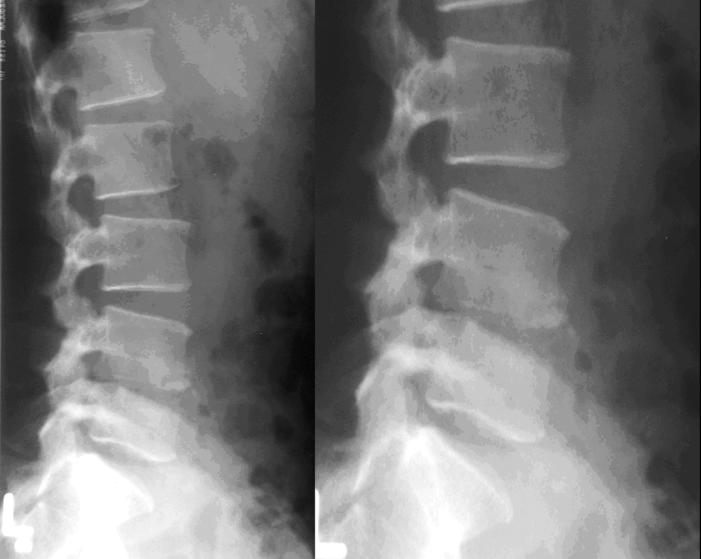
A tentative diagnosis of L5 radiculopathy was made, but the offending structure or mechanism affecting this peripheral nerve was not clear. Due to the severity and duration of the symptoms and the history of failed conservative treatments, x-rays were ordered. Moderate disc narrowing at L4–5 is associated with significant bony erosion and destruction of the upper third of the L5 vertebral body and inferior endplate of L4 (Figure 1). The findings are consistent with infectious spondylodiscitis at L4–5. After reviewing the radiographs, the patient was referred to an emergency department. He subsequently received intravenous antibiotic therapy. Laboratory tests identified staphylococcus to be the offending organism. The patient responded favorably to the antibiotic therapy and did not require surgical intervention.
Figure 1.
Lateral and close-up lateral lumbar radiographs show moderate disc narrowing at L4–5 with significant bony erosion and destruction of the upper third of the L5 vertebral body and inferior endplate of L4. These findings are consistent with spondylodiscitis at L4–5.
Discussion
Although spinal infections are not as common since the development of antibiotic therapy, individuals with conditions such as diabetes, drug addictions, alcoholics and others with depressed immune function may be more susceptible to an infective process.1–4 A recent study estimated the incident rate of septic discitis at two busy district general hospitals, over two and a half years to be 2/100,000/year.5 It was more common in the older population, and in this subgroup, fever may or may not be present in all cases. The most common predisposing factor was invasive procedures, followed by underlying cancer and diabetes.
The most frequent organism for spinal infection is staphylococcus aureus, a common organism present in the epidermis of the skin and in respiratory tract. In acute hematogenous osteomyelits, the gram-positive staphylococcus aureus affects 75–80% of the patients.6 There are four mechanisms by which infection can gain access into the body;4
hematogenous spread (most common)
spread from the contiguous site of infection
direct implantation of organism (nail, acupuncture, etc.)
post operative
The most likely route of this patient’s spinal infection is via hematogenous spread by blood vessel, either arterial or venous. Due to the anastomosing veins and arteries of the lumbar musclature and vertebrae, organisms can be transported to any part of the osseous structures where small capillaries favor their seeding. The anterior subchondral region of the vertebral body is a common location where organisms can get lodged frequently.7 Once seeded, they cause osseous destruction of the vertebral body with extension into the adjacent disc. Rapid destruction of the disc and vertebral body is highly suggestive of an infectious process. If the infection is left unchecked, it will spread across the disc, which may lead to the destruction of the adjacent vertebra. The end result is an angular deformity and possible neurological compression.
Spinal infection is readily differentiated from degenerative disc disease (intervertebral osteochondrosis), in that degenerative disc disease manifests as disc space narrowing with osteophytosis and reactive sclerosis of the end-plates, while infection will cause endplate destruction. Furthermore, sclerosis of the endplates caused by the degenerative disc disease is usually smooth and well defined. The vacuum phenomenon, which is associated with degenerative disc disease, is exceedingly rare in infection.7
Early detection of spinal infection may be difficult using plain film radiographs, as there may be a latent period before any radiographic changes of spondylodiscitis are evident. On plain films, up to 21 days may pass, after the development of back pain before any radiographic changes are observed. Therefore, in cases with clinical suspicion of discitis, (such as unexplained fever, malaise or other constitutional symptoms in patients with immunocompromising conditions), a bone scan, such as Gallium-67 or an MRI would be the diagnostic imaging of choice, since they may detect spondylodiscitis as early as 48 hours after inoculation.
Norheim reported on the adverse effects of acupuncture in the study of the literature between 1981–1994.3 A total of 193 adverse reactions were reported over 14 years. The most common adverse reaction of mechanical organ injury was pneumothorax, while hepatitis was the most common infection. Cases of endocarditis, thrombophlebitis, thrombosed pseudoaneurysm, medulla spinalis injury, psoas abscess and staphylococcal sepsis as well as HIV, are a few of the complications, which have been reported. The author felt that in cases of infection arising from acupuncture treatments, the most likely factor is related to use of non-sterile needles and other possible hygienic problems. However, the author also concluded that acupuncture treatment, cannot be considered to be a therapy without adverse effects. Other cases of spinal infection following acupuncture treatment have been reported.8–11
In summary, a case is reported to outline an uncommon form of lower back pain, potentially caused by direct inoculation of the staphylococcus organism following an acupuncture treatment. The patient presented clinically with L5 radiculopathy, but further imaging revealed characteristic changes of spondylodiscitis. The patient did not have any other systemic infections, direct trauma or fevers to explain a source of infection other than acupuncture treatments.
The patient was immediately referred to the emergency department, where he received intravenous antibiotic therapy, without surgical intervention. This was considered as a “favourable outcome”. Although the type of antibiotic therapy is beyond the scope of this paper, it should be noted that a typical course of antibiotic therapy in spinal infection is about 8–12 weeks.12 If this fails to control the infection, surgical intervention becomes the next step in controlling the process Typically, surgical procedure may include drainage, debridement, irrigation and appropriate parenteral antibiotic therapy.13 Thus, early detection and appropriate referral for discitis is paramount in order to minimize potential complications and disability.
Although the effectiveness of acupuncture in the treatment of low back pain is still uncertain,14 it has nevertheless gained greater acceptance and is currently being used by a number of different health care professionals, including chiropractors. A recent survey conducted by the Canadian Chiropractic Protective Association in 1997 identified that out of the 2000+ respondents, more than 10% reported using acupuncture as an adjunctive therapy, making it one of the more commonly used modalities.15 Increased utilization of this alternative therapy may be related to the potential complications associated with other, more allopathic interventions, typically used to treat mechanical low back pain. For example, NSAIDs, has a potential complication rate of 0.8–1.6% risk of hospitalization due to peptic ulcer complications.16
Recent studies have outlined a number of different potential complications associated with acupuncture therapy.1–3,5,8–11 Even though the rate of serious adverse effects is low,11 it would be prudent for any health care provider using such a modality to discuss risk/benefit factors with the patient prior to recommending this intervention. It would seem reasonable to consider such potential adverse effects from acupuncture treatments, particularly with respect to infection, since even in the most sterile conditions of an operating arena, the risk of post-operative infection is 1–2%. A recent survey found post instrumentation infection rate to be 1.9%.13
Summary
A case is presented in which a patient developed lumbar radiculopathy after receiving a course of acupuncture treatment. Although a definitive causal relationship was not established, there were no other systemic infections or other events, which could explain such an infective process in an otherwise healthy individual.
Individuals presenting to a chiropractic clinic with a history of unrelenting pain with or without fever, increased ESR and conditions compromising the immune system should have diagnostic imaging to rule out a septic etiology, particularly if they have recently received acupuncture treatment. In such cases, early detection and appropriate management is critical since discitis in adults can lead to significant destruction of tissues and morbidity.
References
- 1.Ha KY, Kim YH. Chronic inflammatory granuloma mimics clinical manifestations of lumbar spinal stenosis after acupuncture: a case report. Spine. 2003;28(11):E217–E220. doi: 10.1097/01.BRS.0000067278.67428.40. [DOI] [PubMed] [Google Scholar]
- 2.Rampes H, James R. Complications of acupuncture. Acup Med. 1995;13:26–33. [Google Scholar]
- 3.Norheim AJ. Adverse effects of acupuncture: A study of the literature for the years 1981–1994. J Altern Complement Med. 1996;2:291–7. doi: 10.1089/acm.1996.2.291. [DOI] [PubMed] [Google Scholar]
- 4.Yochum TR, Rowe LJ. Essentials of skeletal radiology. Baltimore, Williams & Wilkins, 1987, 921–960.
- 5.Hopkinson N, Stevenson J, Benjamin S. A case ascertainment study of septic discitis: clinical, microbiological and radiological features. QJ Med. 2001;94:465–470. doi: 10.1093/qjmed/94.9.465. [DOI] [PubMed] [Google Scholar]
- 6.The Merck Manual 14th Edition. West Point, Merck Sharp & Dohme Research Laboratories, 1982, 76–78.
- 7.Resnick D, Niwayama G. Diagnosis of bone and joint disorders. 2nd Ed. Philadelphia, WB Saunders, 1981, 2135–2141.
- 8.Lau SM, Chou CT, Huang CM. Unilateral sacroilitis as an unusual complication of acupuncture. Clin Rheumatol. 1998;17:357–358. doi: 10.1007/BF01451023. [DOI] [PubMed] [Google Scholar]
- 9.Hadden WA, Swanson AJ. Spinal infection caused by acupuncture mimicking a prolapsed intervertebral disc: a case report. J Bone Joint Surg Am. 1982;64:624–626. [PubMed] [Google Scholar]
- 10.Ernst E, White A. Life-threatening adverse reactions after acupuncture? A systematic review. Pain. 1997;71:123–126. doi: 10.1016/s0304-3959(97)03368-x. [DOI] [PubMed] [Google Scholar]
- 11.White A, Hayhoe S, Hart A, Ernst E. Adverse events following acupuncture: prospective survey of 32 000 consultations with doctors and physiotherapists. BMJ. 2001;323:485–486. doi: 10.1136/bmj.323.7311.485. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.The Merck Manual 14th Edition. West Point, Merck Sharp & Dohme Research Laboratories, 1982, 1245–1247.
- 13.Naderi S, Acar F, Mertol T. Is spinal instrumentation a risk factor for late-onset infection in cases of distant infection or surgery? Neurosurg Focus. 2003;15(3):1–3. doi: 10.3171/foc.2003.15.3.15. [DOI] [PubMed] [Google Scholar]
- 14.van Tulder MW, Cherkin DC, Berman B, Lao L, Koes BW. The effectiveness of acupuncture in the management of acute and chronic low back pain. (cochrane review) Spine. 1999;24(11):1113–1123. doi: 10.1097/00007632-199906010-00011. [DOI] [PubMed] [Google Scholar]
- 15.CCPA communication/Canadian chiropractic resources databank 1997. (Ms. Hussein).
- 16.Garcia Rodriguez LA, Walker AM, Perez Gutthann S. Nonsteroidal antiinflammatory drugs and gastrointestinal hospitalization in Saskatchewan: a cohort study. Epidemiology. 1992;3:337–342. doi: 10.1097/00001648-199207000-00008. [DOI] [PubMed] [Google Scholar]