SYNOPSIS
Objectives.
Studies continue to document that people with human immunodeficiency virus (HIV) experience discrimination in their interactions with the health-care system, which can have negative implications for maintaining continuity in care and outcomes. We explored the patient characteristics associated with perceived discrimination and whether these experiences are associated with health-care system quality ratings in a survey of severely disadvantaged people with HIV who are at great risk of inconsistent access to appropriate health care.
Methods.
Five hundred and twenty-three participants were recruited from temporary housing facilities for people with HIV in the New York City area and administered a survey using audio computer-assisted self-interviewing technology.
Results.
Of the 207 participants (39.6%) who reported experiencing discrimination in the health-care system, the most common attributions were HIV infection (n=122, 59.8%), drug use (n=100, 49.8%), homelessness (n=71, 34.6%), and race/ethnicity (n=69, 35.2%). Length of time HIV infected, use of non-prescription opioids, white race, higher education, female gender, younger age, and poorer self-reported health status were all significantly associated with greater odds of perceived discrimination. After adjusting for participant characteristics, perceived discrimination was significantly associated with poorer participant ratings of quality of health care.
Conclusions.
Members of this vulnerable population commonly report experiences of discrimination from within the health-care system and these experiences are associated with poor health-care ratings. These findings support the need for closer examination of the adequacy of cultural competency training within the HIV health-care delivery system to improve access to appropriate care for disadvantaged people.
Studies continue to document that people with human immunodeficiency virus (HIV) report experiences of discrimination in their interactions within the health-care system.1–3 Personal experiences of discrimination as well as the expectation of discrimination can inhibit people from disclosing HIV risk behaviors to their health-care providers and from maintaining consistent contact with the HIV service system.2,4,5 Thus, people affected by discrimination may be less likely to have access to the recent HIV treatment advances that can prolong life and greatly improve quality of life. To eliminate disparities in the quality of and access to health care for people with HIV, it is important to understand the nature, sources, and consequences of perceived discrimination within the health-care system.
A recent study documented patterns of perceived discrimination and its correlates in a nationally representative sample of people receiving care for HIV across the U.S.1 In this study, 26% reported experiencing some form of discrimination from within the health-care system, which had a significant impact on patients' ratings of health-care quality.1 These data reinforce the need to reevaluate the medical-care delivery system for people with HIV/acquired immunodeficiency syndrome (AIDS). However, it is important to remember that HIV disproportionately affects populations that are at great risk of receiving inconsistent health care even though they frequently have substantial health and social service needs,6–14 such as racial/ethnicity minorities,15,16 sexual minorities,15 drug users, people with recent interactions with the criminal justice system,17 and people with unstable housing situations.8,9 Despite numerous large-scale efforts by the health policy makers and providers to engage and retain this population in care,18 significant barriers to accessing appropriate long-term integrated care exist. To further reduce these barriers, it is important to understand the predictors of perceived discrimination and its potential impact on patient ratings of the quality of health-care delivery systems available for these vulnerable populations.
This study examined perceived discrimination in a sample of predominantly black and Latino people who are living in temporary emergency housing for people with HIV in New York City. This population typically includes a significant proportion of people who have co-morbid drug, alcohol, and/or psychiatric conditions, and typically have inconsistent patterns of health-care utilization.19 Because this population is traditionally difficult to engage in both research and health care, it is often underrepresented in study samples. The objectives of this study were to examine (1) the frequency, attributions, and sources of perceived discrimination from within the health-care system; (2) participant characteristics associated with perceived discrimination from within the health-care system in this severely disadvantaged population; and (3)associations between perceived discrimination and ratings of the HIV care system.
METHODS
Participants
Participants for this study were recruited from individuals living in single-room occupancy (SRO) hotels in the Bronx and Manhattan that function as transitional emergency housing facilities for homeless people with HIV/AIDS in these areas. We targeted the 14 hotels that are served by the Montefiore/CitiWide collaborative medical outreach program. Eligibility criteria included HIV infection, at least 18 years old, English- or Spanish-speaking, and willing to give informed consent. HIV status was confirmed during the interview and by medical records. Residents who were acutely intoxicated were not eligible. The Institutional Review Boards at Montefiore Medical Center and the Centers for Disease Control and Prevention approved this study.
Two research interviewers knocked on every door in the target SRO hotels and invited eligible residents to participate. The interviewers returned to each hotel on at least three consecutive days to invite participation from as many hotel residents as possible. Interested residents were informed about the study procedures and administered written informed consent. They were also asked to sign consent to release medical information from their primary HIV health-care provider (if they had one). Participants received a $15 honorarium for their time. A total of 611 people were approached for the study, 533 (87%) agreed to participate, and 524 (86%) completed the interview.
Data collection
Interviews were administered through audio computer-assisted self-interviewing (ACASI) technology in the participants' SRO hotel rooms. This method allows for direct entry of data into the computer by the study participants and may result in participants' reporting higher rates of sensitive behavior than from other survey methods.20 While most participants were willing and able to complete the interviews using ACASI technology, 57 participants (10.9% of the final sample) requested assistance from interviewers. The interview took approximately 45 minutes to complete. The ACASI interview was comprised of a series of questions taken from standardized questionnaires.
We obtained medical charts when possible from participants who reported having a regular provider for their HIV. A physician reviewed charts using a standardized chart extraction form. Data used in the present analysis include whether or not the participant had at least one ambulatory care visit noted in the chart in the past six months.
Perceived discrimination was measured by asking participants if someone in the health-care system ever exhibited hostility or lack of respect toward them, ever paid less attention to them compared to others, or ever refused them service.1 Participants who responded positively to any of these questions were considered to have experienced discrimination. Those who experienced any of these forms of discrimination were then asked what they believe was the reason for the discrimination. Response categories included their HIV infection, gender, sexual orientation, race/ethnicity, drug use, homelessness, or physical appearance. Finally, those who experienced discrimination were asked to identify who was responsible for the discrimination. Response categories included a health-care provider, nurse or other medical support staff, nonmedical staff, and other.
Three measures of participant ratings of quality of the HIV care system and their provider were used, including perceived access to health care, mistrust in the HIV health-care system, and trust in the HIV provider. All three measures were derived from scales that have been previously applied in research in similar populations and/or have established psychometric properties.21–23 Access to health care consists of six items rated on a five-point Likert scale, including items related to ease of hospital admission, access to emergency care, access to specialists, location of services, and cost of care.21 Mistrust in the health-care system was measured by seven items developed by Altice, Mostashari, and Friedland.22 Statements regarding issues of mistrust related to hospitals, scientists, and the pharmaceutical industry were rated using a five-point Likert scale. Trust in one's provider was measured by seven items from the Primary Care Assessment Survey.23 Items included: I can tell my provider anything; my provider pretends to know things when s/he is not really sure; I completely trust my provider's judgments; my provider cares more about hold-down costs than doing what is needed for my health; my provider would always tell me the truth; my provider cares as much as I do about my health; and my provider would hide a mistake in my treatment from me.
To derive summary measures for our analyses, we calculated the mean ratings across all items completed by the participant on each scale. For each scale, participants were included in analyses if they responded to four or more items on the scale. In supplemental analyses we included only participants who responded to all items on a scale, and the main results were essentially the same (data not shown). Following Schuster et al.1 we converted all three scales to a range of 0 to 100.
Covariates included in these analyses included participants' sociodemographic characteristics (age, gender, race/ethnicity, primary language [English or Spanish], education, and insurance status), perceived current homelessness status (yes or no), length of time living in the SRO system, self-reported health status (excellent, very good, or good vs. fair or poor), length of time infected with HIV, current drug use (nonprescription opioid or cocaine use in the past 30 days from the Addiction Severity Index),24 current problem alcohol use (reported drinking alcohol “to black out” in the past 30 days), and whether or not the participant had a regular provider for his HIV care. Also included was one variable derived from medical records: whether or not the participant had at least one ambulatory visit with his/her provider in the past six months.
Data analysis
Analyses were conducted in two steps. We first reported prevalence estimates for overall perceived discrimination and type of perceived discrimination (exhibited hostility or lack of respect, less attention, or refusal of services), attribution for discrimination (HIV infection, gender, sexual orientation, race/ethnicity, drug use, homelessness, or physical appearance), and source of discrimination (health-care provider, nurse or other medical support staff, or nonmedical staff). We then explored whether covariates listed previously are associated with perceived discrimination (yes or no) using chi-square statistics, and conducted multivariable analyses using logistic regression to identify covariates that were independently associated with perceived discrimination.
In the second step of this analysis, we tested whether perceived discrimination was associated with participant ratings of the health-care system by comparing mean scale scores for each measure (access to care, mistrust in the health-care system, and trust in the provider) for those who reported discrimination with those who reported no discrimination. We conducted linear regression analyses to test whether perceived discrimination was associated with each rating of the health-care system after adjusting for potential confounders. Variables were selected for inclusion in multivariable models if they were associated with any of these three health-care quality ratings at p<0.20 in bivariate analyses.25 Outcome measures for this analysis were approximately normally distributed, and therefore were untransformed in regression models. Unstandardized regression coefficients associated with discrimination were reported.
We additionally conducted post hoc analyses to determine whether type of discrimination (hostility or lack of respect, less attention, or refusal of services) was associated with each outcome (access, mistrust in system, and trust in provider). For these analyses, we conducted linear regression analyses as described previously, except we entered dichotomous variables representing each of the three specific types of discrimination simultaneously into the model rather than the overall discrimination variable. We also evaluated whether the number of types of discrimination (ranging from one to all three types measured) was associated with each outcome.
RESULTS
One participant was dropped from this analysis because we could not determine whether s/he had ever experienced discrimination from her/his responses (s/he answered “don't know” to whether s/he had experienced two of the three forms of discrimination and responded negatively to whether s/he had experienced the third form). Thus our analysis sample consisted of 523 participants.
The median age of our sample was 45 years. They were predominantly male (n=374, 71.5%), black, or Latino (n=459, 87.8%), and the majority achieved at least a high school education (n=300, 58%). A total of 281 (53.7%) had their first HIV positive test 10 or more years ago. Two hundred forty-four participants (47.1%) considered themselves homeless, and about one-third (n=188, 36.9%) of the participants had been living in the SRO system for more than three years. One hundred eight (21.1%) reported using nonprescription opioids in the past 30 days, 245 (48.7%) reported using cocaine in the past 30 days, and 50 (9.7%) reported using alcohol “to black out” in the past 30 days. Overall, 70 participants (13.4%) reported not having a regular HIV provider. We obtained medical record information for a total of 422 participants (80.7% of the sample), and 154 (34.5% of those with medical records available) had no ambulatory care visits with their primary-care provider in the past six months.
Perceived discrimination: frequency, attributions, and sources
A total of 207 participants (39.6%) reported at least one of the three forms of discrimination in the health-care system: 163 (31.2%) reported someone in the health-care system had ever exhibited hostility or a lack of respect toward him/her; 158 participants (30.2%) reported that someone in the health-care system had ever paid less attention to him/her; and 84 participants (16.1%) reported that someone in the health-care system had ever refused him/her service. Together, 63 participants (12%) reported one type of discrimination, 90 (17.2%) reported two types, and 54 (10.3%) reported three types.
Participants who experienced discrimination were asked why they thought they were discriminated against. The most common reasons included: HIV infection (n=122, 59.8%), drug use (n=100, 49.8%), homelessness (n=71, 34.6%), and race/ethnicity (n=69, 35.2%). Fewer reported sexual orientation and gender as reasons for discrimination. Several participants reported more than one of these attributions for discrimination experiences (n=125).
Among those who experienced discrimination and were able to report a source of discrimination (n=131), 61 participants (46.6%) reported discrimination by a health-care provider and 103 participants (78.6%) reported discrimination by a nonprovider. Among those reporting discrimination by a nonprovider, 71 participants (68.9%) reported a nurse or other medical support staff as the source and 59 people (57.3%) reported nonmedical support staff as the source.
Participant characteristics associated with perceived discrimination
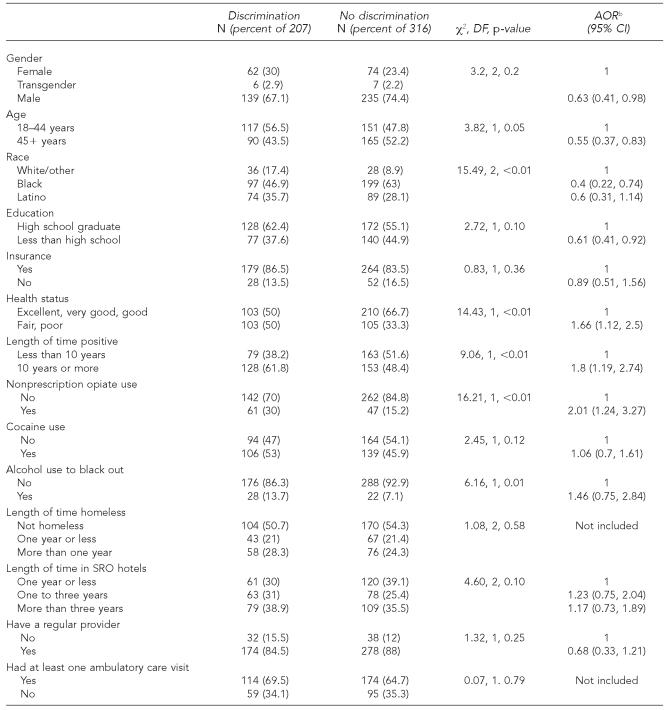
A number of participant characteristics were associated with perceived discrimination (Table 1). An experience with discrimination in the health-care system was associated with female gender, younger age, white race/ethnicity, high school education, longer time since first testing HIV positive, worse self-reported health status, and nonprescription opioid use in multivariable analyses.
Table 1.
Sociodemographic and clinical characteristics associated with discrimination in a sample of unstably housed people with HIV in New York Citya
Numbers reported in this table reflect the few missing data points on this item.
AOR are estimated in logistic regression models that included all variables listed in the table except length of time homeless, as this variable is correlated with length of time in SRO and had at least one ambulatory visit and because this variable is correlated with having a regular provider.
HIV = human immunodeficiency virus
AOR = adjusted odds ratio
SRO = single-room occupancy
DF = degree of freedom
CI = confidence interval
Ratings of the health-care system associated with perceived discrimination
In this sample, the mean rating on the access-to-care scale (where 0 = lowest access and 100 = best access) among those reporting discrimination was 61.39 (standard deviation [SD] = 22.98) and among those not reporting discrimination was 70.50 (SD=21.51) (t=–4.61, degrees of freedom [DF] = 521, p<0.01). The mean rating on mistrust in the health-care system scale (where 100 = most mistrust and 0 = least mistrust) among those reporting discrimination was 65.00 (SD=24.71) and among those not reporting discrimination was 51.57 (SD=26.19) (t=5.90, DF=520, p<0.01). The mean rating on trust in provider (where 0 = lowest trust and 100 = highest trust) among those reporting discrimination was 63.31 (SD=22.47) and among those not reporting discrimination was 73.33 (SD=20.05) (t=–4.97, DF=376, p<0.01).
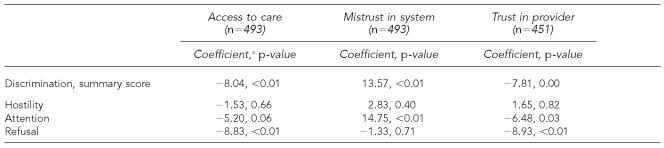
The association between perceived discrimination and these quality-of-care ratings remained statistically significant after adjusting for potential confounders (Table 2). Even though having someone in the health-care system exhibit hostility or a lack of respect was the most common form of perceived discrimination, it was least likely to be independently associated with these health-care quality ratings (Table 2). Having experienced more types of discrimination experiences was statistically significantly associated with poorer access to care and less trust in one's provider (data not shown).
Table 2.
Relationship between perceived discrimination and patient ratings of the health-care system in a sample of unstably housed people with HIV in New York City
Unstandardized regression coefficients are presented. Models include discrimination variables, as well as participant race/ethnicity, education, insurance, current nonprescription opioid use, current cocaine use, current alcohol use to black out, length of time in the single-room-occupancy hotel system, self-reported health status, and having a regular provider for HIV care. The Ns vary because only patients who responded to four or more items on a scale were included in this analysis, and there are a few missing data points on covariates. Additionally, 44 people were excluded from the analysis of trust in provider because, due to a computer error, these participants were not asked to rate items on this scale.
HIV = human immunodeficiency virus
DISCUSSION
In this sample of disadvantaged people with HIV infection residing in New York City, we found that almost 40% reported experiences of perceived discrimination from within the health-care system. This estimate is higher than that reported in a previous study of a nationally representative sample of HIV-infected people in care,1 which might be expected as our sample consists of HIV-infected people who face more severe social and economic disadvantages and have been infected with HIV for longer on average. However, this finding indicates that fear of discrimination from within the health-care system might be a particularly significant barrier to accessing appropriate health care for this population that is at great risk of receiving no or inconsistent HIV care. It underscores the urgent need to identify the components of the health-care system that patients have found to be alienating in our efforts to improve their HIV care.
Participants in our study attributed their experiences of perceived discrimination to a number of factors, particularly HIV status, drug use, homelessness, and race, and were more likely to report discrimination by medical or other support staff than by health-care provider. It is likely that these patterns are reflective of the local health-care and social services systems that serve this population in New York City, as well as the characteristics of the study population. People with HIV often rely on multiple resources to meet their various needs, including services designed for specialty HIV care, substance abuse treatment, and housing and other social service assistance.26,27 Fragmentation in the overall service system for this population can result in poor communication patterns and more impersonal relationships between patients and providers,28 which may foster perceived and/or actual discrimination experiences in any one of these settings.3,29 Establishing integrated care systems may reduce this problem, as providers can develop expertise in serving a heterogeneous patient population and providing a broader range of services, and can develop formal and ongoing relationships with providers in other service sectors.28,30 Additionally, the finding that nonproviders were a significant source of perceived discrimination in this study highlights the fact that all members of the health-care system can influence, both negatively and positively, patient engagement and retention in HIV care.
In our sample, which includes some HIV-infected participants who were not currently receiving HIV care, characteristics that were associated with perceived discrimination were largely consistent with those reported in the previous nationally representative sample of treated HIV patients. We add to the literature on discrimination experiences in this population by additionally exploring whether drug and alcohol use and unstable housing status are associated with greater odds of perceived discrimination. We found that nonprescription opioid use was significantly associated with perceived discrimination and problem alcohol use was associated with elevated odds of perceived discrimination, although this association did not reach statistical significance. Several previous studies have shown that HIV-infected people who are drug or heavy alcohol users are less likely to receive recommended treatment, like antiretroviral medications, than non-substance users.31,32 While there are a number of possible explanations—including various patient-related factors—our findings raise concern that substance abusers may be inappropriately denied life-prolonging treatments.
Evidence that drug users have different treatment patterns and different experiences of discrimination in the health-care system indicates that closer attention must be paid to the way their HIV care is delivered. To avoid patients' negative perceptions of treatment decisions, encourage patient-centered care, and improve patient outcomes, physicians must be adept at developing a strong therapeutic alliance with their HIV-infected patients.33,34 Toward this end, interventions to improve physician skills and knowledge related to successfully managing HIV care among substance-using patients across settings might be needed to improve care patterns for difficult-to-reach populations, like the one on which this study focuses. These findings provide further evidence of the need for truly integrated health care for this population of severely disadvantaged people with HIV.
One initially puzzling finding was that minority race/ethnicity did not consistently predict perceived discrimination. In fact, white participants in this study were more likely to report experiences of discrimination than black or Latino/a participants. While this finding was unexpected, other studies indicate that measures of perceived discrimination that are not specifically related to race can impact whites as well as racial/ethnic minorities.1,34,35 Because the men and women in this study frequently reported membership in multiple disadvantaged groups, their explanations of perceived discrimination might be complex.35 Future research is needed to understand how patients place meaning to their experiences of discrimination and whether their attributions of perceived discrimination predicts different health behaviors or attitudes toward the health-care system.
Participants' ratings of the health-care system and their provider were strongly and consistently negatively associated with our summary measure of perceived discrimination. Because we do not know when participants experienced discrimination, we cannot conclude that having experiences of discrimination caused participants to rate the health-care system poorly. However, it is noteworthy that these measures varied together. At the very least, participants who experienced hostility/lack of respect, less attention compared with others, or service refusal are often the same patients that had greater difficulty achieving adequate access to health care, more mistrust in the HIV care system as a whole, and poorer relationships with their physicians. Furthermore, our post hoc analyses indicated that perception of receiving less attention compared with others might be a particularly strong correlate of lack of trust in both the health-care system and HIV providers in this population. While it would be theoretically interesting to understand directionality, it is clearly important to address patients' feelings of discrimination even before understanding the pathways in these associations.
While “discrimination” is conceptually different from “access to care,” one of the specific items used to measure discrimination—refusal of care—is similar to some of the items we used to rate access to care. However, we note that poorer ratings of access to care were associated with discrimination even when having been refused care was not included in the discrimination scale (data not shown).
This study had other limitations that should be considered when interpreting our results. Our study sample consisted of a convenience sample of men and women who lived in the target SRO hotels during the study period. While great effort was made to approach all residents in these hotels and the study participation rate was high, there are no data available to inform us about the completeness of our sample or the potential influence of selection biases. Second, our study measured perceived discrimination and did not attempt to verify whether or not perceptions of hostility/lack of respect, less attention, or refusal of services actually occurred. Other research might seek to investigate whether similar experiences in the health-care system are differently perceived by patients with different sociodemographic and illness characteristics in order to target interventions and quality improvement efforts for this population. It is uncertain if participants in this study continue to experience discrimination in the health-care system or if the experiences reported occurred largely in the distant past. However, the correlation between discrimination and current health-care quality ratings indicated that efforts must be made to both prevent future experiences and address past experiences in this population.
Finally, although it is troubling that perceived discrimination is associated with poor patient ratings of health-care quality, it is uncertain whether these factors then led to poorer health-care utilization or poor health. We examined two measures of engagement in care in our bivariate analysis—having a regular provider for HIV and having at least one ambulatory visit with a health-care provider in the past six months—and neither was associated with perceived discrimination. We believe that, although discrimination is a strong predictor of health-care ratings, it is only one of many strong barriers to actual engagement with the health-care system, which we could not explore in the present analysis. Further research is needed to understand the contribution of perceived discrimination on other measures of health-care patterns, such as medication adherence and missed appointments, as well as health outcomes of this disadvantaged population.
Despite these limitations, this study sheds light on the potential correlates and impact of perceived discrimination for a sample of disadvantaged men and women with HIV in New York City, many of whom are likely to have multiple health and social services needs. Many reported experiencing discrimination from within the health-care system, and recent drug use, as well as other sociodemographic and health characteristics, was significantly associated with these experiences. Furthermore, perceived discrimination was associated with poorer ratings of quality of the HIV health-care system and trust in HIV providers. These findings support the need for specific improvements in the HIV health-care delivery system for this population, which is at substantial risk for poor health, suboptimal health care, and further transmission of HIV.
Footnotes
This study was supported by the Centers for Disease Control and Prevention, Minority HIV/AIDS Research Initiative (#U65/CCU223363-03), the Center for AIDS Research at the Albert Einstein College of Medicine and Montefiore Medical Center funded by the National Institutes of Health (NIH AI-51519), and the Health Resources and Services Administration, HIV/AIDS Bureau, Special Projects of National Significance (#H97 HA 00247-03). Dr. Cunningham is supported by the Robert Wood Johnson Foundation's Harold Amos Medical Faculty Development Program. Preliminary results from this analysis were presented in part at the 5th International Conference on Urban Health; 2006 Oct 25–28; Amsterdam, the Netherlands.
REFERENCES
- 1.Schuster MA, Collins R, Cunningham WE, Morton SC, Zierler S, Wong M, et al. Perceived discrimination in clinical care in a nationally representative sample of HIV-infected adults receiving health care. J Gen Intern Med. 2005;20:807–13. doi: 10.1111/j.1525-1497.2005.05049.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Bird ST, Bogart LM, Delahanty DL. Health-related correlates of perceived discrimination in HIV care. AIDS Patient Care STDS. 2004;18:19–26. doi: 10.1089/108729104322740884. [DOI] [PubMed] [Google Scholar]
- 3.Bird ST, Bogart LM. Perceived race-based and socioeconomic status (SES)-based discrimination in interactions with health care providers. Ethn Dis. 2001;11:554–63. [PubMed] [Google Scholar]
- 4.Marks G, Mason HR, Simoni JM. The prevalence of patient disclosure of HIV infection to doctors. Am J Public Health. 1995;85:1018–9. doi: 10.2105/ajph.85.7.1018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Jeffe DB, Khan SR, Meredith KL, Schlesinger M, Fraser VJ, Mundy LM. Disclosure of HIV status to medical providers: differences by gender, “race,” and immune function. Public Health Rep. 2000;115:38–45. doi: 10.1093/phr/115.1.38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Mor V, Fleishman JA, Dresser M, Piette J. Variation in health service use among HIV-infected patients. Med Care. 1992;30:17–29. doi: 10.1097/00005650-199201000-00002. [DOI] [PubMed] [Google Scholar]
- 7.Culhane DP, Gollub E, Kuhn R, Shpaner M. The co-occurrence of AIDS and homelessness: results from the integration of administrative databases for AIDS surveillance and public shelter utilisation in Philadelphia. J Epidemiol Community Health. 2001;55:515–20. doi: 10.1136/jech.55.7.515. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Riley ED, Bangsberg DR, Guzman D, Perry S, Moss AR. Antiretroviral therapy, hepatitis C virus, and AIDS mortality among San Francisco's homeless and marginally housed. J Acquir Immune Defic Syndr. 2005;38:191–5. doi: 10.1097/00126334-200502010-00010. [DOI] [PubMed] [Google Scholar]
- 9.Kapadia F, Cook JA, Cohen MH, Sohler N, Kovacs A, Greenblatt RM, et al. The relationship between non-injection drug use behaviors on progression to AIDS and death in a cohort of HIV seropositive women in the era of highly active antiretroviral therapy use. Addiction. 2005;100:990–1002. doi: 10.1111/j.1360-0443.2005.01098.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Shapiro MF, Morton SC, McCaffrey DF, Senterfitt JW, Fleishman JA, Perlman JF, et al. Variations in the care of HIV-infected adults in the United States: results from the HIV Cost and Services Utilization Study. JAMA. 1999;281:2305–15. doi: 10.1001/jama.281.24.2305. [DOI] [PubMed] [Google Scholar]
- 11.Catz SL, McClure JB, Jones GN, Brantley PJ. Predictors of outpatient medical appointment attendance among persons with HIV. AIDS Care. 1999;11:361–73. doi: 10.1080/09540129947983. [DOI] [PubMed] [Google Scholar]
- 12.Kissinger P, Cohen D, Brandon W, Rice J, Morse A, Clark R. Compliance with public sector HIV medical care. J Natl Med Assoc. 1995;87:19–24. [PMC free article] [PubMed] [Google Scholar]
- 13.Israelski D, Gore-Felton C, Power R, Wood MJ, Koopman C. Sociodemographic characteristics associated with medical appointment adherence among HIV-seropositive patients seeking treatment in a county outpatient facility. Prev Med. 2001;33:470–5. doi: 10.1006/pmed.2001.0917. [DOI] [PubMed] [Google Scholar]
- 14.Piette JD, Mor V, Mayer K, Zierler S, Wachtel T. The effects of immune status and race on health service use among people with HIV disease. Am J Public Health. 1993;83:510–4. doi: 10.2105/ajph.83.4.510. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.MacKellar DA, Valleroy LA, Secura GM, Behel S, Bingham T, Celentano DD, et al. Unrecognized HIV infection, risk behaviors, and perceptions of risk among young men who have sex with men: opportunities for advancing HIV prevention in the third decade of HIV/AIDS. J Acquir Immune Defic Syndr. 2005;38:603–14. doi: 10.1097/01.qai.0000141481.48348.7e. [DOI] [PubMed] [Google Scholar]
- 16.Poundstone KE, Strathdee SA, Celentano DD. The social epidemiology of human immunodeficiency virus/acquired immunodeficiency syndrome. Epidemiol Rev. 2004;26:22–35. doi: 10.1093/epirev/mxh005. [DOI] [PubMed] [Google Scholar]
- 17.Blankenship KM, Smoyer AB, Bray SJ, Mattocks K. Black-white disparities in HIV/AIDS: the role of drug policy and the corrections system. J Health Care Poor Underserved. 2005;16(Suppl B):140–56. doi: 10.1353/hpu.2005.0110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Tobias C, Wood S, Drainoni ML. Ryan White CARE Act Title II survey: services for HIV-positive substance users. AIDS Patient Care STDS. 2006;20:205–12. doi: 10.1089/apc.2006.20.205. [DOI] [PubMed] [Google Scholar]
- 19.Cunningham CO, Sohler NL, McCoy K, Heller D, Selwyn PA. Health care access and utilization patterns in unstably housed HIV-infected individuals in New York City. AIDS Patient Care STDS. 2005;19:690–5. doi: 10.1089/apc.2005.19.690. [DOI] [PubMed] [Google Scholar]
- 20.Perlis TE, Des Jarlais DC, Friedman SR, Arasteh K, Turner CF. Audio-computerized self-interviewing versus face-to-face interviewing for research data collection at drug abuse treatment programs. Addiction. 2004;99:885–96. doi: 10.1111/j.1360-0443.2004.00740.x. [DOI] [PubMed] [Google Scholar]
- 21.Cunningham WE, Andersen RM, Katz MH, Stein MD, Turner BJ, Crystal S, et al. The impact of competing subsistence needs and barriers on access to medical care for persons with human immunodeficiency virus receiving care in the United States. Med Care. 1999;37:1270–81. doi: 10.1097/00005650-199912000-00010. [DOI] [PubMed] [Google Scholar]
- 22.Altice FL, Mostashari F, Friedland GH. Trust and the acceptance of and adherence to antiretroviral therapy. J Acquir Immune Defic Syndr. 2001;28:47–58. doi: 10.1097/00042560-200109010-00008. [DOI] [PubMed] [Google Scholar]
- 23.Safran DG, Kosinski M, Tarlov AR, Rogers WH, Taira DH, Lieberman N, et al. The Primary Care Assessment Survey: tests of data quality and measurement performance. Med Care. 1998;36:728–39. doi: 10.1097/00005650-199805000-00012. [DOI] [PubMed] [Google Scholar]
- 24.McLellan AT, Kushner H, Metzger D, Peters R, Smith I, Grissom G, et al. The Fifth Edition of the Addiction Severity Index. J Subst Abuse Treat. 1992;9:199–213. doi: 10.1016/0740-5472(92)90062-s. [DOI] [PubMed] [Google Scholar]
- 25.Tabachnik BG, Fidell LS. 3rd ed. New York: HarperCollins College Publishers; 1996. Using multivariate statistics. [Google Scholar]
- 26.Klinkenberg WD, Sacks S. HIV/AIDS Treatment Adherence, Health Outcomes and Cost Study Group. Mental disorders and drug abuse in persons living with HIV/AIDS. AIDS Care. 2004;16(Suppl 1):S22–42. doi: 10.1080/09540120412331315303. [DOI] [PubMed] [Google Scholar]
- 27.Douaihy AB, Stowell KR, Bui T, Daley D, Salloum I. HIV/AIDS and homelessness, part 2: treatment issues. AIDS Read. 2005;15:604–6. 611-3, 618. [PubMed] [Google Scholar]
- 28.Jacobs JL, Damson LC, Rogers DE. One approach to care for patients infected with human immunodeficiency virus in an academic medical center. Bull N Y Acad Med. 1996;73:301–13. [PMC free article] [PubMed] [Google Scholar]
- 29.Piette JD, Bibbins-Domingo K, Schillinger D. Health care discrimination, processes of care, and diabetes patients' health status. Patient Educ Couns. 2006;60:41–8. doi: 10.1016/j.pec.2004.12.001. [DOI] [PubMed] [Google Scholar]
- 30.Weiner SJ, Barnet B, Cheng TL, Daaleman TP. Processes for effective communication in primary care. Ann Intern Med. 2005;142:709–14. doi: 10.7326/0003-4819-142-8-200504190-00039. [DOI] [PubMed] [Google Scholar]
- 31.Turner BJ, Fleishman JA, Wenger N, London AS, Burnam MA, Shapiro MF, et al. Effects of drug abuse and mental disorders on use and type of antiretroviral therapy in HIV-infected persons. J Gen Intern Med. 2001;16:625–33. doi: 10.1046/j.1525-1497.2001.016009625.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Tucker JS, Orlando M, Burnam MA, Sherbourne CD, Kung FY, Gifford AL. Psychosocial mediators of antiretroviral nonadherence in HIV-positive adults with substance use and mental health problems. Health Psychol. 2004;23:363–70. doi: 10.1037/0278-6133.23.4.363. [DOI] [PubMed] [Google Scholar]
- 33.Knowlton A, Arnsten J, Eldred L, Wilkinson J, Gourevitch M, Shade S, et al. Individual, interpersonal, and structural correlates of effective HAART use among urban active injection drug users. J Acquir Immune Defic Syndr. 2006;41:486–92. doi: 10.1097/01.qai.0000186392.26334.e3. [DOI] [PubMed] [Google Scholar]
- 34.Noring S, Dubler NN, Birkhead G, Agins B. A new paradigm for HIV care: ethical and clinical considerations. Am J Public Health. 2001;91:690–4. doi: 10.2105/ajph.91.5.690. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.LaVeist TA, Rolley NC, Diala C. Prevalence and patterns of discrimination among U.S. health care consumers. Int J Health Serv. 2003;33:331–44. doi: 10.2190/TCAC-P90F-ATM5-B5U0. [DOI] [PubMed] [Google Scholar]