SYNOPSIS
Objective.
This study examines race variations in quality of care through the proxy of ambulatory care sensitive (ACS) conditions. Hospital admission rates for eight ACS conditions were examined for African American and white Medicare beneficiaries in North Carolina. Temporal variations for ACS were also examined.
Method.
Enrollment and inpatient claims files from the Centers for Medicare and Medicaid Services (CMS) for a 1999–2002 cohort who were aged 65 years or older in 1999 were examined. Descriptive statistics were computed for each year. Cochran-Mantel Haenszel tests were performed to assess differences in the admission rates for both individual and aggregate ACS conditions controlling for time. The Cochran-Armitage test for trend was used to evaluate changes in admission rates over time.
Results.
African Americans had higher admission rates for five of the eight ACS conditions. The highest rates were for diabetes among African Americans (odds ratio [OR]=2.86; 95% confidence interval [CI] [2.73, 2.99]) and adult asthma (OR=1.51; 95% CI [1.43, 1.61]). African Americans tended to have lower ACS admission rates than white patients for chronic obstructive pulmonary disease (OR=0.67; 95% CI [0.65, 0.69]); bacterial pneumonia (OR=0.86; 95% CI [0.84, 0.89]), and angina (OR=0.90; 95% CI [0.84, 0.97]).
Conclusions.
Using the ACS proxy for quality of health care as applied to examining race and ethnicity is a promising approach, though challenges remain. Admissions for ACS conditions between African American and white patients differ, but it is unclear why. This exploratory study must lead to an examination of social, economic, historical, and cultural factors for preventive, remedial, and beneficial policy initiatives.
The health disadvantages experienced by African Americans in the United States have been recognized since vital records were first collected early in this century. African Americans are more likely to require health care but are less likely to receive health-care services.1,2 Recent studies have suggested that even when African Americans gain access to the health-care system, they are less likely than white patients to receive high-quality treatment.3–8 Despite well-documented research detailing a lack of appropriate medical care among African Americans, there is a paucity of knowledge regarding the measurement of quality of care for this population.2 In addition, ongoing surveillance is necessary to determine changes in these patterns of care over time.
The occurrence of sentinel health events—later called ambulatory care sensitive (ACS) conditions—which are diseases, disabilities, and deaths that are deemed potentially avoidable through prevention or through appropriate treatment, can provide a basis for an assessment of quality.9 This occurrence can signal failures in public health and medical care and point to social factors and personal behavior that, if altered, could lead to better health of the population. This occurrence can also trigger both the investigations of underlying causes and the search for corrective actions and can serve as indicators of potentially unmet needs for services. The value of negative indicators of health-care utilization in signaling possible problems in health-care delivery and quality of care has long been established; maternal mortality and infant mortality rates are good examples.10 Neither of these indicators, however, applies to broad segments of the population and to the broad spectrum of circumstances that influences people's health.
Two lists (single-case indexes and indexes based on rates) of medical conditions for which either the occurrence of a particular condition or a death from a particular condition may be considered avoidable, called sentinel health events, were developed in the mid–1970s and updated in 1980.9 These lists were composed of single-case and rate-based indices. Single-case indexes contain about 100 medical conditions in which, for most conditions, the disease itself is so clearly avoidable that even one case of disease, disability, or death is sentinel. Examples of these events include cases of botulism and disabling congenital rubella syndrome and death from cancer of the cervix. The single-case indexes also include five surgical procedures from which no death should result.
Indexes based on rates are 23 conditions such as vascular complications of the heart or brain associated with hypertensive diseases, in which a rate of occurrence of deaths or diseases above an acceptable level or threshold requires investigation. This list also includes five surgical procedures for which no death should result. This list of sentinel events encompasses conditions such as ruptured appendix or diphtheria and tetanus that should never be found in a well-functioning health-care system.
In the 1990s, Billings et al. (1993) described a pattern of ACS conditions by using the principal diagnosis codes from the International Classification of Diseases, 9th Revision, Clinical Modification (ICD-9-CM).11 The modification from sentinel conditions to ACS allowed a broader range of conditions identified by population-based hospitalization rates. This approach recognized that while not every hospitalization for conditions such as asthma is preventable, the lack of timely and quality ambulatory care is correlated with higher rates of hospitalization. Only a limited number of studies have applied Rutstein's sentinel events approach, with limited scope and breadth.12–15 These studies, with the exception of Woolhandler et al., have not examined racial and social inequalities in detail and have generally employed only subsets of conditions from Rutstein's lists.15 Woolhandler et al. found that the total death rate for African Americans from newborn to 65 years of age in Alameda County, California, exceeded that of white respondents by 58%. Rates of death due to preventable and manageable conditions for people from newborn to 65 years of age were 77% higher for African Americans than for white respondents.15 More than one-third of the excess total death rate of African Americans relative to white respondents could be explained by the excess of potentially preventable deaths. The authors concluded that improvements in health might be achieved by improved access to existing medical, public health, and other preventive measures.
Our study examined the rates of hospitalization for African Americans in comparison to white patients in the Medicare population, a population in which barriers to health care are reduced due to insurance. We examined race differentials with respect to admissions for ACS conditions and also looked at the temporal effects for these conditions for the state of North Carolina. The important issues that this study addresses are a comprehensive assessment of the quality of care received by African Americans and an examination of race variations in the quality of care at various levels for the state of North Carolina.
METHODS
Data sources
Data for this study came from the Centers for Medicare and Medicaid Services (CMS) Denominator and Medicare Provider Analysis and Review Record (MEDPAR) databases from the years 1999–2002 and the 2000 U.S. Census.16,17 Medicare data was obtained from a cohort of North Carolina beneficiaries who were 65 years of age or older in 1999. The claims information for each hospital discharge, which included the diagnosis and procedure codes, was obtained from the MEDPAR datasets. The beneficiary's demographic and eligibility data was extracted from the CMS Denominator enrollment database. Several studies provide details of the CMS Denominator and MEDPAR datasets.18–20 The 2000 U.S. Census data were merged with the aforementioned data sources using zip code to obtain additional demographic information about the beneficiaries.
The study population included only beneficiaries who resided in North Carolina during the study period and whose race was African American or white. Our study also excluded all those individuals who were under 65 years of age, because in the Medicare population these beneficiaries are generally disabled individuals with substantial preexisting morbidities. We further excluded all beneficiaries whose eligibility was based on disability or end-stage renal disease (ESRD). These groups were excluded because ESRD cases are severely and chronically ill and generally do not benefit from proactive treatment. We excluded those beneficiaries who did not have Medicare Part A and B insurance coverage. Medicare Part A insurance covers hospitalization costs, while Part B insurance covers outpatient services including preventive care services, thus it was necessary to require inclusion of both insurance coverages. Cases whose five-digit zip code could not be matched with the 2000 U.S. Census data were also eliminated from the sample. Finally, only beneficiaries for whom an inpatient hospital claim had been filed between 1999 and 2002 and had all resulting claim data were selected for analysis.
Study design
This study conducted an analysis of the hospital admissions for ACS conditions among Medicaid beneficiaries. In all, 287,903 hospitalization cases were selected for analysis for 1999; 281,114 cases for 2000; 263,466 cases for 2001; and 252,930 cases for 2002. Because the unit of analysis was a respondent's hospitalization, it was possible that an individual could be counted more than once. However, preliminary analyses indicate that on average only 36% of the population had multiple hospitalizations, which was comparable between both African American patients (39%) and white patients (36%).
Measures
Dependent variables
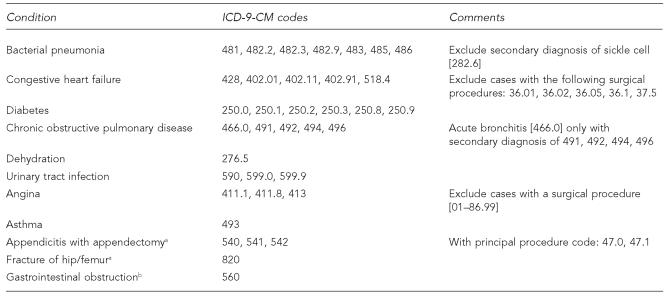
This study initially used the specification of ACS conditions proposed by the Institute of Medicine and the Massachusetts Rate Setting Commission.21,22 However, because these studies specified ACS conditions for the general population rather than just the population of patients aged 65 years and older, on which our study is based, we decided upon the ACS conditions that affect older populations as specified by a recent report from the Department of Health and Human Services (DHHS) Agency for Healthcare Research and Quality.23 Admissions for each of the following ACS conditions were coded as a binary (yes or no) variable: bacterial pneumonia, congestive heart failure (CHF), diabetes, chronic obstructive pulmonary disease (COPD), dehydration, urinary tract infection, angina, and asthma. ICD-9-CM coding used in determination of diagnosis for each condition is included in Table 1.
Table 1.
ICD-9-CM diagnosis/procedure codes for ACS conditions and markersa
Codes adapted from Billings. ACS Algorithm, John Billings, New York University Center for Health and Public Service Research [cited 2005 Jun 21]. Available from: URL: http://www.nyu.edu/wagner/chpsr/acs_codes.pdf
Indicates marker condition.
ICD-9-CM = International Classification of Diseases, 9th Revision, Clinical Modification
CM = clinical modification
ACS = ambulatory care sensitive
We also assessed “marker” conditions that are generally considered to not vary substantially according to access to care.24 Marker conditions included the following conditions: appendicitis with appendectomy, gastrointestinal obstruction, and fracture of the hip/femur. Each condition was coded as a binary (yes or no) variable and then summed for total admissions for marker conditions. These conditions are not substantially subject to prevention and prediction in the general population and occur randomly. Therefore, they can be used as a point of reference from which to view ACS conditions in the population studied.
Independent variables
Two independent variables used in this study are race and year. Only African American and white patients are included in the study. Race was determined from the CMS denominator enrollment database.
ANALYSIS
The primary outcome was rates of hospitalization for ACS conditions. Rates for ACS conditions were determined as a percentage of total hospital claims. Descriptive statistics by race were computed at each time point. Cochran-Mantel-Haenszel tests were used to test the association between hospitalization rates for African American and white patients controlling for time. Tests for trends in admission rates from 1999 to 2002 were conducted using the Cochran-Armitage test for trend.25 All analyses were conducted using SAS/STAT® software Version 9.1.26
RESULTS
Demographics
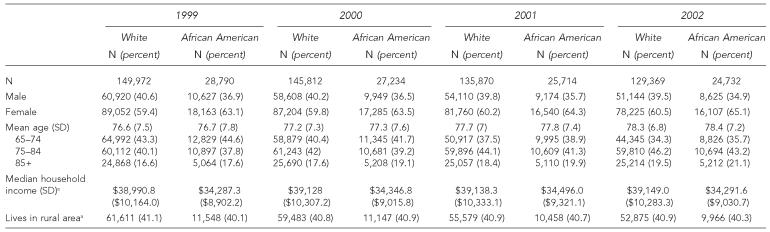
Table 2 shows the sample demographics by year and race. The sample included mostly female and white patients. There were no notable differences by race in regard to gender, age, or location (rurality), although the ages for African Americans showed greater variation. The mean age for white patients ranged from 76.6 (with standard deviation [SD]=7.5) in 1999 to 78.3 (SD=6.8) in 2002. The mean age for African Americans ranged from 76.7 (SD=7.8) in 1999 to 78.4 (SD=7.2) in 2002. Data from the 2000 U.S. Census indicated differences in the median household incomes of zip codes in which white patients and African American patients lived. The median household income for white patients was higher by $4,781 in 2000.
Table 2.
Demographics of Medicare beneficiaries by race and year
Median household income and rurality for each year is based on 2000 Census zip code level data. Rural area is zip code where 50% or more of the area is rural.
SD = standard deviation
Rates for ACS conditions
Table 3 shows the admission frequency of avoidable ACS conditions and rates per 1,000 admissions. There was a consistent decrease in admission rates for COPD and angina from 1999 to 2002. During the same time period, results showed a consistent increase in the rates of diabetes (7.2 in 1999 to 7.8 in 2002), dehydration (17.5 in 1999 to 20.7 in 2002), and urinary tract infection (18.8 in 1999 to 21.6 in 2002), while admission rates for other conditions fluctuated. Some of the highest admission rates were for CHF (63.3 in 2000) and bacterial pneumonia (53.1 in 2002).
Table 3.
Admission rates for ACS conditions by yeara
Rates per 1,000 hospital admissions
Marker conditions include appendicitis with appendectomy, hip fracture, and gastrointestinal obstruction.
ACS = ambulatory care sensitive
Differences in ACS rates by race
Results in Table 4 show the distribution of admission rates for ACS conditions by race for each year. Odds ratios (OR) obtained from Cochran-Mantel-Haenszel statistics are reported. For all of these comparisons, an odds ratio of less than one indicates a higher risk of hospitalization for white patients; if the OR is greater than one, African Americans have a higher risk of hospitalization.
Table 4.
Admission rates for ACS conditions by year and racea
Rates per 1,000 hospital admissions.
Odds of condition in African Americans vs. white patients controlling for year obtained from Cochran-Mantel-Haenszel statistics.
Marker conditions include appendicitis with appendectomy, hip fracture, and gastrointestinal obstruction. Mean admission rates and standard deviations (SD): appendicitis with appendectomy: African Americans 0.53 (SD50.13), white patients 0.98 (SD=0.10); gastrointestinal obstruction: African Americans 14.2 (SD=0.38), white patients 12.4 (SD=0.25); hip fracture: African Americans 11.3 (SD=0.48), white patients 27.2 (SD=0.54).
ACS = ambulatory care sensitive
OR = odds ratio
CI = confidence interval
For bacterial pneumonia, we observed lower rates of hospitalization among African American patients than white patients (OR=0.86; 95% CI [0.84, 0.89]). Conversely, African Americans were more likely to be admitted for CHF than white patients (OR=1.41; 95% CI [1.38, 1.44]). Admission rates for CHF declined for both groups between 2001 and 2002. Rates for white patients dropped from 59.6 in 2001 to 56.0 in 2002. Similarly, rates for African Americans dropped from 81.1 in 2001 to 76.6 in 2002.
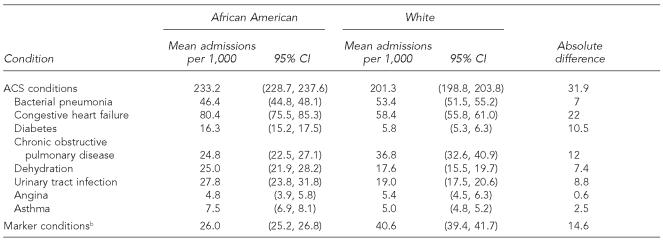
Admission rates for diabetes were nearly three times higher for African Americans than for white patients (OR=2.86; 95% CI [2.73, 2.99]). Rates for African Americans ranged from a low of 16.1 in 1999 to a high of 17.3 in 2001, while rates for the white population ranged from a low of 5.4 in 1999 to a high of 6.2 in 2002. The mean values for all years of study reveal diabetes as one of the diseases with the highest disparity between African Americans and white patients (Table 5). This disparity remained fairly consistent during all four years.
Table 5.
Mean admission rates for ACS conditions for North Carolina Medicare beneficiaries by race (1999 to 2002)a
Rates per 1,000 hospital admissions
Marker conditions include appendicitis with appendectomy, hip fracture, and gastrointestinal obstruction.
ACS = ambulatory care sensitive
CI = confidence interval
Other conditions for which African Americans had higher admission rates were primary dehydration (OR=1.43; 95% CI [1.39, 1.48]), urinary tract infection (OR=1.47; 95% CI [1.42, 1.52]), and asthma (OR=1.51; 95% CI [1.43, 1.61]). With respect to primary dehydration, admission rates increased from 23.4 in 1999 for the African American population to a high of 27.3 in 2002; concomitantly for the white population, the rates ranged from a low of 16.3 in 1999 to a high of 19.4 in 2002. The rates for urinary tract infection also increased for both groups, ranging from a low of 24.4 in 1999 for African Americans to a high of 30.5 in 2002. Rates for the white population ranged from a low of 17.7 in 1999 to a high of 19.8 in 2002. There was little variation in rates of asthma within groups, with the magnitude of disparity remaining consistent during all four years.
Lower rates of hospitalization were seen among African Americans for both COPD (OR=0.67; 95% CI [0.65, 0.69]) and angina (OR=0.90; 95% CI [0.84, 0.97]). COPD rates for white patients ranged from a high of 40.3 in 1999 to a low of 34.2 in 2002. In contrast, African Americans tend to evince a much lower affliction of this condition with a high of 26.8 in 1999 to a low of 23.3 in 2002. Absolute differences in rates of hospitalization for angina between African American and white patients ranged from 0.1 in 1999 to 1.0 in 2002 and were the least among the eight ACS and summed marker conditions assessed (Table 5).
Rates for marker conditions were fairly stable within racial groups for the period studied. However, rates were consistently higher for white patients, a difference that was mostly driven by higher rates for hip fracture in white patients.
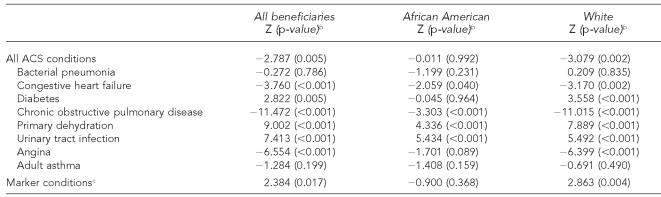
Trend analysis
Test results for trends over time for each of the ACS and marker conditions are presented in Table 6. Examination of overall ACS admissions rates for all beneficiaries revealed a decreasing trend over time (Z=–2.787; p=0.005). However, this trend was driven primarily by white beneficiaries (Z=–3.079; p=0.002). Among African Americans, significant decreasing trends in admission rates were found for CHF (Z=–2.059; p50.040) and COPD (Z=–3.303; p<0.001). Among white patients there were significant decreasing trends in admission rates for angina (Z=–6.399; p<0.001), CHF (Z=–3.170; p=0.002), and COPD (Z=–11.015; p<0.001). CHF and COPD showed a faster rate of decrease for white patients than for African American patients over time.
Table 6.
Trend analysis to determine the effect of time on ACS admission ratesa
Results from Cochran-Armitage trend test using normal approximation. Z<0 indicates decreasing trend in admission rates from 1999–2002; Z>0 indicates increasing trend from 1999–2002.
Two-sided p-value.
Marker conditions include appendicitis with appendectomy, hip fracture, and gastrointestinal obstruction.
ACS = ambulatory care sensitive
ACS conditions showing significant increasing trends for African Americans were primary dehydration (Z=4.336; p<0.001) and urinary tract infection (Z=5.434; p<0.001). Among white beneficiaries, there was a significant increasing trend in admission rates for diabetes (Z=3.558; p<0.001), primary dehydration (Z=7.889; p<0.001), and urinary tract infection (Z=5.492; p<0.001). Primary dehydration showed a faster rate of increase for white patients than for African American patients over time.
DISCUSSION
The premise of ACS conditions is that the increased rate of the conditions indicates a problem with the health-care delivery system; more specifically, a lack of timely and/or effective ambulatory care resulting in an increased rate of hospitalization in one group compared with another. Our study examined the rates of ACS condition hospitalization for African Americans in comparison to white patients in the Medicare population, a population in which barriers to health care are reduced due to insurance. We examined race differentials with respect to admissions for ACS conditions and also looked at the temporal effects for these conditions for the state of North Carolina.
The findings of our study show racial disparity in rates of admission for multiple important and common conditions. We note temporal trends that are significant for planners and those responsible for making social policy. While the rates for some conditions are falling, the disparity between races remains, indicating that the burden of disease, and potentially preventable morbidity, is disproportionately falling on African Americans.
Proactive health-care service utilization can have tremendous benefits to society. The economic and social costs of health care can be controlled if ACS conditions are detected and treated during the early stages of morbidity. These conditions, if treated in a proactive manner, can lead to better health outcomes and decreased use of costly emergency treatment and inpatient hospitalization. Quantifying race differentials for admissions for ACS conditions will underscore the need to address poor health outcomes due to access or utilization of health care that disproportionately affect specific populations. For instance, Husaini et al. found that African Americans were more likely to use emergency care or to be hospitalized as inpatients, and were less likely to see a doctor regularly for preventive care and early detection.27
The important issues that our study addresses are a comprehensive assessment of the quality of care received by African Americans and an examination of race variations in the quality of care at various levels for the state of North Carolina. An examination of our study results does suggest that overall ACS admission rates for all beneficiaries revealed a decreasing trend over time. And the results lend some support for the thesis that African Americans tend to have higher rates of admission for most ACS conditions. What remains is the need to examine whether these effects are real or artificial; that is, whether race is a proxy for other factors such as socioeconomic status, social support, or usual source of care.28
The DHHS reports several recent studies that have noted that the mortality gap between African American and white patients remains remarkably constant across the 20th century.29 Demographic research consistently reveals that mortality rates are higher for African Americans at every age, with the possible exception among those aged 85 years and older, where most studies find a mortality crossover.18,19,30 Recent demographic research has tried to explain the racial and ethnic gaps in mortality as a function of demographic characteristics, social characteristics (marital status, family size, residential location, socioeconomic status), and behavioral factors, as well as patterns of morbidity.30–32 For example, Johnson used data from the Survey on Asset and Health Dynamics Among the Oldest Old (AHEAD) and found significantly higher rates of disability, comorbidity, and mortality among African Americans when compared to white respondents even after controls for smoking, body mass index, and socioeconomic status.30
Rogers et al. and Hummer et al. used data from the National Health Interview Survey to determine whether ethnic differentials in mortality could be explained by other factors.31,32 These studies found that controls for socioeconomic status, marital status, and smoking do not erase the significant difference in overall mortality between white patients and African Americans. They suggest that cause-specific mortality for circulatory diseases and cancer may be a function of these social and behavioral factors, although they do not have enough cases to convincingly demonstrate this theory.
In lieu of these and other studies, Manton and Manton and Stallard called for a more accurate documentation of morbidity processes in mortality data.33,34 Ferraro and Wilmoth found that even in large national surveys, the statistical power of binary indicators of many morbid conditions is low, especially for subsamples of African Americans.35 In our study, the rates of admission for ACS conditions appear to be going down, possibly representing general improvements in access to and quality of care. However, the persistence of disparities in rates of admission between white patients and African Americans is indicative of ongoing structural problems with the health-care system by race.
An ancillary finding of our study involves the use of admissions for marker conditions. Our study used the conditions fractured hip, appendicitis, and small bowel obstruction to gauge hospitalizations that are not substantially influenced by ambulatory care.36 We found that the hospitalizations for the marker conditions were significantly more common in the white Medicare population compared with the African American Medicare population. Given that our study's marker condition was mostly driven by high rates of hip fracture, the racial difference found is reflective of the difference in the prevalence of osteoporosis between the two groups and not due to racial differences in access. Because hip fracture is a common diagnosis in the elderly, this prevalence difference was responsible for much of the disparity between racial groups in the marker conditions. The risk of hip fracture in white patients is substantially greater than in African Americans, even after controlling for body mass index.37 As such, the adjustment for prevalence of underlying marker conditions seems important for future work in ACS conditions.
Finally, because this was an exploratory study of one state, future examinations are needed to scrutinize what the variable effects of these conditions are on a regional and temporal scale. It may be fruitful to examine regional effects on ACS rates accounting for the socioeconomic capital of various communities. Previous research has demonstrated that ACS rates correlate with the median income in a county or zip code.38 An expansion of our work will allow us to examine the relationships of ACS rate, regional income, and race. For example, do some communities have lower morbidity rates because of better facilities in the communities?
Limitations
This study only examined people aged 65 years and older. It is possible to arrive at different conclusions when all age groups are examined. However, the Medicare population is an interesting one for the purposes of studying ACS as the entire population is insured, which reduces insurance as a reason for problems with access to care. We have not controlled for median income of the area of residence and other social and economic factors that could be responsible for differential rates. However, we will address this variable in subsequent studies. Finally, this study measures hospitalizations for a population with greater prevalence of an ACS condition along with an equivalent risk of hospitalization per person. In such a contingency, the rate of hospitalization will appear greater for that ethnic group.
Implications
The implications of these findings for future disparity research are numerous. There is a need to explore the many social and economic factors that could be responsible for the differential admission rates for ACS conditions that lead to racial disparity. Moreover, interdisciplinary studies can and should examine these issues from multiple perspectives, including sociological factors such as social support, local health infrastructure, and family cohesion. Also, the differential prevalence of the underlying marker conditions needs to be addressed in future studies. Secondary data analyses such as these ACS studies are similar to finding an elevated temperature in a patient—we know that there is a problem, but we must identify the cause.
Acknowledgments
This research was funded by the Department of Health and Human Services Agency for Healthcare Research and Quality grant R24 HS013353. Investigators were supported in part by the National Institutes of Health, National Center on Minority Health and Health Disparities, and grants R24 MD000167 and P60 MD000239. Investigators are from the Institute for Health, Social, and Community Research at Shaw University (Drs. Howard, Hakeem, and Njue and Yhenneko Jallah) and from the University of North Carolina at Chapel Hill Cecil G. Sheps Center for Health Services Research and School of Medicine (Dr. Carey).
REFERENCES
- 1.LaVeist TA, Arthur M, Morgan A, Rubinstein M, Kinder J, Kinney LM, et al. The cardiac access longitudinal study. A study of access to invasive cardiology among African American and white patients. J Am Coll Cardiol. 2003;41:1159–66. doi: 10.1016/s0735-1097(03)00042-1. [DOI] [PubMed] [Google Scholar]
- 2.Institute of Medicine. Washington: National Academies Press; 2002. Unequal treatment: what health care system administrators need to know about racial and ethnic disparities in healthcare. [Google Scholar]
- 3.Whittle J, Conigliaro J, Good CB, Lofgren RP. Racial differences in the use of invasive cardiovascular procedures in the Department of Veterans Affairs medical system. N Engl J Med. 1993;329:621–7. doi: 10.1056/NEJM199308263290907. [DOI] [PubMed] [Google Scholar]
- 4.American Medical Association Council on Ethical and Judicial Affairs. Black-white disparities in health care. Conn Med. 1990;54:625–8. [PubMed] [Google Scholar]
- 5.Blendon RJ, Aiken LH, Freeman HE, Corey CR. Access to medical care for black and white Americans. A matter of continuing concern. JAMA. 1989;261:278–81. [PubMed] [Google Scholar]
- 6.Ford E, Cooper R, Castaner A, Simmons B, Mar M. Coronary arteriography and coronary bypass survey among whites and other racial groups relative to hospital-based incidence rates for coronary artery disease: findings from NHDS. Am J Public Health. 1989;79:437–40. doi: 10.2105/ajph.79.4.437. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Wenneker MB, Epstein AM. Racial inequalities in the use of procedures for patients with ischemic heart disease in Massachusetts. JAMA. 1989;26:253–7. [PubMed] [Google Scholar]
- 8.Oberman A, Cutter G. Issues in the natural history and treatment of coronary heart disease in black populations: surgical treatment. Am Heart J. 1984;108(3 Pt 2):688–94. doi: 10.1016/0002-8703(84)90656-2. [DOI] [PubMed] [Google Scholar]
- 9.Rutstein DD, Berenberg W, Chalmers TC, Child DG, III, Fishman AP, Perrin EB. Measuring the quality of medical care. N Engl J Med. 1976;294:582–8. doi: 10.1056/NEJM197603112941104. [DOI] [PubMed] [Google Scholar]
- 10.Goodrum LA. Maternal mortality: strategies in prevention and care. Hospital Physician. 2001;1:44–51. [Google Scholar]
- 11.Billings J, Zeitel L, Lukomnik J, Carey TS, Blank AE, Newman L. Impact of socioeconomic status on hospital use in New York City. Health Aff (Millwood) 1993;12:162–73. doi: 10.1377/hlthaff.12.1.162. [DOI] [PubMed] [Google Scholar]
- 12.Adler GS. Measuring the quality of medical care. N Engl J Med. 1978;298:574. doi: 10.1056/NEJM197803092981020. [DOI] [PubMed] [Google Scholar]
- 13.Charlton JR, Hartley RM, Silver R, Holland WW. Geographical variation in mortality from conditions amenable to medical intervention in England and Wales. Lancet. 1983;1:691–6. doi: 10.1016/s0140-6736(83)91981-5. [DOI] [PubMed] [Google Scholar]
- 14.Heineken PA, Charles G, Stimson DH, Wenell C, Stimson RH. The use of negative indexes of health to evaluate quality of care in a primary-care group practice. Med Care. 1985;23:198–208. doi: 10.1097/00005650-198503000-00002. [DOI] [PubMed] [Google Scholar]
- 15.Woolhandler S, Himmelstein DU, Silber R, Bader M, Harnly M, Jones AA. Medical care and mortality: racial differences in preventable deaths. Int J Health Serv. 1985;15:1–22. doi: 10.2190/90P3-LEFF-WNU0-GLY6. [DOI] [PubMed] [Google Scholar]
- 16.North Carolina State Segment for Denominator and MEDPAR Research Identifiable Files. Center for Medicare and Medicaid Services (US) 2003. [cited 2003 Dec 30]. Available from: URL: http://resdac.umn.edu/medicare/data_file_descriptions.asp#rif.
- 17.Census Bureau (US) Decennial census of population and housing: 2000 summary file 3. [cited 2005 Sep 1]. Available from: URL: http://dataferrett.census.gov/TheDataWeb/index.html.
- 18.Kestenbaum B. Description of the extreme aged population based on improved Medicare enrollment data. Demography. 1992;29:565–80. [PubMed] [Google Scholar]
- 19.Parnell AM, Owens CR. Evaluation of U.S. mortality patterns at old ages using Medicare Enrollment Data Base. Demogr Res. 1999;1(30) doi: 10.4054/demres.1999.1.2. [DOI] [PubMed] [Google Scholar]
- 20.Husaini BA, Blasi AJ, Miller O. Does public and private religiosity have a moderating effect on depression? A bi-racial study of elders in the American South. Int J Aging Hum Dev. 1999;48:63–72. doi: 10.2190/F5MT-RTYH-7XR1-TFQU. [DOI] [PubMed] [Google Scholar]
- 21.Milman M. Washington: National Academies Press; 1993. Access to health care in America. [PubMed] [Google Scholar]
- 22.Baker C. Boston, MA: Massachusetts Rate Setting Commission; 1994. Preventable hospitalization in Massachusetts. William F. Weld, Governor, Commonwealth of Massachusetts. [Google Scholar]
- 23.Department of Health and Human Services (US) Rockville, MD: Agency for Healthcare Research and Quality; 2004. Nov 24, [cited 2006 Feb 17]. AHRQ quality indicators—guide to prevention quality indicators: hospital admission for ambulatory care sensitive conditions. Revision 4. AHRQ Pub. No. 02-R0203. Also available from: URL: http://www.qualityindicators.ahrq.gov/downloads/pqi/pqi_guide_v30a.pdf. [Google Scholar]
- 24.Saha S, Ady O, Bindman A. Impact of the Oregon Medicaid demonstration on preventable hospitalization rates. Academy Health Conference. 2003. [cited 2006 Feb 20]. Available from: URL: http://www.oregon.gov/DAS/OHPPR/OHREC/Docs/Preventions/ImpHospRts11_03.pdf.
- 25.Mantel N, Haenszel W. Statistical aspects of the analysis of data from retrospective studies of disease. J Natl Cancer Inst. 1959;22:719–48. [PubMed] [Google Scholar]
- 26.SAS Institute, Inc. Cary (NC): SAS Institute, Inc; SAS/STAT Software: Version 9.1 for Windows. 2002–2003. [Google Scholar]
- 27.Husaini BA, Sherkat DE, Levine R, Bragg R, Holzer C, Anderson K, et al. Race, gender, and health care service utilization and costs among Medicare elderly with psychiatric diagnoses. J Aging Health. 2002;14:79–95. doi: 10.1177/089826430201400105. [DOI] [PubMed] [Google Scholar]
- 28.Pekoz EA, Shwartz M, Iezzoni LI, Ash AS, Posner MA, Restuccia JD. Comparing the importance of disease rate versus practice style variations in explaining differences in small area hospitalization rates for two respiratory conditions. Stat Med. 2003;22:1775–86. doi: 10.1002/sim.1398. [DOI] [PubMed] [Google Scholar]
- 29.Department of Health and Human Services (US) Healthy people 2010: conference edition, volume 1 and volume 2. Washington: U.S. Government Printing Office; 2000. [Google Scholar]
- 30.Johnson NE. The racial crossover in comorbidity, disability, and mortality. Demography. 2000;37:267–83. [PubMed] [Google Scholar]
- 31.Hummer RA, Rogers RG, Nam CB, LeClere FB. Race/ethnicity, nativity, and U.S. adult mortality. Social Science Quarterly. 1999;80:136–53. [Google Scholar]
- 32.Rogers RG, Hummer RA, Nam CB, Peters K. Demographic, socioeconomic, and behavioral factors affecting ethnic mortality by cause. Social Forces. 1996;74:1419–38. [Google Scholar]
- 33.Manton KG. Sex and race specific mortality differentials in multiple cause of death data. Gerontologist. 1980;20:480–93. doi: 10.1093/geront/20.4.480. [DOI] [PubMed] [Google Scholar]
- 34.Manton KG, Stallard E. Medical demography: interaction of disability dynamics and mortality. Demography of Aging. 1997:217–78. [Google Scholar]
- 35.Ferraro KF, Wilmoth JM. Measuring morbidity: disease counts, binary variables, and statistical power. J Gerontol B Psychol Sci Soc Sci. 2000;55:S173–89. doi: 10.1093/geronb/55.3.s173. [DOI] [PubMed] [Google Scholar]
- 36.ACS Algorithm, John Billings, New York University Center for Health and Public Service Research. [cited 2005 Jun 21]. Available from: URL: http://www.nyu.edu/wagner/chpsr/acs_codes.pdf.
- 37.Barrett-Connor E, Siris ES, Wheren LE, Miller PD, Abbott TA, Berger ML, et al. Osteoporosis and fracture risk in women of different ethnic groups. J Bone and Miner Res. 2005;20:185–94. doi: 10.1359/JBMR.041007. [DOI] [PubMed] [Google Scholar]
- 38.Billings J, Hasselblad V. A preliminary study: use of small area analysis to assess the performance of the outpatient delivery system in New York City. Health Systems Agency of New York City. 1989 [Google Scholar]