Abstract
Objectives
To evaluate the effectiveness of a problem-based learning (PBL) model implemented in 1995 at the University of Mississippi School of Pharmacy.
Design
The third-professional (P3) year curriculum was reoriented from a faculty-centered model of teaching to a student-centered model of learning. Didactic lectures and structured classroom time were diminished. Small student groups were organized and a faculty facilitator monitored each group's discussions and provided individual student assessments. At the end of each 8-week block, students were assessed on group participation, disease and drug content knowledge, and problem-solving abilities. Faculty and student input was solicited at the end of each year to aid programmatic improvement. In 2000, a formal 5-year review of the PBL program was conducted.
Assessment
Recommendations for improvement included clarifying course objectives, adopting a peer-review process for examination materials, refining the group assessment instruments, and providing an opportunity for student remediation after a course was failed. A weekly case conference presided over by a faculty content expert was also recommended. Ongoing critical evaluation during the following 5-year period was provided by graduates of the program, faculty participants, and accreditation reviews.
Conclusion
Over our 10-year experience with a PBL model of P3 education, we found that although the initial challenges of increased demands on personnel and teaching space were easily overcome, student acceptance of the program depended on their acknowledgment of the practical benefits of active learning and on the value afforded their input on curricular development.
Keywords: active learning, problem-based learning, student-centered learning
INTRODUCTION
The profession of pharmacy evolves to meet the changing demands of the society it serves. With each metamorphosis new opportunities arise for expanding the scope of pharmacy practice. The responsibilities of pharmacists have grown from appropriately dispensing medications to providing services that optimize the benefits of pharmaceutical therapies. The knowledge base and skill sets of pharmacists must expand to address the patient and institutional needs for such medication therapy management. The Accreditation Council for Pharmacy Education (ACPE) recognizes that pharmacy education must change to accommodate this heightened expectation of its practitioners. The ACPE's enhanced requirements for accreditation encouraged all schools and colleges of pharmacy to implement a lengthier and more rigorous curriculum that prepares pharmacists to fulfill these new responsibilities and that insures its graduates can adapt to future professional imperatives.
The Standards for Curriculum published by ACPE state that “The educational process should promote lifelong learning through the emphasis on active, self-directed learning.” The standards further state that curricula should include “teaching strategies to ensure the adeptness of critical thinking and problem-solving.”1 To assess whether the pharmacy curriculum at the University of Mississippi conformed to ACPE requirements, a review of our course content and teaching methods was undertaken. Many of our courses were found to be structured along the lines of traditional medical school education: they were organ-based and they relied upon a didactic lecture format for teaching. This organization was especially evident in the third-professional (P3) year, when drug information was presented to students in a modularized fashion (ie, cardiovascular medications were considered in isolation from gastrointestinal therapies). This teaching model did not profit from the recent insights of adult learning theorists, in that it provided few opportunities for active, self-directed learning. From an assessment standpoint, our curriculum was also deemed deficient in that educators could not evaluate a student's ability to integrate information from different modules and to apply such integrated content knowledge by solving clinical problems.2 Over-reliance on clinical practice experiences in the fourth and final curriculum year to develop a student's critical thinking skills was also noted. Given that the quality of these extramural experiences could not be uniformly ensured, no certainty that graduates had developed these crucial professional capabilities could be anticipated. After identifying manifold deficiencies with the currently employed faculty-centered model of teaching, the School of Pharmacy reoriented the curriculum by adopting a student-centered model of learning.
A movement away from a didactic teaching model to an educational design that fostered active, self-directed learning did not necessarily mean that a problem-based learning (PBL) model would be adopted. Active-learning techniques such as small-group discussions or writing exercises can exist within the confines of a lecture format, which may also be enhanced by classroom debate, role-playing, or peer teaching.3 A taskforce of Department of Pharmacy Practice faculty members carefully considered different options for increasing the student role in facilitating self-education. Their review and recommendations led to a decision to implement a PBL model at the University of Mississippi. Our PBL program provides students the opportunity to develop critical thinking and problem-solving skills in a controlled environment. We employ these innovative teaching methods in the P3 year of the curriculum, which is now termed the Pharmaceutical Care course series. The following is a descriptive report of our program and an overview of our experiences with a PBL model of pharmacy education.
DESIGN
Expected Outcomes and Learning Objectives
Faculty members were initially enthused to design a pharmacy curriculum based upon an active-learning model. However, it became clear that any innovation would require consensus building within the Department prior to implementation, as these curricular changes could be perceived not only as an explicit rejection of the existing teaching model, but also as an implicit criticism of the educational theories held by current course directors. To ease this transition, a committee of interested faculty members was formed to identify barriers to curricular innovation and to formalize a PBL proposal to present to the whole of the Department of Pharmacy Practice and to the School of Pharmacy and University of Mississippi administrators. The PBL Committee began work in the fall semester of 1994 and set a goal of implementing a revised curriculum 1 year later.
The committee ratified the ACPE standards, which emphasize that the development of active, self-directed learning skills is essential to contemporary pharmacy practice. They also enumerated curricular objectives drawn from those articulated by Barrows et al.4 The objectives of the PBL course series were to help students acquire and retain a sound knowledge base, to learn to use indexing and pharmacy literature resources, to develop and utilize critical thinking and communication skills in clinical problem-solving, and to appreciate the need for lifelong learning.
In their initial review of challenges facing the adoption of a PBL model of education, the committee was able to identify several issues. Salient among these were the significant start-up and maintenance costs, including increased demands for teaching space and on personnel time, and the lack of student recognition of the need for curricular change. A heightened awareness of the obstacles ahead allowed the School of Pharmacy the opportunity to address these concerns head on and to avoid potential roadblocks to implementation. However, as with all institutional change, many issues arose that were not initially apparent.
Educational Environment
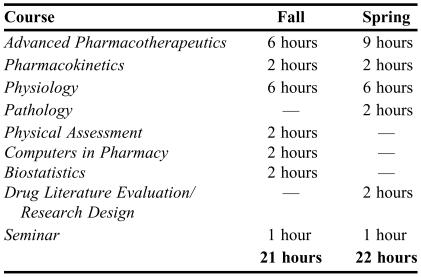
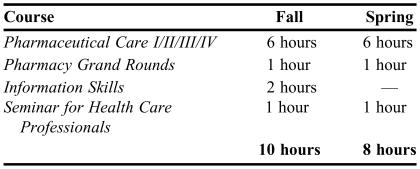
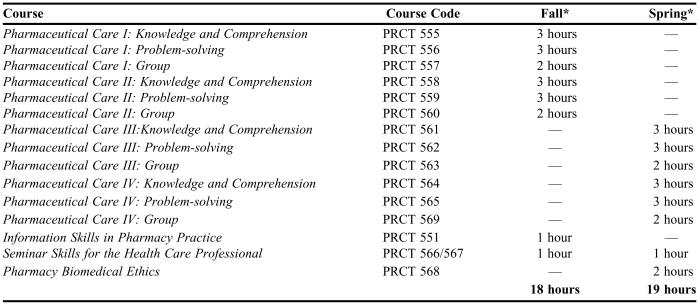
The University of Mississippi grants the doctor of pharmacy degree (PharmD) after the successful completion of 6 years of course work, the last 4 years of which are referred to as professional years (P1-P4). The P3 curriculum is largely under the purview of the Department of Pharmacy Practice, which is located on the main health sciences campus adjacent to the University of Mississippi Medical Center in Jackson. The structure of the P3 year was completely revised. The existing course requirements expected students to be present for didactic, classroom lectures approximately 20 hours per week (Table 1). This structure provided little opportunity for student-teacher or student-student interaction. Active learning is time consuming as it is student-directed and thus less efficient than teacher-centered learning; therefore, mandatory classroom attendance time was reduced to accommodate out-of-classroom research and study. The revised course curriculum restructured what had been standalone courses in physiology, pathology, pharmacokinetics, pharmacotherapeutics, and physical assessment into a vertically integrated, single-entity course series called Pharmaceutical Care. The learning topics previously covered over multiple courses were incorporated into clinical case scenarios presented to students for discussion in small groups facilitated by a faculty mentor. Physical assessment skills were to be acquired during advanced pharmacy practice experiences (APPEs) in the P4 year. The PBL format was not believed to be conducive to learning biostatistical analysis, principles of research design, drug literature evaluation, and the use of computers in pharmacy, so these curricular elements were combined as a programmed learning course presented on compact disc (CD) for at-home study entitled Information Skills in Pharmacy Practice. Our existing 1-hour course, Seminar Skills Development for Health Care Professionals, was continued so that students could forge and hone their public-speaking skills. All students attended a 1-hour per week class referred to as Pharmacy Grand Rounds, which allowed students to interact with faculty members or outside content experts about issues that arose in their small group discussions. In this revised curriculum, the time students spent in class decreased by approximately 10 hours per week, which opened up significant time for self-directed learning (Table 2).
Table 1.
Third-Year Pharmacy Curriculum Prior to Implementation of Problem-based Learning Model
Table 2.
Implemented Third-Professional Year Pharmacy Curriculum
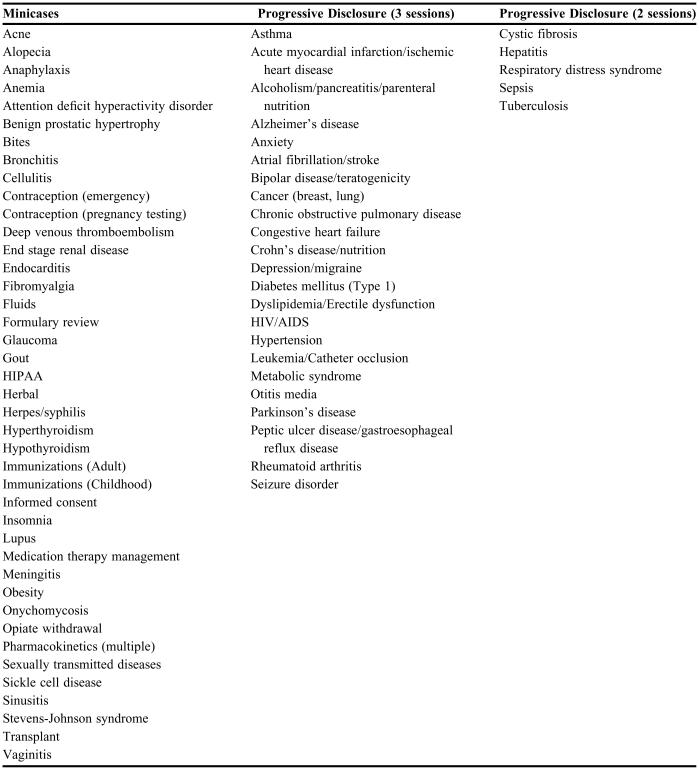
Students were assigned to small groups of their peers (maximum 8 students per group) under the direction of a faculty facilitator. Students and facilitators met 3 times per week for 2 hours over an 8-week period or “block.” Block I and block II comprised the fall semester, and block III and block IV comprised the spring semester. Groups and facilitators were randomly reassigned every 8 weeks or at the start of each block. Most full-time faculty members facilitated two 8-week blocks per academic year. The focus of small-group learning was problem-based clinical care scenarios or “cases” developed by faculty members. Case topics to be discussed during group sessions were selected to address basic science or pharmacologic principles, to review common clinical practice problems, or to explore business, legal, or ethical concerns encountered by pharmacists (Table 3).
Table 3.
Case Topics Covered in a Problem-based Learning Model Within a PharmD Curriculum
To foster communication among group members and faculty facilitators outside of meeting times, students were required to have a computer with Internet access and e-mail capabilities. In keeping with a model of self-directed learning, no textbooks were identified as “required.” A “suggested” reading list was provided, which included pharmacokinetics and therapeutics references, a medical dictionary, anatomy and physiology texts, and a pharmacology text. MicroMedex Healthcare Series (Thomson Micromedex, Greenwood Village, Colo.) was made available electronically. Student access to the University Medical Center's library was assured. To enable confidential communication between students, faculty facilitators, and course directors, a dedicated, password-protected web site was developed.
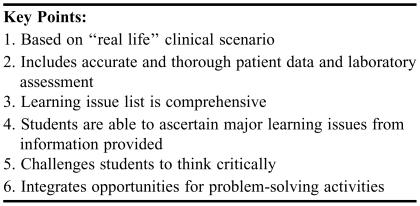
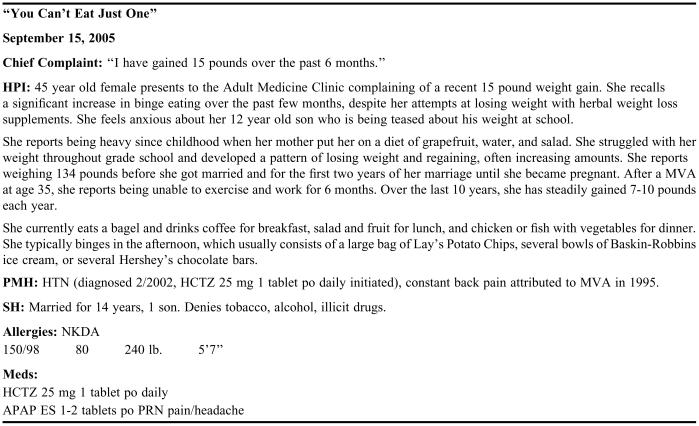
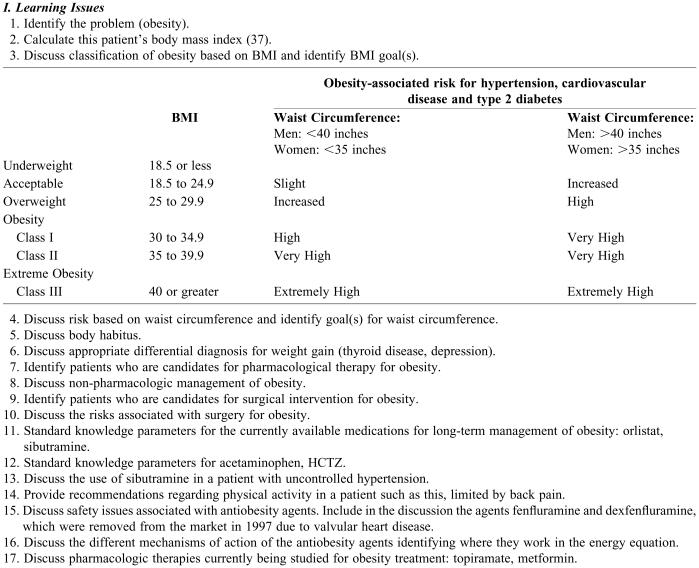
An early challenge in implementing the PBL curriculum was to develop faculty case-writing skills in order to generate an operative set of teaching cases. It was estimated that it would take between 20 to 80 hours to develop a teaching case, depending on its complexity and the content expertise and experience of the author. A template for PBL case construction and an accompanying facilitator's guide were developed with the cooperation of consultants from the Mississippi State University College of Veterinary Medicine (a patient case template is available from the author upon request.). Mississippi State had established a PBL curriculum in the early 1990s, and proponents of that program were hired to hold a full-day case writing workshop to demonstrate how to adapt teaching cases from actual patient encounters. The key points they emphasized were that good teaching cases reflected real life practice and permitted students to discern pertinent issues of pathophysiology and practical therapeutics while mastering clinical assessment and problem-solving skills (Table 4).
Table 4.
Key Points of Consideration for Faculty in Case Development
Faculty manpower demands were also impacted by this curricular reorientation. Small student group organization is labor-intensive, as a full complement of faculty facilitators is required for each 8-week block. It was clear that the personnel required by a PBL model could not be met by the Department of Pharmacy Practice's full-time faculty members. Therefore, employees of the University Medical Center's Department of Pharmacy as well as faculty members and staff from other disciplines, including advanced practice nurses and physicians, were incorporated into the PBL teaching team. These case authors and facilitators were granted adjunct faculty status. Unlike full-time faculty members, this cadre of educators committed to facilitate only one 8-week block of PBL group sessions each academic year, a time commitment of approximately 10 hours per week. Pharmacy Practice assignments were made by the department chair and faculty members with significant research commitments or clinical responsibilities were considered for a reduced teaching load. Faculty members who accepted the responsibilities for coordinating the activities within a block were also assigned a less rigorous facilitator load. No additional support personnel were sought for initial implementation of the PBL model. An existing clerical position was upgraded to a position for a project coordinator whose job responsibilities were solely dedicated to the maintenance of the PBL program.
Most academic campuses have ample auditoria and lecture hall space. However, such large classrooms are not conducive to group discussions. Facilities for small-group learning were virtually nonexistent when the PBL program was conceived. Several acceptable on-site spaces were initially identified, including faculty and staff conference rooms, study rooms in the medical library, and small classrooms within the Medical Center complex. In 1997, space was leased at a private facility, although the accommodations were not ideal. In 1998, the opportunity to occupy space in an abandoned retail center that was converted into a medical mall became available. The Jackson Medical Mall lies approximately 1 mile from the main Medical Center and was renovated to consolidate its outpatient clinics and to provide space for other health care organizations and community resources. With the support of the School's administrators, 10,000 square feet of space was leased to house the PBL program and an associated clinical practice site for P4 and graduate resident training. Ten small group meeting rooms, each approximately 150 square feet, were specifically designed for PBL use. These rooms are equipped with round conference tables, comfortable chairs, white dry-erase boards, flip charts, and abundant bulletin board hanging space to enhance active-learning processes. A large classroom with sophisticated audiovisual and electronic media capabilities was added to accommodate meetings of the entire P3 class.
The PBL curriculum was phased in for a select group of students in the fall of 1995. Students classified as P2 in the 1994-1995 and 1995-1996 academic years were presented with a curricular option: either complete the traditional bachelor of science in pharmacy (BSPharm) program already in place or enter the 2-year program leading to a PharmD. Those who chose to enroll in the doctoral program track would be choosing to participate in the new PBL model during their P3 year. In 1997, the bachelor degree program was eliminated, those who initially opted out of PBL participation were the last class of University of Mississippi students granted this degree. Conversion to an exclusively doctoral granting program led to smaller class sizes, which facilitated the transition to the new active, self-directed PBL format. The entering Pharmacy School class size has remained consistent at 90 students per year since the beginning of the PBL program. Since 1997, the average number of students entering the PBL program in the P3 year is 80. As the PBL structure utilizes 9 to 12 facilitators per 8-week block for 4 curricular blocks each academic year, approximately 30 trained faculty facilitators are required to fully service the program.
Pedagogy/Andragogy
During each week of PBL group sessions, students were to identify pertinent clinical issues in the care scenarios distributed. They were responsible for generating differential diagnoses and recommending therapeutic strategies. Moreover, they were to determine which teaching points required further investigation outside of group meeting times. Group members rotated through assigned leadership tasks each week. The “reader” would read aloud the case being discussed, so as to mimic a real-time patient case presentation. The “board scribe” would map patient data, diagnostic hypotheses, and treatment alternatives on a board in front of the group, as input from the students were solicited in turn. The “table scribe” was responsible for maintaining a list of “learning issues” that arose and for distributing the list to the other students following class, usually in an e-mail communication. At the end of the each group discussion, the responsibility for researching each of the identified learning issues and for presenting that material at the next session was divided among the students. In this manner, small group participants relied upon each other's individual efforts for their learning and in this process became teachers themselves.
The role of the faculty facilitator was to create an educational environment in which cooperative learning could occur. Facilitators were not to steer student discussions, but to stimulate thought by asking pertinent, open-ended questions when the group members seemed at an impasse. Facilitators were also charged to assess individual student performances in the group setting and to report summary judgments at defined intervals. Although content expertise might be helpful, it was not deemed an essential element to the facilitator's role. But, to better ensure uniformity in each small group's learning experience, a weekly facilitators' meeting was conducted. During this 2-hour session, the case author for the material to be presented the following week previewed the upcoming clinical care scenario. Since faculty facilitators often had outstanding research and patient care responsibilities, they could schedule classes to accommodate their obligations. Group sessions could be held from 7:00 am to 7:00 pm. Badge access to the PBL space was monitored by security guards, and group rooms were under the lock-and-key control of the facilitators. Substitute facilitators were available to cover unavoidable facilitator absences.
Content
The PBL course materials were based on instructive patient cases prepared in a standardized format. Eight major cases, termed “progressive disclosure cases,” were covered in each 8-week PBL block. These cases were presented over 2 to 3 group sessions during which patient information was revealed and discussed as it was disclosed, so as to mimic real-world pharmacy practice in an ambulatory clinic, hospital setting, or retail space (an example of a progressive disclosure case is available upon request). Case materials were presented over approximately 20 to 30 pages, of which the facilitator would distribute 5 to 10 pages per group session. Students would identify and discuss learning issues after each page was distributed and prior to the progressive disclosure of the next page of clinical information. To ensure the uniform quality of the educational content, each progressive disclosure case was previewed by a faculty member who had attended the workshop on case authorship.
Although students were to work through the presenting complaint, past medical history, physical findings, and diagnostic test results of the patient case as it unfolded, the patient diagnosis was identified at the close of the first group meeting. Each student was held responsible for preparing a proposed “treatment plan” to submit at the next group meeting for facilitator review. To allow adequate time to complete this assignment, one day must elapse between the scheduling of the first and second group sessions. The treatment plan should include initial medication recommendations, therapeutic and adverse effect monitoring parameters, a plan for patient and family education, and an alternate treatment plan in case the initially outlined therapy was not tolerated or was ineffective (Appendix 1). The faculty assessment of the quality of these treatment plans was one factor considered in their final evaluation of each student's group performance.
The week-long progressive disclosure cases were supplemented by so-called “minicases.” These clinical care scenarios were designed to be read during a single group session and did not require the preparation of a written treatment plan. Learning issues contained in a minicase were to be straightforward and limited. These cases were provided prior to class sessions and students were expected to be fully acquainted with the disease state presented, the pharmacokinetic or pharmacodynamic issues addressed, or the common pharmacologic intervention employed. The academic demands imposed by minicases escalated over the year, beginning with 1 minicase per week in the second block and increasing to 3 minicases per week in the fourth block (Appendix 2, Appendix 3).
Evaluation Methods
Faculty members believed that students should be evaluated on more than knowledge acquisition and retention, since the fundamental premise of a PBL model was the development of critical thinking and problem-solving skills. An evaluation system was proposed that consisted of facilitator assessments of student group performance, a content-based written examination, and an examination to test problem-solving skills based upon the presentation of a novel clinical care scenario. Students were to receive a final grade for each 8-week block constructed from a weighted average of these and other evaluation components (Table 5). The group performance assessment was to be based upon student participation in group learning: to what degree they cooperated with their peers during group sessions and how well they communicated their research insights to the group during subsequent meetings. Self- and peer evaluations were also solicited, and these assessments as well as those of the facilitator evaluations would contribute to the final grade. Evaluation was reciprocal, with students completing a blinded evaluation of each new facilitator they encountered in their group sessions. The knowledge and comprehension, or content examinations not only emphasized those learning issues prompted by case discussions for that block, but also assessed cumulative learning across the curriculum. The questions which composed the content examinations were submitted by case authors. The problem-solving examination was grounded in cases that were not presented during group sessions, so as to test the students' abilities to work through unfamiliar patient care concerns. These cases were provided in advance, so that students had the opportunity to generate responses after self-directed investigation. The novel case for the problem-based examination was constructed by one of the faculty case authors as well. Both written examinations were administered only once at the end of each 8-week block.
Table 5.
Determination of Course Grades in the Initial Problem-based Learning Model
Approval of Proposed Design
The PBL Committee circulated its proposal on curricular reform among Department of Pharmacy Practice faculty for comment before formally presenting its recommendations in final form in January 1995. It was approved after the unanimous acquiescence of all departmental faculty members. Before proceeding beyond department-level approval, the Executive Director of ACPE was consulted. Departmental leaders desired to reassure potential skeptics that these innovative curricular revisions would not jeopardize school accreditation. Specific concerns were addressed with the Director, paramount among these was the fact that by adopting an integrated PBL model explicit course identifiers would be lost (eg, no “pharmacotherapeutics” grade would be so identified on a student transcript). The Director reviewed the proposal and offered full and enthusiastic support, though he encouraged the faculty to adopt a rigorous program of course evaluation.
After favorable extramural acceptance was assured, further University approval was sought and granted. Over several months, the Curriculum Committee of the School of Pharmacy, the full faculty of the School, the Undergraduate Council of the University of Mississippi, and the Academic Council of the University all agreed to approve the proposed PBL curriculum. Under the optimistic assumption that all necessary approvals would be obtained, faculty development and additional logistic planning was initiated in the spring of 1995. This foresight allowed successful implementation of the new educational model in the fall semester of 1995. Adoption of a PBL model of education at the University of Mississippi was achieved through an open process that sought consensus on curricular change at each phase in its development.
ASSESSMENT
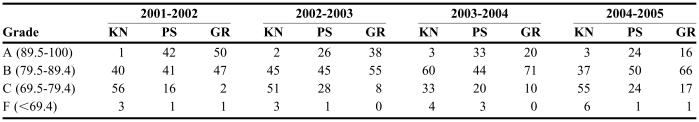
Curricular innovations are usually conducted in small test groups that can be evaluated concurrently with the standing teaching model. We committed all of our educational resources to a complete overhaul of the P3 curriculum; therefore, a comparator cohort was not available to assess the effectiveness of the PBL model. Longitudinal comparisons against historical data were also problematic, as we adopted new performance measures for the new program. Overall student performance has been tracked, and while the data do not definitively reveal improved outcomes, no decline in student achievement has been seen (Table 6). Consistent graduate performances on extramural measures such as the North American Pharmacist Licensure Examination (NAPLEX) has been the rule.
Table 6.
Third-professional Year PharmD Curriculum (2001-present)
*Credit hours (not time spent in class)
Stakeholder perspectives on the PBL initiative were actively sought since the program's inception. As our initial curricular review was spurred by new ACPE standards, we eagerly anticipated their accreditation review in 2000. The ACPE had previously visited the School of Pharmacy in 1993, prior to the implementation of the doctor of pharmacy degree program. Their more recently registered Evaluation Form Report commended the Department of Pharmacy Practice for its new PBL model of professional education. The accreditation body observed that successful implementation had occurred, and recommended an ongoing internal review process to identify any needed curricular refinements.
The student body did not uniformly accept our educational innovation. Some self-appointed advocates voiced strong concerns over the curriculum's sole reliance on PBL instruction and the academic burdens imposed by self-directed learning. They also criticized what they viewed as vague and subjective performance assessments. Concerned faculty members also believed that the grading scheme was flawed, but for different reasons. As initially conceived, the final grade for the Pharmaceutical Care course series was a calculated average of performance on its different components (Table 5). Faculty members came to realize that students could essentially fail one curricular component, yet achieve a summary passing grade by focusing their attention on 1 or 2 components and disregarding the others. Some faculty members also questioned whether a PBL model was adequate to convey sophisticated or complicated content knowledge. Like many students, some group facilitators believed that supplemental didactic lecture presentations were still necessary to insure content knowledge acquisition. Due to these and other concerns, a formal review of the PBL initiative was conducted at the 5-year mark.
PBL Commission Review (1995-2000)
In 2000, a PBL Commission was charged with conducting a thorough review of the structure and content of the Pharmaceutical Care course series and with recommending any curricular changes deemed necessary to improve student education. The 5 member panel was composed of 4 Department of Pharmacy Practice faculty members, all of whom were aware of the development of the program and had participated as case authors or facilitators. The final commissioner was recruited from outside the Medical Center campus. Although the fifth member was not fully acquainted with the program, she was knowledgeable in undergraduate education design and was positioned to provide an extramural perspective.
The Commission solicited input from faculty members, students, and graduates, and based on this narrative feedback identified several areas for improvement. They specifically drew attention to the need to clarify course objectives, vet the examination materials, refine the assessment tools, and offer failed students an opportunity for remediation. They also recommended the addition of a weekly case conference to be attended by the P3 class as a whole.
The Commission found that stated course objectives did not correlate well with items on the content and problem-solving examinations. Indeed, the examinations themselves did not always adhere to their curricular intent. Problem-solving abilities were necessary to answer questions on the content examination, and the tool used to assess problem-solving skills required a sufficient level of content knowledge for successful completion. The commissioners also found a lack of consistency in the formatting of examination questions. Examinations were constructed from questions submitted by multiple case authors, many of whom did not adhere to the recommended standards.
The panel members accepted the student argument that the examinations were “high stakes” endeavors that provoked significant performance anxiety. As initially structured, only one content and one problem-solving examination was administered at the close of the 8-week block, which cumulatively covered the case material over that period. The commissioners believed that stress over this single opportunity to demonstrate proficiency might hinder the performance of vulnerable individuals.
The Commission also expressed concern over the assignment of a single final grade for the Pharmaceutical Care course series. For students who failed, the only option for those who desired to progress in their professional education was to repeat the same course during the same time period the following academic year. Educational blocks were built of unique content materials that were only offered in a scheduled sequence. Because it was thought that mastery of 1 block was necessary for the completion of subsequent blocks, the initial PBL grading policy prohibited progression to the next course in the series, should a student be unsuccessful in an earlier Pharmaceutical Care course. The commissioners believed that this system was flawed and that students were disadvantaged both educationally and financially by this unforgiving structure.
Finally, the Commission recognized the student desire for an opportunity to interact with faculty members after completing their patient case reviews, to discuss unresolved learning issues and to have their outstanding questions answered by the case authors. The panel members also ratified faculty concerns that some PBL course materials might require content expert presentation. The originally adopted PBL model allocated no class time specifically for case author-student interaction, which the commissioners viewed as problematic.
DISCUSSION
The PBL Commission completed their review, presented their recommendations to the Department faculty, and received final approval for a curricular update in July 2000. The prompt and timely completion of their work allowed for these structural changes to be implemented in the fall semester of the 2000-2001 academic year (Table 7).
Table 7.
Pharmacy Students' Course Grades in the Knowledge, Problem-solving, and Group Portion of a Problem-based Learning Course, %
KN = knowledge; PS= problem-solving; GR = group
To rectify the misalignment between curricular intent and test assessment, the Pharmaceutical Care course series was restructured. This 8-credit hour course that formerly yielded a single grade, which was the average of performance measures over an 8-week block, was divided into 3 separate and individually graded courses based upon Bloom's taxonomy of learning: Knowledge and Comprehension (3 credit hours), Problem-solving (3 credit hours), and Group (2 credit hours).5 Content examinations were recast to minimize problem-solving and to focus on knowledge recall. The format was no longer patient case-based, but consisted of multiple-choice, listing, matching, and true or false questions. A mid-point examination was also instituted to reduce student stress over the perceived “all or nothing” nature of a comprehensive final. The new Problem-solving examination remained at the end of each block. In order to minimize content knowledge, this test was designed to be administered open book. Questions were constructed to assess higher-level learning: application, analysis, synthesis, and evaluation.5 Education theorists believe that these abilities move up a pyramid in a hierarchical manner. Block I problem-solving focuses on application, thereafter moving in Block II to analysis, Block III to synthesis, and ending with problem-solving focused on evaluation aspects of clinical care in Block IV. The Problem-solving examination is now given in 2 separate 4-hour sessions on the last day of each 8-week block. A wide variety of standard reference materials are available at the test site, but students may not access their own prepared study materials or electronic media.
To address the PBL Commission' s concerns over test preparation, 2 standing committees were formed to review the examination materials submitted by case authors. The Knowledge and Comprehension Committee reviews submissions for appropriateness and clarity as well as accuracy. Committee members are empanelled for an entire academic year and are responsible for vetting the preparation of 2 tests per 8-week block or 8 examinations per academic year. This Content Committee meets for approximately 2 hours each week. The Problem-solving Examination Committee members also serve a 1-year term, but they compose the examination questions themselves to ensure that each open-book test assesses the appropriate problem-solving skills. This committee meets for one hour each week to prepare a single examination for each 8-week block, or 4 examinations per academic year. These committees consist of 3 members, plus a chair and a chair-elect. The chair of each committee is also the course director for that respective component of the Pharmaceutical Care course series. Faculty participation on a committee or as a course director is voluntary. However, full faculty participation is encouraged, so that case authors develop test-writing skills and gain experience with the examination review process.
The revision of the Pharmaceutical Care course series allowed for the implementation of a student remediation process. The prerequisites for student advancement were adjusted to allow a student who fails 1 course to progress to the P4 year if the course is successfully remediated. A remediation period is now offered during the summer term. Because the number of students needed to constitute a small group during the remediation period cannot be guaranteed each year, a student who fails a Group course is allowed to advance, but their professional experience rotations will be interrupted so that they may repeat the Group course they failed when it is offered to the following P3 class. This allows students to participate in graduation ceremonies with their respective entering class, as those requiring Group remediation only need to return to complete the missed P4 rotation after graduation.
To provide students with a formal opportunity to interact with faculty case authors, a weekly “case management conference” (CMC) was instituted in the time period during which pharmacy grand rounds were previously held. These conferences were intended to allow students to directly interact with the content expert who prepared the case considered that week. CMCs were the venue for students to ask questions or to discuss problems they encountered with the progressive disclosure case. However, the CMC was not intended as a forum to review the case, narrow down the information presented, or highlight potential examination material. CMCs were to consist of presentations of alternate patient scenarios or clinical vignettes, which might illuminate or elaborate on learning issues developed during group sessions. The case author or their designee was to lead the discussion, but they were cautioned not to lecture, as didactic presentations would be contrary to a self-directed learning model.
Recent Curricular Revisions (2001-2005)
The PBL Commission recommendations were put into practice with departmental consent, but they did not fully rectify several areas of concern. Students agreed with the rationale for the tripartite partitioning of the Pharmaceutical Care course series grade. But they continued to express dissatisfaction with the seemingly subjective assessment of their small group activities. Judgments regarding group performance were the sole purview of the faculty facilitator. Despite attempts to delineate performance domains on a standardized instrument, statistical analysis revealed that robust differences in faculty member assessments remained. An attempt to correct these discrepancies with mathematical adjustments to submitted Group grades that took into account differences in rater variability also proved problematic. Students received a “raw” grade from their faculty facilitator, which then underwent a statistical adjustment resulting in a “final” grade for group performance. Grade adjustment was abandoned when it became evident that such modeling destabilized grade distributions. Student concern for the objectivity of Group grading was eventually addressed by the weekly rotation of facilitators over a PBL block. Students remained together for 8 weeks so that group cohesion was not disrupted, but they were now assessed by 8 different faculty facilitators. It was hoped that faculty rotation would balance differences in their assessments of student performance over time.
Students and faculty also raised concerns over the weekly CMCs. These conferences were intended to be interactive, to provide students an opportunity to directly question content experts. A student survey revealed that CMCs were not viewed favorably and were only seen as helpful when faculty members conducted a didactic content review or provided direction with regard to upcoming examination material. Many faculty members found it difficult to actively engage a large group of 70 to 80 students, and so some reverted to a lecture format. As these adaptations were contrary to the goals of an active, self-directed learning model, an administrative decision was made to discontinue CMCs for the academic year 2005-2006. Students are now provided with a list of faculty members' expertises and encouraged to contact them individually with any questions. Large group sessions with a case author or a content expert may be organized by the course directors if requested by the students; however, no regularly scheduled case conferences are currently offered.
SUMMARY
Pharmacy education should promote lifelong professional learning through an emphasis on active, self-directed learning. Pharmacy curricula should promote teaching strategies that ensure graduate competence in critical thinking and problem-solving. The University of Mississippi School of Pharmacy developed and implemented an innovative PBL model in accord with these educational objectives. Fundamental to the success of any new educational endeavor is the value placed on input from those involved: students, faculty members, and administrators. Diligent attention to the concerns of stakeholders is necessary for the acceptance and continuing improvement of programmatic innovations. In this manuscript, we share an overview of our experiences in the hope that other educators may learn from our successes and failures. Those seeking to move their institutional curricula toward student-centered learning should be cognizant of the teaching space and personnel demands that small group organization requires and the need to obtain student support at the inception of any educational reorientation as well as to solicit their ongoing input for curricular development. Our PBL program has evolved over 10 years to fulfill its objectives, as our students are more engaged in their own learning processes and more aware of the need for continuing professional education after graduation. We hope that our PBL model will better prepare our graduates to become lifelong learners and assume leadership roles in pharmacy.
ACKNOWLEDGEMENTS
The authors would like to express our gratitude to Dr. Phil Bushby, Mississippi State University School of Veterinary Medicine, for his assistance in the development our PBL model, to Dean Kenneth Roberts for his support of the initial proposal, and to Dean Barbara Wells and Associate Dean Marvin Wilson for their continued support of this educational endeavor.
Appendix 1. Treatment Plan Outline.
Appendix 2. Example of Minicase.
Appendix 3. Example of Minicase Facilitator Guide.
REFERENCES
- 1. Accreditation Manual. 9th edition. Chicago, Illinois: American Council on Pharmaceutical Education; 2000:52-3.
- 2.Papa FJ, Harasym PH. Medical curriculum reform in North America, 1765 to the present: a cognitive science perspective. Academic Med. 1999;74:154–64. doi: 10.1097/00001888-199902000-00015. [DOI] [PubMed] [Google Scholar]
- 3. Bonwell CC, Eison JA. Active learning: creating excitement in the classroom. ERIC Digest. 1991;ED340272. Available at: http://www.ntlf.com/html/lib/bib/91-9dig.htm. Accessed December 8, 2005.
- 4.Barrows HS. Practice-Based Learning: Problem-Based Learning Applied to Medical Education. Springfield, Ill: Southern Illinois University School of Medicine; 1994. [Google Scholar]
- 5.Bloom BS. Taxonomy of Educational Objectives: Book 1, Cognitive domain. New York: Longman; 1956. [Google Scholar]