Abstract
Objectives
To describe the extent of psychiatric pharmacy instruction in US pharmacy curricula, including course and faculty characteristics and mental health topics taught in clinical therapeutics-based courses.
Methods
An 11-item survey instrument (54% response) was developed and mailed to 91 colleges and schools of pharmacy.
Results
Over 75% of colleges and schools employed a psychiatric pharmacist; however, less than 50% of faculty teaching psychiatric pharmacy content were psychiatric pharmacy specialists as defined in the study. All colleges and schools included psychiatric topics as part of a therapeutics-based course with an average of 9.5% of course content devoted to these topics. About 25% of colleges and schools offered elective didactic courses in psychiatric pharmacy. Only 2 schools required a psychiatric pharmacy advanced pharmacy practice experience (APPE), but about 92% offered elective APPEs. The mean number of hours spent on lecture- and case-based instruction across all colleges and schools was highest for depression and lowest for personality disorders.
Conclusions
There is a need for colleges and schools of pharmacy to better identify and standardize the minimal acceptable level of didactic instruction in psychiatric pharmacy as well as the minimal level of specialty qualifications for faculty members who teach this subject.
Keywords: psychiatric pharmacy, pharmacy education, curriculum, mental health
INTRODUCTION
Approximately 26% of Americans aged 18 years and older suffer from a diagnosable mental illness.1 In addition, mental illness accounts for over 15% of the burden of disease in established market economies, such as the United States.2 Not surprisingly, psychotropic medications represent approximately 13% of the top 300 most frequently prescribed medications in the United States.3 In addition to dispensing these medications, pharmacists can play vital roles in the treatment of mentally ill patients,4 and activities such as medication counseling and monitoring of therapy have been documented to improve both satisfaction and adherence to drug therapy in this patient population.5 Clearly, an appropriate knowledge base regarding mental illnesses and psychopharmacotherapy is crucial for the new practitioner.
Faculty credentials in this specialty area of practice are also important to ensure relevant and complete instruction. Although not large in number, residencies (approximately 20) and fellowships (fewer than 10) in psychiatric pharmacy are available to those pharmacists desiring to practice pharmaceutical care and/or conduct research in mental health settings. Psychiatric pharmacy was recognized as a specialty by the Board of Pharmaceutical Specialties in 1992,6 and pharmacists have been eligible to be granted board certification in this field since 1996. There are currently 463 board-certified psychiatric pharmacists (BCPP). Ideally, academicians with these types of qualifications would teach psychiatric content in colleges and schools of pharmacy.
While the scope and nature of the teaching of a number of pharmacy topics have been documented previously,7-18 a review of the literature revealed that no published studies have examined the status of psychiatric pharmacy education within pharmacy school curricula since the early nineties.19 The current study was undertaken to update and more thoroughly describe the extent of psychiatric pharmacy instruction provided by colleges and schools of pharmacy in the United States, including course and faculty characteristics, specific mental health topics taught in clinical therapeutics-based courses, and course time dedicated to those topics.
METHODS
A survey instrument was developed based on previous examples published in the literature,7-15 pre-tested by the authors, and approved by the Samford University Institutional Review Board. The survey instrument was divided into 3 sections. Section 1 dealt with background information, including: designation of school as public or private; total student enrollment; faculty full-time equivalents; percentage of therapeutics-based didactic course content spent on psychiatric disorders; number of psychiatric pharmacists on the faculty; plans to hire psychiatric pharmacist(s) within the next 5 years; required and elective didactic courses or APPEs in psychiatric pharmacy and the percentage of each pharmacy cohort taking these elective courses; and availability of psychiatric pharmacy practice sites for faculty members. Section 2 dealt with course content (ie, didactic therapeutics-based course sequence), including specific topics taught, number of contact hours of lecture-based instruction per topic, and number of contact hours of case-based instruction per topic. Section 3 dealt with instructor characteristics, including employment status of each instructor (eg, full-time or part-time); delineation of courses taught by each instructor (eg, clinical therapeutics-based course, psychiatric pharmacy didactic elective, psychiatric pharmacy APPE); and description of instructor qualifications (eg, residency, fellowship, board certification). For the purposes of this study, a psychiatric pharmacist was defined as one who had completed at least one of the following: a residency or fellowship in psychiatric pharmacy or board certification in psychiatric pharmacy practice (ie, BCPP). A copy of the survey instrument may be obtained from the authors.
In Spring 2004 a cover letter, survey instrument, and preaddressed stamped enveloped were mailed using the modified Dillman method20 to the dean at each of the 91 colleges and schools of pharmacy in the United States accredited by the Accreditation Council for Pharmacy Education (ACPE). The cover letter requested that the survey instrument be forwarded to the most appropriate faculty member to complete the information in the survey. After 1 month a reminder card was mailed; however, no second mailing of the survey instrument was done because a satisfactory response rate (>50%) was achieved. Survey responses were coded, entered into a Microsoft Excel database and analyzed using descriptive statistics.
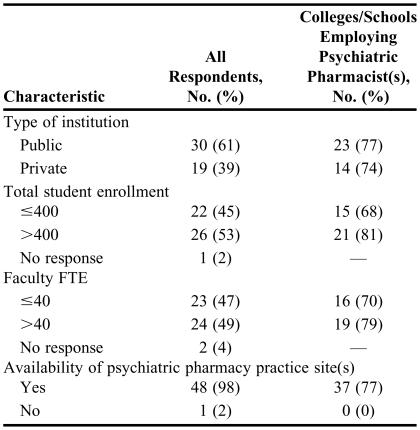
RESULTS
Fifty-one survey instruments were returned (56% response rate); however, 2 were eliminated from the study because they were from new colleges and schools that had not yet finalized their curriculum and therefore could not complete the survey instrument. The resulting usable response rate was 54% (49/91). Some survey instruments were returned but incomplete; therefore, the results discussed for each question are based on the number of actual respondents to that item and the total number of responses may vary between items. Table 1 contains a summary of respondent demographics. The majority of respondent colleges and schools were publicly funded. The mean total student enrollment was 525 ± 361 (range 100-2000) and the mean number of full-time faculty members/positions was 46.3 ± 19.3. Colleges and schools that employed a psychiatric pharmacist were somewhat more likely to have a larger student enrollment and possess a greater number of full-time faculty members. Only one school claimed to have no potential practice site in psychiatric pharmacy available to faculty members and students.
Table 1.
Demographics of Colleges and Schools of Pharmacy Responding to a Survey on Instruction of Mental Health and Psychiatric Pharmacy
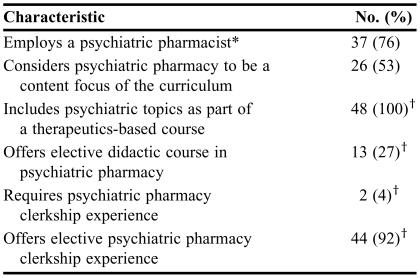
Table 2 provides an overview of psychiatric pharmacy in US colleges and schools of pharmacy. Approximately three fourths of the colleges and schools employed at least 1 psychiatric pharmacist. Of these colleges and schools, 62% (23/37) employed 1 psychiatric pharmacist, while 38% (14/37) employed more than 1 psychiatric pharmacist. Examining the total for all colleges and schools, only 3.3% of reported full-time faculty positions was dedicated to this specialty area. Of the 12 colleges and schools that did not employ a psychiatric pharmacist, 4 planned to do so within the next 5 years.
Table 2.
Overview of Psychiatric Pharmacy in US Colleges and Schools of Pharmacy (N = 49)
*For the purposes of this study, a psychiatric pharmacist was defined as one who had completed at least one of the following: a residency or fellowship in psychiatric pharmacy or board certification in psychiatric pharmacy practice (ie, BCPP)
†Only 48 colleges and schools responded to this item
Over 50% (26/49) of colleges and schools considered psychiatric pharmacy to be a content focus of their curriculum. All colleges and schools included psychiatric topics as part of a therapeutics-based course, and the mean percentage of the course dedicated to such topics was 9.5% ± 3.9% (range 2.0%-20.0%). Interestingly, the amount of the course dedicated to psychiatric topics varied little between those colleges and schools employing a psychiatric pharmacist and those not employing a psychiatric pharmacist (9.7% vs. 9.0%, respectively). Only about one fourth of colleges and schools offered elective didactic courses in psychiatric pharmacy, but the mean student enrollment (ie, percentage of each pharmacy cohort taking the course) in such cases was 26.2% ± 18.8% (range 2.0%-55.0%). Only 2 colleges and schools required a psychiatric pharmacy APPE. Over 90% of colleges and schools offered an elective psychiatric pharmacy APPE, and the mean student enrollment in such cases was 20.2% ± 19.5% (range 3.0%-60.0%).
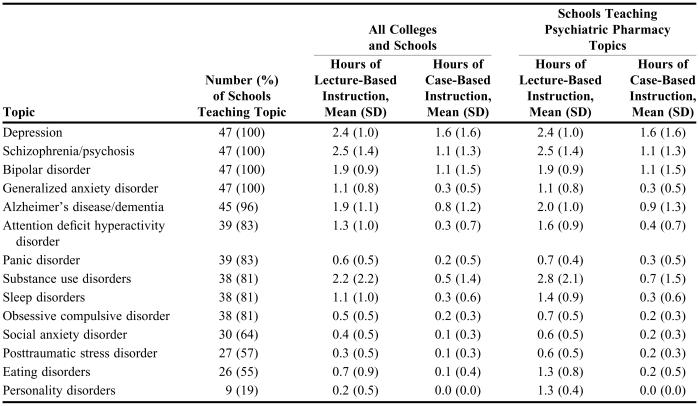
Table 3 details the various topics covered in clinical therapeutics-based courses. All respondent colleges and schools covered the topics of depression, schizophrenia, bipolar disorder, and generalized anxiety disorder. Those topics taught in fewer than two thirds of colleges and schools included social anxiety disorder, posttraumatic stress disorder, eating disorders, and personality disorders. For those colleges and schools teaching the topics, the most amount of time was dedicated to depression and schizophrenia (4.0 hours and 3.6 hours, respectively), whereas the least amount of time was dedicated to social anxiety disorder and posttraumatic stress disorder (0.8 hours). Psychiatric topics were usually taught via lecture-based vs. case-based methods, with approximately three fourths of time dedicated to the former. Depression, schizophrenia, and bipolar disorder had more time dedicated to case-based instruction compared to other psychiatric topics.
Table 3.
Psychiatric Pharmacy Topics Taught in Clinical Therapeutics Courses (n = 47)
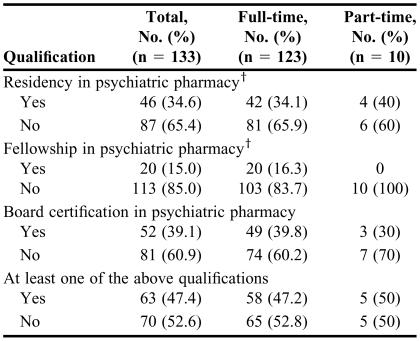
Faculty instructors of psychiatric content were employed full-time in 92% of cases and part-time in 8% of cases. Only approximately one third of instructors had completed specialized postgraduate training in psychiatric pharmacy (residency ± fellowship), and about 40% had obtained board certification in psychiatric pharmacy (Table 4). Fewer than half (47.4%) of the instructors possessed at least 1 of the aforementioned qualifications. Psychiatric pharmacists typically taught in both clinical therapeutics-based courses (92.1%) and psychiatric pharmacy APPEs (85.7%), whereas nonpsychiatric pharmacists were far more likely to be utilized in clinical therapeutics-based courses (98.6%) than in psychiatric pharmacy APPEs (11.4%).
Table 4.
Qualifications of Full-Time and Part-Time Instructors of Psychiatric Subject Matter in US Colleges and Schools of Pharmacy*
*In either a clinical therapeutics-based course, didactic elective course, or clerkship rotation
†Sixteen instructors had completed both residency and fellowship training in psychiatric pharmacy
DISCUSSION
The majority (75.5%) of US colleges and schools of pharmacy employed at least 1 psychiatric pharmacist, the likelihood of which appeared to be marginally influenced by total student enrollment and total number of full-time faculty members, but uninfluenced by type of institution (eg, public or private). This number is lower than that reported in 1991when 96.7% (58/60) of colleges and schools reported employing at least 1 psychiatric pharmacist.19 However, the term was defined in that study as any faculty member practicing specifically in psychiatric pharmacy, while the current study addressed only faculty members who had completed a specialized residency and/or fellowship or had been board certified in psychiatric pharmacy.
Psychiatric pharmacy subject matter was found in all therapeutics-based courses. Although having increased significantly since the previous study,19 elective didactic courses were still relatively rare (offered by only 27.1% of colleges and schools in the current study vs. 9.0% of doctor of pharmacy programs in 1991). The percentage of colleges and schools that offered elective psychiatric experiences were unchanged from the previous study19 (91.7% in the current study vs. 92.0% of doctor of pharmacy programs in 1991), while required practice experiences decreased from 31.0% of doctor of pharmacy programs in 199119 to 4.2% in the current study. Student interest appeared to be strong in elective courses (didactic and APPE) based on mean student enrollments, so it would seem that colleges and schools not currently offering such courses should consider doing so.
Most colleges and schools dedicated between 5.5% to 13.5% of therapeutics-based course content to psychiatric disorders and their treatment, and the time dedicated to these topics varied little between colleges and schools that employed a psychiatric pharmacist and those that did not. It was not possible to compare these figures with the study by Marken and Evans19 because they reported average number of didactic hours devoted to psychopharmacy in the curriculum while we asked respondents to indicate the percentage of a therapeutics-based course devoted to these topics. Not surprisingly, teaching efforts were geared toward the major mood disorders and schizophrenia. However, there was a fair amount of variability between colleges and schools in terms of which specific psychiatric topics were taught, the extent to which they were taught, and the pedagogy used to teach them. This is an area of the curriculum where colleges and schools of pharmacy should evaluate the level of their instruction in order to be in line with other colleges and schools as well as to strike the well-known balance between training students to be competent generalists vs. specialized practitioners.11 Given the rather esoteric nature of psychiatric disorders, the relatively small amount of case-based instruction was an unexpected finding.
Most faculty members who taught psychiatric subjects had not received postgraduate training or board certification in psychiatric pharmacy. This was especially true for those teaching in therapeutics-based courses as opposed to APPEs. Of course, this finding may well be due to the relative scarcity of such highly qualified practitioners, especially given much publicized difficulties in the academy to recruit and retain qualified faculty members as well as the increase in the number of colleges and schools in order to meet the demand for more pharmacists.21
Perhaps the greatest limitation to this study was that those colleges and schools with at least 1 psychiatric pharmacist on the faculty may have been more inclined to respond to the survey--and to do so more completely and accurately--than those without a psychiatric pharmacist on the faculty. Also, we counted on deans to forward the survey instrument to the most appropriate person in the school; thus, the most knowledgeable person may not have been the one to actually complete the survey. Finally, we failed to inquire about teaching of developmental disorders in section 2 of the survey instrument. However, we did provide an “other” category, and none of the respondents indicated the teaching of this particular topic.
CONCLUSIONS
This study found that the provision of instruction in psychiatric pharmacy varies widely between colleges and schools, especially in regard to didactic content. Given the escalating number of prescriptions for psychotropic medications and growing complexity of psychopharmacotherapeutics, there is a need for colleges and schools of pharmacy to better identify and standardize the minimal acceptable level of didactic instruction in this important area as well as the minimal level of postgraduate training and board certification for faculty members who teach this subject.
ACKNOWLEDGEMENTS
This study was funded by a Samford University Faculty Development Grant. Presented as a poster at the American Association of Colleges of Pharmacy Annual Meeting, Salt Lake City, Utah, July 11, 2004.
REFERENCES
- 1. National Institute of Mental Health. The numbers count: mental disorders in America (updated 2006). Available at www.nimh.nih.gov/publicat/numbers.cfm. Accessed June 21, 2006.
- 2. National Institute of Mental Health. The impact of mental illness on society. Available at www.nimh.nih.gov/publicat/burden.cfm. Accessed June 27, 2006.
- 3. The top 300 prescriptions for 2005 by number of US prescriptions dispensed. Available at www.rxlist.com/top200.html. Accessed June 21, 2006.
- 4.Hitchens K. The pharmacist's role in mental health. Drug Top. 1997;141(suppl):28s–37. [Google Scholar]
- 5.Bullman DC, Svarstad BL. Effects of pharmacist monitoring on patient satisfaction with antidepressant medication therapy. J Am Pharm Assoc. 2002;2:36–43. doi: 10.1331/108658002763538053. [DOI] [PubMed] [Google Scholar]
- 6. Frequently Asked Questions. Board of Pharmaceutical Specialties. Available at: www.bpsweb.org/FAQs/FAQs.shtml. Accessed June 26, 2006.
- 7.Monk MT, Brown TR, Garner DD, Smith MC. National survey on the status of home health care instruction in US schools and colleges of pharmacy. Am J Pharm Educ. 1991;55:120–5. [Google Scholar]
- 8.Cooper JB, Brock TP, Ives TJ. The spiritual aspects of patient care in the curricula of colleges of pharmacy. Am J Pharm Educ. 2003;67(2) Article 15. [Google Scholar]
- 9.Keitt SK, Wagner C, Tong C, Marts SA. Positioning women's health curricula in US medical schools. Medscape Gen Med. 2003;5:1–9. [PubMed] [Google Scholar]
- 10.Dismuke SE, Burns BW, Moranez CA, Ellerbeck E. Curriculum assessment for prevention topics and the population perspective. Am J Prevent Med. 2001;20:286–90. doi: 10.1016/s0749-3797(01)00295-1. [DOI] [PubMed] [Google Scholar]
- 11.Bednarczyk EM, Mayer D, Wong LK. Nuclear pharmacy instruction in colleges and schools of pharmacy. Am J Pharm Educ. 2004;68(1) Article 6. [Google Scholar]
- 12.Shields KM, McQueen CE, Bryant PJ. Natural products education in school of pharmacy in the United States. Am J Pharm Educ. 2003;67(1) Article 10. [Google Scholar]
- 13.Low JK, Baldwin JN, Greiner GE. Pediatric pharmacy education for US entry-level Doctor of Pharmacy programs. Am J Pharm Educ. 1999;63:323–7. [Google Scholar]
- 14.Heske SM, Hladic WB, III, Laven DL, Lavula MP., Jr Status of radiologic pharmacy education at colleges of pharmacy. Am J Pharm Educ. 1996;60:152–60. [Google Scholar]
- 15.Miller SJ. Nutrition education in colleges of pharmacy. Am J Pharm Educ. 1995;59:379–82. [Google Scholar]
- 16.Rascati KL, Conner TM, Draugalis JR. Pharmacoeconomic education in US schools of pharmacy. Am J Pharm Educ. 1998;62:167–9. [Google Scholar]
- 17.Rowell DM, Kroll DJ. Complementary and alternative medicine education in United States pharmacy schools. Am J Pharm Educ. 1998;62:412–9. [Google Scholar]
- 18.Johnson MS, Latif DA, Gordon B. Medication error instruction in schools of pharmacy curricula: a descriptive study. Am J Pharm Educ. 2002;66:364–71. [Google Scholar]
- 19.Marken PA, Evans RL. Survey of psychopharmacy curricula and faculty at schools of pharmacy. Am J Pharm Educ. 1993;57:330–2. [Google Scholar]
- 20.Dillman DA. Mail and Internet Surveys: The Tailored Design Method. New York, NY: Don Wiley & Sons, Inc; 2000. [Google Scholar]
- 21.Leslie S. Pharmacy workforce: Increasing the numbers and holding to high standards of excellence. Am J Pharm Educ. 2005;69(5) Article 93. [Google Scholar]