Abstract
OBJECTIVE
Uterine leiomyomata represent a major public health problem for black women in the United States, but limited data are available on age–incidence curves in this high-risk population. We estimated overall and age-specific incidence rates for self-reported uterine leiomyomata in a large cohort of African-American women in the United States.
METHODS
Data were derived from the Black Women’s Health Study, an ongoing prospective cohort study of 59,000 black women from across the United States who were aged 21–69 years at baseline (ie, 1995). From March 1997 through March 2001, we followed up 22,895 premenopausal women with no prior diagnosis of uterine leiomyoma. Poisson regression was used to estimate overall and age-specific incidence rates and 95% confidence intervals (CIs) for self-reported uterine leiomyoma. In a subset of 248 patients who were selected randomly from the total case group, the self-reported diagnosis was verified in 96% of cases who released their medical records.
RESULTS
During 76,711 woman-years of follow-up, 2,637 incident cases of uterine leiomyomata reported as confirmed by pelvic examination (n = 358), ultrasonography (n = 2,006), or hysterectomy (n = 273) were observed. Incidence rates per 1,000 woman-years were 34.4 (95% CI 33.1–35.7) for all cases combined, 29.7 (95% CI 28.5–30.9) for cases confirmed by ultrasonography or hysterectomy, and 3.6 (95% CI 3.2–4.0) for cases confirmed by hysterectomy. The incidence rate peaked at ages 40–44 years for all cases combined (incidence rate 45.6, 95% CI 42.0–49.5) and for cases confirmed by ultrasonography or hysterectomy (incidence rate 39.8, 95% CI 36.5–43.4), and peaked at ages 45–49 years for cases confirmed by hysterectomy (incidence rate 8.3, 95% CI 6.4–10.7).
CONCLUSION
Overall incidence rates for self-reported uterine leiomyomata were consistent with other U.S studies in black women and confirmed a high burden of disease in this population. Age-specific incidence rates showed a later peak incidence than that observed among U.S. black women in previous studies.
LEVEL OF EVIDENCE
II-2
Uterine leiomyomata are the most common tumors of the female reproductive tract and the leading indication for hysterectomy among women in the United States.1 Black women are disproportionately affected by this condition. The incidence of uterine leiomyomata is greater in black women than in white women,2–4 and black women have more severe disease at the time of diagnosis.5
Incidence rates of uterine leiomyoma diagnoses in U.S. populations are based largely on data from the National Hospital Discharge Survey,2,6 the National Health and Nutrition Examination Survey Epidemiologic Follow-up Study,4 and the Nurses’ Health Study II.3 Estimated rates vary according to case definition,7 ranging from 9.2 per 1,000 woman-years for diagnoses confirmed by ultrasonography or hysterectomy3 to approximately 2.0 per 1,000 woman-years for diagnoses confirmed by hysterectomy.2–4 Rates among women hospitalized for gynecologic conditions unrelated to pregnancy (3.0 per 1,000 woman-years) are similar to rates for hysterectomy-confirmed diagnoses.6 Regardless of case definition, rates of uterine leiomyomata increase with age throughout the reproductive years.2,3,6,8,9
Incidence rates among black women are 2 to 3 times higher than rates among white women,2–4 and the higher rates among black women are evident at all ages.3,6 Cumulative incidence data derived from a U.S. cross-sectional study that screened all participants with ultrasonography also suggest higher rates for black women.9 One question that has emerged from the incidence data and from earlier case-series data5,10 is whether black women have an earlier peak age at diagnosis than white women. To date, the most definitive data on race-specific incidence rates come from the Nurses’ Health Study II, which suggests that self-reported diagnoses confirmed by ultrasonography or hysterectomy peak earlier among black women (35–39 years) than among white women (40–44 years).3 However, the Nurses’ Health Study II rates were based on only 140 black cases (5% of total case group). Using data from the Black Women’s Health Study, a large prospective cohort study of black women in the United States, we estimated overall and age-specific incidence rates of self-reported uterine leiomyomata according to age and method of diagnostic confirmation.
MATERIALS AND METHODS
The Black Women’s Health Study is an ongoing prospective cohort study that was established in 1995, when approximately 59,000 black women in the United States aged 21–69 years were enrolled through self-administered questionnaires mailed to subscribers of Essence magazine, members of black professional organizations, and friends and relatives of early respondents.11 The baseline questionnaire elicited information on demographic and behavioral characteristics, health care use, and medical conditions. On the 1997 questionnaire, participants were asked “what is your race?” and to select all that applied from the following categories: “black,” “white,” “Asian or Pacific Islander,” or “American Indian or Alaskan Native.” Those who selected “black,” regardless of any other group selected, were retained in the cohort. Six percent of the sample was foreign-born (54% Caribbean, 7% Africa, 39% South or North America/Europe/Asia/other), and less than 2% reported Hispanic ethnicity. The cohort is followed every 2 years by postal questionnaire, and more than 80% of the original cohort has completed a questionnaire in each follow-up cycle. Respondents in the Black Women’s Health Study represent various geographic regions of the United States, with most residing in California, New York, Illinois, Michigan, Georgia, and New Jersey. The study protocol was approved by the institutional review boards of Boston University Medical Center and Howard University Cancer Center.
Follow-up for the present analysis began in 1997, the start of the second questionnaire cycle, because self-reported method of confirmation for uterine leiomyoma was first elicited on the 1999 questionnaire. Of the 53,279 women who completed the 1997 questionnaire, we restricted the sample to premenopausal women because uterine leiomyomata are rare after menopause.12 We therefore excluded women who reported natural menopause (n = 5,143), hysterectomy (n = 6,625), bilateral oophorectomy (n = 4,175), medication-induced menopause (n = 218), or unknown menopausal status (n = 522). We further excluded women who reported a diagnosis of uterine leiomyomata before 1997 (n = 10,450), who reported the condition without information on year of diagnosis (n = 99) or method of confirmation (n = 208), who did not complete a follow-up questionnaire (n = 2,193), or who had missing data on key stratification variables (n = 751). The remaining 22,895 women were followed for incidence of uterine leiomyomata during the subsequent 4-year period. The small proportion of women who were lost to follow-up or who had incomplete covariate data had lower educational attainment than respondents but were similar with respect to age, parity, body mass index, and other risk factors for uterine leiomyomata.
On the 1999 and 2001 follow-up questionnaires, women were asked whether they had been diagnosed with “fibroids in uterus” in the previous 2-year interval, the calendar year in which they were first diagnosed, and whether their diagnosis was confirmed by “pelvic exam” and/or by “ultrasound/hysterectomy.” Among cases reporting confirmation by “ultrasound/hysterectomy,” a diagnosis was considered “hysterectomy-confirmed” if the woman reported hysterectomy on the same questionnaire and “ultrasonography-confirmed” otherwise. A diagnosis was considered “confirmed by pelvic examination” if only that method was reported.
Incident cases were defined as women who self-reported a first diagnosis of leiomyomata that was confirmed by pelvic examination, ultrasonography, or hysterectomy. In the present study, “incident” refers to the initial diagnosis rather than the true onset of uterine leiomyomata, which could differ by an extended time period if tumors were present before they became palpable or symptomatic.12 The diagnosis of uterine leiomyoma often is suspected when an enlarged irregular uterine contour is palpable on pelvic examination. Ultrasonography is the standard used to confirm diagnoses.12 Ultrasonography has high sensitivity (99%) and specificity (91%) relative to histologic evidence.13,14 Because histologically confirmed cases represent only 10–30% of cases for whom ultrasonography evidence is available and studies restricted to histologically confirmed cases may spuriously identify risk factors associated with large tumor size, symptoms, or treatment preference,15 we examined all 3 methods of confirmation. For comparisons of peak age at diagnosis across studies, however, we restricted our case group to cases confirmed by ultrasonography or hysterectomy because diagnoses confirmed only by pelvic examination may represent other pathology.13 This definition also was used by the Nurses’ Health Study II, a prospective study with similar methodology to the Black Women’s Health Study.3
We assessed the accuracy of self-report in a random sample of 248 ultrasonography- or hysterectomy-confirmed cases. These cases were mailed supplemental surveys regarding their initial date of diagnosis, method of confirmation, symptoms, and treatment, and they were asked for permission to review their medical records. We obtained medical records from 126 of the 128 women who gave us permission and verified the self-report by medical record in 121 (96%). Among the 188 (76%) cases who completed the supplemental survey, 71% reported leiomyoma-related symptoms before being diagnosed with the condition. This proportion was higher among hysterectomy-confirmed cases (79%). When cases were asked how their diagnosis came to clinical attention, 55% of cases reported they were diagnosed because they sought medical care for leiomyoma-related symptoms; 32% were diagnosed during a routine pelvic examination, and the remaining 13% were diagnosed while receiving care for some other condition (with more than 85% citing “pregnancy” as the other condition).
No statistically significant differences were observed between cases who did and did not release their medical records with respect to important demographic and lifestyle factors (age, body mass index, education, oral contraceptive use, recency of Pap test, and health insurance coverage: χ2 test P > .2); self-reported method of confirmation (64% ultrasound examination compared with 71% hysterectomy, P = .55); the report of symptoms before the initial diagnosis (73% compared with 66%, P = .31); the type of presenting symptoms (menorrhagia: 56% compared with 47% [P = .28]; pelvic pain: 48% compared with 42% [P = .47]; frequent urination: 21% compared with 25% [P = .53]; infertility: 10% compared with 12% [P = .89]); or how initial diagnosis was made (sought care for leiomyoma-related symptoms: 57% compared with 46% [P = .18]; diagnosed during a routine pelvic examination: 31% compared with 34% [P = .64]; diagnosed while receiving care for another condition: 10% compared with 14% [P = .42]). Therefore, the cases who released their medical records appeared to be representative of the larger case group.
Woman-years at risk were calculated from the start of follow-up (March 1997) until the diagnosis of uterine leiomyomata, menopause, death, loss to follow-up, or end of follow-up (March 2001), whichever came first. Age was updated at the start of each questionnaire cycle. Incidence rates for each age category were computed as the number of incident cases divided by the woman-years accumulated. Poisson regression16 was used to estimate overall and age-specific incidence rates and 95% confidence intervals (95% CIs) for self-reported uterine leiomyomata confirmed by pelvic examination, ultrasonography, or hysterectomy. Analyses were repeated within strata of education (≤12, 13–16, 17 + years), oral contraceptive use (current compared with never), cigarette smoking (current, former, never), body mass index (< 25, 25–29, 30+ kg/m2), and geographic region of residence (West, Midwest, South, Northeast). All analyses were conducted using SAS statistical software (SAS Institute, Cary, NC).
RESULTS
Baseline characteristics of the sample are shown in Table 1. Participants of the Black Women’s Health Study represented all geographic regions of the United States. Nearly 50% were college-educated, 30% had a body mass index of 30 or greater, and more than 90% reported a recent Pap test. Fifty-seven percent were parous, and 23% were current users of oral contraceptives. During 76,711 woman-years of follow-up, 2,637 incident cases of uterine leiomyomata reported as confirmed by pelvic examination (n = 358), ultrasonography (n = 2,006), or hysterectomy (n = 273) were observed. Incidence rates of uterine leiomyomata per 1,000 woman-years were 34.4 (95% CI 33.1–35.7) for all cases combined, 29.7 (95% CI 28.5–30.9) for diagnoses confirmed by ultrasonography or hysterectomy, and 3.6 (95% CI 3.2–4.0) for diagnoses confirmed by hysterectomy (Table 2).
Table 1.
Characteristics of 22,895 Participants in the Black Women’s Health Study, 1997
| Characteristic | % | |
|---|---|---|
| Demographic and lifestyle factors | ||
| Age (y) | ||
| < 30 | 27.8 | |
| 30–34 | 24.5 | |
| 35–39 | 20.9 | |
| 40–44 | 15.4 | |
| 45–49 | 8.6 | |
| 50+ | 2.8 | |
| Geographic region of residence | ||
| Northeast | 28.0 | |
| South | 31.3 | |
| Midwest | 22.7 | |
| West | 18.0 | |
| Education (y) | ||
| ≤ 12 | 13.2 | |
| 13–15 | 38.0 | |
| 16 | 27.4 | |
| 17+ | 21.4 | |
| Body mass index (kg/m2) | ||
| < 20 | 6.3 | |
| 20–24 | 34.4 | |
| 25–29 | 29.4 | |
| 30+ | 29.9 | |
| Smoking history | ||
| Current | 14.1 | |
| Former | 13.7 | |
| Alcohol consumption, 1+ drinks/d | 3.4 | |
| Papanicolaou test within previous 2 y | 90.5 | |
| Reproductive and hormonal factors | ||
| Age at menarche (y) | ||
| ≤ 11 | 27.6 | |
| 12–13 | 53.5 | |
| 14+ | 18.9 | |
| Parous | 57.5 | |
| Oral contraceptive use, current | 23.1 | |
Table 2.
Rates of Self-Reported Uterine Leiomyomata by Method of Confirmation Among Premenopausal Women From the Black Women’s Health Study, 1997–2001
| Pelvic Exam, Ultrasound, or Hysterectomy
|
Ultrasound or Hysterectomy
|
Hysterectomy
|
|||||
|---|---|---|---|---|---|---|---|
| Woman-Years | n | IR (95% CI) | n | IR (95% CI) | n | IR (95% CI) | |
| Overall | 76,711 | 2,637 | 34.4 (33.1–35.7) | 2,279 | 29.7 (28.5–30.9) | 273 | 3.6 (3.2–4.0) |
| Age (y) | |||||||
| < 30 | 18,966 | 387 | 20.4 (18.5–22.5) | 338 | 17.8 (16.0–19.8) | 4 | 0.2 (0.1–0.6) |
| 30–34 | 19,289 | 628 | 32.6 (30.1–35.2) | 544 | 28.2 (25.9–30.7) | 21 | 1.1 (0.7–1.7) |
| 35–39 | 16,841 | 679 | 40.3 (37.4–43.5) | 583 | 34.6 (31.9–37.5) | 74 | 4.4 (3.5–5.5) |
| 40–44 | 12,637 | 576 | 45.6 (42.0–49.5) | 503 | 39.8 (36.5–43.4) | 103 | 8.1 (6.7–9.9) |
| 45–49 | 6,987 | 296 | 42.4 (37.8–47.5) | 250 | 35.8 (31.6–40.5) | 58 | 8.3 (6.4–10.7) |
| 50+ | 1,991 | 71 | 35.7 (28.3–45.0) | 61 | 30.6 (23.8–39.4) | 13 | 6.5 (3.8–11.2) |
IR, incidence rate per 1,000 woman-years; CI, confidence interval.
Regardless of self-reported method of confirmation, incidence rates tended to increase with age (Table 2). Age-specific incidence rates for diagnoses confirmed by ultrasonography or hysterectomy peaked at ages 40–44 years and then declined. Rates among hysterectomy-confirmed cases peaked at ages 45–49 years. Restriction of the sample to women with a recent Pap test (91%), a marker for pelvic examination, produced the same age-incidence peaks as the full sample (data not shown). Results were similar when we stratified analyses by oral contraceptive use, cigarette smoking, body mass index, and geographic region (data not shown). However, the peak age at diagnosis appeared to vary across levels of education. Compared with all other education groups, women with 17+ years of education had an earlier peak age of diagnosis (35–39 years) among cases confirmed by ultrasonography or hysterectomy (n = 553) and a later peak age of diagnosis (50+ years) among cases confirmed by hysterectomy (n = 43).
Overall incidence rates for uterine leiomyomata according to self-reported method of confirmation were similar to rates found for black women in other U.S. studies (Fig. 1). However, age-specific incidence rates (Fig. 2) showed a later peak age at diagnosis in the Black Women’s Health Study (40–44 years) than that observed for black women in the Nurses’ Health Study II (35–39 years). Rather, the peak age at diagnosis in the Black Women’s Health Study was consistent with the peak observed for white women in the Nurses’ Health Study II (40–44 years).
Fig. 1.
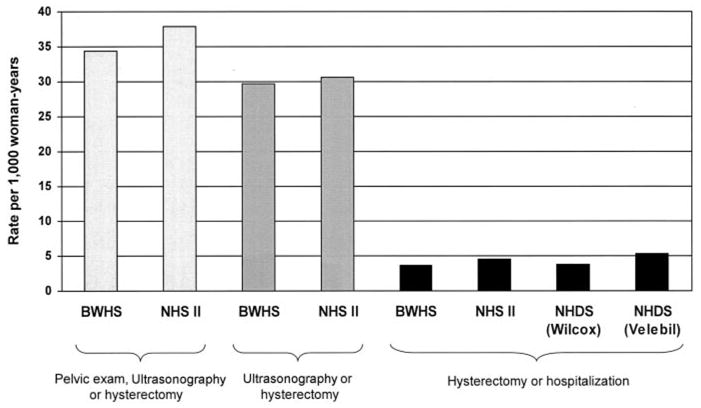
Incidence rates of uterine leiomyomata among black women in the United States according to reported method of detection and study. BWHS, Black Women’s Health Study; NHS, Nurses’ Health Study; NHDS, National Hospital Discharge Survey.
Wise. Rates for Uterine Leiomyomata in Black Women. Obstet Gynecol 2005.
Fig. 2.
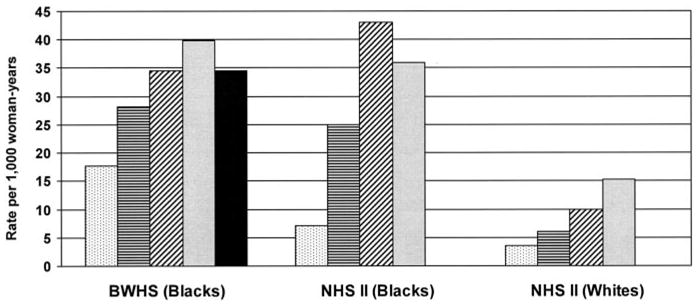
Incidence rates for uterine leiomyomata reportedly detected by ultrasonography or hysterectomy according to age and race (Black Women’s Health Study [BWHS] and Nurses’ Health Study II [NHS II]). Number of cases: BWHS (Blacks) = 2,279, NHS II (Blacks) = 140, and NHS II (Whites) = 2,679. Dotted bar, 25–29 years; horizontal line bar, 30–34 years; diagonal line bar, 35–39 years; gray bar, 40–44 years; solid black bar, 45+ years.
Wise. Rates for Uterine Leiomyomata in Black Women. Obstet Gynecol 2005.
DISCUSSION
The present study estimated incidence rates for self-reported uterine leiomyomata from a large and heterogeneous cohort of black women in the United States. Overall incidence rates were consistent with data from other U.S. studies that included black women.2,3,6 Age-specific incidence rates increased throughout the reproductive years and peaked at ages 40–44 years for cases reported as confirmed by ultrasonography or hysterectomy and at ages 45–49 years for cases reported as confirmed by hysterectomy. The peak age of diagnosis among ultrasonography- or hysterectomy-confirmed cases in the Black Women’s Health Study did not agree with data on black women from the Nurses’ Health Study II (35–39 years). Both studies enrolled convenience samples and used the same outcome definition, but the Black Women’s Health Study, with 2,279 ultrasonography- or hysterectomy-confirmed cases, had a substantially greater number of black cases than the Nurses’ Health Study II, which had 140 cases. Discrepant results also may be attributable to differences in disease awareness, screening practices, and the prevalence of key risk factors.
The Black Women’s Health Study is not a nationally representative sample of black women from the United States. However, prevalence estimates of suspected risk factors for uterine leiomyomata—age at menarche,17 parity,17 body mass index18—are similar to those found in nationally representative studies, with the exception of educational attainment, which is higher in the Black Women’s Health Study relative to the general population. Whereas 85.1% of U.S. black women aged 25–44 years had graduated from high school as of March 1995,19 98.3% of the same-aged participants in the Black Women’s Health Study had graduated from high school. Because the Black Women’s Health Study over-represents women with higher education and because education is positively associated with ultrasonography confirmed uterine leiomyomata, we may have overestimated incidence rates compared with the general population. Participants in the Black Women’s Health Study with 17+ years of education had an earlier peak incidence (35–39 years) than other education groups, but we found the same peak incidence among the total sample (40–44 years) as we did for all education groups other than 17+ years, providing reassurance that these findings may extend to the general population of U.S. black women.
We validated the self-report of uterine leiomyomata through a detailed supplementary questionnaire and review of medical records. We were able to verify the diagnosis in 96% of the cases from whom we obtained medical records. We cannot rule out the possibility that women who released their records reported with greater accuracy than those who did not, although comparisons made with available data did not show any significant differences between groups with respect to reported symptomatology, method of diagnosis, or demographic and lifestyle factors.
Because of the large size of the cohort and the geographic distribution of its participants, it was not feasible to screen all women for uterine leiomyomata. The use of self-reported diagnoses could have resulted in the underestimation of rates because some women with asymptomatic tumors may have been missed. However, it is likely that data from the Black Women’s Health Study more accurately represent the number of women with symptomatic tumors because most cases on the validation survey (71%) reported symptoms before the initial diagnosis of the disease and because a low percentage of cases (13%) were detected incidentally.
Symptomatic disease represents the health burden in reproductive-aged women and has the greatest impact on a woman’s reproductive health, quality of life, and health care use. The high incidence rates for uterine leiomyomata observed in the Black Women’s Health Study are compatible with other U.S. studies3,9 and provide additional evidence that black women are disproportionately affected by the condition. The estimated rates from the present study translate into approximately 3% of premenopausal black women being diagnosed with the condition each year. Uterine leiomyomata are a major pubic health problem for black women in the United States, and efforts toward primary prevention of this condition are needed.
Footnotes
Supported by National Cancer Institute grant CA58420.
References
- 1.Farquhar CM, Steiner CA. Hysterectomy rates in the United States 1990–1997. Obstet Gynecol. 2002;99:229–34. doi: 10.1016/s0029-7844(01)01723-9. [DOI] [PubMed] [Google Scholar]
- 2.Wilcox LS, Koonin LM, Pokras R, Strauss LT, Xia Z, Peterson HB. Hysterectomy in the United States, 1988–1990. Obstet Gynecol. 1994;83:549–55. doi: 10.1097/00006250-199404000-00011. [DOI] [PubMed] [Google Scholar]
- 3.Marshall LM, Spiegelman D, Barbieri RL, Goldman MB, Manson JE, Colditz GA, et al. Variation in the incidence of uterine leiomyoma among premenopausal women by age and race. Obstet Gynecol. 1997;90:967–73. doi: 10.1016/s0029-7844(97)00534-6. [DOI] [PubMed] [Google Scholar]
- 4.Brett KM, Marsh JV, Madans JH. Epidemiology of hysterectomy in the United States: demographic and reproductive factors in a nationally representative sample. J Womens Health. 1997;6:309–16. doi: 10.1089/jwh.1997.6.309. [DOI] [PubMed] [Google Scholar]
- 5.Kjerulff KH, Langenberg P, Seidman JD, Stolley PD, Guzinski GM. Uterine leiomyomas: racial differences in severity, symptoms, and age at diagnosis. J Reprod Med. 1996;41:483–90. [PubMed] [Google Scholar]
- 6.Velebil P, Wingo PA, Xia Z, Wilcox LS, Peterson HB. Rate of hospitalization for gynecologic disorders among reproductive-age women in the United States. Obstet Gynecol. 1995;86:764–9. doi: 10.1016/0029-7844(95)00252-M. [DOI] [PubMed] [Google Scholar]
- 7.Schwartz SM, Marshall LM. Uterine leiomyomata. In: Goldman MB, Hatch MC, editors. Women and health. San Diego (CA): Academic Press; 2000. pp. 240–52. [Google Scholar]
- 8.Ross RK, Pike MC, Vessey MP, Bull D, Yeates D, Casagrande JT. Risk factors for uterine fibroids: reduced risk associated with oral contraceptives [published erratum in Br Med J (Clin Res Ed) 1986;293:1027] Br Med J (Clin Res Ed) 1986;293:359–62. doi: 10.1136/bmj.293.6543.359. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Day Baird D, Dunson DB, Hill MC, Cousins D, Schectman JM. High cumulative incidence of uterine leiomyoma in black and white women: ultrasound evidence. Am J Obstet Gynecol. 2003;188:100–7. doi: 10.1067/mob.2003.99. [DOI] [PubMed] [Google Scholar]
- 10.Kjerulff K, Langenberg P, Guzinski G. The socioeconomic correlates of hysterectomies in the United States. Am J Public Health. 1993;83:106–8. doi: 10.2105/ajph.83.1.106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Rosenberg L, Adams-Campbell L, Palmer JR. The Black Women’s Health Study: a follow-up study for causes and preventions of illness. J Am Med Womens Assoc. 1995;50:56–8. [PubMed] [Google Scholar]
- 12.Stewart EA. Uterine fibroids [review] Lancet. 2001;357:293–8. doi: 10.1016/S0140-6736(00)03622-9. [DOI] [PubMed] [Google Scholar]
- 13.Loutradis D, Antsaklis A, Creatsas G, Hatzakis A, Kanakas N, Gougoulakis A, et al. The validity of gynecological ultrasonography. Gynecol Obstet Invest. 1990;29:47–50. doi: 10.1159/000293299. [DOI] [PubMed] [Google Scholar]
- 14.Dueholm M, Lundorf E, Hansen ES, Ledertoug S, Olesen F. Accuracy of magnetic resonance imaging and transvaginal ultrasonography in the diagnosis, mapping, and measurement of uterine myomas. Am J Obstet Gynecol. 2002;186:409–15. doi: 10.1067/mob.2002.121725. [DOI] [PubMed] [Google Scholar]
- 15.Schwartz SM. Epidemiology of uterine leiomyomata [review] Clin Obstet Gynecol. 2001;44:316–26. doi: 10.1097/00003081-200106000-00018. [DOI] [PubMed] [Google Scholar]
- 16.Frome EL. The analysis of rates using Poisson regression models. Biometrics. 1983;39:665–74. [PubMed] [Google Scholar]
- 17.Abma JC, Chandra A, Mosher WD, Peterson LS, Piccinino LJ. Fertility, family planning, and women’s health: New data from the 1995 National Survey of Family Growth. Vital Health Stat 23. 1997;19:1–114. [PubMed] [Google Scholar]
- 18.Flegal KM, Carroll MD, Ogden CL, Johnson CL. Prevalence and trends in obesity among US adults, 1999–2000. JAMA. 2002;288:1723–7. doi: 10.1001/jama.288.14.1723. [DOI] [PubMed] [Google Scholar]
- 19.Educational Attainment in the United States: March 1995. P20-489. US Bureau of the Census. Washington, DC: U.S. Department of Commerce; Aug, 1996. [Google Scholar]


