Abstract
We describe the case of a 42-year-old man who presented with dyspnea on exertion and a history of anticoagulation therapy for what was thought to be pulmonary arterial thromboembolism. He underwent surgery for obstruction of the right ventricular outflow tract. This is a very rare case of an intimal sarcoma of the pulmonary artery, which we confirmed by pathologic studies.
Key words: Antineoplastic combined chemotherapy protocols; diagnosis, differential; epirubicin; ifosfamide; prognosis; pulmonary artery/pathology; pulmonary embolism/diagnosis; sarcoma/complications/diagnosis/drug therapy/pathology/surgery; vascular neoplasms/diagnosis/drug therapy/pathology/surgery
Primary intimal sarcoma of the pulmonary artery (PA) is a very rare tumor, and it is highly lethal. Retrograde extension of the sarcoma to the pulmonic valve and the right ventricle is reported to be an extremely rare condition frequently mistaken for pulmonary thromboembolism.1 We report a case—initially diagnosed as PA thromboembolism—of an intimal sarcoma of the PA with retrograde extension to the pulmonic valve and the right ventricle.
Case Report
In July 2005, a 42-year-old man with exertional dyspnea and chest pain was referred to our clinic after having been diagnosed with PA thromboembolism. He had taken an anticoagulant agent for this presumed condition for 3 months. Except for a systolic ejection murmur in the pulmonary area, the results of the patient's physical examination were normal.
Results of the laboratory tests and chest radiography revealed no abnormalities. Electrocardiography showed sinus rhythm. Transthoracic echocardiography showed a mobile thrombus-like mass (60 × 20 mm) in the PA. The mass protruded into the right ventricular outflow tract. The patient's PA pressure was 50 mmHg. The peak and mean gradients across the pulmonic valve were 71 and 42 mmHg, respectively. The right ventricular diameter was 59 mm, and the right atrial diameter was 64 mm. There was a moderate degree of tricuspid insufficiency. The ejection fraction was 0.70. On the basis of these findings, the patient was scheduled for surgery.
The patient was placed under general anesthesia. After median sternotomy and aortic arterial and bicaval venous cannulation, a vent was placed into the right superior pulmonary vein. Cardiopulmonary bypass was instituted. Then the aorta was clamped, and isothermal, hyperkalemic blood cardioplegic solution was infused into the antegrade cardioplegic cannula. Cardiac arrest was maintained by retrograde infusion of cardioplegic solution.
A longitudinal pulmonary arteriotomy was performed. In the lumen of the PA was a huge round mass (Fig. 1A) that extended distally to the main PA branches; most of it was adhered to the vascular wall. The mass, which almost completely occluded the artery, was also firmly adhered to the pulmonic valve. A longitudinal right ventriculotomy was extended to the infundibulum. A polypoid mass (Fig. 1B), seen protruding from the PA into the ventricular cavity, was resected. Because of the adherent nature of the mass, part of the PA wall and the pulmonic valve were also resected. The right ventriculotomy was closed primarily; the pulmonary arteriotomy was closed with a polytetrafluoroethylene patch. Cardiopulmonary bypass was discontinued, with the patient receiving minimal inotropic support.
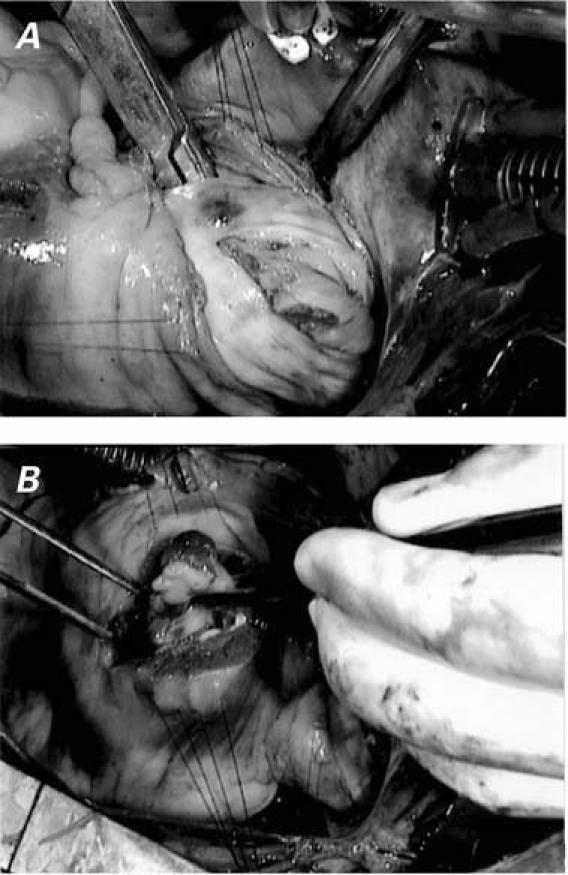
Fig. 1 A) The large tumor took the shape of the main pulmonary artery and extended to its branches, adhering to the vascular wall and the pulmonic valve. B) The polypoid mass—protruding from the pulmonary artery into the ventricular cavity—is seen through the right ventriculotomy.
After the mass was excised, the patient's condition improved. He experienced no complications and was discharged from the hospital on the 6th day. Postoperative transthoracic echocardiography at discharge showed a peak transpulmonary gradient of 11 mmHg, with a mild degree of tricuspid insufficiency.
The pathology evaluation was done by means of a Nikon Eclipse E600W light microscope (Nikon Corporation Co., Ltd.; Kanagawa, Japan). The biopsy material contained markedly atypical spindle and oval cells with varying degrees of atypia and nuclear polymorphism. The mitotic activity was extremely high (Fig. 2A). Pleomorphic tumor cells surrounded the endothelium, in particular (Fig. 2B). Smooth-muscle actin, myoglobin, and factor VIII were immunohistochemically positive, whereas striated-muscle actin, CD31, and CD34 were negative. Accordingly, a diagnosis of primary intimal sarcoma was made. The patient was referred to the medical oncology clinic for further evaluation; he underwent 4 cycles of chemotherapy with ifosfamide and epirubicin in combination. One month, 6 months, and 16 months after his surgery, screening by magnetic resonance imaging, computed tomography, and echocardiography revealed no metastasis or recurrence of the malignancy.
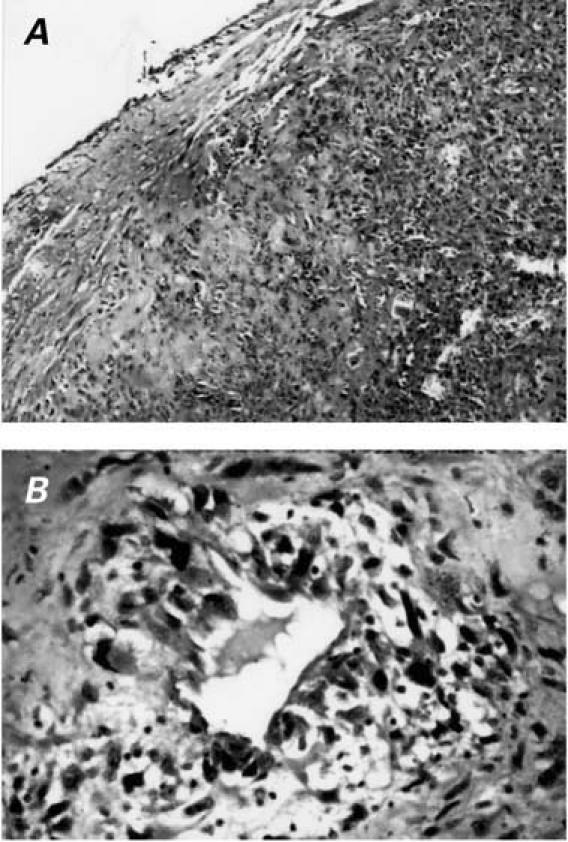
Fig. 2 A) The tumor originated in the intimal layer of the pulmonary artery (H & E, orig. ×10). B) The endothelially lined vascular cleft, surrounded by pleomorphic cells (H & E, orig. ×40).
Discussion
Intimal sarcomas are malignant mesenchymal tumors that arise in large arteries. The defining features of these tumors are intraluminal growth with obstruction of the lumen and seeding of emboli. The incidence of pulmonary intimal sarcoma is almost twice that of aortic origin. The mean age of diagnosis is 48 years for patients with pulmonary intimal sarcoma and 62 years for those with aortic intimal sarcoma.2
Intimal sarcoma of the aorta is a rare condition that is usually diagnosed postoperatively or at autopsy. The median survival time is only a few months.3–6 Primary intimal sarcomas of the aorta are aggressive tumors that can metastasize to bones and visceral organs, including the liver, kidneys, adrenal glands, and lungs.5
Few reports describe intimal sarcoma of the PA. Primary intimal sarcoma of the PA is also rare.2,6–8 Most commonly diagnosed at surgery or autopsy,1 this sarcoma can metastasize to the brain, pancreas, adrenal glands, and lungs.7 The prognosis after the onset of symptoms is unfavorable; life expectancy is usually 12 to 18 months.1,2
Intimal sarcoma of the PA is often mistaken for pulmonary thromboembolism, as it was in our patient.2,9 This mistaken diagnosis can lead to inappropriate therapy, such as anticoagulation or thrombolysis. Surgical resection of the tumor offers the best chance of prolonged survival.2,10 After performing surgery on a 63-year-old woman, Uchida and colleagues10 detected the persistence of an intraluminal mass, and they successfully treated the patient with combination ifosfamide and epirubicin chemotherapy.
Herein, we have reported a very rare case of PA intimal sarcoma that was misdiagnosed as PA thromboembolism. If a mass has invaded the vascular structures or neighboring tissues, or if malignancy is suspected, the mass should be extensively resected. Such resection might prolong the patient's life. In addition, it is important that the patient be evaluated postoperatively for metastasis.
Footnotes
Address for reprints: Bilgin Emrecan, MD, 226 sok. 17/10 Hatay, 35280 Izmir, Turkey. E-mail: bilginemrecan@yahoo.com
References
- 1.Choi EY, Yoon YW, Kwon HM, Kim D, Park BE, Hong YS, et al. A case of pulmonary artery intimal sarcoma diagnosed with multislice CT scan with 3D reconstruction. Yonsei Med J 2004;45:547–51. [DOI] [PubMed]
- 2.Bode-Lesniewska B, Komminoth P. Intimal sarcoma. In: Fletcher CDM, Unni KK, Mertens F, editors. Pathology & genetics: tumours of soft tissue and bone. Oxford: World Health Organization Classification of Tumours; 2002. p. 223–4.
- 3.Tucci M, Quatraro C, Calvani N, Serio G, Marzullo A, Dammacco F, Silvestris F. Primary intimal sarcoma of the thoracic aorta. J Exp Clin Cancer Res 2005;24:139–42. [PubMed]
- 4.Thalheimer A, Fein M, Geissinger E, Franke S. Intimal angiosarcoma of the aorta: report of a case and review of the literature. J Vasc Surg 2004;40:548–53. [DOI] [PubMed]
- 5.Osei-Agyemang T, Geks J, Wagner HJ, Feek U, Gerdes B. High-grade intimal sarcoma in an aneurysm of the infrarenal aorta [in German]. Chirurg 2004;75:823–7. [DOI] [PubMed]
- 6.Brocheriou I, Quillard A, Gatecel C, Wassef M. An unusual primary vascular tumor: intimal sarcoma of the pulmonary artery [in French]. Ann Pathol 2000;20:69–72. [PubMed]
- 7.Araki Y, Tajima K, Yoshikawa M, Abe T, Suenaga Y. A case of primary pulmonary intimal sarcoma of the pulmonary artery [in Japanese]. Nippon Kyobu Geka Gakkai Zasshi 1997;45:1039–43. [PubMed]
- 8.Gosalbez F, Gudin C, Miralles M, Naya J, Valle JM. Intimal sarcoma of the left pulmonary artery: diagnosis, treatment and survival. Cardiovasc Surg 1993;1:447–8. [PubMed]
- 9.Madu EC, Taylor DC, Durzinsky DS, Fraker TD Jr. Primary intimal sarcoma of the pulmonary trunk simulating pulmonary embolism. Am Heart J 1993;125:1790–2. [DOI] [PubMed]
- 10.Uchida A, Tabata M, Kiura K, Tanimoto Y, Kanehiro A, Aoe M, et al. Successful treatment of pulmonary artery sarcoma by a two-drug combination chemotherapy consisting of ifosfamide and epirubicin. Jpn J Clin Oncol 2005;35:417–9. [DOI] [PubMed]


