Abstract
Low-cost diabetes education programs that target Mexican Americans are essential to reduce the observed health disparities in this population. A culturally appropriate intervention was developed as the centerpiece of the Community Diabetes Education (CoDE) program. This article describes the structure, patient acceptance, and costs of this one-to-one educational model delivered in 7 patient contact hours by a community health worker over 12 months in a community clinic serving the uninsured. A total of 162 patients—predominantly female, Spanish-speaking Mexican American patients with type 2 diabetes of mean duration of 6.5 years—enrolled in the program, and a dropout rate of 22% was observed during the 12-month period. Preliminary analysis indicated that program capacity was 120 patients per month, and the annual direct medical expenditure per CoDE participant was $461. The hemoglobin A1c was significantly reduced in patients who participated in the program for 12 months. Sustainable, low-cost, community-based programs like CoDE and long-term patient participation will help reduce the burden of diabetes in the underserved Hispanic population.
Diabetes affects 20.8 million children and adults in the USA, and 1.5 million new cases in people over the age of 20 were reported in 2005 (1). Mexican Americans, the largest Hispanic/Latino subgroup, are 1.7 times more likely to have diabetes than non-Hispanic whites of similar age (1). Approximately 24% of Mexican Americans between the ages of 45 and 74 have diabetes, and the diabetes-related complications of retinopathy and end-stage renal disease are two to four times more prevalent in this population than in the rest of the diabetic population (1–3). These numbers are of particular concern in light of the USA's rapidly growing Hispanic population (from 22.4 million in 1990 to 35.3 million in 2000), especially in Texas and California, where half of all people in the USA of Hispanic heritage live (4).
In addition to the obvious health-related concerns associated with the rising incidence of diabetes, this epidemic represents a substantial economic burden. The cost estimate for direct and indirect expenditures related to diabetes care in the USA was $132 billion in 2002 and is expected to rise as both the prevalence of diabetes and the cost of health care services increase (5). The annual direct medical cost of type 2 diabetes per individual ranges from $1700 for a patient who is diet controlled to $63,100 for a patient with end-stage renal disease (6).
The population of Dallas, Texas, is 35.6% Hispanic—a population group disproportionately affected by poverty in Texas (4). The East Dallas area also has a larger number of uninsured residents (39.2%) than Dallas County (26.6%), the State of Texas (23.6%), and the nation as a whole (15.6%) (7). These factors are important to consider in diabetes management, as low income and lack of health insurance are associated with worse health status among patients with diabetes (8).
Traditional approaches to diabetes education and chronic disease management are less effective when applied to the most vulnerable segments of the diabetes population (9–11). Long-term, culturally competent diabetes self-management educational strategies addressing the specific needs of the underserved Hispanic population have been developed and implemented in both California and Texas (12, 13) and have demonstrated improved health outcomes in the Mexican American/Hispanic population (12–14). However, the translation of clinical research to real-world settings is always problematic and is complicated further when the target population includes substantial numbers of uninsured, non–English-speaking patients.
The limited opportunities for uninsured individuals with diabetes in East Dallas to obtain educational services prompted a community-based effort to develop an abbreviated, low-cost, one-to-one educational program with long-term follow-up integrated into the medical services of an existing community health clinic, designed to improve the quality of diabetes care and health outcomes for clinic patients in accordance with standards established by the American Diabetes Association (ADA) (15). We describe this intervention, known as the Community Diabetes Education (CoDE) program, and its implementation at Central Dallas Ministries Community Health Services (CDM-CHS).
METHODS
Setting
CDM-CHS, a nonprofit organization located near downtown Dallas, was established in 1988 and has grown to include three full-time family practice physicians and a class D pharmacy in 2007. One of the physicians is fluent in Spanish. Support personnel include medical assistants and community health workers, 70% of whom are bilingual. To enroll for medical services at CDM-CHS, patients must have no medical insurance and have no alternative source of health care. Patient visits in 2004 exceeded 12,000 encounters.
Diabetes care at CDM-CHS
Clinic physicians utilize Texas Department of Health treatment algorithms for diabetes management (16). The clinic relies upon committed volunteer physician support for ophthalmologic evaluations and has access to low-cost laboratory services for lipid measurements and other required laboratory testing. Nominal fees are charged for physician services, laboratory testing, and glucose testing strips and prescriptions, though a financial waiver of fees is granted on an individual basis. Patients are referred to the CoDE program by the clinic physician and must be enrolled as clinic patients to participate. There is no fee for the CoDE educational intervention or quarterly assessment.
CoDE educator training
The CoDE educator is a community health worker who helps patients self-manage their disease and provides individual case management under direct physician supervision. The bilingual community health worker holds a high school equivalency certificate and is certified by the State of Texas as a promotora (community health worker). Certified diabetes educators and registered dietitians from the Ruth Collins Diabetes Center at Baylor University Medical Center at Dallas provided 12 hours of didactic classroom education and 5 hours of one-to-one training for the community health worker at no cost to the clinic but had no contact with any patients from the CoDE program. In addition, a volunteer endocrinologist provided 10 hours of one-to-one education to the community health worker, focusing on diabetes knowledge, dietary assessment, meal planning, and technical interviewing skills. The community health worker passed a written final examination (available on request) with questions derived from the American Association of Diabetes Educators' core curriculum (17) and received continuing education during monthly case conferences and weekly chart reviews provided by the physicians in the clinic.
The CoDE office is conveniently located within the CDM-CHS–owned clinic facility. This space accommodates the educational materials, glucose monitors, computer, patient records, and Bayer DCA 2000+ Analyzer for hemoglobin A1c (HbA1c) testing, with ample room for supportive family members to attend the one-to-one educational sessions.
CoDE intervention
The copyrighted written protocols for the CoDE program (Table) were developed collaboratively by the community health worker and an endocrinologist (E.A.P.) utilizing ADA standards of care (15), Texas Department of Health practice guidelines (16), and the national standards of diabetes self-management education (18). The educational intervention consisted of three initial 60-minute visits and quarterly assessments scheduled for 30 to 60 minutes, for a maximum of 7 patient contact hours over 12 consecutive months. After completion of the initial 12 months, the CoDE program patients continued to participate indefinitely through quarterly assessment visits.
Table.
Community Diabetes Education (CoDE) intervention protocol
| Visits∗ | |||||||
| Activity | 1 (day 1) | 2 (7–14 days) | 3 (6–8 weeks) | 4 (3 months) | 5 (6 months) | 6 (9 months) | 7 (12 months) |
| Measure height, weight | X | X | X | X | X | X | X |
| Measure blood pressure | X | X | X | X | X | X | X |
| Measure waist circumference | X | ||||||
| Gather demographic information | X | ||||||
| Complete Diabetes Quality of Life survey | X | ||||||
| Take diabetes knowledge test | X | ||||||
| Test hemoglobin A1c | X | X | X | X | X | ||
| Obtain a lipid profile | X | ||||||
| Provide self–blood glucose monitor | X | ||||||
| Analyze glucose monitor readings | X | X | X | X | X | X | |
| Review medications | X | X | X | X | X | X | X |
| Explain hypoglycemia signs, symptoms, and treatment | X | # | # | # | # | # | # |
| Explain hyperglycemia signs, symptoms, and treatment | X | # | # | # | # | # | # |
| Explain sick day rules | X | # | # | # | # | # | # |
| Provide educational materials | X | X | X | X | X | X | X |
| Test microalbumin | X | ||||||
| Give food record instructions | X | ||||||
| Review food record | X | ||||||
| Create meal plan | X | ||||||
| Review blood sugar targets | X | X | X | X | X | X | |
| Review/revise meal plan | X | X | X | X | X | ||
| Explain diabetes complications | X | ||||||
| Examine foot | X | ||||||
| Set goal | X | X | X | X | X | ||
| Review exercise recommendation | X | X | X | X | X | ||
| Discuss smoking and alcohol use | X | X | X | X | X | ||
| Document activity in clinic charts | X | X | X | X | X | X | X |
∗The initial three visits were 60 minutes; quarterly assessments were scheduled for 30 to 60 minutes.
X indicates activity performed; # shows review if necessary.
HbA1c was measured at baseline and quarterly thereafter. Blood pressure, height, and weight were measured at all patient encounters. Urine microalbumin was measured annually. The community health worker recorded vital signs, anthropometric measurements, foot examinations, and meal plans and documented skills taught and educational topics discussed with the patient in a unique chart (available on request) created for each participant. All relevant data were duplicated for the clinic medical record for immediate physician review and approval. Medication changes were prescribed by the primary care provider.
Educational materials were obtained at no cost to the clinic from various sources, including the Texas Department of Health (16) and the ADA (19) in English, Spanish, and picture format. During the first educational visit, the patient completed a demographic and medical history form, the Diabetes Quality of Life survey (20), and a diabetes knowledge test. Literacy was determined based on the patient's ability to read and write answers to these surveys. A glucose monitor (Home Diagnostics Prestige IQ) and 100 testing strips were provided at no charge to the patient, who was required to demonstrate mastery of the device. Testing blood glucose twice daily before breakfast and before or after one additional meal was recommended. Fasting blood glucose readings of 80 to 120 mg/dL and postprandial glucose readings of <140 mg/dL were the specific targets identified for most patients. A point-of-care HbA1c test was performed during the visit, and the results were explained to the patient using a simple chart. Signs, symptoms, and treatment of hypoglycemia along with sick day rules were discussed in detail, and educational materials addressing these issues were provided. The patient was given a food diary with instructions to record food and beverage intake for 3 days chosen randomly over a 1-week period.
The second visit focused on personalized meal planning, consistent with American Association of Diabetes Educators' recommendations that meal plans be individualized and appropriate to the language, culture, and educational level of the patient (17). The community health worker estimated the caloric intake required for the patient to maintain current body weight based on a ratio of 100 kcal per pound of body weight. This was compared with the caloric intake needed to maintain a normal body weight based upon a body mass index (BMI) table and an estimate of the patient's actual caloric intake derived from the 3-day food diary. The total daily caloric intake recommended by the community health worker was as close to the estimated maintenance intake as realistically prudent. While no patient was prescribed more than 2200 kcal per day, weight loss was not the primary emphasis for this educational intervention. The community health worker was able to identify eating patterns through the food diary, which generally included excessive carbohydrate intake from foods and beverages throughout the day.
The time of day that meals were consumed, the number of meals per day, and the work schedule of the patient were taken into account in designing the meal plan. Patients who were able to read English or Spanish were taught to identify and understand the carbohydrate content listed on a food label. Fat, carbohydrate, and protein portion sizes were demonstrated with actual-size models and measuring utensils. Consumption of calorie-containing beverages was discussed in detail, and recommendations for more appropriate choices were made. Finally, a rudimentary meal plan that emphasized healthy ways of preparing protein-rich foods, limited fat servings to ≤4 per day, and contained 50% to 60% carbohydrate was constructed using a reasonable calculated caloric intake based upon the patient's current body weight and ideal body weight. The maximum number of carbohydrate servings to be consumed at each meal was clearly specified on the meal plan, and personally formulated meal suggestions were given based upon patient preferences. The physician reviewed the meal plan, and a copy was included in the clinic record. Patients were given printed materials appropriate to their language and literacy to reinforce food choices and portion sizes. Consumption of fast food was strongly discouraged through representations of fast food meals that were accurately sized and embellished with food labels.
The third visit emphasized prevention of short-term and long-term diabetes complications. The physician was notified in real time if a patient experienced three or more blood glucose readings of <70 mg/dL (21) (as documented by the home glucose monitor) with or without symptoms of hypoglycemia. The community health worker interviewed the patient in detail about the timing of medication use and food and beverage intake relative to the hypoglycemia episodes, as well as his or her exercise or physical activity and the time of day the hypoglycemia symptoms occurred.
Blindness, kidney failure, nerve damage, heart disease, and limb amputation that can result from poor diabetes control were discussed in detail. The community health worker performed a full foot examination, including visual inspection, assessment of pedal pulses, and monofilament testing. Results were documented in the CoDE chart and the clinic medical record. Foot abnormalities were reported immediately to the physician. Appropriate footwear and daily home foot care were discussed.
Consistent with the current recommendation, patients were encouraged to engage in 150 minutes of activity per week (15). Neighborhood locations offering organized exercise activities were identified for the patient. Smoking cessation and alcohol use were addressed if appropriate, and patient information regarding these lifestyle issues was available.
At the conclusion of the third educational session, the educator and the patient negotiated a single goal to improve glycemic control and personal well-being. The educator guided goal selection to address the most pertinent issues for the individual based on information gathered during the three sessions. Examples of goals included refilling medications on time, taking medication on a regular basis exactly as prescribed, following the rudimentary meal plan, performing regular home glucose monitoring, starting a simple walking program, discontinuing smoking, or using alcohol in moderation. Progress toward goal attainment was addressed at each subsequent patient visit, and goals were changed as individuals achieved success.
Quarterly assessment follow-up visits began with a point-of-care HbA1c test, allowing immediate discussion of the result with the patient. Meal plans were reviewed and revised, including review of portion sizes using food models. Patients were encouraged to bring food packaging and labels from items used at home that they found difficult to quantify or characterize. Patients who did not meet the target HbA1c (<7%) were questioned extensively about possible explanations for these findings related to medication use, weight fluctuation, dietary and activity level changes, social and personal issues, and the development of new medical problems and recent hospitalizations. Findings were reported to the physician, facilitating medical decision making and reducing duplication of effort, particularly when a translator would have been necessary. At the conclusion of each quarterly session, the educator and patient again chose a goal to work on over the next 3 months. Medication compliance was the first priority, followed by meal plan adherence, exercise, smoking cessation, and limitation of alcohol use.
Population and sample
To be eligible for referral to the CoDE program by a clinic physician, patients had to be actively enrolled in the CDM-CHS clinic; be older than 18 years; be diagnosed with either type 1 or type 2 diabetes that was treated with oral agents, insulin, or no medication; have no advanced complications associated with diabetes; not be pregnant; and have stable blood pressure with or without medication. Patients of all ethnic backgrounds were included, though the clinic primarily served a Hispanic community of predominantly Mexican origin. The study was approved by the institutional review board at Baylor University Medical Center at Dallas. Patient recruitment took place at CDM-CHS from July 2003 to March 2005. Consent forms were available in English and Spanish.
Data collection and analysis
Patient participation rates, program expenditures, and the health indicators HbA1c, blood pressure, and BMI were the measured outcomes for this study. Data extracted from CoDE patient charts were entered into an Excel spreadsheet. Descriptive univariate summary statistics were used to illustrate the sociodemographic characteristics of the participants. Program capacity, no-show rates, and direct expenditures were calculated based upon the monthly activity reports generated by the clinic and accounting sheets kept by the clinic supervisor. Losses to follow-up were recorded, and reasons for leaving the program were determined to the extent possible. Patient attendance at clinic visits was analyzed using the independent samples t test. Changes in health indicators from baseline to the 6- and 12month time points were analyzed using paired-samples t tests.
RESULTS
Description of participants
From July 2003 through March 2005, 162 patients were enrolled in the CoDE program. Most were Mexican Americans (78%), followed by African Americans (15%), Caucasians (6%), and Asians (1%). Patients seeking care generally resided in six ZIP codes within a 10-mile radius of the clinic. Most of the Mexican American population spoke and read only Spanish (73%), although most had lived in Texas for more than 5 years. Most of the participants were women (64%) and almost all (99%) had type 2 diabetes, with an average time since diagnosis of 6.5 years. The average age was 48 years.
Program capacity and direct costs
Full capacity for a single community health worker was 120 patient encounters per month (1440 patient visits per year) based on 60 minutes per individual session. The CoDE community health worker handled 564 patient contacts during 2004, which increased to 1170 visits during 2005. This represented a progressive increase in utilization of CoDE program services from 39% of capacity to 81% of capacity by the second full year of operation. The program costs of $461 per patient per year—which included educator salary ($82), home glucose monitor and strips ($260), and supplies ($119) —remained stable. Although determining the HbA1c during the educational visit was slightly more expensive than sending the sample to the laboratory (approximately $1 more per test), discussing the result in person may have had an additional impact on patient compliance (22). The availability of the point-of-care HbA1c testing has been reported to increase the frequency of therapy intensification and improve glycemic control (15, 22).
Patient participation and compliance
Of the 162 patients enrolled in the CoDE program, 92 participated for at least 12 consecutive months. Of these, 55 patients had a 12-month HbA1c value available, and they were further characterized as compliant (n = 36) if they attended all CoDE visits or noncompliant (n = 19) if they missed one or two quarterly assessment CoDE visits. The CoDE compliant group attended more clinic visits for general medical care than did the CoDE noncompliant group (P < 0.05).
Thirty-five of the 162 patients (22%) dropped out of the educational program. Reasons for leaving the program included lack of interest (13 individuals), relocation to other cities or countries (18 individuals), acquisition of health insurance (3 individuals), and resolution of secondary diabetes (1 patient). The monthly no-show rate for the year 2004 varied from a high of 20% to a low of 3.5%, with an average of 12% over 12 months. The introduction of a computerized patient scheduling system in 2005 increased the number of scheduled CoDE program appointments by 30%, while the annual no-show rate remained stable at 12.8%. Patients were accountable for either keeping or rescheduling appointments because of the possibility of dismissal from clinic services after three documented no-shows.
Outcomes measures
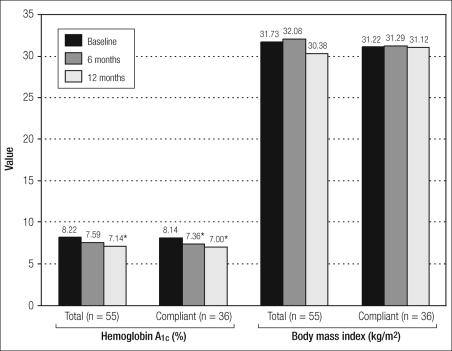
Fifty-five patients completed at least 12 consecutive months of the CoDE program and had a 12-month HbA1c value available. The mean HbA1c at baseline for this group was 8.22% (Figure). The change from baseline to 6 months was not statistically significant, but the overall change from baseline to 12 months was significant (P < 0.01). The subsample of compliant patients (n = 36) had significant changes not only from baseline to 12 months (P < 0.01) but also from baseline to 6 months (P < 0.01). The BMI measured at baseline did not change significantly by 6 months or 12 months for the entire sample of 55 patients or for the compliant group when analyzed separately (Figure). The mean blood pressures recorded at baseline, 6 months, and 12 months were <130/80 mm Hg and did not change significantly over this time period.
Figure.
Changes in hemoglobin A1c and body mass index among patients who participated in the Community Diabetes Education (CoDE) program over 12 months and for whom a 12-month hemoglobin A1c value was available. Compliant indicates that the patient completed all CoDE visits. ∗P ≪ 0.01.
DISCUSSION
The CoDE program featured several key elements that distinguish it from other published models for diabetes education in the Mexican American population (12–14). The intervention team consisted of full-time primary care physicians and a single specially trained bilingual community health worker. No other published models utilized a community health worker in a similar capacity, though the American Association of Diabetes Educators (23), the Institute of Medicine (24), and others (25–27) support the use of community health workers to provide diabetes education. The Starr County Border Health Initiative has been a proactive model in the use of bilingual community health workers as members of their intervention teams (12). The program, a long-standing diabetes self-management intervention located on the Texas-Mexico border where 97% of residents are Mexican American, featured an intensive instructional and support group intervention of 52 contact hours over 12 months provided by a team of bilingual Mexican American nurses, dietitians, and community workers (12). A compressed version of this intervention provided 16 hours of education and an additional 6 hours of group support (25).
The total patient contact time for the CoDE intervention was 7 hours over 12 months, which was considerably less than that of the Starr County Border Health Initiative and other published models. Project Dulce in San Diego, California, utilized a nurse case management/peer education approach in multiple community clinics (13). The nurse case manager educated the patients individually during an average of eight 2-hour sessions over 1 year and made medication adjustments with the approval of the primary care physician. Patients were then educated in a group setting by specially trained community health workers for twelve 2-hour sessions over 12 weeks. In addition, a bilingual dietitian was available for two individual 45-minute sessions. An educational intervention designed for Caribbean Hispanic individuals with type 2 diabetes utilized a nutritionist, a nurse, and an intervention assistant (14). The intervention involved an initial 1 hour individual session followed by 10 weekly 2½- to 3-hour group sessions and two 15-minute individual sessions that occurred during the 10-week period immediately prior to the group session.
The statistically significant improvement of HbA1c over the 12-month CoDE program intervention suggests that the lower intensity of the patient contact time, the educational background of the CoDE educator, the lack of additional more specialized diabetes education personnel, and the one-to-one delivery structure of the program did not adversely affect this desired outcome. BMI was not significantly changed over the 12 months of observation in spite of improvement in glycemic control.
The capacity for a single community health worker to educate and assess patients with diabetes on a quarterly basis is substantial. Per-patient expenditures for the program have been kept to a stable minimum while the program utilization has more than doubled over the first 2 years of operation. The low attrition rate indicated high patient acceptance, and patients who were compliant with CoDE attended a greater number of clinic visits.
Financial and organizational constraints faced by CDMCHS prohibited the employment of certified diabetes educators, registered nurses, and dietitians for diabetes care. Consequently, this model did not comply with this criterion of published national standards defined for diabetes self-management education programs (18). However, this limitation was overcome by the direct supervision of the community health worker by the primary care physicians. The closed-loop system that connected the patient, educator, and physician facilitated the expedient flow of pertinent clinical information. While no formal advisory body was established to oversee the CoDE program, the professional staff, CoDE program director, community health worker, and all clinic staff met monthly to plan and review processes, including scheduling, patient participation, information flow, and outcomes evaluation.
CoDE has been initiated through a grassroots, community-based effort to improve access to diabetes educational services and reduce health disparities in the predominantly uninsured, underserved Mexican Americans living in East Dallas. The patient population participating in the CoDE program is young and has a relatively short average duration of diabetes, which suggests that we have a window of opportunity to reduce diabetes-related morbidity and mortality. Our initial experience with CoDE demonstrated that a physician-supervised community health worker is capable of providing educational services, a task typically assigned to more highly trained and highly paid individuals, to patients with diabetes in community clinics serving the uninsured.
Funding from several sources has been secured for a randomized controlled trial planned to rigorously evaluate the effectiveness and efficiency of the CoDE program based on a preliminary feasibility study. Documenting the improvement in quality of care and health-related outcomes and reducing diabetes-associated morbidity and mortality, at minimal cost, has important implications for the ongoing maintenance of this intervention and its implementation in other community clinical settings.
Acknowledgments
The authors thank the Baylor Health Care System Foundation, the Ruth Collins Diabetes Center, the HealthTexas Provider Network, and Central Dallas Ministries for their vision of community health improvement and their support in the development of this program. The commitment of the physicians, Maura Thielen, MD, and Demetria M. Smith, MD, as well as Patricia L. Leczynski, the entire staff of CDM-CHS, and the talents and dedication of Helen Rodriguez Farias, CHW, are gratefully acknowledged. The authors are indebted to Karen Harker, MLS, MPH, for statistical assistance and to Craig L. Hanis, PhD, for critical review of this manuscript.
References
- 1.American Diabetes Association. Diabetes facts and figures Available at www.diabetes.org; accessed January 6, 2007.
- 2.Ayanian JZ, Weissman JS, Schneider EC, Ginsburg JA, Zaslavsky AM. Unmet health needs of uninsured adults in the United States. JAMA. 2000;284(16):2061–2069. doi: 10.1001/jama.284.16.2061. [DOI] [PubMed] [Google Scholar]
- 3.Harris MI. Racial and ethnic differences in health insurance coverage for adults with diabetes. Diabetes Care. 1999;22(10):1679–1682. doi: 10.2337/diacare.22.10.1679. [DOI] [PubMed] [Google Scholar]
- 4.US Census Bureau. The Hispanic Population: Census 2000 Brief Available at http://www.census.gov/prod/2001pubs/c2kbr01-3.pdf; accessed January 6, 2007.
- 5.Hogan P, Dall T, Nikolov P. Economic costs of diabetes in the US in 2002. Diabetes Care. 2003;26(3):917–932. doi: 10.2337/diacare.26.3.917. [DOI] [PubMed] [Google Scholar]
- 6.Brandle M, Zhou H, Smith BR, Marriott D, Burke R, Tabaei BP, Brown MB, Herman WH. The direct medical cost of type 2 diabetes. Diabetes Care. 2003;26(8):2300–2304. doi: 10.2337/diacare.26.8.2300. [DOI] [PubMed] [Google Scholar]
- 7.The Dallas Foundation, Foundation for Community Empowerment. Demographic Profile of the Texas Population Without Health Insurance in 2001. Sustaining a Healthy Community Available at www.dallasindicators.org; accessed January 6, 2007.
- 8.Gulliford MC, Mahabir D, Rocke B. Diabetes-related inequalities in health status and financial barriers to health care access in a population-based study. Diabet Med. 2004;21(1):45–51. doi: 10.1046/j.1464-5491.2003.01061.x. [DOI] [PubMed] [Google Scholar]
- 9.Anderson RM. Into the heart of darkness: reflections on racism and diabetes care. Diabetes Educ. 1998;24(6):689–692. doi: 10.1177/014572179802400604. [DOI] [PubMed] [Google Scholar]
- 10.Anderson RM, Goddard CE, Garcia R, Guzman JR, Vazquez F. Using focus groups to identify diabetes care and education issues for Latinos with diabetes. Diabetes Educ. 1998;24(5):618–625. doi: 10.1177/014572179802400507. [DOI] [PubMed] [Google Scholar]
- 11.Harris MI. Medical care for patients with diabetes. Epidemiologic aspects. Ann Intern Med. 1996;124(1 Pt 2):117–122. doi: 10.7326/0003-4819-124-1_part_2-199601011-00007. [DOI] [PubMed] [Google Scholar]
- 12.Brown SA, Garcia AA, Kouzekanani K, Hanis CL. Culturally competent diabetes self-management education for Mexican Americans: the Starr County Border Health Initiative. Diabetes Care. 2002;25(2):259–268. doi: 10.2337/diacare.25.2.259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Philis-Tsimikas A, Walker C, Rivard L, Talavera G, Reimann JO, Salmon M, Araujo R, Project Dulce Improvement in diabetes care of underinsured patients enrolled in Project Dulce: a community-based, culturally appropriate, nurse case management and peer education diabetes care model. Diabetes Care. 2004;27(1):110–115. doi: 10.2337/diacare.27.1.110. [DOI] [PubMed] [Google Scholar]
- 14.Rosal MC, Olendzki B, Reed GW, Gumieniak O, Scavron J, Ockene I. Diabetes self-management among low-income Spanish-speaking patients: a pilot study. Ann Behav Med. 2005;29(3):225–235. doi: 10.1207/s15324796abm2903_9. [DOI] [PubMed] [Google Scholar]
- 15.Standards of medical care in diabetes—2007 Diabetes Care. 2007;30(Suppl 1):S4–S41. doi: 10.2337/dc07-S004. [DOI] [PubMed] [Google Scholar]
- 16.Texas Department of Health. Diabetes treatment algorithms Available at http://www.dshs.state.tx.us/diabetes/hcstand.shtm; accessed January 6, 2007.
- 17.Franz MJ, editor. A Core Curriculum for Diabetes Educators. 5th ed. Chicago: American Association of Diabetes Educators; 2003. [Google Scholar]
- 18.Mensing C, Boucher J, Cypress M, Weinger K, Mulcahy K, Barta P, Hosey G, Kopher W, Lasichak A, Lamb B, Mangan M, Norman J, Tanja J, Yauk L, Wisdom K, Adams C. National standards for diabetes self-management education. Diabetes Care. 2007;30(Suppl 1):S96–S103. doi: 10.2337/dc07-S096. [DOI] [PubMed] [Google Scholar]
- 19.American Diabetes Association. All About Diabetes; Nutrition and Recipes; Weight Loss and Exercise Available at www.diabetes.org; accessed January 6, 2007.
- 20.Jacobson AM, De Groot M, Samson JA. The evaluation of two measures of quality of life in patients with type I and type II diabetes. Diabetes Care. 1994;17(4):267–274. doi: 10.2337/diacare.17.4.267. [DOI] [PubMed] [Google Scholar]
- 21.American Diabetes Association Workgroup on Hypoglycemia Defining and reporting hypoglycemia in diabetes: a report from the American Diabetes Association Workgroup on Hypoglycemia. Diabetes Care. 2005;28(5):1245–1249. doi: 10.2337/diacare.28.5.1245. [DOI] [PubMed] [Google Scholar]
- 22.Heisler M, Piette JD, Spencer M, Kieffer E, Vijan S. The relationship between knowledge of recent HbA1c values and diabetes care understanding and self-management. Diabetes Care. 2005;28(4):816–822. doi: 10.2337/diacare.28.4.816. [DOI] [PubMed] [Google Scholar]
- 23.American Association of Diabetes Educators Diabetes community health workers. Diabetes Educ. 2003;29(5):818–821. doi: 10.1177/014572170302900511. 824. [DOI] [PubMed] [Google Scholar]
- 24.Smedley BD, Stith AY, Nelson AR, editors. Unequal Treatment: Confronting Racial and Ethnic Disparities in Health Care. Washington, DC: National Academy Press; 2002. [PubMed] [Google Scholar]
- 25.Brown SA, Blozis SA, Kouzekanani K, Garcia AA, Winchell M, Hanis CL. Dosage effects of diabetes self-management education for Mexican Americans: the Starr County Border Health Initiative. Diabetes Care. 2005;28(3):527–532. doi: 10.2337/diacare.28.3.527. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Witmer A, Seifer SD, Finocchio L, Leslie J, O'Neil EH. Community health workers: integral members of the health care work force. Am J Public Health. 1995;85(8 Pt 1):1055–1058. doi: 10.2105/ajph.85.8_pt_1.1055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Zuvekas A, Nolan L, Tumaylle C, Griffin L. Impact of community health workers on access, use of services, and patient knowledge and behavior. J Ambul Care Manage. 1999;22(4):33–44. doi: 10.1097/00004479-199910000-00007. [DOI] [PubMed] [Google Scholar]