In 1850 Dr. A. Notta, an “interné” in Paris, described four adult patients between the ages of 20 and 60 who had a nodule on a flexor tendon of a finger, thereby inhibiting its normal movement (1). This publication in the Archives Générales de Médecine led to these “nodules” being named “Notta's nodules,” but a multitude of subsequent papers have largely ignored his claim to fame.
Trigger digit occurs from infancy to old age. In infants it usually occurs in the thumb but is not often diagnosed at birth. The flexed position of the thumb is often recognized sometime after the first 3 months of life. About 30% of these thumbs will gradually gain a full range of motion, and early attempts to passively straighten the thumb often cause significant pain. Some recommend splinting the thumb in full extension, but the reported results vary considerably and I have not usually employed this treatment. The reported rate of spontaneous relief from the flexed posture varies from 0% to 49% but is probably in the area of 30%. This rate drops to 10% to 12% between 6 months and 3 years of age.
Beyond age 3 the standard surgical release of the A1 pulley is a definitive treatment. Surgical release can be done earlier but should certainly be done by age 3. Occasionally the thumb is not fixed in flexion, but it clicks on motion. It has rarely been reported as being in interphalangeal joint extension or even extension of the metacarpophalangeal joint. In all postures, if movement is possible, a click may be heard and can certainly be felt on the palmar surface of the thumb, usually in the region of the metacarpophalangeal joint.
Dobyns (2) has emphasized the importance of differentiating a true trigger thumb from other palm-clutched thumb conditions. Anomalies such as spastic thumb, arthrogryposis, and varieties of hypoplastic thumbs should all be excluded before treatment is undertaken. A trigger finger at birth is about one tenth as common as a trigger thumb, and there is a high rate of abnormalities of the flexor tendons that are often diagnosed only after a standard release of the A1 pulley fails to give complete relief (3).
In adult men and women, the most common age for the triggering of digits is between 50 and 60 years. Bonnici and Spencer (4) reviewed their operative results in 37 patients. Multiple digits were involved in one third. Hereditary factors are said to be very rare, but these authors reported a nurse with all five digits involved on her right hand and a similar condition in her sister's hand.
Repeated minor trauma is probably the most likely cause of trigger digit, but heavy manual labor with the direct palmar pressure of power grasp may precipitate the symptoms at any adult age. Even ordinary use of the hand is associated with a higher incidence of trigger digit in the dominant right hand. The ring finger is most commonly affected; next in involvement is the long finger, then the small finger, while the index finger is rarely involved. For some inexplicable reason, trigger thumb is far more common in women.
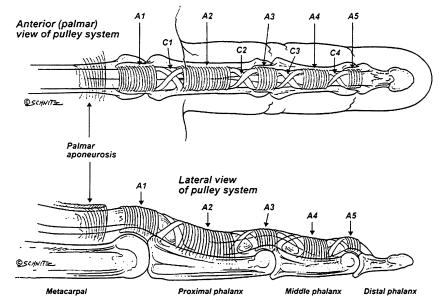
The fundamental etiology of a trigger digit is a size mismatch between the flexor tendon and the proximal end of the digital tendon sheath, particularly at the A1 pulley (Figure 1). Hueston and Wilson (5) have shown that the tendon nodule, which is very often palpable, is caused by a bunching up or spiraling of the fibers of the flexor tendon at the entrance to the A1 pulley. After the nodule has built up to a significant size, triggering will result. They proposed that the chronic repetitive friction between the tendon and its sheath producing the nodule can be compared with the fraying that occurs at the end of a piece of thread after it has been passed numerous times through the eye of a needle.
Figure 1.
The digital pulley system of a finger. Reprinted with permission from Ryzewicz Wolf, 2006 (3).
Histological analyses of diseased A1 pulleys and the superficialis tendons from trigger finger patients have shown fibrocartilaginous metaplasia. Sampson and Badalamente et al (6) commented that tendovaginitis is a more accurate term to describe the condition than tenosynovitis because the inflammatory changes are in the retinacular sheath and peritendinous tissue rather than in the tenosynovium. However, they remarked that both terms are used interchangeably in the literature.
The standard operative procedure at all ages is to incise the A1 pulley, thus allowing the entrance to expand and liberate movement of the flexor tendons. Subsequently the nodule usually subsides. However, opinions vary on how to achieve this result.
What has not been acknowledged in most published operative procedures has been the inevitable biomechanical result of sheath-widening liberation. During normal grasp the fingers tend to move ulnarwards as grasp pressure increases. If a single finger is to be treated, no major mechanical disturbance ensues. However, the site of the incisional release is important. I believe the incision should always be placed not in the central line but on the radial side of the sheath. This preserves the inherent strength of the sheath in resisting the normal ulnarward pressure of the flexor tendons. It is reasonable to assume that in a single digit no significant biomechanical disturbance will occur. With increasing “release” of adjacent fingers, the ulnar torque of the fingers increases. The ultimate result of “releasing” all four trigger fingers will be ulnar drift (Figure 2).
Figure 2.
This hand of a heavy manual laborer had four separate trigger finger releases done over a period of years. This destruction of the normal tendon restraints results in ulnar drift of the fingers.
OTHER PROCEDURES
Steroid injection
“Simpler” procedures, such as injection of steroids in triggering of short duration, are often employed. Betamethasone sodium phosphate is frequently used because it is water soluble and does not leave a residue in the tendon sheath. Freiberg, Mulholland, and Levine (7) reported that with up to three injections, 60% to 90% of patients can obtain long-term relief. These injections are not for the tyro; a keen understanding of the local anatomy is essential. The digital nerves are close to the tendon sheath and do not respond kindly to steroid injections. Nor does the affected tendon; rupture of the tendon has been reported after misplaced injections. A beginner is wise to practice in the dissecting room, using either a lateral or a palmar approach.
Percutaneous release of the A1 pulley
Anatomical knowledge of the area is essential since the slicing of the A1 pulley is done “blind” whether a large-gauge hypodermic needle, a specially designed knife, or even a tenotome is used. The neurovascular bundles of the thumb and index finger are particularly at risk since they lie within 2 to 3 mm of the skin puncture site.
As an elderly surgeon, I like to see where my knife is cutting, and I still believe that no operation is simple until it is successfully completed.
ASSOCIATED DISEASES
While trigger digit frequently exists alone, a number of conditions have a high association with digital triggering.
Carpal tunnel syndrome and trigger fingers frequently coexist, and no conclusive reason for this commingling has been published. It follows that patients with one condition should always be checked for the other.
In diabetes mellitus the hands are often affected by neuropathy, carpal tunnel syndrome, and Dupuytren's contracture; the incidence of trigger fingers is higher than in the nondiabetic population. The longer the diabetes has been present, the greater the incidence of hand involvement.
Rheumatoid arthritis affects synovial tissue anywhere in the body, and the digits are not exempt. Triggering occurs, and in such cases local release of the A1 pulley is inadequate. Tenosynovectomy with preservation of the A1 and A2 pulleys is essential. This procedure is often difficult, and to obtain free movement of the tendons within the sheath it may be necessary to excise the ulnar slip of the superficialis tendon.
If contracture of the proximal interphalangeal joint has been present with trigger finger for a long time, it usually cannot be corrected by release of the A1 pulley alone. If the flexion contracture is more than 30 degrees, a release and removal of the ulnar superficialis slip should certainly be done. This procedure will not necessarily provide full extension of the joint even after gentle passive stretching, but there should be a significant functional improvement. Le Viet et al reported a large series (8).
General metabolic diseases, including amyloidoses, can be associated with digital triggering. Carpal tunnel syndrome will develop in patients having hemodialysis. Infiltrative amyloid tenosynovitis in the palm and fingers can cause trigger finger and subsequent flexion contractures. A1 pulley release and tenosynovectomy are helpful for these patients. Van Heest et al (9) reported that children with mucopolysaccharidosis can be treated in a similar fashion if they have triggering associated with their carpal tunnel syndrome. In these patients, release of the A1 and A3 pulleys may be necessary, and occasional removal of a superficialis slip will provide some overall functional improvement.
Author's note
I have collected 89 papers in my files regarding this subject. All have been culled, but by far the most useful has been the lengthy paper by Ryzewicz and Wolf. I am grateful to them for permission to reproduce their Figure 1, and I trust that I can heartily recommend quotes from their paper and not be guilty of rampant plagiarism.
References
- 1.Notta A. Recherches sur une affection particuliere des gaines tendineuses de la main. Arch Gen Med. 1850;24:142. [Google Scholar]
- 2.Dobyns JH. Trigger digits. In: Green DP, editor. Operative Hand Surgery. 3rd ed. Vol. 1. New York: Churchill Livingstone; 1993. p. 374. [Google Scholar]
- 3.Ryzewicz M, Wolf JM. Trigger digits: principles, management, and complications. J Hand Surg [Am] 2006;31(1):135–146. doi: 10.1016/j.jhsa.2005.10.013. [DOI] [PubMed] [Google Scholar]
- 4.Bonnici AV, Spencer JD. A survey of ‘trigger finger’ in adults. J Hand Surg [Br] 1988;13(2):202–203. doi: 10.1016/0266-7681_88_90139-8. [DOI] [PubMed] [Google Scholar]
- 5.Hueston JT, Wilson WF. The aetiology of trigger finger explained on the basis of intratendinous architecture. Hand. 1972;4(3):257–260. doi: 10.1016/s0072-968x(72)80010-x. [DOI] [PubMed] [Google Scholar]
- 6.Sampson SP, Badalamente MA, Hurst LC, Seidman J. Pathobiology of the human A1 pulley in trigger finger. J Hand Surg [Am] 1991;16(4):714–721. doi: 10.1016/0363-5023(91)90200-u. [DOI] [PubMed] [Google Scholar]
- 7.Freiberg A, Mulholland RS, Levine R. Nonoperative treatment of trigger fingers and thumbs. J Hand Surg [Am] 1989;14(3):553–558. doi: 10.1016/s0363-5023(89)80024-3. [DOI] [PubMed] [Google Scholar]
- 8.Le Viet D, Tsionos I, Boulouednine M, Hannouche D. Trigger finger treatment by ulnar superficialis slip resection (U.S.S.R.) J Hand Surg [Br] 2004;29(4):368–373. doi: 10.1016/j.jhsb.2004.03.004. [DOI] [PubMed] [Google Scholar]
- 9.Van Heest AE, House J, Krivit W, Walker K. Surgical treatment of carpal tunnel syndrome and trigger digits in children with mucopolysaccharide storage disorders. J Hand Surg [Am] 1998;23(2):236–243. doi: 10.1016/S0363-5023(98)80120-2. [DOI] [PubMed] [Google Scholar]