Abstract
The present study evaluates the effectiveness of ischemic preconditioning and Bcl-2 overexpression against the liver and lung damage that follow hepatic ischemia-reperfusion and investigates the underlying protective mechanisms. Preconditioning and Bcl-2, respectively, reduced the increased tumor necrosis factor (TNF) and macrophage inflammatory protein-2 (MIP)-2 levels observed after hepatic reperfusion. Bcl-2 overexpression or anti-MIP-2 pretreatment seems to be more effective than preconditioning or anti-TNF pretreatment against inflammatory response, microcirculatory disorders, and subsequent hepatic ischemia-reperfusion injury. Furthermore, each one of these strategies individually was unable to completely inhibit hepatic injury. The combination of preconditioning and Bcl-2 overexpression as well as the combined anti-TNF and anti-MIP-2 pretreatment totally prevented hepatic injury, whereas the benefits of preconditioning and Bcl-2 were abolished by TNF and MIP-2. In contrast to preconditioning, Bcl-2 did not modify lung damage induced by hepatic reperfusion. This could be explained by the differential effect of both treatments on TNF release. Anti-TNF therapy or preconditioning, by reducing TNF release, reduced pulmonary inflammatory response, whereas the benefits of preconditioning on lung damage were abolished by TNF. Thus, the induction of both Bcl-2 overexpression in liver and preconditioning, as well as pharmacological strategies that simulated their benefits, such as anti-TNF and anti-MIP-2 therapies, could be new strategies aimed to reduce lung damage and inhibit the hepatic injury associated with hepatic ischemia-reperfusion.
Hepatic ischemia-reperfusion (I/R) injury remains a significant limitation of both liver resectional surgery and liver transplantation and may be responsible for liver failure, lung injury, and death. 1-4 Inflammation is considered to be a major cause of I/R-induced tissue injury. The local inflammatory reaction that follows reperfusion involves multiple inflammatory mediators, recruitment of neutrophils, platelet aggregation, and neutrophil-endothelium interactions. 5,6 Indeed, pharmacological treatments that focus on the inhibition of individual mediators involved in the inflammatory response often ameliorate but are not sufficient to prevent hepatic I/R injury. 7-9 Thus, there is a need for alternative strategies for the treatment of hepatic lesions associated with I/R.
Recent studies in experimental models of renal I/R indicates that apoptotic cell death, either directly or indirectly, significantly contributes to I/R-induced inflammation, as well as to the subsequent tissue damage. 10,11 Thus, the inhibition of apoptosis with Z-Val-Ala-Asp-CH2H (Z-VAD) effectively prevented macrophage inflammatory protein (MIP)-2 up-regulation and the ensuing neutrophil influx and functional impairment. The concept of apoptosis-induced inflammation after I/R offers important new opportunities to effectively prevent clinical manifestations of reperfusion injury, since the blockade of apoptosis could reduce the inflammatory response and the subsequent hepatic I/R injury. The various aspects of apoptosis are regulated, independently, by different control systems. 12,13 This implies that inhibition of ongoing apoptosis by external agents is extremely difficult toachieve, whereas the induction of overexpression of apoptosis-inhibitory proteins such as Bcl-2, probably by acting simultaneously in a pleiotropic fashion on several aspects of the early effector stage, could be more effective in preventing apoptosis and hence hepatic I/R injury. 12,13 Previous studies have shown Bcl-2 to be protective in the liver in different experimental models, including hepatic I/R, 14-17 although the mechanisms by which Bcl-2 confers protection remain to be elucidated. We hypothesize that Bcl-2 overexpression in liver could protect against the deleterious effects of ischemia on ATP and GSH depletion. Several biological effects of Bcl-2 on intact cells have been reported, including increases in antioxidants and ATP preservation. 12,13,18,19 Furthermore, the possibility that Bcl-2 could protect against the liver and lung damage following hepatic I/R, by reducing the increased MIP-2 levels, could be considered. For this, we need to take into in account previous studies in renal I/R indicating that Bcl-2 is able to reduce MIP-2 up-regulation, thus reducing the inflammatory response 11 ; the fact that hepatic I/R is associated with increased MIP-2 levels 20 ; and previous studies in several inflammatory diseases indicating that this chemokine is involved in liver and lung damage. 21,22 Accordingly, the potential protective mechanisms of Bcl-2 on hepatic I/R have been investigated in the present work.
Another new protective strategy against I/R injury is ischemic preconditioning. This is an endogenous mechanism, consisting of repetitive, short periods of ischemia separated by intermittent reperfusion, that protects against subsequent sustained I/R injury. This phenomenon, firstly described in the heart by Murray et al in 1986, 23 has been recently reported in the liver. 24 Preconditioning, by reducing tumor necrosis factor (TNF) release, is able to attenuate the inflammatory damage in both, liver and lung following hepatic I/R. 25,26 Recent studies in an experimental model of normothermic ischemia indicated that preconditioning also confers protection by inhibiting pro-apoptotic mechanisms including the activation of caspases but did not result in up-regulation of antiapoptotic factors such as Bcl-2. 27 Ischemic preconditioning ameliorated but was unable to prevent hepatic I/R injury. Taking into in account the important antiapoptotic role of Bcl-2 in liver 13,17 and that apoptosis contributes to renal I/R induced inflammation, 10,11 we hypothesized that the induction of Bcl-2 overexpression could potentiate the resistance to hepatic I/R injury already conferred by ischemic preconditioning.
To date, no protective strategies are available in the clinical practice to effectively prevent hepatic I/R injury. The present study compares the effectiveness of surgical and genetic strategies, such as preconditioning and Bcl-2 overexpression against liver and lung damage that follow hepatic I/R, and investigates the underlying protective mechanisms. The aim is to ascertain whether the use of combined preconditioning and gene therapy approaches may contribute to the development of novel strategies for preventing hepatic I/R injury.
Materials and Methods
Experimental Animals
Transgenic mice overexpressing Bcl-2 and nontransgenic littermates (CBA/B6D2) weighing between 25 and 30 g were used in this study. Animals were anesthetized with ketamine (100 mg/kg) and xylazine (8 mg/kg). 15
Surgical Procedure
To induce hepatic ischemia, laparotomy was performed and the blood supply to the left lateral lobe was interrupted by placement of a bulldog clamp to the vascular pedicle. 27 Reflow was initiated by removing the clamp. This study was performed in accordance to the European Union regulations (Directive 86/609 EEC) for animal experiments.
Experimental Design
Protocol 1
To evaluate the effect of preconditioning and Bcl-2 overexpression on the liver and lung damage consequent to hepatic reperfusion, the following experimental groups were studied.
Group 1. Cont (n = 6): Control, anesthesia, and laparotomy.
Group 2. I (n = 12): 90 minutes of ischemia followed by 6 hours (n = 6) or 24 hours (n = 6) of reperfusion.
Group 3. PC (n = 12): As group 2 but with previous preconditioning induced by 10 minutes of ischemia followed by 15 minutes of reperfusion. This preconditioning period has been demonstrated to be the most effective against the hepatic injury in the same experimental model shown in the present study. 27
Group 4. Bcl (n = 12): Transgenic animals overexpressing Bcl-2 in the liver were subjected to the same surgical procedure as in group 2.
Group 5. Bcl+PC (n = 12): Transgenic animals overexpressing Bcl-2 in the liver were subjected to the same surgical procedure as group 3.
To evaluate the role of P-selectin, TNF and MIP-2 on the protective effects of Bcl-2 and ischemic preconditioning on the liver and lung damage induced by hepatic I/R, the following experimental groups were studied:
Group 6. aPsel (n = 12): Same surgical procedure as group 2, but animals were subjected to administration of a mAb directed against P-selectin, RMP-1 (Upjohn Laboratories, Kalamazoo, MI) at dose of 1 mg/kg, 5 minutes prior to ischemia. 28
Group 7. GdCl (n = 12): Same surgical procedure as group 2 but animals were treated with gadolinium chloride (Sigma Chemical Co., St. Louis, MO) to inactivate Kupffer cells at dose of 10 mg/kg, 24 hours before ischemia. 29
Group 8. aTNF (n = 12): Same surgical procedure as group 2, but animals were subjected to administration of a rabbit anti-TNF-α polyclonal antibody directed against mouse TNF (Endogen, Boston, MA) at dose of 3 mg/kg, 30 minutes before ischemia. 26
Group 9. aMIP (n = 12): Same surgical procedure as group 2 but animals were subjected to administration of a rabbit polyclonal antibody directed against mouse MIP-2 (Biosource, Camarillo, CA), at dose of 8 mg/kg, 5 minutes before ischemia. 30
Group 10. aTNF+aMIP (n = 12): Same surgical procedure as group 2, but animals were subjected to administration of a rabbit anti-TNF-α polyclonal antibody directed against mouse TNF, at dose of 3 mg/kg, 30 minutes before ischemia 26 and rabbit polyclonal antibody directed against mouse MIP-2 at dose of 8 mg/kg, 5 minutes before ischemia. 30
Group 11. PC+TNF (n = 12): Same surgical procedure as group 3 but animals were treated with TNF (Endogen, Woburn, MA) at dose of 20 μg/kg, 5 minutes before preconditioning. 26
Group 12. Bcl+MIP (n = 12): Transgenic animals overexpressing Bcl-2 in the liver were subjected to the same surgical procedure as group 2 but treated with murine MIP-2 (Endogen, Woburn, MA) at dose of 20 μg/kg, 5 minutes before ischemia. 31
Group 13. Bcl+PC+TNF+MIP (n = 12): Transgenic animals overexpressing Bcl-2 in the liver were subjected to the same surgical procedure as group 3 but treated with TNF at dose of 20 μg/kg, 26 and MIP-2 at dose of 20 μg/kg, 5 minutes before preconditioning. 31
Group 14. Bcl+PC+TNF+MIP+aPsel (n = 12): Transgenic animals overexpressing Bcl-2 in the liver were subjected to the same surgical procedure as group 3, but treated with TNF at dose of 20 μg/kg, 26 MIP-2 at dose of 20 μg/kg, 31 and a mAb directed against P-selectin (RMP-1), at dose of 1 mg/kg, 5 minutes before preconditioning. 28
Group 15. PC+aMIP (n = 12): Same surgical procedure as group 3 but animals were treated with rabbit polyclonal antibody directed against mouse MIP-2, at dose of 8 mg/kg, 5 minutes before preconditioning. 30
Group 16. Bcl+aTNF (n = 12): Transgenic animals overexpressing Bcl-2 in the liver were subjected to the same surgical procedure as group 2 but treated with a rabbit anti-TNF-α polyclonal antibody directed against mouse TNF, at dose of 3 mg/kg, 30 minutes before ischemia. 26
In these studies, control experiments for P-selectin, TNF, and MIP-2 were performed by administration of non-bindings Abs.
Hepatic blood perfusion was measured in liver throughout 1 hour of reperfusion. After 6 or 24 hours of hepatic reperfusion, liver and lung samples were collected. TNF and MIP-2 levels were measured in liver and plasma samples. Malondialdehyde (MDA) levels, myeloperoxidase (MPO) activity, vascular permeability and edema were analyzed in liver and lung samples. Histological and immunohistochemical studies of P-selectin in liver and lung were also performed.
Protocol 2
To evaluate the effect of preconditioning and Bcl-2 overexpression on ATP degradation and GSH depletion during hepatic ischemia, additional experimental groups as 2, 3, 4, and 5 were subjected to hepatic ischemia without the reperfusion period. After sustained ischemia, liver samples were obtained, immediately frozen and maintained at −80°C until analytical determinations of nucleotides (adenine nucleotides, adenine nucleosides, and bases), lactate and GSH.
Generation of Transgenic Mice Overexpressing BCL-2 in the Liver
These transgenic mice express the human Bcl-2 cDNA under the control of the liver-specific pyruvate kinase promoter. An 0.9-kb fragment corresponding to the human Bcl-2 α cDNA was linked to the regulatory regions of the rat L-type pyruvate kinase (L-PK) extending from position −5700 bp to position +712 bp in the second exon. Mutation of the Bcl-2 α initiation codon ATG (ATG into ACG) leads to the synthesis of two hybrid PK-Bcl-2 proteins, whose translation starts in the first and second exon of the L-PK gene. Transgenic mice were identified by Southern blot analysis and hybridized with the 0.9-kb fragment containing the Bcl-2 α coding sequence. The transgene copy number was determined by densitometric scanning. 17
Biochemical Determinations
Nucleotide Analysis
Liver samples were freeze-clamped and immediately homogenized in 10 volumes of 3.6% HClO4. Following homogenization, tissues were allowed to extract for 30 minutes at 0.5°C, and then centrifuged at 850 × g for 15 minutes. Supernatants were adjusted to pH 6.0–6.5 and centrifuged at 14,000 × g. Then, 50 μl of the supernatant was injected in a Waters 717 plus Autosampler liquid chromatographic equipment. Nucleotide profiles were obtained using a reversed-phase Spherisorb ODS column (C18, 5 μm particle size, 15 × 0.4 cm; Teknokroma, San Cugat, Spain) coupled to a 600 HPLC system (Waters, Milford, MA) equipped with a Waters 996 Photodiode Array Detector. The absorbance was monitored at 254 nm. Nucleotide separation was allowed to proceed in a isocratic fashion with 100 mmol/L ammonium phosphate (pH 5.5), until ATP, ADP, hypoxanthine, xanthine, and AMP were separated. At this point, a mixture of water/methanol (96:4) was introduced into the column, eluting inosine. A mixture of water/methanol (60:40) was introduced after inosine to elute adenosine. 32 Calibration chromatograms for the standards ATP, ADP, AMP, adenosine, inosine, hypoxanthine, and xanthine were generated by injecting 50 μl of a mixture of known concentrations. The profiles were processed by a Millennium system.
Lactate Content
Livers were freeze-clamped and the lactate extracted with H2O/acetone (1:1.2, v/v). 32 The lactate content was measured using a commercial kit from Boehringer Mannheim.
Glutathione Measurement
For the analysis of GSH, liver samples were homogenized in 1.1% KCl. After protein precipitation, the samples were neutralized with 10% K2CO3. The amount of GSH was measured using glutathione transferase and 1-chloro-2,4-dinitrobenzene. 33 Fifty microliters of the previous treated sample were mixed with 225 μl of 0.1 mol/L potassium phosphate buffer, pH 7.0, and 10 μl of 10 mmol/L 1-chloro-2,4-dinitrobenzene in ethanol. The reaction was started with 5 μl of glutathione transferase solution (12 U/L) and monitored at 340–400 nm, reaching the end-point 5 minutes after enzyme addition.
Lipid Peroxidation Assay
Lipid peroxidation has been used as an indirect measurement of oxidative damage induced by reactive oxygen species (ROS). 34 Lipid peroxidation in liver and lung samples was determined by the thiobarbiturate (TBA) reaction measuring the formation of malondialdehyde (MDA). 35 For this purpose, 2 ml of trichloroacetic acid (20%) was added to 2 ml of homogenate. After mixing and centrifuging, 1 ml of TBA-water solution (0.67%) was added to the supernatant and boiled for 60 minutes. After cooling, the optical density at 530 nm was measured.
Myeloperoxidase Assay
Myeloperoxidase (MPO) has been used as a marker of neutrophil infiltration and activation. 36,37 MPO activity was measured photometrically using 3,3′,5,5′-tetramethylbenzidine as a substrate. 38 Liver and lung samples were macerated with 0.5% hexadecyltrimethylammonium bromide in 50 mmol/L phosphate buffer, pH 6. Homogenates where then disrupted for 30 seconds using sonication and subsequently snap-frozen in dry ice and thawed on three consecutive occasions before a final 30 second sonication. Samples were incubated at 60°C for 2 hours and then spun down at 4000 × g for 12 minutes. Supernatants were collected for MPO assay. Enzyme activity was assayed photometrically. The assay mixture consisted of 20 μl of supernatant, 10 μl of tetramethylbenzidine (final concentration 1.6 mmol/L) dissolved in dimethylsulfoxide and 70 μl of H2O2 (final concentration 3.0 mmol/L) diluted in 80 mmol/L phosphate buffer, pH 5.4. An enzyme unit is defined as the amount of enzyme that produces an increase of 1 absorbance unit per minute.
Vascular Permeability Analysis
Vascular permeability in liver and lung was estimated using the Evans Blue method. Animals received 20 mg/kg of Evans Blue by cava vein injection 15 minutes prior to sacrifice. Tissues were added to 10 volumes of deionized formamide and incubated at room temperature for 24 hours and the Evans Blue extracted from tissue was quantitated by spectrophotometric analysis and compared to results obtained from standards of known concentrations. 25
Edema Formation
After resection, liver and lung samples were weighed and then placed in an oven at 55°C until a constant weight was obtained. In this determination, edema is represented by an increase in the wet-to-dry weight ratios. 25
TNF and MIP-2 Assay
For liver TNF assay, tissues were homogenized in 10 volumes of 50 mmol/L phosphate buffer (pH 6), and after centrifugation at 4000 × g, the supernatants were frozen at −20°C and saved for measurement of TNF levels. 26 For liver MIP-2 assay, tissue were homogenized in 5 mmol/L phosphate-buffered saline (pH 7.5) containing an antiprotease cocktail consisting of 2 mmol/L phenylmethylsulfonyl fluoride and 1 mg/ml each antipain, aprotinin, leupeptin, and pepstatin A and centrifuged at 2000 × g for 15 minutes. The supernatants were then filtered through a 1.2-μm filter, stored at −70°C, and saved for measurement of MIP-2 levels. 20 Blood samples obtained from the cava vein were centrifuged to obtain plasma, and 100-μl aliquots of plasma were saved for measurement of TNF and MIP-2 levels. TNF and MIP-2 levels in liver and plasma were measured using commercial immunoassay kits from Biosource (Camarillo, CA).
Hepatic Injury
Evaluation of hepatic injury was performed by enzymatic determinations of aspartate aminotransferase (AST) and alanine aminotransferase (ALT) plasma levels using a commercial kit from Boehringer Mannheim (Munich, Germany).
Protein Measurement
Total protein concentration in liver and lung homogenates was determined using a commercial kit from Bio-Rad (Munich, Germany).
Hepatic Blood Perfusion Measurement
Hepatic microcirculation was analyzed using a laser-Doppler blood flowmeter (model LD5000, Transonic Systems Inc., Ithaca, NY). A fiber optic probe was positioned against the surface of the left lobe of the liver for monitoring hepatic perfusion. The laser-Doppler flowmeter provides continuous measurement of relative changes in microcirculatory blood flow in various tissues. 39
Histology
Liver and lung samples were obtained, fixed in 10% neutral buffered formalin, paraffin-embedded (Sigma, Madrid, Spain), cut into 5-μm sections, and stained with hematoxylin-eosin according to standard procedures.
Immunohistochemical Study of P-Selectin Expression
To detect P-selectin in formalin-fixed and paraffin-embedded tissues, sections were placed in 0.01 mol/L citrate buffer (pH 6) and heated for 10 minutes in a microwave oven for antigen retrieval. 40 After blocking nonspecific binding, sections were incubated with the primary rabbit polyclonal antibody against mouse P-selectin from Pharmingen (San Diego, CA) diluted 1:50 in 0.05 mol/L Tris-buffered saline (pH 7.6) at 4°C overnight. A biotinylated goat anti-rabbit Ig G (Dako, Glostrup, Denmark) was used as a secondary antibody diluted in Tris-buffered saline, pH 7.6, at 1:200. Reactions were developed with the avidin-biotin horseradish peroxidase complex using as chromogen 0.05% solution of 3,3′-diaminobenzidine with 0.03% H2O2 in 0.1 mol/L imidazole buffer (pH 7.1). Sections incubated with isotype-matched antibodies served as negative control. 40
Statistics
Data are expressed as means ± SEM. Mean of different groups were compared using a one-way analysis of variance. Student’s t-test was performed for evaluation of significant differences between groups. Significance was determined at the 5% level (P < 0.05).
Results
A significant increase in hepatic TNF and MIP-2 levels were observed after 6 and 24 hours of hepatic reperfusion. As it has been postulated that Kupffer cells are one of the main sources of TNF and MIP-2, 21,41 these cells were inactivated with GdCl3. As shown in Figure 1 ▶ , GdCl3 treatment prevented the significant increase in hepatic TNF and MIP-2 levels. The administration of anti-TNF and anti-MIP-2 antibodies before ischemia (aTNF+aMIP) resulted in hepatic TNF and MIP-2 levels similar to those of the control group. The effect of preconditioning and Bcl-2 overexpression on TNF and MIP-2 levels was evaluated. The induction of preconditioning (PC) reduced the increased TNF levels but did not modify the increases in MIP-2 levels observed after hepatic reperfusion. By contrast, Bcl-2 overexpression (Bcl) reduced the increased MIP-2 levels but did not modify TNF values. The combined strategies, preconditioning and Bcl-2 overexpression, (Bcl+PC) reduced both the increased TNF and MIP-2 levels. The administration of TNF and MIP-2 to the Bcl+PC group (Bcl+PC+TNF+MIP) resulted in hepatic TNF and MIP-2 levels similar to those observed after hepatic reperfusion. These results closely match those observed for plasma TNF and MIP-2.
Figure 1.
TNF and MIP-2 levels in liver and plasma after 6 hours and 24 hours of hepatic reperfusion. Cont, control, anesthesia and laparotomy; I, 90 minutes of ischemia; GdCl, I+GdCl3; aTNF+aMIP, I+anti-TNF and anti-MIP-2 antibodies; PC, I with previous preconditioning induced by 10 minutes of ischemia followed by 15 minutes of reperfusion; Bcl, I in transgenic animals overexpressing Bcl-2; Bcl+PC, PC in transgenic animals overexpressing Bcl-2; Bcl+PC+TNF+MIP, PC+Bcl+TNF and MIP-2 administration. *P < 0.05 vs. Cont; +P < 0.05 vs. I.
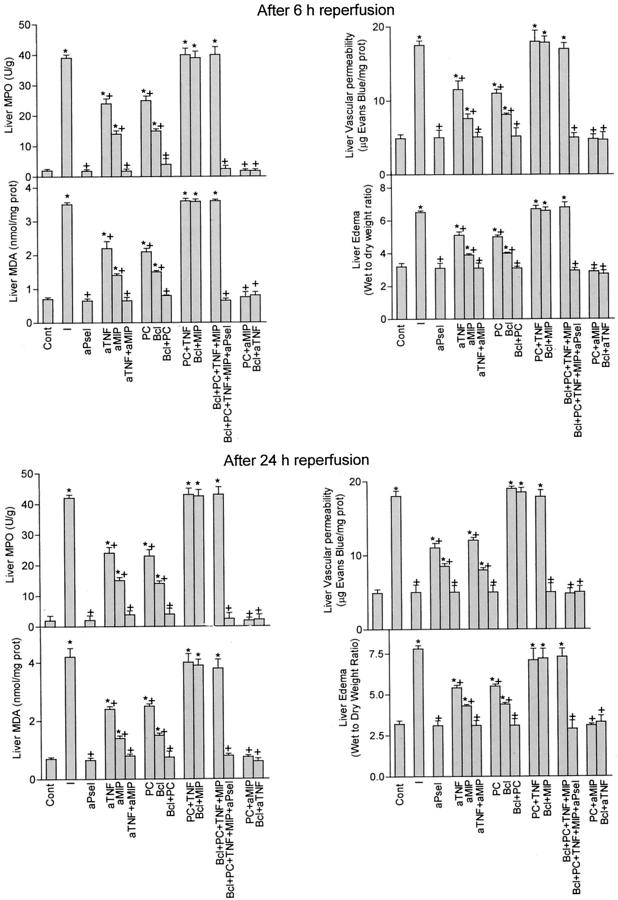
As shown in Figure 2 ▶ , the administration of antibodies against anti-P-selectin before ischemia (aPsel) prevented neutrophil accumulation in liver and this was associated with MDA, vascular permeability, and edema values similar to those observed in control group. Reduced transaminase levels with respect to those observed after hepatic reperfusion were found (Figure 3) ▶ . In addition, the changes in MPO levels in the different groups of study were reflected in changes in MDA, vascular permeability and values of edema. These results suggest that neutrophil accumulation is at least partially responsible for the microvascular disorders, oxidative stress, and edema formation observed after hepatic reperfusion. Anti-TNF or anti-MIP-2 pretreatment (aTNF, aMIP-2) as well as the induction of preconditioning or Bcl-2 overexpression (PC, Bcl) were effective in reducing the overall inflammatory response in liver and the hepatic reperfusion injury (Figures 2 and 3) ▶ ▶ . However, anti-MIP-2 pretreatment or Bcl-2 overexpression (aMIP, Bcl) resulted in biochemical parameters of inflammatory response and hepatic injury lower that those observed when anti-TNF therapy or preconditioning were carried out. As shown in Figure 1 ▶ , in contrast to anti-TNF pretreatment, preconditioning reduced but did not completely prevent the increased TNF levels observed after hepatic reperfusion. However, the beneficial effect of both treatments (aTNF, PC) on inflammatory response and hepatic injury was similar. These findings suggest that the reduction in TNF levels induced by preconditioning could be enough to prevent the deleterious effects of this mediator. This contention is supported by the observation that a similar inflammatory reaction and hepatic injury in preconditioned animals with or without anti-TNF pretreatment (data not shown). The combined anti-TNF and anti-MIP-2 therapies (aTNF+aMIP) as well as the application of both strategies, ischemic preconditioning and Bcl-2 overexpression (Bcl+PC) totally prevented liver I/R-induced inflammation and hepatic injury associated with this process (Figures 2 and 3) ▶ ▶ . As preconditioning (PC) and BCl-2 overexpression (Bcl) respectively, reduced the increases in TNF and MIP-2 observed after hepatic reperfusion (Figure 1) ▶ , we evaluated whether this fact could explain the benefits of these strategies on the inflammatory response and hepatic injury. The administration of TNF in PC and MIP-2 and Bcl-2 groups (PC+TNF, Bcl+MIP) resulted in parameters of inflammatory response and hepatic injury comparable to those observed after hepatic reperfusion (Figures 2 and 3) ▶ ▶ . In addition, similar results were obtained when both TNF and MIP-2 were administered to the Bcl+PC group (Bcl+PC+TNF+MIP). The deleterious effects of both mediators on the inflammatory reaction and hepatic injury were reduced by previous blockade of P-selectin (Bcl+PC+TNF+MIP+aPsel). The administration of anti-TNF antibodies to the Bcl-2 group and anti-MIP-2 to the PC group (PC+aMIP, Bcl+aTNF) could increase the benefits of PC and/or Bcl-2 overexpression. This prevented the inflammatory response and the hepatic damage associated with hepatic reperfusion.
Figure 2.
Effect of preconditioning and Bcl-2 overexpression on the increases in MPO and MDA levels, vascular permeability, and edema seen in liver after 6 and 24 hours of reperfusion. Cont, control, anesthesia and laparotomy; I, 90 minutes of ischemia; aPsel, I+ anti-P-selectin antibody; aTNF, I+ anti-TNF antibody; aMIP, I+ anti-MIP-2 antibody; aTNF+aMIP, I+ anti-TNF and anti-MIP-2 antibodies; PC, I with previous preconditioning induced by 10 minutes of ischemia followed by 15 minutes of reperfusion; Bcl, I in transgenic animals overexpressing Bcl-2; Bcl+PC, PC in transgenic animals overexpressing Bcl-2; PC+TNF, PC+TNF administration; Bcl+MIP, Bcl+MIP-2 administration; Bcl+PC+TNF+MIP, Bcl+PC+TNF and MIP-2 administration; Bcl+PC+TNF+MIP+aPsel, Bcl+PC+TNF+MIP+anti-P-selectin antibody; PC+aMIP, PC+anti-MIP-2 antibody; Bcl+aTNF, Bcl+anti-TNF antibody. *P < 0.05 vs. Cont; +P < 0.05 vs. I.
Figure 3.
Effect of preconditioning and Bcl-2 overexpression on hepatic injury at 6 hours and 24 hours after hepatic reperfusion. Cont, Control, anesthesia and laparotomy; I, 90 minutes of ischemia; aPsel, I+anti-P-selectin antibody; aTNF, I+anti-TNF antibody; aMIP, I+anti-MIP-2 antibody; aTNF+aMIP, I+anti-TNF and anti-MIP-2 antibodies; PC, I with previous preconditioning induced by 10 minutes of ischemia followed by 15 minutes of reperfusion; Bcl, I in transgenic animals overexpressing Bcl-2; Bcl+PC, PC in transgenic animals overexpressing Bcl-2; PC+TNF, PC+TNF administration; Bcl+MIP, Bcl+MIP-2 administration; Bcl+PC+TNF+MIP, Bcl+PC+TNF and MIP-2 administration; Bcl+PC+TNF+MIP+aPsel, Bcl+PC+TNF+MIP+anti-P-selectin antibody; PC+aMIP, PC+anti-MIP-2 antibody; Bcl+aTNF, Bcl+anti-TNF antibody. *P < 0.05 vs. Cont; +P < 0.05 vs. I.
As shown in Figure 4 ▶ , hepatic reperfusion up-regulated P-selectin expression in liver vessels (4B). Both, anti-TNF and anti-MIP-2 pretreatment (aTNF+aMIP) as well as the induction of both strategies, ischemic preconditioning and Bcl-2 overexpression (PC+Bcl, 4C) prevented P-selectin up-regulation. The administration of TNF and MIP-2 to the Bcl+PC group (Bcl+PC+TNF+MIP, 4D) resulted in P-selectin expression similar to that observed after hepatic reperfusion.
Figure 4.

Immunohistochemical detection of P-selectin in liver (A–D) and lung (E–I) at 24 hours after hepatic reperfusion. A: Cont, negative staining. B: I, positive staining in postsinusoidal venules (arrowheads). C: Bcl+PC, negative staining. D: Bcl+PC+TNF+MIP, positive staining in postsinusoidal venules (arrowheads). E: Cont, negative staining. F: I, positive staining in small vessels (arrowheads). G: Bcl, positive staining in small vessels (arrowheads). H: PC, negative staining. I: PC+TNF, positive staining in small vessels (arrowheads). I, 90 minutes of ischemia; PC, I with previous preconditioning induced by 10 minutes of ischemia followed by 15 minutes of reperfusion; Bcl, I in transgenic animals overexpressing Bcl-2; Bcl+PC, PC in transgenic animals overexpressing Bcl-2; PC+TNF, PC+TNF administration; Bcl+PC+TNF+MIP, Bcl+PC+TNF and MIP-2 administration. Original magnification, ×1070.
As for changes in blood flow, Bcl-2 overexpression or the administration of antibodies against anti-MIP-2 (Bcl, aMIP) resulted in higher recoveries of blood hepatic perfusion than when PC or anti-TNF pretreatment were carried out (Figure 5) ▶ . The combination of Bcl-2 overexpression and preconditioning (Bcl+PC) as well as anti-TNF and anti-MIP-2 pretreatment (aTNF+aMIP) totally recovered hepatic blood perfusion. Similar results were observed in PC+aMIP and Bcl+aTNF groups. The benefits of ischemic preconditioning and Bcl-2 overexpression on microcirculatory alterations were abolished with TNF and MIP-2 addition. Hepatic blood perfusion was measured in all groups at 1 hour of reperfusion. From these reperfusion times, the differences in hepatic blood perfusion values observed in experimental groups were unmodified.
Figure 5.
Blood hepatic perfusion measured at 1 hour of hepatic reperfusion. Cont; I, 90 minutes of ischemia; aTNF, I+anti-TNF antibody; aMIP, I+ anti-MIP-2 antibody; aTNF+aMIP, I+TNF and MIP-2 antibodies; PC, I with previous preconditioning induced by 10 minutes of ischemia followed by 15 minutes of reperfusion; Bcl, I in transgenic animals overexpressing Bcl-2; Bcl+PC, PC in transgenic animals overexpressing Bcl-2; PC+TNF, PC+TNF administration; Bcl+MIP, Bcl+MIP-2 administration; Bcl+PC+TNF+MIP, Bcl+PC+TNF and MIP-2 administration; PC+aMIP, PC+anti-MIP-2 antibody; Bcl+TNF, Bcl+anti-TNF antibody. Values are expressed as percentages of the initial blood flow.
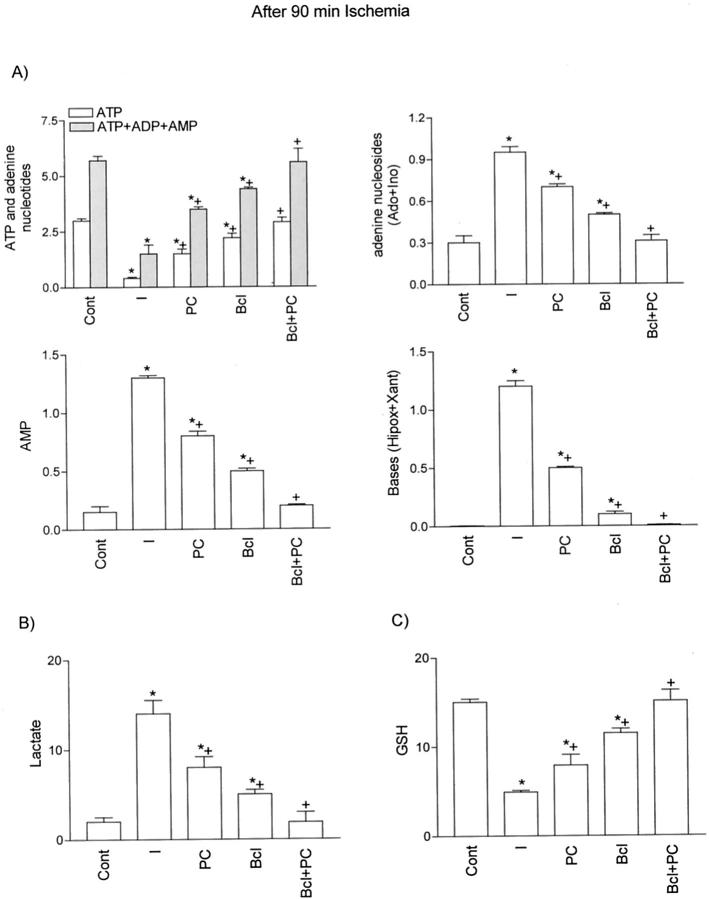
The decrease in ATP and adenine nucleotides (ATP+ADP+AMP) observed during sustained ischemia was associated with a significant increase in adenine nucleosides and bases (Figure 6A) ▶ . Either, preconditioning or Bcl-2 overexpression reduced both ATP and the adenine nucleotide pool depletion as well as the accumulation of adenine nucleosides and bases during sustained ischemia, reflecting a slower adenine nucleotide degradation. Both treatments together (Bcl+PC) resulted in values of ATP, adenine nucleotide, adenine nucleoside and bases similar to those observed in the control group. ATP degradation during ischemia was associated with activation of anaerobic glycolysis, as shown by lactate accumulation (Figure 6B) ▶ . The differences in ATP depletion in all of the experimental groups were reflected in changes in lactate accumulation. As previously reported, 42,43 the deleterious effects of ischemia are not limited to ATP degradation, since decreased GSH levels have also been observed (Figure 6C) ▶ . The effect of preconditioning and/or Bcl-2 overexpression on GSH was similar to that observed for ATP depletion.
Figure 6.
A: Energy metabolism. ATP, adenine nucleotides (ATP+ADP+AMP), adenine nucleosides [lsqb]adenosine (Ado)+ inosine (Ino)[rsqb], AMP and bases (xanthine+hypoxanthine). B: lactate and C: GSH content in liver after 90 minutes of ischemia. Cont, control, anesthesia and laparotomy; I, 90 minutes of ischemia; PC, I with previous preconditioning induced by 10 minutes of ischemia followed by 15 minutes of reperfusion; Bcl, I in transgenic animals overexpressing Bcl-2; Bcl+PC, PC in transgenic animals overexpressing Bcl-2. *P < 0.05 vs. Cont; +P < 0.05 vs. I. Energy metabolic and lactate concentrations are expressed in μmol/g wet wt, and GSH as nmol/mg protein.
The histological study of the liver after hepatic reperfusion (I, Figure 7A ▶ ) showed focal and extensive areas of coagulative hepatocyte necrosis, randomly distributed throughout the hepatic parenchyma with polymorphonuclear leukocyte infiltration. The liver of animals previously subjected to preconditioning (PC, Figure 7B ▶ ) showed focal and small areas of coagulative liver necrosis. However, histological sections of liver for Bcl-2 overexpressing mice undergoing ischemia without preconditioning (Bcl-2, Figure 7C ▶ ) showed focal and small areas of incipient liver necrosis. No hepatic lesions were observed in hepatic tissue in the Bcl+PC group (Figure 7D) ▶ .
Figure 7.

Histological lesions in liver (A–D) and lung (E–H) at 24 hours after hepatic reperfusion. A: I, extensive areas of coagulative liver necrosis with neutrophil infiltration. B: PC, small area of coagulative liver necrosis. C: Bcl, small areas of incipient liver necrosis, D: Bcl+PC, no hepatic lesions. E: I, moderate and diffuse thickening of alveolar walls. F: Bcl, moderate and diffuse thickening of alveolar walls. G: PC, no apparent lesions in the lung parenchyma. H: PC+TNF, moderate and diffuse thickening of alveolar walls. I, 90 minutes of ischemia; PC, I with previous preconditioning induced by 10 minutes of ischemia followed by 15 minutes of reperfusion; Bcl, I in transgenic animals overexpressing Bcl-2; Bcl+PC, PC in transgenic animals overexpressing Bcl-2; PC+TNF, PC+TNF administration. Hematoxylin & eosin; original magnification, ×255).
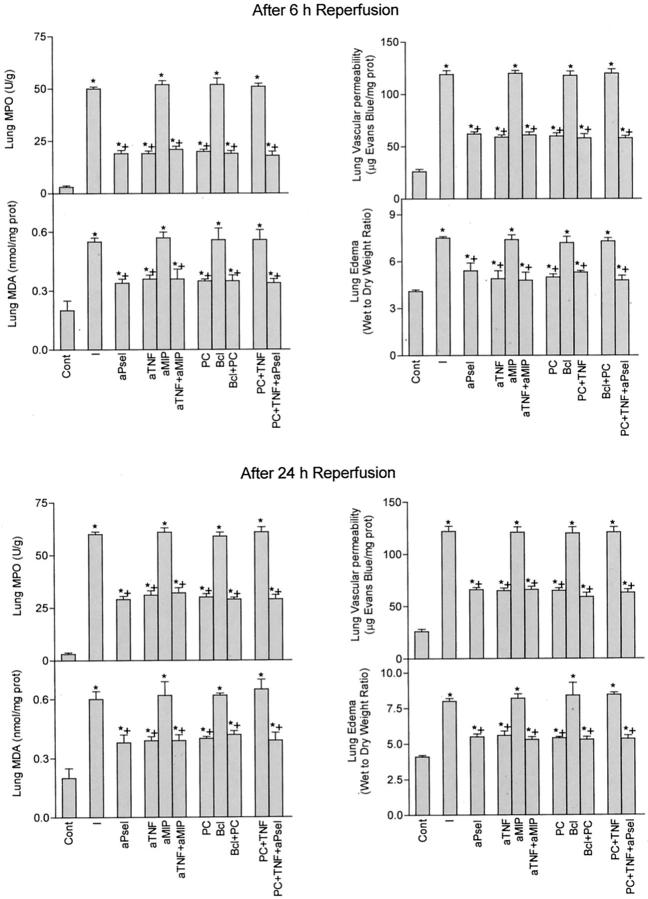
As in liver, anti-P-selectin pretreatment reduced the inflammatory response in lung (Figure 8) ▶ . Anti-MIP-2 pretreatment or Bcl-2 overexpression in the liver (aMIP, Bcl) did not modify lung damage, as indicated by the values of MPO, MDA, vascular permeability, and edema similar to those observed after hepatic reperfusion. On the other hand, anti-TNF pretreatment or the induction of preconditioning (aTNF, PC) attenuated pulmonary inflammatory damage. As in liver, the reduction in TNF levels induced by preconditioning was enough to abolish the deleterious effects of this mediator. No differences in inflammatory response were obtained in preconditioned animals with or without anti-TNF pretreatment (data not shown). As shown in Figure 8 ▶ , the application of both treatments (Bcl+PC), resulted in benefits on lung damage comparable to those observed when only PC was carried out. The administration of TNF in the preconditioned group (PC+TNF) abolished the benefits of preconditioning on lung damage whereas the injurious effect of TNF was prevented with previous anti-P-selectin pretreatment (PC+TNF+aPsel).
Figure 8.
Effect of preconditioning and Bcl-2 overexpression on the lung damage at 6 and 24 hours after hepatic reperfusion. Cont, control, anesthesia and laparotomy; I, 90 minutes of ischemia; aPsel, I+ anti-P-selectin antibody; aTNF, I+anti-TNF antibody; aMIP, I+anti-MIP-2 antibody; aTNF+aMIP, I+ TNF and MIP-2 antibodies; PC, I with previous preconditioning induced by 10 minutes of ischemia followed by 15 minutes of reperfusion; Bcl, I in transgenic animals overexpressing Bcl-2; Bcl+PC, PC in transgenic animals overexpressing Bcl-2; PC+TNF, PC+TNF administration; PC+TNF+aPsel, PC+TNF+anti-Pselectin antibody. *P < 0.05 vs. Cont; +P < 0.05 vs. I.
Immunohistochemical studies revealed P-selectin expression in small vessels of lung following hepatic reperfusion (Figure 4F) ▶ . Similar results were obtained when anti-MIP-2 pretreatment or Bcl-2 overexpression (aMIP; Bcl, Figure 4G ▶ ) were carried out. However, anti-TNF pretreatment or the induction of preconditioning (PC, Figure 4H ▶ ) abrogated the P-selectin up-regulation in lung. TNF administration in PC group (PC+TNF, 4I) resulted in P-selectin expression in lung similar to that observed after hepatic reperfusion (Figure 4) ▶ .
The histological study of the lungs in the I (Figure 7E) ▶ , Bcl-2 (Figure 7F) ▶ , or anti-MIP-2 pretreatment revealed moderate and diffuse septal thickening of the alveolar walls with polymorphonuclear infiltration and perivascular neutrophil infiltration. By contrast, in anti-TNF and PC groups (PC, Figure 7G ▶ ), minimal or no apparent lesions in the lung parenchyma were observed, whereas the administration of TNF to the preconditioned group (PC+TNF, Figure 7H ▶ ) resulted in a thickening of the alveolar wall and neutrophil infiltration much like those observed after hepatic reperfusion.
Discussion
The concept of apoptosis-induced inflammation after I/R was initially reported in kidney. 10,11 To our knowledge, the possibility that the inhibition of apoptosis by Bcl-2 overexpression might reduce the inflammatory response in liver has not been previously tested. The present study shows that the induction of Bcl-2 overexpression seems to be more effective than preconditioning in blunting the inflammatory response and the subsequent hepatic reperfusion injury. Both treatments together, preconditioning and Bcl-2 overexpression are able to completely block the hepatic injury associated with hepatic I/R, being the effects additive. Transaminase levels similar to those in control group and no apparent lesions in the hepatic parenchyma were observed. The mechanisms by which the combination of both strategies prevent hepatic I/R injury were investigated in the present study.
Neutrophils are capable of producing oxidative stress and may contribute to the development of microvascular dysfunctions and edema formation associated with hepatic I/R. 44,45 P-selectin is expressed on the surface of endothelial cells and plays a major role in the recruitment of leukocytes in the hepatic microvasculature after I/R. 46,47 In line with these observations, hepatic reperfusion increased the expression of P-selectin in liver, and anti-P-selectin pretreatment, by preventing neutrophil recruitment, reduced the inflammatory response and hepatic injury associated with this process. Although blockade of TNF or MIP-2 reduced inflammatory reaction and decreased the extent of hepatic injury, these parameters were still elevated compared with control group. However, combined blocking of TNF and MIP-2 prevented the neutrophil accumulation, oxidative stress, alterations in vascular permeability and hepatic edema, observed after hepatic reperfusion. This was associated with transaminase levels similar to those observed in control group and no apparent histological hepatic lesions. These results underscore the key role of these cytokines and chemokines in the pathophysiology of hepatic I/R injury. Thus, taking account that each individual strategy, preconditioning or Bcl-2 overexpression is able to reduce only TNF or MIP-2, respectively, we evaluated whether the combination of preconditioning and Bcl-2 overexpression could prevent inflammatory response and hepatic injury by reducing both the increased TNF and MIP-2 levels observed after hepatic reperfusion. In fact, this turned out to be the case, since the inflammatory response and histological hepatic lesions were abrogated by the combination of preconditioning and Bcl-2 overexpression. The contention that this maneuver exerted their beneficial effect by decreasing TNF and MIP-2 levels is supported by the finding that administration of both TNF and MIP-2 to the Bcl+PC group (Bcl+PC+TNF+MIP) resulted in neutrophil accumulation, oxidative stress, inflammatory response, transaminase levels and histological lesions similar to those observed after hepatic reperfusion. The deleterious effects of TNF and MIP-2 on hepatic reperfusion injury is at least partially related to neutrophil infiltration and inflammatory response, since administration of an anti-P-selectin mAb to the Bcl+PC+TNF+MIP-2 group (Bcl+PC+TNF+MIP+aPsel) significantly reduced the inflammatory reaction and hepatic lesions observed at reperfusion. Nevertheless, anti-P-selectin mAb treatment did not completely abolish the injurious effects of TNF and MIP-2 on hepatic reperfusion injury, suggesting also the involvement of both cytokines and chemokines in other neutrophil-independent mechanisms, including microcirculatory disorders, 48,49 potentially responsible for this pathogenesis. In that regard, the administration of antibodies against both, anti-MIP-2 and anti-TNF prevented the failure in the recovery of hepatic blood perfusion associated with hepatic reperfusion. As regards to the inflammatory response, the benefits of combined preconditioning and Bcl-2 overexpression (Bcl+PC) on microcirculatory alterations could be explained by the reduction in TNF and MIP-2 levels, since its benefits were abolished with TNF and MIP-2 addition (Bcl+PC+TNF+MIP).
Taken together, these results indicate that the reduction in both TNF and MIP-2 could be important to the benefits of ischemic preconditioning and Bcl-2 overexpression on hepatic injury. This would take place by preventing neutrophil accumulation, inflammatory response and microcirculatory disorders associated with hepatic reperfusion. Both strategies could also modulate the deleterious effects of ischemia on ATP and GSH depletion. The effects of both treatments on ATP could be related to an induction of metabolic arrest and/or associated metabolic down-regulation as energetic cost saving mechanisms. 32,50 ATP preservation induced by Bcl-2 overexpression or ischemic preconditioning does not seem to be related to ATP production via anaerobic glycolysis because there is a close inverse relationship between ATP and glycolytic activity, as estimated by lactate production. Consequently, ATP preservation probably results from improving mitochondrial function 51 and/or redistribution of high energy phosphoryl transfer reactions leading to an improved postischemic functional recovery. 52 Similarly, Bcl-2 overexpression could better preserve GSH modifying the activity of enzymes involved in GSH synthesis and degradation 53 and suppressing free radical generation and lipid peroxidation. 18
It has been established that a consequence of hepatic I/R is the induction of important pulmonary pathological alterations, such as adult respiratory distress syndrome associated with human liver transplantation and multiple organ failure associated with primary graft failure. 2,3 There is evidence indicating that this process is mediated by neutrophil infiltration. 36,54 In keeping with this concept, neutrophil accumulation in lung, following hepatic reperfusion, was associated with oxidative stress, microvascular dysfunction, and edema. Considering the results from previous studies in renal I/R, 10,11 we evaluated the possibility that Bcl-2 could protect against the lung damage following hepatic I/R by reducing the systemic release of proinflammatory mediators from the liver, including, MIP-2. However, the studies on the relative role of MIP-2 on neutrophil infiltration in several pulmonary diseases are complex. For example, in a rat model of lung injury induced by intrapulmonary deposition of IgG immune complexes, anti-MIP-2 pretreatment reduced neutrophil infiltration and lung edema, 55 whereas in other inflammatory experimental models, the blocking of MIP-2 had not effect on pulmonary inflammatory response. 56 The published data in hepatic I/R indicate that MIP-2 is involved in lung edema. 57 On the other hand, in the present study, anti-MIP-2 blocking resulted in biochemical and histological parameters of lung damage similar to those observed after hepatic reperfusion, indicating that MIP-2 could not play a central role in lung damage associated with hepatic reperfusion, at least, in the conditions evaluated in the present study. The reason for the discrepancies in findings between both studies of hepatic I/R might be related to the differences in the experimental protocols used, including the percentage of hepatic ischemia and reperfusion times. On the other hand, in our conditions, lung damage appears to center around the TNF, since the administration of anti-TNF antibodies resulted in biochemical parameters of lung damage and histological results similar to those observed in the control group. Thus, the differential effect of ischemic preconditioning and Bcl-2 overexpression on TNF release could explain the different effects of both strategies on pulmonary integrity. In contrast to Bcl-2 overexpression, ischemic preconditioning, by reducing TNF levels, was able to attenuate the lung damage following hepatic reperfusion. The injurious effects of TNF could be mediated by an increase in P-selectin expression.
It is clear from the results presented herein that Bcl-2 overexpression by itself is not sufficient to completely prevent hepatic I/R injury. However, preconditioning is able to partially block the release of effectors of liver and lung damage, including TNF, so that Bcl-2 overexpression is then able to completely prevent hepatic I/R injury. Therefore, we propose that a surgical or pharmacological treatment that prevents the release of effectors of liver and lung damage (ie, preconditioning or anti-TNF pretreatment) may be required to completely inhibit hepatic I/R injury in clinical situations where blocking apoptosis in liver is intended using pharmacological treatments. The combination of ischemic preconditioning and Bcl-2 overexpression could inhibit hepatic injury and reduce lung damage after hepatic reperfusion. The future clinical applications of gene therapy, consisting in the transfection of Bcl-2 will depend on improvements in transfection efficiencies of non-toxic gene delivery systems. On the other hand, after elucidation of the biochemical bases of preconditioning, application of this surgical strategy has already proved successful in hepatic resections in humans 58 and is undergoing evaluation in the field of hepatic transplantation. The comparison of the protective mechanisms of both strategies has provided new and more efficient strategies against hepatic I/R injury. Thus, the results of the present study indicate that combination approaches, such as the use of combined ischemic preconditioning and Bcl-2 overexpression, or anti-TNF and anti-MIP-2 therapies, which simulate their benefits may be specially beneficial since it resulted in elimination of hepatic injury and significant reduction of lung damage in hepatic I/R processes. Intensive investigations will be necessary to evaluate if the benefits of these strategies observed in experimental models of hepatic I/R could be extrapolated to the clinical practice.
Footnotes
Address reprint requests to Dr. Joan Roselló-Catafau, Department of Medical Bioanalysis, Instituto de Investigaciones Biomédicas de Barcelona, CSIC-IDIBAPS, C/Rosellón 161, 6a y 7a Planta, 08036-Barcelona, Spain. E-mail: jrcbam@iibb.csic.es.
Supported by Fundación Marató TV3 and by a Ramón y Cajal Research Contract from the Ministerio de Ciencia y Tecnologia, Madrid, Spain (to C.P. and J.C.P.).
References
- 1.Clavien PA, Harvey PRC, Strasberg SM: Preservation and reperfusion injuries in liver allografts: an overview and synthesis of current studies. Transplantation 1992, 53:957-978 [DOI] [PubMed] [Google Scholar]
- 2.Matuschak GM, Rinaldo JE, Pinski MR, Gavaler JS, Van Thiel DH: Effect of end stage liver failure on the incidence and resolution of the adult respiratory distress syndrome. J Crit Care 1987, 2:162-173 [Google Scholar]
- 3.Ringe B, Pinchlmayr R, Lübbe N, Bornscheuer A, Kuse E: Total hepatectomy as a temporary approach to acute hepatic or primary graft failure. Transplant Proc 1998, 20:552-557 [PubMed] [Google Scholar]
- 4.Pirenne J, Gunson B, Khaleef H, Hubscher S, Afford S, McMaster P, Adams D: Influence of ischemia-reperfusion injury on rejection after liver transplantation. Transplant Proc 1997, 29:366-367 [DOI] [PubMed] [Google Scholar]
- 5.Jaenscke H, Smith CW, Clemens MG, Ganey PE, Roth RA: Mechanisms of inflammatory liver injury: adhesion molecules and cytotoxicity of neutrophils. Toxicol Appl Pharmacol 1996, 139:213-226 [DOI] [PubMed] [Google Scholar]
- 6.Fan C, Zwacka RM, Engelhard JF: Therapeutic approaches for ischemia/reperfusion injury in the liver. J Mol Med 1999, 77:577-592 [DOI] [PubMed] [Google Scholar]
- 7.Lentsch AB, Yoshidome H, Warner RL, Ward PA, Edwards MJ: Secretory leukocyte protease inhibitor in mice regulates local and remote organ inflammatory injury induced by hepatic ischemia/reperfusion. Gastroenterology 1999, 117:953-961 [DOI] [PubMed] [Google Scholar]
- 8.Blonder JM, McCladen TA, Hsia CJ, Billings RE: Polynitroxyl albumin plus tempol attenuates liver injury and inflammation after hepatic ischemia and reperfusion. Life Sci 2000, 17:3231-3239 [DOI] [PubMed] [Google Scholar]
- 9.Kato A, Yoshidome H, Edwards MJ, Lentsch AB: Reduced hepatic ischemia/reperfusion injury by IL-4: potential anti-inflammatory role of STAT6. Inflamm Res 2000, 49:275-279 [DOI] [PubMed] [Google Scholar]
- 10.Daemen M, Veer C, Denecker G, Heemskerk VH, Wolfs T, Clauss M, Vandenabeele P, Buurman WA: Inhibition of apoptosis induced by ischemia-reperfusion prevents inflammation. J Clin Invest 1999, 104:541-549 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Daemen M, De Vries M, Van’t Veer C, Wolfs T, Buurman WA: Apoptosis and chemokine induction after renal ischemia-reperfusion. Transplantation 2001, 71:1007-1011 [DOI] [PubMed] [Google Scholar]
- 12.Hengartner MO: The biochemistry of apoptosis. Nature 2000, 407:770-776 [DOI] [PubMed] [Google Scholar]
- 13.Adams JM, Cory S: Life-or-death decisions by Bcl-2 protein family. Trends Biochem Sci 2001, 26:61-66 [DOI] [PubMed] [Google Scholar]
- 14.Yamabe K, Shimizu S, Kamiike W, Waguri S, Eguchi Y, Hesegawa J, Okuno S, Yoshioka Y, Ito T, Sawa Y, Uchiyama Y, Tsujimoto Y, Matsuda LL: Prevention of hypoxic liver cell necrosis by in vivo human Bcl-2 gene transfection. Biochem Biophys Res Commun 1998, 243:217-223 [DOI] [PubMed] [Google Scholar]
- 15.Bilbao G, Contreras JL, Eckhoff DE, Mikheeva G, Kransykh V, Douglas JT, Thomas FT, Thomas JM, Curiel DT: Reduction of ischemia-reperfusion injury of the liver in vivo adenovirus-mediated gene transfer of the antiapoptotic Bcl-2 gene. Ann Surg 1999, 230:185-193 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Bilbao G, Contreras JL, Gómez-Navarro J, Eckhoff DE, Mikheeva G, Kransnykh V, Hynes T, Thomas FT, Thomas JM, Curiel DT: Genetic modification of liver grafts with an adenoviral vector encoding the Bcl-2 gene improves organ preservation. Transplantation 1999, 67:775-783 [DOI] [PubMed] [Google Scholar]
- 17.Lacronike V, Mignon A, Fabre M, Viollet B, Rouquet N, Molina T, Porteu A, Llerion A, Bouscary D, Varlet P, Joulin V, Kahn A: Bcl-2 protects from lethal hepatic apoptosis induced by an anti-FAS antibody in mice. Nat Med 1996, 2:80-86 [DOI] [PubMed] [Google Scholar]
- 18.Hockenbery DM, Oltvai ZN, Yin XM, Milliman CL, Korsmeyer SJ: Bcl-2 functions in an antioxidant pathway to prevent apoptosis. Cell 1993, 75:241-251 [DOI] [PubMed] [Google Scholar]
- 19.Jacobson MD, Burne JF, King MP, Miyashita T, Reed JC, Raff MC: Bcl-2 blocks apoptosis in cells lacking mitochondrial DNA. Nature 1993, 361:365-369 [DOI] [PubMed] [Google Scholar]
- 20.Colletti LM, Green ME, Strieter RM: The ratio of ELR+ to ELR-CXC chemokines affects the lung and liver injury following hepatic ischemia/reperfusion in the rat. Hepatology 2000, 31:435-445 [DOI] [PubMed] [Google Scholar]
- 21.Gupta S, Feng L, Yoshimura T, Redick J, Fu SM, Rose CE: Intra-alveolar macrophage-inflammatory peptide 2 induces rapid neutrophil localization in the lung. Am J Respir Cell Mol Biol 1996, 3:656-663 [DOI] [PubMed] [Google Scholar]
- 22.Lentsch AB, Yoshidome H, Cheadle WG, Miller FN, Edwards MJ: Chemokine involvement in hepatic ischemia/reperfusion injury in mice: roles for macrophage inflammatory protein-2 and KC. Hepatology 1998, 27:1172-1777 [DOI] [PubMed] [Google Scholar]
- 23.Murray CE, Jenning RB, Reimer KA: Preconditioning with ischemia: a delay in lethal cell injury in ischemic myocardium. Circulation 1986, 74:1124-1136 [DOI] [PubMed] [Google Scholar]
- 24.Peralta C, Hotter G, Closa D, Gelpi E, Bulbena O, Roselló-Catafau J: Protective effect of preconditioning on the injury associated with hepatic ischemia-reperfusion in the rat: role of nitric oxide and adenosine. Hepatology 1997, 320:241-248 [DOI] [PubMed] [Google Scholar]
- 25.Peralta C, Prats N, Xaus C, Gelpí E, Roselló-Catafau J: Protective effect of liver ischemic preconditioning on liver and lung injury induced by hepatic ischemia-reperfusion in the rat. Hepatology 1999, 30:1481-1489 [DOI] [PubMed] [Google Scholar]
- 26.Peralta C, Fernández L, Panés J, Prats N, Sans M, Piqué JM, Gelpí E, Roselló-Catafau J: Preconditioning protects against systemic disorders associated with hepatic ischemia-reperfusion through blockade of tumor necrosis factor-induced P-selectin up-regulation in the rat. Hepatology 2001, 33:100-113 [DOI] [PubMed] [Google Scholar]
- 27.Surinder SY, Sindram D, Perry DK, Clavien PA: Ischemic preconditioning protects the mouse by inhibition of apoptosis through a caspase-dependent pathway. Hepatology 1999, 30:1223-1231 [DOI] [PubMed] [Google Scholar]
- 28.Sans M, Salas A, Soriano A, Prats N, Gironella M, Pizcueta P, Elena M, Anderson DC, Piqué JM, Panés J: Differential role of selectins in experimental colitis. Gastroenterology 2001, 120:1162-1172 [DOI] [PubMed] [Google Scholar]
- 29.Horie Y, Wolf R, Russell J, Shanley TP, Granger DN: Role of Kuffer cells in gut ischemia/reperfusion-induced hepatic microvascular dysfunction in mice. Hepatology 1997, 26:1499-1505 [DOI] [PubMed] [Google Scholar]
- 30.Hiroyuki Y, Lentsch AB, Cheadle WG, Miller FN, Edwards MJ: Enhanced pulmonary expression of CXC chemokines during hepatic ischemia/reperfusion-induced lung injury in mice. J Surg Res 1999, 81:33-37 [DOI] [PubMed] [Google Scholar]
- 31.Bajt ML, Farhood A, Jaeschke H: Effects of CXC chemokines on neutrophil activation and sequestration in hepatic vasculature. Am J Physiol 2001, 281:G1188-G1195 [DOI] [PubMed] [Google Scholar]
- 32.Peralta C, Bartrons R, Riera L, Manzano A, Xaus C, Gelpí E, Roselló-Catafau J: Hepatic preconditioning preserves energy metabolism during sustained ischemia. Am J Physiol 2000, 279:G163-G171 [DOI] [PubMed] [Google Scholar]
- 33.Brigelius R, Muckel C, Akerboom TPM, Sies H: Identification and quantification of glutathione in hepatic protein mixed disulfides and its relationship to glutathione disulfide. Biochem Pharmacol 1983, 32:2529-2534 [DOI] [PubMed] [Google Scholar]
- 34.Baykal A, Kaynaroglu V, Demirpençe E, Kilinç K, Sayek I, Sanaç Y: Experimental study of the effect of adrenaline tolerance on intestinal ischaemia-reperfusion. Br J Surg 1998, 85:947-950 [DOI] [PubMed] [Google Scholar]
- 35.Jha VC, Von Reclinghausen G, Zilliken F: Inhibition of in vitro microsomal lipid peroxidation by isoflavonoids. Biochem Pharmacol 1985, 34:1367-1369 [DOI] [PubMed] [Google Scholar]
- 36.Colletti LM, Remick DG, Burtch GD, Kunkel SL, Strieter RM, Campbell DAJ: Role of tumor necrosis factor-α in the pathophysiologic alterations after hepatic ischemia/reperfusion injury in the rat. J Clin Invest 1990, 85:1936-1943 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Schmekel B, Karlsson SE, Linden M, Sundström C, Tegner H, Venge P: Myeloperoxidase in human lung lavage: a marker of local neutrophil activity. Inflammation 1990, 14:447-454 [DOI] [PubMed] [Google Scholar]
- 38.Trush MA, Egner PA, Kensler TW: Myeloperoxidase as a biomarker of skin irritation and inflammation. Food Chem Toxicol 1994, 32:143-147 [DOI] [PubMed] [Google Scholar]
- 39.Seino Y, Ohki K, Nakamura T, Tsukamoto H, Takano T, Aramaki T, Okumura H, Hayakawa H: Pathophysiological characteristics of cutaneous microcirculation in patients with liver cirrhosis: relationship to cardiovascular hemodynamics and plasma neurohormonal factors. Microvasc Res 1993, 46:206-215 [DOI] [PubMed] [Google Scholar]
- 40.López S, Prats N, Marco AJ: Expression of E-selectin, P-selectin, and intracellular adhesion molecule-1 during experimental murine listeriosis: animal model. Am J Pathol 1999, 155:1391-1397 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Mosher B, Dean R, Harkema J, Remick D, Palma J, Crokett E: Inhibition of Kupffer cells reduced CXC chemokine production and liver injury. J Surg Res 2001, 99:201-210 [DOI] [PubMed] [Google Scholar]
- 42.Stein HJ, Ossthuuizen JMJ, Hinder RA, Lampreschts H: Oxygen-free radicals and glutathione in hepatic ischemia-reperfusion injury. J Surg Res 1991, 50:398-402 [DOI] [PubMed] [Google Scholar]
- 43.Vreugdenhil PK, Belzer FO, Southard JH: Effect of cold store on tissue and cellular glutathione. Cryobiology 1991, 28:143-149 [DOI] [PubMed] [Google Scholar]
- 44.Jaeschke H, Farhood A: Neutrophil and Kupffer cell-induced oxidant stress and ischemia-reperfusion injury in rat liver. Am J Physiol 1991, 23:G355-G362 [DOI] [PubMed] [Google Scholar]
- 45.Suzuki S, Toledo-Pereyra LH, Rodriguez FJ, Cejalvo D: Neutrophil infiltration as an important factor in liver ischemia and reperfusion injury: modulating effects of FK506 and cyclosporine. Transplantation 1993, 55:1265-1272 [DOI] [PubMed] [Google Scholar]
- 46.Sawaya DE, Zibari GB, Minardi A, Bilton B, Burney D, Granger DN, McDolnald JC, Brown M: P-selectin contributes to the initial recruitment of rolling and adherent leukocytes in hepatic venules after ischemia/reperfusion. Shock 1999, 12:233-234 [DOI] [PubMed] [Google Scholar]
- 47.Garcia-Criado FJ, Toledo-Pereyra LH, Lopez-Neblina F, Phillips ML, Paez-Rollys A, Misawa K: Role of P-selectin in total hepatic ischemia and reperfusion. J Am Coll Surg 1995, 181:327-334 [PubMed] [Google Scholar]
- 48.Vollmar B, Glasz J, Leiderer R, Post S, Menger MD: Hepatic microcirculatory perfusion failure is a determinant of liver dysfunction in warm ischemia-reperfusion. Am J Pathol 1994, 145:1421-1431 [PMC free article] [PubMed] [Google Scholar]
- 49.Vollmar B, Glasz J, Post S, Menger MD: Role of microcirculatory derangements in manifestation of portal triad cross-clamping-induced hepatic reperfusion injury. J Surg Res 1996, 60:49-54 [DOI] [PubMed] [Google Scholar]
- 50.Garland JM, Halestrap A: Energy metabolism during apoptosis: Bcl-2 promotes survival in hematopoietic cells induced to apoptose by growth factor withdrawal by stabilizing a form of metabolic arrest. J Biol Chem 1997, 272:4680-4688 [DOI] [PubMed] [Google Scholar]
- 51.Harris MH, Thompson CB: The role of the Bcl-2 family in the regulation of outer mitochondrial membrane permeability. Cell Death Differ 2000, 7:1182-1191 [DOI] [PubMed] [Google Scholar]
- 52.Pucar D, Dzeja PP, Bast P, Juranic N, Macura S, Terzi A: Cellular energetics in the preconditioned state: protective role for phosphotransfer reactions captured by 18O-assisted 31P NMR. J Biol Chem 2001, 276:44812-44819 [DOI] [PubMed] [Google Scholar]
- 53.Das DK, Liu X, Jones RM, Prasad: preconditioning of heart by repeated stunning induces oxidative stress protection and attenuates myocardial reperfusion injury. FASEB J 1991, 5:A8-A16 [Google Scholar]
- 54.Liu DL, Jeppsson B, Hakansson CH, Odselius R: Multiple-system organ damage resulting from prolonged hepatic flow interruption. Arch Surg 1996, 131:442-447 [DOI] [PubMed] [Google Scholar]
- 55.Shanley TP, Schmal H, Warner RL, Schmid E, Friedl HP, Ward PA: Requirement for C-X-C chemokines (macrophage inflammatory protein-2 and cytokine-induced neutrophil chemoattractant) in IgG immune complex-induced lung injury. J Immunol 1997, 158:3439-3448 [PubMed] [Google Scholar]
- 56.Chouchakova N, Skokowa J, Baumann U, Tscherning T, Philippens KM, Nieswandt B, Schmidt RE, Gessner JE: Fc γ RIII-mediated production of TNF-α induces immune complex alveolitis independently of CXC chemokine generation. J Immunol 2001, 166:5193-5200 [DOI] [PubMed] [Google Scholar]
- 57.Hiroyuki Y, Lentsch AB, Cheadle WG, Miller FN, Edwards MJ: Enhanced pulmonary expression of CXC chemokines during hepatic ischemia/reperfusion-induced lung injury in mice. J Surg Res 1999, 81:33-37 [DOI] [PubMed] [Google Scholar]
- 58.Clavien PA, Yadav S, Sindram D, Bentley RC: Protective effects of ischemic preconditioning for liver resection performed under inflow occlusion in humans. Ann Surg 2000, 232:155-162 [DOI] [PMC free article] [PubMed] [Google Scholar]