Abstract
In this study, the authors used an attachment framework to examine how drug-dependent mothers’ early bonding experience, depression, illicit drug use, and perceived support work together to influence the family environment. The authors hypothesized that (a) depression and drug use function as proxies for a stronger risk factor, the perceived absence of support available in everyday life, and (b) associations between mothers’ early bonding experience and family environment are mediated by perceptions of support and nurture available in everyday life. The authors used a “building block” analytic approach and data collected from 125 mothers enrolled in methadone maintenance to test hypotheses. Both hypotheses were confirmed for 1 outcome, family adaptability. For the 2nd outcome, family cohesion, only perceived support was a significant predictor. Although preliminary, the findings suggest that perceptions of relationships in everyday life play a critical role in the etiology of drug-dependent mothers’ parenting.
Mothers who become physically and/or psychologically dependent on illicit drugs (e.g., heroin and cocaine) are at risk for a wide range of parenting deficits beginning when their children are infants and continuing as their children move through school-aged and adolescent years (for a review, see Mayes, 1995). As a group, drug-dependent mothers fare worse than nondrug-dependent mothers on a wide range of parenting indices and more frequently lose their children to foster care than nondrug-dependent mothers (Mayes & Bornstein, 1996). Observations of mother–infant dyads have shown patterns of mothers’ poor sensitivity and responsiveness to infants’ emotional cues juxtaposed with heightened physical activity, provocation, and intrusiveness (Burns, Chethik, Burns, & Clark, 1997; Hans, Bernstein, & Henson, 1999; Mayes et al., 1997; Rodning, Beckwith, & Howard, 1991). Studies reporting perspectives of substance-abusing mothers about parenting have indicated a lack of understanding about basic child development issues, ambivalent feelings about having and keeping children, and lower capacities to reflect on their children’s emotional and cognitive experience (Levy, Truman, & Mayes, 2001; Mayes, 1995; Murphy & Rosenbaum, 1999). Self-reported behaviors among drug-dependent mothers have also revealed harsh, threatening, overly involved, authoritarian parenting styles juxtaposed with permissiveness, neglect, poor involvement, low tolerance of child demands and misbehavior, and parent–child role reversals (Bauman & Dougherty, 1983; Harmer, Sanderson, & Mertin, 1999; Mayes, 1995; Suchman & Luthar, 2000).
Multiple Psychosocial Risk Factors Associated With Maternal Drug Dependence and Parenting
Growing evidence in developmental research indicates that the parenting problems incurred by drug-dependent mothers are not simply a function of drug dependence alone. For instance, a number of studies have shown that, within given samples of drug-dependent mothers, parenting quality varies considerably (Goodman, Hans, & Cox, 1999; Hofkosh et al., 1995; Rodning et al., 1991). In one earlier study, Jeremy and Bernstein (1984) found, in a sample of 31 methadone-maintained mothers of 4-month-old infants, that mothers’ interactions with their infants ranged from poor to adequate. In another study involving 32 opioid-dependent and 37 nondrug-dependent mothers, Hans et al. (1999) reported that, despite having more difficulty fostering interpersonal connection and attunement with their infants, opioid-dependent mothers performed similarly to nondrug-dependent mothers on parenting tasks involving encouragement and guidance. In a third study, with 32 cocaine-using mothers, Hofkosh et al. (1995) found that mothers who were more experienced parents, who were engaged in treatment, and whose partners were not using illicit drugs were capable of providing a home environment that was more conducive to children’s development.
Findings in the developmental and addiction literature suggest, instead, that parenting problems of drug-dependent mothers are more often a function of multiple psychosocial risk factors working together. Psychosocial risk factors associated with maternal drug dependence and the maladaptive parenting practices of drug-dependent mothers occur at multiple levels of influence, including the mother’s early family environment, individual psychological adjustment, and social environment. Evidence of risk factors at each of these levels of influence is summarized in the following sections.
Early Family Environment
The influence of the early caregiving environment, particularly relationships with early caregivers, on subsequent generations of parent–child relationships is well known to developmental psychologists (see Sroufe, Carlson, Levy, & Egeland, 1999), and there is ample evidence that drug-dependent mothers commonly experience multiple disruptions and traumas in the early family context. In their family of origin, drug-dependent women have typically been exposed to higher than average rates of parental death, desertion, discord, divorce, substance abuse, physical abuse, and sexual abuse (Dawe, Harnett, Staiger, & Dadds, 2000; Haller, Knisely, Dawson, & Schnoll, 1993; Widom, Weiler, & Cottler, 1999). The family environment in which drug-using mothers were reared has often been characterized by dysfunctional internal and external boundaries, poor communication, chaotic and rigid interaction patterns, and role distortions and reversals (Bekir, McLellan, Childress, & Gariti, 1993; Luthar & Suchman, 1999; McMahon & Luthar, 1998; Sheridan, 1995). Studies examining the recollections of drug-dependent adults in treatment (including users of opiates, cocaine, and multiple substances) about caregiving in their family of origin consistently characterize parents as emotionally distant and overcontrolling (Bernardi, Jones, & Tennant, 1989; Cosden & Cortez-Ison, 1999; Friedemann & Musgrove, 1994; Schweitzer & Lawton, 1989; Spain & Spain, 1988; Torresani, Favaretto, & Zimmermann, 2000).
Psychological Adjustment
Diagnoses of affect disorders (Hans et al., 1999), anxiety disorders, and personality disorders (Beckwith, Howard, Espinosa, & Tyler, 1999) are common among drug-dependent mothers. In one study of opioid- and cocaine-dependent mothers of 7–17-year-old children, 90% of the mothers met criteria for at least one lifetime Diagnostic and Statistical Manual of Mental Disorders (3rd ed., rev; American Psychiatric Association, 1987) diagnosis in the affective or anxiety category (Luthar, Cushing, Merikangas, & Rounsaville, 1998). The many deleterious effects of maternal depression among disadvantaged women on the mother–child relationship and on children’s behavioral and emotional development have been well documented (for a review, see Lovejoy, Graczyk, O’Hare, & Neuman, 2000). Psychological disturbance among drug-dependent mothers has also been linked with maladaptive parenting in several studies, in some cases accounting for more variance than drug use alone in parenting behavior. In one aforementioned study, Jeremy and Bernstein (1984) were among the first investigators to examine correlates of parenting interactions and found that mothers’ psychological and psychosocial resources (e.g., intelligence, psychopathology, presence of paternal support) were better predictors of parenting interaction quality than drug use per se. In another home-based observation of 78 cocaine-using mothers of infants, Beckwith et al. (1999) found that chronic depression and paranoia during and after pregnancy were associated with less sensitive caregiving at 6 months. Hans et al. (1999) similarly found that personality characteristics and depression predicted many aspects of opioid-dependent mothers’ parenting behavior, even after maternal substance abuse was taken into account.
Substance abuse itself is also a form of psychological maladjustment. Primarily on the basis of clinical observations and interviews, proponents of the self-medication hypothesis of addiction (see Khantzian, 1997; Krystal, 1997; Wurmser, 1997) have conceptualized drug use as a compensatory (albeit self-destructive) attempt to regulate overwhelming and persistent negative affect that otherwise causes extreme levels of emotional distress. Empirical findings from studies examining affect regulation have also generally indicated that drug-dependent adults are less tolerant of affective distress than nondrug-dependent adults and that drug use severity tends to increase along with levels of affect dysregulation (Keller & Wilson, 1994; Krystal, 1997).
Social Environment
Involvement in supportive and satisfying social networks plays an important protective role in parenting processes (see Cochran & Niego, 1995, for a review). Social support in particular (i.e., the perceived availability of others to provide encouragement and support during episodes of emotional distress) has been identified as a critical buffer for parents who face multiple sociodemographic adversities (e.g., single and minority status, poverty, limited access to resources, social stigmatization) in their everyday life as parents. In a comprehensive review of the role of social support in parenting, Cochran and Niego (1995) suggested that, as a buffer, social support helps to “[prevent] the parent from being adversely affected by a stressful event, like divorce or job loss, and [enables] the parent to maintain satisfactory child rearing routines in difficult situations” (p. 403). More so than actual supportive transactions or availability of social support, it is the subjective experience of support that appears to predict well-being and optimal parenting (Polansky, Gaudin, Ammons, & Davis, 1985; Procidano, 1992).
Drug-dependent mothers are highly vulnerable to experiencing limited social support. Many are involved in ongoing adult relationships that reflect a range of problems, including physical, emotional, and sexual abuse (Duncan, Saunders, Kilpatrick, Hanson, & Resnick, 1996; Grice, Brady, Dustan, Malcolm, & Kilpatrick, 1995; Wald, Harvey, & Hibbard, 1995). Perhaps as a means of self-protection against further emotional and physical suffering, drug-dependent mothers often become socially isolated from their peers and other sources of social support (Luthar & Walsh, 1995). Many also engage in antisocial behaviors, such as prostitution, theft, and drug dealing, that may limit their involvement in social networks. Drug-dependent mothers are also exposed to stigma from society and service providers (Chang, Carroll, Behr, & Kosten, 1992; Eliason & Skinstad, 1995; Luthar, Cushing, & McMahon, 1997). More so than other psychiatrically disordered groups, adults diagnosed with substance abuse disorders are often seen as morally reprehensible for willfully and consciously creating problems in their life (Kandall & Gaines, 1991; Murphy & Irwin, 1992).
Attachment Theory: An Explanatory Model of How Psychosocial Risk Factors Work Together to Influence Parenting
Although the above psychosocial risk factors have been clearly identified as correlates of maternal drug dependence and parenting problems, few studies have examined their underlying mechanisms of interaction (i.e., how they work together) in relation to parenting problems encountered by drug-dependent mothers. A theoretically driven, systematic approach to examining how psychosocial vulnerabilities work together is essential for understanding the complex etiology of maladaptive parenting processes involving drug-dependent mothers and their children and for developing intervention strategies based on mechanisms change.
One systematic approach to understanding the etiology of parenting problems is attachment theory, a structural developmental theory that conceives of development as a complex, organic process that builds on preceding experience while also transforming it (Sroufe et al., 1999). Attachment theory began with the theoretical work of John Bowlby (1982), who viewed early attachment relationships as influencing the nature and course of relationships throughout life, especially for intimate love relationships and parenting. At the center of attachment theory is the concept of internal working models—the mental representations that children form from their early relational experience with caregivers. These mental representations include the likely behaviors of caretakers toward the child and the child’s likely cognitive–emotional response, and they are thought to have special significance because they frame a child’s subsequent transactions with the environment with specific preconceptions and interpretive tendencies. Consequently, even in new circumstances, the context is not independent of the child’s relational history (Slade & Aber, 1992; Sroufe et al., 1999).
Attachment theorists have also proposed that early relationships establish the context for the child’s developing capacities for emotional regulation and self-regulation. Self-regulation is the natural outgrowth of the child’s internalization of a parent’s sensitive and containing responses to bids for comfort and care. Although initially this regulatory function occurs only in the context of caregiving relationships, as a child internalizes a general representation of the soothing and responsive caregiving relationship, he or she begins to be able to soothe and regulate himself or herself. Along the same lines, when caregivers are less sensitively responsive to children’s cues for comfort and care, children are thought to internalize a representational model of others as more dismissive, rejecting, and inconsistent and the self as unworthy and unlovable. This generalized model of a less secure relationship is thought to have important implications as both a prototype for subsequent relationships and a precursor for psychological maladjustment (Sroufe et al., 1999).
From the perspective of attachment theory, it seems reasonable to presume that, like generalized internal working models of attachment, adults’ perceptions of social support reflect a general underlying schema of relationships with others in the social environment. This model or schema, derived from early experiences of seeking care, influences how social information is processed and attributions of others are drawn (Anan & Barnett, 1999; Crittenden, 1981, 1985; Crockenberg, 1988; Lakey & Cassady, 1990). Thus, perceptions of support play a central role in explaining how early family environment and individual psychological maladjustment influence the parenting processes of drug-dependent mothers. First, disruptions in the early family environment, particularly in bonding relationships with early care-givers, may predispose drug-dependent mothers to adopt lower generalized expectations for support and nurture from others in their everyday social environment. Early childhood studies partially support this tenet, showing that attachment relationships with early caregivers shape children’s broad-based models of the availability of support from others (Anan & Barnett, 1999). Studies on antecedents of perceived support have also shown links between recollections of early bonding experience and subsequent expectations for social support during adulthood (Asendorpf & Wilpers, 2000; Collins & Feeney, 2000; Ognibene & Collins, 1998; Sarason, Pierce, Bannerman, & Sarason, 1993). In the addiction literature, one study, involving 46 mothers enrolled in an inpatient treatment for alcohol and drug addiction in Australia, has also shown that mothers’ negative childhood experiences (e.g., harsh punishment and neglect) are associated with lowered expectations for social support from family and friends (Harmer et al., 1999).
Second, like internal working models of attachment, perceived social support may transmit or mediate the influence of early bonding experience on subsequent caregiving relationships. In other words, the influence of a mother’s early bonding on subsequent caregiving relationships with children may be mediated by the generalized model she has for support and nurture available in her everyday social environment. Developmental research supports this notion that mothers’ representations of attachment (see van IJzendoorn, 1995, for a review) and perceptions of social support (Crittenden, 1985; Crockenberg, 1988) influence their approach to parenting and their children’s emotional development.
Finally, like internal working models of attachment, the general schema of relationships represented in mothers’ perceptions of social support may reflect a relational context in which psychological maladjustment has developed. Researchers have consistently found a significant relation between perceptions of social support and adult psychological adjustment (Anan & Barnett, 1999; Lakey & Cassady, 1990). In the aforementioned study involving 46 mothers in recovery, Harmer et al. (1999) reported strong associations between mothers’ perceived social support and depression. From an attachment theory perspective, the well-documented associations between psychological maladjustment and parenting problems of drug-dependent mothers may reflect an even stronger relation between a generalized model of social support as absent or unavailable (derived from early bonding disruptions) and problems experienced in caregiving.
In summary, our aim in this study is to use an attachment theory framework to test the following hypotheses about how four psychosocial factors associated with maternal drug dependence (i.e., early bonding, depression, illicit drug use, and perceived support) work together to influence the caregiving experience of drug-dependent mothers:
Drug-dependent mothers’ early bonding experience will be associated with their perceptions of support currently available in their everyday life.
Although drug-dependent mothers’ early bonding experience will be associated with their perceptions of the caregiving relationship with their children, this association will be mediated by their perceptions of social support available in their everyday life.
Associations between mothers’ experiences in the caregiving relationship and (a) depression and (b) drug use severity will be proxies for, or symptoms of, a stronger risk factor—disturbance in perceived availability of support in everyday life.
Method
Participants
Participants in this study were drawn from a cohort of 162 women who were admitted across a 36-month period to a methadone maintenance program for women based in New Haven, Connecticut, and funded by the Center for Substance Abuse Treatment. Two previous studies based on data from this cohort have examined within-gender differences in clinical presentation at the time of admission (see McMahon & Luthar, 2000) and relations between parenting responsibilities and treatment history (see McMahon, Winkel, Suchman, & Luthar, 2002). Complete data for 125 of 132 women, who were the biological mothers of at least one child, were available for analysis. Data for 7 mothers were missing because, shortly after admission, these women were imprisoned, hospitalized, or discharged because they did not return for ongoing treatment.
Demographic data are presented in Tables 1 and 2. The majority of women in this sample were single mothers (85.4%), primarily of European American (41.8%) and African American (41.0%) descent, and had completed a high school education (63.2%). Although a majority of mothers were unemployed at the time of admission (67.5%), half of the mothers (49.6%) reported having a specific profession or skill. On average, mothers in the sample had 2.7 children, whose ages ranged between 1 and 35 years. The majority of mothers (87.2%) had at least one minor child (under 17 years of age) at the time of admission; 72.0% had at least one minor child living with them, and the other 15.2% had recently lost custody of their minor children. On average, the mothers had used heroin and/or other opiates illicitly for 9.5 years.
Table 1.
Demographic Characteristics of the Sample (N = 125)
| Variable | % |
|---|---|
| Marital status | |
| Never married | 47.2 |
| Married | 8.9 |
| Separated/divorced | 38.2 |
| Widowed | 5.7 |
| Ethnicity | |
| European American | 41.8 |
| African American | 41.0 |
| Hispanic origin | 15.5 |
| Native American | 1.6 |
| Education | |
| College/university graduate | 3.2 |
| Partial college training | 20.8 |
| High school graduate/GED | 39.2 |
| Partial high school | 32.0 |
| Junior high school | 2.4 |
| Elementary school | 2.4 |
| Occupation | |
| No profession or skill | 50.4 |
| Employment statusa | |
| Employed (full or part time) | 29.2 |
| Unemployed | 67.5 |
| Student | 3.3 |
| Mother of minor children | |
| Under 6 years | 42.4 |
| Between 6 and 17 years | 75.2 |
| Mother caring for minor children | 72.0 |
During 3 years prior to assessment.
Table 2.
Descriptive Statistics for All Variables (N = 125)
| Variable | M | SD | Clinical cutoff scorea | % sample beyond clinical cutoff |
|---|---|---|---|---|
| Demographic characteristic | ||||
| Mother’s age | 36.0 | 6.1 | ||
| Years of education | 11.8 | 1.9 | ||
| Number of children | 2.7 | 1.3 | ||
| Number of minor children | ||||
| Under 6 years | 0.6 | 0.9 | ||
| Between 6 and 17 years | 1.4 | 1.1 | ||
| Years of opiate use | 9.5 | 7.1 | ||
| Early bonding | ||||
| Care | 21.7 | 7.9 | <19.0b | 38.4 |
| Overprotection | 17.3 | 6.6 | >19.9b | 30.0 |
| Depression | 9.2 | 7.2 | >8.0c | 50.0 |
| Drug use severity | 0.2 | 0.1 | ||
| Perceived support | ||||
| Family | 13.2 | 5.0 | <11.9b | 33.6 |
| Friends | 13.3 | 6.0 | <8.0b | 24.0 |
| Caregiving problems | ||||
| Family adaptability | 30.5 | 9.0 | <19c | 10.0 |
| Family cohesion | 26.9 | 6.4 | <34c | 87.2 |
Corresponds to cutoff scores beyond which scores represent potential vulnerability.
Clinical cutoff scores (means plus 1 standard deviation) derived from published means and standard deviations for comparable normative populations (e.g., women, mothers; cited in Parker et al., 1979; Wade & Procidano, 1986).
Clinical cutoff scores were provided by authors of measures in administration manuals.
Procedure
All mothers completed an assessment interview during the orientation phase of treatment. Interviews were conducted individually by trained clinical assistants, who provided assistance with reading and comprehension as needed. Assessment interviews included a battery of self-report measures of psychosocial adjustment and family environment and standardized assessments of global intelligence and addiction severity.
Constructs and Measures
Early bonding
The majority of mothers enrolled in this study designated their mother as their primary caregiver, and a large percentage (30.0%) reported the absence of their father in any caregiving role. Early bonding experience was therefore defined as early bonding experience with mothers prior to age 16 and assessed with the Parental Bonding Instrument (PBI; Parker, Tupling, & Brown, 1979), a 25-item questionnaire rated on a four-point scale. The PBI consists of two subscales: The 13-item Care scale assesses respondents’ perceptions of their mother’s affection, emotional warmth, and empathy (e.g., “My mother could make me feel better when I was upset”). The 12-item Overprotection scale assesses respondents’ perceptions of their mother’s intrusions and prevention of independence (e.g., “My mother felt I could not look after myself unless she was around”). The PBI has demonstrated satisfactory reliability and validity in other samples of drug-dependent adults (Cosden & Cortez-Ison, 1999; Parker, 1989; Torresani et al., 2000). For this sample, Cronbach’s alpha coefficients were .87 for the Care scale and .73 for the Overprotection scale.
Depression
The Short Form Beck Depression Inventory (BDI-SF; Beck & Beck, 1972), a 13-item questionnaire, served as the measure of general depression. Rated on a four-point scale, the BDI-SF has demonstrated good construct validity (Foelker, Shewchuk, & Niederehe, 1987; Leahy, 1992) and convergent validity with the standard Beck Depression Inventory (Gould, 1982). The BDI-SF has also demonstrated good internal consistency for samples of women (Leahy, 1992) and methadone-maintained patients (Reynolds & Gould, 1981). For this sample, Cronbach’s alpha coefficient was .93.
Drug use severity
The Addiction Severity Index (McLellan et al., 1992), a widely used structured interview designed to document current and lifetime problems commonly associated with substance abuse, was used to assess drug use severity. The composite score of drug use is a widely used standardized rating of problem severity (see McGahan, Griffith, & McLellan, 1986) computed with 13 items pertaining to drug use (e.g., number of days of drug use during the past 30 days, perceived severity of drug use problems). Rather than corresponding to specific levels of clinical severity, the drug use composite is a measure designed to examine relative distress. The reliability and validity of the composite drug use score have been well documented in studies conducted with substance-abusing adults (e.g., Cacciola, Koppenhaver, McKay, & Alterman, 1999; McDermott et al., 1996; McLellan et al., 1992). In this sample, Cronbach’s alpha coefficient for the composite score for drug use was .72.
Perceived support
The Perceived Social Support Scale (PSSS; Procidano & Heller, 1983), a 40-item self-report instrument, was used to measure mothers’ perceptions of emotional support available from family and friends at the time of the interview. The PSSS is rated on a two-point (yes–no) scale and consists of two subscales. One 20-item subscale assesses emotional support available from the mother’s family (e.g., “There is a member of my family I could go to if I were just feeling down, without feeling funny about it later”). The second 20-item subscale assesses emotional support available from the mother’s friends (e.g., “I have a deep sharing relationship with a number of friends”). The psychometric properties of both scales have been described by Procidano and Heller (1983), and the factor structure, reliability, and validity of the instrument have been verified in studies conducted with individuals seeking substance abuse treatment (Rice & Longabaugh, 1996). The family and friend support subscales were conceptually and statistically related (r = .47, p <.001) and had similar relations with other variables, and they were therefore combined into a single measure of social support with an alpha of .88.
Caregiving problems
Mothers’ perceptions of parenting problems were assessed with the Family Adaptability and Cohesion Evaluation Scale (Olson, Portner, & Lavee, 1985), a 20-item questionnaire rated on a five-point scale. The 10-item Adaptability scale assesses parents’ perceptions of the degree of flexibility in their relationship with their children (e.g., “Parents and children discuss punishment together”). Higher scores (30–50) indicate greater flexibility in allowing children to be involved in many aspects of family decisions and rules. Lower scores (10–19) indicate more rigidity, such that the mother (or parents) alone makes decisions and establish rules. The 10-item Cohesion scale assesses parents’ perceptions of emotional bonding versus disengagement among members of the family (e.g., “Family members like to spend free time with each other”). Higher scores on this scale (46–50) indicate greater closeness and cohesion, and lower scores (10–34) indicate detachment and disengagement. The psychometric properties of both scales have been discussed by Olson et al. (1985) and Edman, Cole, and Howard (1990). In this sample, Cronbach’s alpha coefficients were .87 for the Adaptability scale and .68 for the Cohesion scale.
Data Analysis
To examine the predicted relations among factors outlined earlier, we used the “building block” approach outlined by Kraemer, Stice, Kazdin, Offord, and Kupfer (2001) for examining underlying etiological mechanisms involving multiple latent risk factors. Kraemer et al. argued that the etiology of complex phenomena (e.g., parenting processes) is likely to be better explained by patterns of association among multiple latent factors rather than by a single causal chain. Their methodological model involves examining associations among factors on the basis of three criteria—intercorrelation, dominance, and temporal precedence. The first step of the building block approach involves setting aside any factor about which there is some question regarding its status as a factor related to the outcome. The next step involves examining associations among co-occurring variables that are presumed to have no temporal associations. In a series of standard linear regressions, co-occurring factors are examined in pairs to determine how they work together in relation to the outcome. There are three possible ways that co-occurring factors might work together: They may overlap if they are correlated with one another and together explain greater variance in the outcome than either single factor alone. They may operate independently if they are unrelated to each other and each factor explains unique variance in the outcome. Finally, one factor may function as a proxy risk factor for the second factor if the factors are intercorrelated but only the second risk factor explains unique variance in the outcome. Once identified, proxy factors are set aside in all subsequent analyses so as not to confuse or impede understanding of potential causes of the phenomenon of interest. The final step in the building block approach involves organizing remaining factors by temporal precedence and testing the predicted mediation or moderation model. For this step, we followed the specifications for mediation analyses outlined by Baron and Kenny (1986) that four conditions be met to confirm a mediation model. These conditions are tested in a series of linear regressions. First, the predictor (early bonding) must be significantly associated with the hypothesized mediator (perceived support). Second, the predictor must be associated with the dependent measure (family adaptability and/or cohesion). Third, the mediator (perceived support) must be associated with the dependent measure (family adaptability and/or cohesion). Finally, the impact of the predictor (early bonding) on the dependent variable (family adaptability and/or cohesion) must be less after the mediator (perceived support) is controlled for. This final condition is tested in a hierarchical linear regression with the mediator entered first, followed by the predictor.
We also considered structural equation modeling (SEM) for testing the predicted model of associations among factors. SEM has the advantage of testing a complex linear equation within a single model. One important disadvantage of SEM, though, is the inability to specify which particular building block of the model has failed when an overall linear model is rejected. Building a model step by step, checking each new building block before it is set in place, was more advantageous because it allowed for a better understanding of how each risk factor did or did not fit into the model as it was tested.
Results
Descriptive Data
Means and standard deviations for all measures are presented in Table 2. Although mean scores on both indices of early bonding approached but did not surpass clinical cutoff scores, a large percentage of mothers’ scores for each scale surpassed the clinical cutoff, indicating that many mothers in this sample experienced their own mother as lacking affection and being overcontrolling. The mean score for depression surpassed the clinical cutoff score, indicating that, as a group, mothers experienced moderate levels of depression. Mothers’ perceptions of support were, on average, within normal limits, although perceptions of family support approached the clinical cutoff, and a moderate percentage of mothers in the sample scored beyond the clinical cutoff as well. The group mean for family adaptability was within normal limits, reflecting moderate flexibility overall in mothers’ relationships with their children. The group mean and the vast majority of mothers’ scores (87.2%) for cohesion fell beyond the clinical cutoff score, indicating that the majority of the mothers experienced their relationship with their children as detached and disengaged. A majority of mothers (95.2%) met criteria for risk on at least one of the indices measured.
Intercorrelations
To determine whether any covariates should be used in subsequent analyses, we examined relations between the mother variables of early bonding, depression, drug use severity, perceived support, adaptability, and cohesion and the demographic/descriptive variables of maternal age, maternal education, and number of minor children (with separate variables for children under 6 years old and children between 6 and 16 years). Maternal education alone was considered a more stable indicator of socioeconomic status than its combination with employment status for several reasons. Mothers in general often leave the work force to have children (Hoff-Ginsberg & Tardif, 1995), an addictive lifestyle can cause fluctuations in employment status (Suchman & Luthar, 2001), and, in this particular sample, mothers’ problems with employment were prevalent (McMahon & Luthar, 2000). As shown in Table 3, maternal age was correlated with perceived support and family adaptability, maternal education was correlated with perceived support, and neither of the minor child variables was correlated with any mother variable. Maternal age and maternal education were entered as covariates in all subsequent analyses.
Table 3.
Intercorrelations Among Variables (N = 125)
| Variable | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 |
|---|---|---|---|---|---|---|---|---|---|---|---|
| 1. Mother’s age | — | ||||||||||
| 2. Mother’s education | .18* | — | |||||||||
| 3. Total children under 6 years | −.50** | −.10 | — | ||||||||
| 4. Total children 6–17 years | −.09 | .11 | −.03 | — | |||||||
| 5. Maternal care | .05 | .00 | −.06 | .06 | — | ||||||
| 6. Maternal overprotection | −.08 | .06 | −.02 | .05 | −.43** | — | |||||
| 7. Depression | −.06 | −.09 | .04 | −.12 | −.25** | .06 | — | ||||
| 8. Drug use severity | .10 | −.11 | −.17 | −.17 | −.12 | .06 | .39** | — | |||
| 9. Perceived support | .21* | .18* | −.11 | −.02 | .45** | −.23* | −.42** | −.27** | — | ||
| 10. Family adaptability | .22* | .00 | .03 | .13 | .34** | −.08 | −.30** | −.26** | .46** | — | |
| 11. Family cohesion | .10 | .02 | −.08 | −.09 | .14 | −.11 | −.08 | .06 | .21* | .29** | — |
p < .05.
p < .01.
Four of the five factors (maternal care, depression, drug use severity, and perceived support) were correlated with the first outcome, family adaptability, whereas maternal overprotection was not. Following guidelines outlined above, we set aside maternal overprotection in subsequent analyses. Only one of the factors—perceived support—was correlated with the second outcome, family cohesion. We therefore did not conduct subsequent analyses with family cohesion. (Reasons for poor intercorrelation of early bonding and psychological maladjustment with cohesion are discussed later).
Patterns of Association Among the Co-Occurring Factors: Depression, Drug Use, and Perceived Support
To test the hypothesis that depression and drug use severity function as proxies for the more global factor, perceived support, in relation to mothers’ perceptions of the caregiving relationship, and guided by the building block approach, we first examined how each pair of factors worked together in relation to mothers’ perceptions of family adaptability. As shown in Table 3, each of the co-occurring factors (i.e., drug use severity, depression, and perceived support) were correlated with mothers’ perceptions of family adaptability. Drug use and depression were intercorrelated (r = .39, p < .01), as also shown in Table 3. In a standard regression in which family adaptability was regressed simultaneously on depression and drug use, depression and drug use together explained 17.0% unique variance (p < .001), depression explained 4.0% unique variance (β = −.21, p < .05), and drug use explained 4.0% unique variance (β = −.22, p < .05). Drug use and depression were thus overlapping risk factors for family adaptability. In a standard regression in which family adaptability was regressed simultaneously on depression and perceived support, depression and perceived support together explained 20.0% unique variance (p < .001), depression explained 1.0% unique variance (β = −.16, p = .14), and perceived support explained 12.0% unique variance (β = .40, p < .001). Depression therefore met criteria as a proxy for, or symptom of, the stronger risk factor, perceived support. In a standard regression in which family adaptability was regressed simultaneously on drug use and perceived support, drug use severity and perceived support together explained 22.0% variance (p < .001), drug use explained 3.0% unique variance (β = −.18, p < .05), and perceived support explained 13.0% unique variance (β = .40, p < .001). Although drug use severity contributed a small amount of unique variance, overall, the pattern of association was most characteristic of an association by proxy, with perceived support as the dominant factor.
Mediation Analyses
To test the hypotheses that early bonding experience is related to perceived support and that perceived support mediates relations between early bonding experience and mothers’ relationship with children, and guided by building block approach, we organized these factors in order of temporal precedence and tested the predicted mediation model. In standard regressions conducted to test the first three criteria of the mediation model (see Figure 1), early maternal care explained 20.0% unique variance in perceived support (β = .44, p < .001) and 11.0% unique variance in family adaptability (β = .33, p < .001). Perceived support explained 19.0% unique variance in family adaptability (β = .45, p < .001). In a multiple regression conducted to test the fourth criterion for mediation (see Figure 1), variance in family adaptability accounted for by early maternal care was decreased by 83.0% (R2 = .02; β = .16, p = .07) when perceived support was added to the mediation model. Thus, all four criteria for confirming the mediation model were met.
Figure 1.
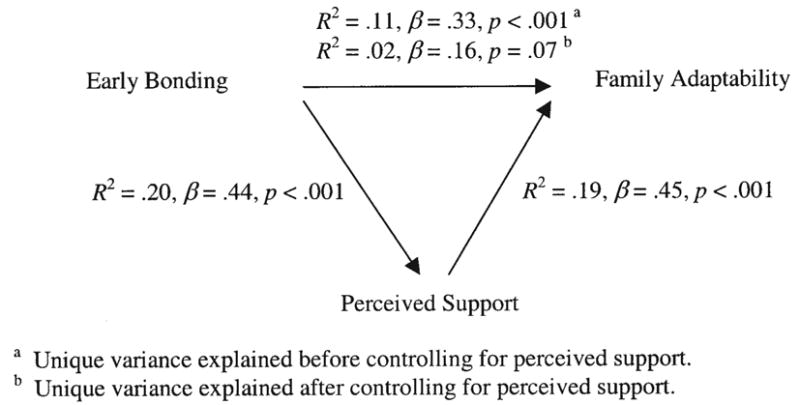
Results of the regression series testing perceived support as a mediator of associations between early maternal care and family adaptability.
Discussion
Although psychosocial factors at multiple levels of influence, including the early family environment, individual psychological adjustment, and the social environment, have been linked to the parenting practices of drug-dependent women, few researchers have examined how these factors might work together to influence parenting. In this study, we have used an attachment theory framework to examine how four psychosocial factors associated with parenting practices of drug-dependent mothers (i.e., bonding with early caregivers, depression, drug use severity, and perceived support) work together to influence care-giving problems reported by mothers enrolled in methadone maintenance. According to attachment theory, psychological maladjustment occurs when representations of the availability of care derived from early bonding experience reflect an absence of support and nurture. We therefore expected that previously reported associations between (a) depression and drug use and (b) parenting problems would be proxies for, or symptoms of, a stronger association between perceived absence of support and parenting problems. Attachment theory also emphasizes the central role of generalized internal working models of attachment as mediators between early caregiving experience and subsequent close relationships in adulthood. Much like internal working models of attachment, perceptions of social support reflect a general underlying schema of relationships. We therefore expected that associations between mothers’ early bonding experience and their perceptions of relationships with their children would be mediated by their perceptions of support and nurture available in their everyday life. Each of these hypotheses was supported for the first outcome, mothers’ perceptions of family adaptability. Few psychosocial factors were associated with the second outcome, mothers’ perceptions of family cohesion, and a majority of mothers (87.2%) in the sample reported no cohesion in their relationships with their children. Each of these findings is discussed, in turn, below.
Depression and Drug Use as Proxies for Absence of Social Support
Rather than having independent associations with mothers’ perceptions of family relationships, depression and drug use severity seem to be proxies for, or symptoms of, a stronger risk factor, mothers’ perceptions of the availability of support and nurture in their everyday life. This finding is consistent with reports in the attachment literature that psychopathology in adulthood develops in conjunction with prototypical internalized models of attachment (derived from early caregiving experiences) that are organized with respect to patterns of emotional dysfunction. These insecure organizations decrease the likelihood that individuals will form relationships that they experience as supportive (Sroufe et al., 1999). Many questions remain, though, as to how internalized models of attachment and emotional dysfunction interact (e.g., whether their associations are bidirectional or unidirectional, whether pathways vary depending on the nature of psychological distress). Above all, this finding highlights the importance of moving beyond simple identification of psychosocial correlates (e.g., drug abuse, psychopathology) of maladaptive parenting among drug-dependent women and applying more complex developmental frameworks to understanding underlying mechanisms linking psychosocial factors with maladaptive parenting. This finding also points to the central role that perceptions of relationships and the availability of care may have in the etiology of parenting problems for drug-dependent mothers. Mechanisms linking perceptions of relationships with psychological maladjustment require further examination to determine specific pathways of influence.
The Mediating Role of Perceived Support
Results of this study also indicate that the influence of mothers’ early bonding experience on their perceptions of adaptability in the caregiving relationship is largely mediated by mothers’ perceptions of support and nurture in their everyday life. Specifically, controlling for perceived support reduced associations between early bonding and mothers’ perceptions of family adaptability by 82.0%. Rather than having a direct influence on parenting problems, early bonding experience appears to influence how mothers come to view the availability of support and nurture in their everyday life, and this generalized model of relationships then directly influences mothers’ experience in the caregiving role. This is consistent with findings in the attachment (Slade & Cohen, 1996; Solomon & George, 1996; Sroufe et al., 1999) and social support literature (Crittenden, 1981, 1985; Crockenberg, 1988) that internalized models of attachment relationships derived from early attachment relationships with caregivers serve as prototypes for subsequent parenting relationships. Although mechanisms of transmission of relational models over time require further study, Crockenberg (1988) has suggested that the experience of social support and nurturance affirms a mother’s sense of herself as a person deserving of care and capable of caring for someone else and, in doing so, encourages the mother’s inclination to be nurturing and flexible toward her children. Crittenden (1981, 1985) has also proposed that internal models of social relationships may change over time in response to new social relationships. New directions in research examining drug-dependent mothers’ perceptions of relationship are essential for further examining mechanisms of transmission, including how models of social relationship and caregiving relationship interact to influence parenting behavior and child outcomes and how changes in models of relationship brought about by psychosocial intervention or new supportive relationships in adulthood might function as buffers that “protect” caregiving relationship from early bonding disruptions.
The Absence of Cohesion and the Presence of Adaptability
One of the most striking findings in this study is the high percentage of mothers (87.2%) who reported experiencing no cohesion or closeness with their own children and instead experienced their family as fragmented and disengaged. This finding is particularly notable in light of common tendencies among drug-dependent mothers to be somewhat guarded in reporting parenting difficulties for fear of losing child custody or learning the impact their drug use might have had on their children’s development (see Mayes, 1995). It also highlights the need for family and parenting interventions to foster stronger bonds within the family.
Although early bonding was associated with perceived support and perceived support was associated with mothers’ perceptions of family cohesion, we failed to find an association between early bonding and family cohesion and were therefore unable to test the mediation model. This finding is consistent with attachment theory in that problems in cohesion are most strongly predicted by mothers’ perceptions of the availability of social support. Nonetheless, it is puzzling that cohesion appears unrelated to early bonding experience with the mother. It may be that, in the case of cohesion, recent relationship experience with peers or partners bears more influence on the experience of family cohesion. Early bonding may only determine how a mother will (or will not) experience support in everyday life, but the latter may have a much more powerful influence on how the caregiving relationship will be experienced.
In contrast to cohesion scores, adaptability scores varied more widely. In fact, a large percentage of the mothers (50.0%) characterized their relationships with their children as very flexible. In light of the high levels of chaos and inconsistency that have been observed in the caregiving relationships of drug-dependent mothers, this finding may not be altogether positive but may instead reflect some abdication of parental authority, consistency, and monitoring, particularly on items reflecting changing rules, leadership, and household responsibilities.
Limitations and Future Research
As with any empirical study, this study has a number of limitations to be addressed in future studies, and findings here must be considered preliminary. First, although temporal relations among variables (e.g., early bonding, perceived support, and the caregiving relationship) were assigned on the basis of developmental theory and prior empirical findings, the cross-sectional nature of the data calls for caution in drawing conclusions about temporal precedence and causality. For instance, associations between current perceptions of support and the caregiving relationship may be bidirectional. That is, problems in the caregiving relationship may “spill over” into relationships with other adults. Only further longitudinal investigation will help to clarify direction of influence.
A second limitation of this study is our reliance on relatively simple measures of mothers’ perceptions of relationships and of early care that do not directly assess mothers’ internal models of attachment. Each of the measures has been widely used and has well-documented reliability and validity. Moreover, the central construct of interest in this study, perceived support, has been well documented in the psychology literature as representing a generalized and enduring cognitive schema for relationship, much like an internal working model of relationship (Anan & Barnett, 1999; Lakey & Cassady, 1990). Nonetheless, future studies involving the use of more in-depth measures of attachment relationships of drug-dependent mothers, including measures of attachment behaviors in early childhood, attachment representations in later childhood and adulthood, and internal models of caregiving relationships, are essential for understanding the internal working models of relationships and corresponding psychopathology in the etiology of maladaptive parenting.
A third limitation of this study is our sole reliance on self-report measures. Drug-dependent mothers’ concerns about losing custody of children and other impending legal problems, as well as their fears about the impact of maternal addiction on their children’s well-being, can unfortunately result in distortions of reports about their parenting (Mayes, 1995). This third limitation notwithstanding, self-reported data constitute the only route to developing a phenomenological understanding of women’s cognitive and emotional experiences as parents. In prior quantitative studies, drug-dependent mothers have typically been studied in terms of their attitudes about parenting, behaviors with children, drug use behaviors, and comorbid psychiatric symptoms, with little attention directed toward mothers’ perceptions and experiences in the caregiving role. Moreover, in this study, if the data were highly confounded by shared method variance, the likelihood of finding a global, diffuse set of equally strong associations among all constructs examined would have increased substantially. Instead, there were distinct patterns of association and mediation and specific links between particular bonding and support indices and family characteristics in directions that were hypothesized on the basis of conceptual and theoretical arguments. Nonetheless, there is a need to examine how mothers’ perceptions of caregiving relationships influence their parenting behavior and their children’s development. Parenting research with nondrug-dependent (e.g., Benoit, Parker, & Zeanah, 1997; Biringen, Matheny, Bretherton, Renouf, & Sherman, 2000; Crittenden, Lang, Claussen, & Partridge, 2000; Grienenberger, Slade, & Kelly, 2001; Slade, 1999; Slade, Grienenberger, Bernbach, Levy, & Locker, 2001; Soares, Fremmer-Bombik, Grossmann, & Silva, 2000; Zeanah & Benoit, 1997) and drug-dependent mothers alike (e.g., Goodman et al., 1999; Schuler, Black, & Starr, 1995) has already established that mothers’ perceptions of the caregiving relationship influence their parenting behaviors and their children’s development. Further study involving direct observations and evaluation of caregiving interactions and child outcomes would help clarify the mechanisms of influence underlying these associations.
For clinical practice, the present findings underscore the need for interventions that target not only drug-dependent women’s drug use and psychiatric symptoms but also, and possibly more important, their capacity to seek and sustain emotional support systems in their family and social networks. In his clinical discussions of treatment for drug dependence, Flores (2001) has noted the limited value of treating drug dependence without addressing the developmental task of becoming more “attached” to others. Drug dependence may bring an individual to treatment, but abstinence from drug use is only likely to occur in the context of the changing experience of self in an interpersonal context (Flores, 2001; Khantzian, Halliday, & McAuliffe, 1990). Consistent with Flores’s view, our results suggest that drug dependence may be a symptom of a broader relational disturbance originating with early childhood bonds that may be ameliorated through new social experiences. If interventions for drug-dependent mothers address only psychological symptoms and drug use, their feelings of isolation and stigmatization are likely to persist, influencing their parenting capacities in negative ways. Conversely, if interventions directly target mothers’ needs as adults for ongoing, trustworthy, predictable, and supportive interpersonal relationships, the adverse effects of more global psychosocial risk and early bonding disruptions on parenting may become attenuated. Consistent with this suggestion, clinical trials data indicate that therapeutic interventions that directly address mothers’ needs for consistent, interpersonal contact and support can effectively reduce child maltreatment risk and also foster adaptive parenting behaviors (see Heinicke et al., 1999; Luthar & Suchman, 1999, 2000).
In summary, this study provides preliminary evidence that perceptions of relationship may be important determinants of the caregiving relationship problems reported by drug-dependent mothers and that previously identified psychosocial correlates of parenting may also be a function of internal working models of relationships. Although prior studies have clearly shown that drug-dependent mothers are at risk for engaging in maladaptive parenting practices and that their infants are at risk for poor developmental outcomes, little work has yet been done to understand how internal representations of relationships might contribute to each of these risks.
Acknowledgments
We thank the clients and staff of the Women in Treatment Program and the administration of the Addiction Prevention and Treatment Foundation for their support of this project. We thank Linda Mayes and Bruce Rounsaville for their thoughtful comments on the manuscript. We are grateful to Kimberly Doyle, Margaret Christinat, Kimberly DiMeola, and Brian Fitzgerald for their assistance with the collection and management of these data.
Footnotes
A limited portion of this article was presented at the 63rd Annual Meeting of the College on Problems of Drug Dependence. Support for this study was provided by Center for Substance Abuse Treatment Grant 5 HR TI00313; National Institute on Drug Abuse Grants K23 DA14606, P50 DA09241, RO1-DA10726, RO1-DA11498, and RO1-DA14385; the William T. Grant Foundation; and the Spencer Foundation.
Contributor Information
Nancy E. Suchman, Yale University School of Medicine.
Thomas J. McMahon, Yale University School of Medicine.
Arietta Slade, City University of New York and Yale Child Study Center.
Suniya S. Luthar, Teachers College, Columbia University.
References
- American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 3. Washington, DC: Author; 1987. [Google Scholar]
- Anan RM, Barnett D. Perceived social support mediates between prior attachment and subsequent adjustment: A study of urban African American children. Developmental Psychology. 1999;35:1210–1222. doi: 10.1037//0012-1649.35.5.1210. [DOI] [PubMed] [Google Scholar]
- Asendorpf J, Wilpers S. Attachment security and available support: Closely linked relationship qualities. Journal of Social and Personal Relationships. 2000;17:115–138. [Google Scholar]
- Baron RM, Kenny DA. The moderator–mediator variable distinction in social psychological research: Conceptual, strategic, and statistical considerations. Journal of Personality and Social Psychology. 1986;51:1173–1182. doi: 10.1037//0022-3514.51.6.1173. [DOI] [PubMed] [Google Scholar]
- Bauman PS, Dougherty FE. Drug-addicted mothers’ parenting and their children’s development. International Journal of the Addictions. 1983;18:291–302. doi: 10.3109/10826088309039348. [DOI] [PubMed] [Google Scholar]
- Beck AT, Beck RW. Screening depressed patients in family practice: A rapid technique. Postgraduate Medicine. 1972;52:81–85. doi: 10.1080/00325481.1972.11713319. [DOI] [PubMed] [Google Scholar]
- Beckwith L, Howard J, Espinosa M, Tyler R. Psychopathology, mother–child interaction, and infant development: Substance-abusing mothers and their offspring. Development and Psychopathology. 1999;11:715–725. doi: 10.1017/s095457949900228x. [DOI] [PubMed] [Google Scholar]
- Bekir P, McLellan T, Childress AR, Gariti P. Role reversals in families of substance misusers: A transgenerational phenomenon. International Journal of the Addictions. 1993;28:613–630. doi: 10.3109/10826089309039652. [DOI] [PubMed] [Google Scholar]
- Benoit D, Parker KC, Zeanah CH. Mothers’ representations of their infants assessed prenatally: Stability and association with infants’ attachment classifications. Journal of Child Psychology & Psychiatry & Allied Disciplines. 1997;38:307–313. doi: 10.1111/j.1469-7610.1997.tb01515.x. [DOI] [PubMed] [Google Scholar]
- Bernardi E, Jones M, Tennant C. Quality of parenting in alcoholics and narcotic addicts. British Journal of Psychiatry. 1989;154:677–682. doi: 10.1192/bjp.154.5.677. [DOI] [PubMed] [Google Scholar]
- Biringen Z, Matheny A, Bretherton I, Renouf A, Sherman M. Maternal representation of the self as parent: Connections with maternal sensitivity and maternal structuring. Attachment and Human Development. 2000;2:218–232. doi: 10.1080/14616730050085572. [DOI] [PubMed] [Google Scholar]
- Bowlby J. Attachment and loss: Vol. 1. Attachment. 2. New York: Basic Books; 1982. [Google Scholar]
- Burns KA, Chethik L, Burns WJ, Clark R. The early relationship of drug abusing mothers and their infants: An assessment at eight to twelve months of age. Journal of Clinical Psychology. 1997;53:279–287. doi: 10.1002/(sici)1097-4679(199704)53:3<279::aid-jclp11>3.0.co;2-f. [DOI] [PubMed] [Google Scholar]
- Cacciola JS, Koppenhaver JM, McKay JR, Alterman AI. Test–retest reliability of the lifetime items on the Addiction Severity Index. Psychological Assessment. 1999;11:86–93. [Google Scholar]
- Chang G, Carroll KM, Behr HM, Kosten TR. Improving treatment outcome in pregnant opiate-dependent women. Journal of Substance Abuse Treatment. 1992;9:327–330. doi: 10.1016/0740-5472(92)90026-k. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cochran M, Niego S. Parenting and social networks. In: Bornstein M, editor. Handbook of parenting: Vol. 3. Applied and practical parenting. Mahwah, NJ: Erlbaum; 1995. pp. 393–418. [Google Scholar]
- Collins NL, Feeney BC. A safe haven: An attachment theory perspective on support seeking and caregiving in intimate relationships. Journal of Personality and Social Psychology. 2000;78:1053–1073. doi: 10.1037//0022-3514.78.6.1053. [DOI] [PubMed] [Google Scholar]
- Cosden M, Cortez-Ison E. Sexual abuse, parental bonding, social support, and program retention for women in substance abuse treatment. Journal of Substance Abuse Treatment. 1999;16:149–155. doi: 10.1016/s0740-5472(98)00043-9. [DOI] [PubMed] [Google Scholar]
- Crittenden P. Abusing, neglecting, problematic, and adequate dyads: Differentiating by patterns of interaction. Merrill-Palmer Quarterly. 1981;27:1–18. [Google Scholar]
- Crittenden P. Maltreated infants: Vulnerability and resistance. Journal of Child Psychology and Psychiatry. 1985;26:85–96. doi: 10.1111/j.1469-7610.1985.tb01630.x. [DOI] [PubMed] [Google Scholar]
- Crittenden PM, Lang C, Claussen AH, Partridge MF. Relations among mothers’ dispositional representations of parenting. In: Crittenden PM, Claussen AH, editors. The organization of attachment relationships: Maturation, culture, and context. New York: Cambridge University Press; 2000. pp. 214–233. [Google Scholar]
- Crockenberg S. Social support and parenting. In: Fitzgerald W, Lester B, Yogman M, editors. Research on support for parents and infants in the postnatal period. New York: Cambridge University Press; 1988. pp. 67–85. [Google Scholar]
- Dawe S, Harnett PH, Staiger P, Dadds MR. Parent training skills and methadone maintenance: Clinical opportunities and challenges. Drug and Alcohol Dependence. 2000;60:1–11. doi: 10.1016/s0376-8716(99)00144-1. [DOI] [PubMed] [Google Scholar]
- Duncan RD, Saunders BE, Kilpatrick DG, Hanson RF, Resnick HS. Childhood physical assault as a risk factor for PTSD, depression, and substance abuse: Findings from a national survey. American Journal of Orthopsychiatry. 1996;66:437–448. doi: 10.1037/h0080194. [DOI] [PubMed] [Google Scholar]
- Edman SO, Cole DA, Howard GS. Convergent and discriminant validity of Faces-III: Family adaptability and cohesion. Family Process. 1990;29:95–103. doi: 10.1111/j.1545-5300.1990.00095.x. [DOI] [PubMed] [Google Scholar]
- Eliason MJ, Skinstad AH. Drug/alcohol addictions and mothering. Alcoholism Treatment Quarterly. 1995;12:83–96. [Google Scholar]
- Flores PJ. Addiction as an attachment disorder: Implications for group therapy. International Journal of Group Psychotherapy. 2001;51:63–81. doi: 10.1521/ijgp.51.1.63.49730. [DOI] [PubMed] [Google Scholar]
- Foelker GA, Shewchuk RM, Niederehe G. Confirmatory factor analysis of the short form Beck Depression Inventory in elderly community samples. Journal of Clinical Psychology. 1987;43:111–118. doi: 10.1002/1097-4679(198701)43:1<111::aid-jclp2270430118>3.0.co;2-s. [DOI] [PubMed] [Google Scholar]
- Friedemann M, Musgrove JA. Perceptions of inner city substance abusers about their families. Archives of Psychiatric Nursing. 1994;8:115–123. doi: 10.1016/0883-9417(94)90042-6. [DOI] [PubMed] [Google Scholar]
- Goodman G, Hans SL, Cox SM. Attachment behavior and its antecedents in offspring born to methadone-maintained women. Journal of Clinical Child Psychology. 1999;28:58–69. doi: 10.1207/s15374424jccp2801_5. [DOI] [PubMed] [Google Scholar]
- Gould J. A psychometric investigation of the standard and short form Beck Depression Inventory. Psychological Reports. 1982;51:1167–1170. doi: 10.2466/pr0.1982.51.3f.1167. [DOI] [PubMed] [Google Scholar]
- Grice D, Brady K, Dustan L, Malcolm R, Kilpatrick D. Sexual and physical assault history and post-traumatic stress disorder in substance-dependent individuals. American Journal on Addictions. 1995;4:297–305. [Google Scholar]
- Grienenberger J, Slade A, Kelly K. Maternal reflective functioning and the caregiving relationship: The link between mental states and mother–infant affective communication; Paper presented at the meeting of the Society for Research in Child Development; Minneapolis, MN. 2001. Apr, [Google Scholar]
- Haller DL, Knisely JS, Dawson KS, Schnoll SH. Perinatal substance abusers: Psychological and social characteristics. Journal of Nervous and Mental Disease. 1993;181:509–513. doi: 10.1097/00005053-199308000-00006. [DOI] [PubMed] [Google Scholar]
- Hans LL, Bernstein VJ, Henson LG. The role of psychopathology in the parenting of drug-dependent women. Development and Psychopathology. 1999;11:957–977. doi: 10.1017/s0954579499002400. [DOI] [PubMed] [Google Scholar]
- Harmer ALM, Sanderson J, Mertin P. Influence of negative childhood experiences on psychological functioning, social support, and parenting for mothers recovering from addiction. Child Abuse and Neglect. 1999;23:421–433. doi: 10.1016/s0145-2134(99)00020-4. [DOI] [PubMed] [Google Scholar]
- Heinicke CM, Fineman NR, Ruth G, Recchia SL, Guthrie D, Rodning C. Relationship-based intervention with at-risk mothers: Outcome in the first year of life. Infant Mental Health Journal. 1999;20:349–374. [Google Scholar]
- Hoff-Ginsberg E, Tardif T. Socioeconomic status and parenting. In: Bornstein M, editor. Handbook of parenting: Vol. 2. Biology and ecology of parenting. Mahwah, NJ: Erlbaum; 1995. pp. 161–188. [Google Scholar]
- Hofkosh D, Pringle JL, Wald HP, Switala J, Hinderliter SA, Hamel SC. Early interactions between drug-involved mothers and infants: Within-group differences. Archives of Pediatrics and Adolescent Medicine. 1995;149:665–672. doi: 10.1001/archpedi.1995.02170190075014. [DOI] [PubMed] [Google Scholar]
- Jeremy RJ, Bernstein VJ. Dyads at risk: Methadone-maintained women and their four-month-old infants. Child Development. 1984;55:1141–1154. [PubMed] [Google Scholar]
- Kandall SR, Gaines J. Maternal substance use and subsequent sudden infant death syndrome (SIDS) in offspring. Neurotoxicology and Teratology. 1991;13:235–240. doi: 10.1016/0892-0362(91)90016-p. [DOI] [PubMed] [Google Scholar]
- Keller DS, Wilson A. Affectivity in cocaine and opiate abusers. Psychiatry. 1994;57:333–347. doi: 10.1080/00332747.1994.11024698. [DOI] [PubMed] [Google Scholar]
- Khantzian EJ. The self-medication hypothesis of substance use disorders: A reconsideration and recent applications. Harvard Review of Psychiatry. 1997 January–February;4:231–244. doi: 10.3109/10673229709030550. [DOI] [PubMed] [Google Scholar]
- Khantzian EJ, Halliday KS, McAuliffe WE. Addiction and the vulnerable self: Modified dynamic group therapy for substance abusers. New York: Guilford Press; 1990. [Google Scholar]
- Kraemer HC, Stice E, Kazdin A, Offord D, Kupfer D. How do risk factors work together? Mediators, moderators, and independent, overlapping, and proxy risk factors. American Journal of Psychiatry. 2001;158:848–856. doi: 10.1176/appi.ajp.158.6.848. [DOI] [PubMed] [Google Scholar]
- Krystal H. Self representation and the capacity for self care. In: Yalisove DL, editor. Essential papers on addiction. New York: New York University Press; 1997. pp. 87–108. [Google Scholar]
- Lakey B, Cassady PB. Cognitive processes in perceived social support. Journal of Personality and Social Psychology. 1990;59:337–343. [Google Scholar]
- Leahy JM. Validity and reliability of the Beck Depression Inventory–Short Form in a group of adult bereaved females. Journal of Clinical Psychology. 1992;48:64–68. doi: 10.1002/1097-4679(199201)48:1<64::aid-jclp2270480109>3.0.co;2-9. [DOI] [PubMed] [Google Scholar]
- Levy DW, Truman S, Mayes L. The impact of prenatal cocaine use on maternal reflective functioning; Paper presented at the meeting of the Society for Research in Child Development; Minneapolis, MN. 2001. Apr, [Google Scholar]
- Lovejoy MC, Graczyk PA, O’Hare E, Neuman G. Maternal depression and parenting behavior: A meta-analytic review. Clinical Psychology Review. 2000;20:561–592. doi: 10.1016/s0272-7358(98)00100-7. [DOI] [PubMed] [Google Scholar]
- Luthar SS, Cushing G, McMahon T. Interdisciplinary interface: Developmental principles brought to substance abuse research. In: Luthar SS, Burack JA, Cicchetti D, Weisz JR, editors. Developmental psychopathology: Perspectives on adjustment, risk, and disorder. New York: Cambridge University Press; 1997. pp. 437–456. [Google Scholar]
- Luthar SS, Cushing G, Merikangas K, Rounsaville BJ. Multiple jeopardy: Risk and protective factors among addicted mothers’ offspring. Development and Psychopathology. 1998;10:117–136. doi: 10.1017/s0954579498001333. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Luthar SS, Suchman NE. Developmentally informed parenting interventions: The Relational Psychotherapy Mothers’ Group. In: Cicchetti D, Toth SL, editors. Rochester Symposium on Developmental Psychopathology: Vol. 9. Developmental approaches to prevention and intervention. Rochester, NY: University of Rochester Press; 1999. pp. 271–309. [Google Scholar]
- Luthar SS, Suchman NE. The Relational Psychotherapy Mothers’ Group: A developmentally informed intervention for at-risk mothers. Development and Psychopathology. 2000;12:235–253. doi: 10.1017/s0954579400002078. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Luthar SS, Walsh K. Treatment needs of drug-addicted mothers: Integrated parenting psychotherapy interventions. Journal of Substance Abuse Treatment. 1995;12:341–348. doi: 10.1016/0740-5472(95)02010-1. [DOI] [PubMed] [Google Scholar]
- Mayes L. Substance abuse and parenting. In: Bornstein M, editor. Handbook of parenting: Vol. 4. Applied and practical parenting. Mahwah, NJ: Erlbaum; 1995. pp. 101–125. [Google Scholar]
- Mayes L, Bornstein M. The context of development for young children from cocaine-abusing families. In: Kato P, Mann T, editors. Handbook of diversity issues on health psychology. New York: Plenum Press; 1996. pp. 69–95. [Google Scholar]
- Mayes LC, Feldman R, Granger RH, Haynes OM, Bornstein M, Schottenfeld R. The effects of polydrug use with and without cocaine on mother–infant interaction at 3 and 6 months. Infant Behavior and Development. 1997;20:489–502. [Google Scholar]
- McDermott PA, Alterman AI, Brown L, Zaballero A, Snider EC, McKay JR. Construct refinement and confirmation for the Addiction Severity Index. Psychological Assessment. 1996;8:182–189. [Google Scholar]
- McGahan PL, Griffith JA, McLellan AT. Composite scores from the Addiction Severity Index: Manual and computer software. Philadelphia: Veterans Administration Press; 1986. [Google Scholar]
- McLellan AT, Kushner H, Metzger D, Peters R, Smith I, Grissom G, et al. The fifth edition of the Addiction Severity Index. Journal of Substance Abuse Treatment. 1992;9:199–213. doi: 10.1016/0740-5472(92)90062-s. [DOI] [PubMed] [Google Scholar]
- McMahon TJ, Luthar SS. Bridging the gap for children as their parents enter substance abuse treatment. In: Hampton RL, Senatore V, Gullotta TP, editors. Substance abuse, family violence, and child welfare: Bridging perspectives: Vol. 10. Issues in children’s and families’ lives. Thousand Oaks, CA: Sage; 1998. pp. 143–187. [Google Scholar]
- McMahon TJ, Luthar SS. Women in treatment: Within-gender differences in the clinical presentation of opioid-dependent women. Journal of Nervous and Mental Disease. 2000;188:679–687. doi: 10.1097/00005053-200010000-00006. [DOI] [PubMed] [Google Scholar]
- McMahon TJ, Winkel JD, Suchman NE, Luthar SS. Drug dependence, parenting responsibilities, and treatment history: Why doesn’t mom go for help? Drug and Alcohol Dependence. 2002;65:105–114. doi: 10.1016/s0376-8716(01)00153-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Murphy S, Irwin J. “Living with the dirty secret”: Problems of disclosure for methadone maintenance clients. Journal of Psychoactive Drugs. 1992;24:257–264. doi: 10.1080/02791072.1992.10471646. [DOI] [PubMed] [Google Scholar]
- Murphy S, Rosenbaum M. Pregnant women on drugs: Combating stereotypes and stigma. New Brunswick, NJ: Rutgers University Press; 1999. [Google Scholar]
- Ognibene TC, Collins NL. Adult attachment styles, perceived social support and coping strategies. Journal of Social and Personal Relationships. 1998;15:323–345. [Google Scholar]
- Olson DH, Portner J, Lavee Y. FACES III. Unpublished manuscript, University of Minnesota; Twin Cities Campus: 1985. [Google Scholar]
- Parker G. The parental bonding instrument: Psychometric properties reviewed. Psychiatric Developments. 1989;4:317–335. [PubMed] [Google Scholar]
- Parker G, Tupling H, Brown LB. A parental bonding instrument. British Journal of Medical Psychology. 1979;52:1–10. [Google Scholar]
- Polansky NA, Gaudin JM, Ammons PW, Davis KB. The psychological ecology of the neglectful mother. Child Abuse and Neglect. 1985;9:265–275. doi: 10.1016/0145-2134(85)90019-5. [DOI] [PubMed] [Google Scholar]
- Procidano ME. The nature of perceived social support: Findings of meta-analytic studies. In: Spielberger CD, Butcher JN, editors. Advances in personality assessment. Vol. 9. Hillsdale, NJ: Erlbaum; 1992. pp. 1–26. [Google Scholar]
- Procidano ME, Heller K. Measures of perceived social support from friends and from family: Three validation studies. American Journal of Community Psychology. 1983;11:1–24. doi: 10.1007/BF00898416. [DOI] [PubMed] [Google Scholar]
- Reynolds WM, Gould JW. A psychometric investigation of the standard and short form Beck Depression Inventory. Journal of Consulting and Clinical Psychology. 1981;49:306–307. doi: 10.1037//0022-006x.49.2.306. [DOI] [PubMed] [Google Scholar]
- Rice C, Longabaugh R. Measuring general social support in alcoholic patients: Short forms for perceived social support. Psychology of Addictive Behaviors. 1996;10:104–114. [Google Scholar]
- Rodning C, Beckwith L, Howard J. Quality of attachment and home environments in children prenatally exposed to PCP and cocaine. Development and Psychopathology. 1991;3:351–366. [Google Scholar]
- Sarason RS, Pierce GR, Bannerman A, Sarason IG. Investigating the antecedents of perceived social support: Parents’ views of and behavior toward their children. Journal of Personality and Social Psychology. 1993;65:1071–1085. [Google Scholar]
- Schuler ME, Black MM, Starr RH. Determinants of mother–infant interaction: Effects of prenatal drug exposure, social support, and infant temperament. Journal of Clinical Child Psychology. 1995;24:397–405. [Google Scholar]
- Schweitzer RD, Lawton PA. Drug abusers’ perceptions of their parents. British Journal of Addiction. 1989;84:309–314. doi: 10.1111/j.1360-0443.1989.tb03464.x. [DOI] [PubMed] [Google Scholar]
- Sheridan MJ. A proposed intergenerational model of substance abuse, family, functioning, and abuse/neglect. Child Abuse and Neglect. 1995;19:519–530. doi: 10.1016/0145-2134(95)00012-w. [DOI] [PubMed] [Google Scholar]
- Slade A. Representation, symbolization and affect regulation in concomitant treatment of a mother and child: Attachment theory and child psychotherapy. Psychoanalytic Inquiry. 1999;19:797–830. [Google Scholar]
- Slade A, Aber JL. Attachments, drives, and development: Conflicts and convergences in theory. In: Barron J, Eagle M, Wolitzky D, editors. Interface of psychoanalysis and psychology. Washington, DC: American Psychological Association; 1992. pp. 154–185. [Google Scholar]
- Slade A, Cohen LJ. The process of parenting and the remembrance of things past. Infant Mental Health Journal. 1996;17:217–222. [Google Scholar]
- Slade A, Grienenberger J, Bernbach E, Levy D, Locker A. Maternal reflective functioning and attachment: Considering the transmission gap; Paper presented at the meeting of the Society for Research in Child Development; Minneapolis, MN. 2001. Apr, [Google Scholar]
- Soares I, Fremmer-Bombik E, Grossmann KE, Silva M. Attachment representation in adolescence and adulthood: Exploring some intergenerational and intercultural issues. In: Crittenden PM, Claussen AH, editors. The organization of attachment relationships: Maturation, culture, and context. New York: Cambridge University Press; 2000. pp. 325–342. [Google Scholar]
- Solomon J, George C. Defining the caregiving system: Toward a theory of caregiving. Infant Mental Health Journal. 1996;17:183–197. [Google Scholar]
- Spain AJI, Spain DM. Opiate addicts and their perceived parental rearing. Acta Psychiatrica Scandanavia. 1988;78:121–126. [PubMed] [Google Scholar]
- Sroufe LA, Carlson EA, Levy AK, Egeland B. Implications of attachment theory for developmental psychopathology. Development and Psychopathology. 1999;11:1–13. doi: 10.1017/s0954579499001923. [DOI] [PubMed] [Google Scholar]
- Suchman NE, Luthar SS. Maternal addiction, child maladjustment, and sociodemographic risks: Implications for parenting behaviors. Addiction. 2000;95:1417–1428. doi: 10.1046/j.1360-0443.2000.959141711.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Suchman NE, Luthar SS. The mediating role of parenting stress in methadone-maintained mothers’ parenting. Parenting: Science and Practice. 2001;1:285–315. doi: 10.1207/s15327922par0104_2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Torresani S, Favaretto E, Zimmermann C. Parental representations in drug-dependent patients and their parents. Comprehensive Psychiatry. 2000;41:123–129. doi: 10.1016/s0010-440x(00)90145-7. [DOI] [PubMed] [Google Scholar]
- van IJzendoorn MH. Adult attachment representations, parental responsiveness, and infant attachment: A meta-analysis on the predictive validity of the adult attachment interview. Psychological Bulletin. 1995;117:387–403. doi: 10.1037/0033-2909.117.3.387. [DOI] [PubMed] [Google Scholar]
- Wade LN, Procidano ME. The effects of childrearing on mothers’ social support; Paper presented at the 94th Annual Convention of the American Psychological Association; Washington, DC. 1986. Aug, [Google Scholar]
- Wald R, Harvey SM, Hibbard J. A treatment model for women substance users. International Journal of the Addictions. 1995;30:881–888. doi: 10.3109/10826089509067013. [DOI] [PubMed] [Google Scholar]
- Widom CS, Weiler BL, Cottler LB. Childhood victimization and drug abuse: A comparison of prospective and retrospective findings. Journal of Consulting and Clinical Psychology. 1999;67:867–880. doi: 10.1037//0022-006x.67.6.867. [DOI] [PubMed] [Google Scholar]
- Wurmser L. Psychoanalytic considerations of the etiology of compulsive drug use. In: Yalisove DL, editor. Essential papers on addiction. New York: New York University Press; 1997. pp. 87–108. [Google Scholar]
- Zeanah CH, Benoit D. Clinical applications of a parent perception interview of infant mental health. Child and Adolescent Psychiatric Clinics of North America. 1997;4:539–554. [Google Scholar]


