Abstract
Ketamine, a synthetic drug commonly consumed by high risk youth, produces a range of experiences, including sedation, dissociation, and hallucinations. While ketamine is more typically sniffed, we describe a small sample of young ketamine injectors (n=25) in New York City and highlight risks associated with this emerging type of injection drug use. Our findings indicate that the injection practices, injection groups, and use norms surrounding ketamine often differ from other injection drug use: intramuscular injections were more common than intravenous injections; injection groups were often large; multiple injections within a single episode were common; bottles rather than cookers were shared; and the drug was often obtained for free. Our findings suggest that the drug injection practices exercised by ketamine injectors place them at risk for bloodborne pathogens, such as HIV, HBV, and HCV. We conclude that ketamine injectors represent an emerging, though often hidden, population of injection drug users, particularly among high risk, street-involved youth.
Introduction
Ketamine, also known as Special K, or K, is among the several illicit substances recently classified as “club drugs.” Ketamine and other so-called club drugs, such as MDMA and GHB, are synthetic substances that are consumed to alter a user’s experience within a recreational setting (Curran & Morgan, 2000; Reynolds, 1997). Among these drugs, ketamine is particularly noteworthy because it is commonly administered in multiple ways. Ketamine is sold illicitly in pill, powder, and liquid form, and it may be swallowed, drunk, smoked, sniffed, and injected (Jansen, 2001). In this article, we describe a small sample of young ketamine injectors living in New York City to highlight the current social and behavioral practices associated with ketamine injection – practices that may place ketamine injectors at risk for infectious diseases.
Ethnographic research that specifically examines injection drug using practices can lead to important discoveries about viral transmission and harm reduction strategies. While the sharing of syringes has been long identified as a primary means of transmitting HIV (Des Jarlais, Friedman, & Stoneburner, 1988), more recently, ancillary injection paraphernalia, such as “cookers,” water, heat sources, and filters, have been found to be additional sources of risk for bloodborne pathogens. For instance, based upon ethnographic interviews and observations of heroin injectors preparing both tar and powder heroin in cookers, Clatts et al. (1999) found that tar heroin required longer exposure to a heat source before dissolving in water. Subsequent laboratory studies modeling these findings revealed that heating heroin solutions in a cooker for 15 seconds of more reduced HIV-1 viability below detectable levels.
Similarly, this article uses qualitative interviews to understand infectious disease risk associated with ketamine injection by focusing on specific injection events among a sample of young drug injectors. As this study demonstrates, ketamine injectors utilize a different series of injection practices and different types of paraphernalia compared to other types of injection drug use, such as heroin. Consequently, ketamine injection practices may pose new or different kinds of injection risks.
Ketamine: A Brief History
Ketamine was developed in the United States in 1962 and later patented by Parke-Davis in 1966. Marketed under trade names such as Ketaset and Ketaject, ketamine was promoted as a fast-acting general anesthetic. Ketamine became the most widely used battlefield anesthetic during the Vietnam War (Siegel, 1978) and was approved by the Food and Drug Administration (FDA) for use among children and elderly in 1970. Gradually, ketamine became used less in medical settings after clinical administrations revealed certain complications in some patients, such as vivid dreaming, hallucinations, and confused states (Fine, Weissman, & Finestone, 1974; Perel & Davidson, 1976). Currently, ketamine is dispensed primarily by veterinarians as an animal sedative (Curran & Morgan, 2000). It is also administered to humans by physicians under certain medical circumstances, such as treating postoperative (Nikolajsen, Hansen, & Jensen, 1997) and chronic pain (Fine, 1997) and sedating pediatric patients (Green et al., 1999). In both veterinary and hospital settings, ketamine is administered via injection and is purchased from pharmaceutical companies where it is manufactured as a liquid.
While recreational ketamine use became increasingly popular in the United States and Europe in the last decade, the nonmedical use of ketamine extends back to the mid-1960s. Ketamine was dispensed by underground “medicinal chemists” from Michigan as early as 1967 (Jansen, 2001), while solutions of ketamine were sold on the streets in Los Angeles and San Francisco in 1971 (Siegel, 1978). By the late 1970s, the FDA released a report on ketamine abuse, and the National Institutes on Drug Abuse (NIDA) published a monograph on phencyclidine that included an article on ketamine intoxication (Jansen, 2001). Recreational ketamine use – sniffing in particular - became more widespread during the late 1980s and early 1990s in combination with new types of dance music played at house parties and raves (Dotson, Ackerman, & West, 1995). In 1997, New York State passed a law criminalizing the sale or possession of ketamine. Following reports of the sale, theft, and abuse of ketamine, the Drug Enforcement Administration (DEA) placed ketamine into schedule III of the Controlled Substance Act (CSA) in August 1999. Upon being listed as a Schedule III drug, it became illegal in the United States to possess ketamine for recreational or nonmedical purposes. In New York State, for instance, the possession of ketamine is a misdemeanor offense, which can carry penalties of six months in jail and a $1,000 fine.
There has been some confusion in classifying ketamine in relation to more common illicit drugs, such as MDMA and LSD, since ketamine can produce a range of experiences depending upon dosage. Ketamine can be a stimulant in low doses and can also cause potent psychedelic experiences in moderate and high doses. It has been described as a “dissociative anesthetic,” meaning the drug causes users to feel both sedated and separated from their bodies (Jansen, 2001), yet the drug is not a depressant. Rather, ketamine is a derivative of phencyclidine, or PCP, and both are chemical compounds known as arylcyclohexylamines. Like PCP, ketamine stimulates the vital functions of heartbeat and respiration, though ketamine is less toxic and shorter acting than PCP (Weil & Rosen, 1983).
While no epidemiological studies currently exist detailing the extent of the nonmedical use of ketamine or the modes of administering it, a 1999 report on drug use in 21 U.S. cities and metropolitan areas reported ketamine use in eight cities while intramuscular injections of ketamine were reported in three of those cities –Boston, New Orleans, and Minneapolis/St. Paul (CEWG, 1999). In an updated 2000 report, eight additional cities or metropolitan areas reported ketamine use, including two cities – New York and Seattle – that reported ketamine injection, though intramuscular versus intravenous injections were not specified (CEWG, 2000). Additionally, intravenous injections of ketamine have been reported among small samples of users (Jansen, 2001; Siegal, 1977) and single individuals (Lilly, 1978). Collectively, these recent report and older accounts suggest that ketamine use – injection in particular – is occurring in cities across the United States. In particular, as we report in this article, injecting ketamine is an emerging practice among youth that carries certain risks for viral transmission. However, these risks have not been described or examined in previous studies.
Methods and Sample
We first learned that youths were injecting ketamine in New York City while conducting ethnographic research on two other at-risk populations – young men who have sex with men (YMSM) and injection drug users who shoot crack cocaine. In the course of interviewing injection drug users from these two populations, and during conversations with outreach workers who served these populations, we learned that ketamine injection was occurring among street-involved youth. Upon realizing the potential risks associated with ketamine injection practices, we initiated an exploratory study focused on high risk youth who injected ketamine.
Our data was gathered by the lead author who recruited 25 ketamine injectors (n=25) from street and park settings in Manhattan’s East and West Villages. To qualify for an interview, a youth had to meet two criteria: aged between 18 and 25 years old and had ever injected ketamine. Upon meeting the criteria, each youth agreed to a 30-minute, semi-structured interview focusing on the details of their most recent ketamine injection, the effects of injecting ketamine, and their history of ketamine and other injection drug use. Hence, our sample constitutes an active drug using, out-of-treatment, youth population.
Table 1 presents the sample demographics of the 25 ketamine injectors recruited into the study. The youths were typically in their early 20s, white, and male. We use the term “street involvement” to describe a particular relationship between youths and informal economic generating activities, such as drug dealing, sex work, and panhandling, or structural housing circumstances, such as homelessness. However, these categories are not mutually exclusive. Nearly all of the youth interviewed were connected to the street economy in some manner, which ultimately had implications for their ketamine use.
Table 1.
Sample Demographics
| Age | Median | N |
|---|---|---|
| Range 18–25 | 21 | 25 |
| Race/Ethnicity | % | N |
| African-American/Black | 8 | 2 |
| Caucasian/White | 64 | 16 |
| Latino/Hispanic | 24 | 6 |
| Native American | 4 | 1 |
| Gender | % | N |
| Male | 92 | 23 |
| Female | 8 | 2 |
| Street Involvement | % | N |
| Homeless | 44 | 11 |
| Sex Work | 36 | 9 |
| Drug Dealing | 32 | 8 |
| Panhandling | 20 | 5 |
Findings
Polydrug Use
The majority of the youth in the sample were injection drug users, or had experimented with injection drug use, prior to injecting ketamine for the first time. The median age at injection initiation of any drug was 17 years old. Over half of the sample (56%) initiated injection drug use with a substance other than ketamine, such as heroin, cocaine, or methamphetamine. However, a relatively large proportion (44%) of the youth began their drug injection career with ketamine. The median age at ketamine injection initiation was 18 years old. Hence, youths were slightly older when they began injecting ketamine compared to other injection drugs.
As the sample’s history of injection drug use suggests, these ketamine injectors were polydrug users. Heroin, cocaine, crack, PCP, MDMA, LSD, methamphetamine, and marijuana were drugs commonly used by these young injectors in the months prior to being interviewed. In fact, 56% of the sample used one or more of these drugs before, during, or after their most recent injection of ketamine. However, equally significant is that 44% of the sample did not use any other drugs in addition to ketamine during their most recent injection. In other words, ketamine was the drug of choice for a number of users during a specific drug injection event.
In addition to injecting ketamine, 80% of the youth had sniffed ketamine during their drug-using careers. Youths reported several advantages of injecting ketamine over sniffing the drug: some found that sniffing aggravated their nasal passages and that injecting produced a “cleaner” high; others who developed a tolerance to ketamine from sniffing found that injecting was a more potent and reliable mode of administering the drug. It is noteworthy that 20% (or five youth) had never sniffed ketamine – a more common mode of administering the drug – and had only injected ketamine. In fact, these five youth had all initiated their injection drug use career with either heroin or cocaine prior to their first time injecting ketamine. Additionally, all five injected ketamine intravenously during their last ketamine injection event. This finding indicates that a user’s preferred mode of administering certain drugs, like heroin or cocaine, is often transferred to administering a new drug, such as ketamine.
K-Hole
Many injectors reported that a primary reason for injecting ketamine was to “fall into” or achieve a “k-hole.” A k-hole is a general term that injectors applied to the intense psychological and somatic state experienced while under the influence of ketamine. K-holes were more reliably achieved – and more intensely experienced – by injecting the drug. After injecting ketamine, users reported feeling a momentary rush of energy followed by physical immobilization and social detachment for the duration of the experience, which could last from 10 to 60 minutes, depending upon the dosage. A k-hole is characterized by a distorted sense of space, such as a small room appearing the size of a football field, and an indistinct awareness of time, such as a few minutes seeming like an hour. As a user’s body slowed and disengaged from everyday conceptions of time and space, his or her mind tuned into often pleasant – though sometimes bizarre – experiential realms, such as spiritual journeys, interactions with famous or fictitious persons, and hallucinatory visions. Once the drug was processed by the body, however, users reported that the k-hole ended rather abruptly but could be quickly reentered following another injection of ketamine.
Injection Risk Factors
Figure 1 displays several factors present during the youths’ last ketamine injection episode that placed them at risk for viral transmission. First, ketamine was almost always injected in a group setting among other injectors. Youths reported that these injection groups were as large as 10 people. Large injection groups pose risks (particularly when paraphernalia is shared) since greater numbers of injectors increase the odds that someone in the group is infected with HIV or hepatitis. Second, multiple injections of ketamine were typical, such as 8 to10 injections over a period of several hours. Multiple injections increase the likelihood that injection paraphernalia will be shared – particularly when the drug injected is one that produces feelings of disorientation. Third, over half of the injectors reported some form of paraphernalia sharing, such as syringes or bottles of ketamine, but most commonly a bottle of ketamine. Liquid ketamine is typically packaged in a sealed 10 cc bottle with a flat rubber lid that is designed to be pierced by a needle point. Youths reported that two or more injectors would pull shots of ketamine from the same common bottle over the course of administering multiple injections of ketamine. Fourth, a relatively large proportion (though less than half) of injectors obtained their syringe from an indirect source, such as a friend who received needles from a needle exchange, a person on the street selling syringes, or an unfamiliar member of the injection group. Injectors who obtain syringes from such indirect sources increase the possibility of obtaining a used or tainted syringe. Fifth, ketamine was frequently obtained for free – a fact suggesting that ketamine is a social or “party drug.” Youths who reported receiving ketamine for free indicated that the injection that followed was often spontaneous. During these unplanned drug injection events, youths reported forgoing certain precautions, such as bringing their own injection paraphernalia to the injection setting.
Figure 1.
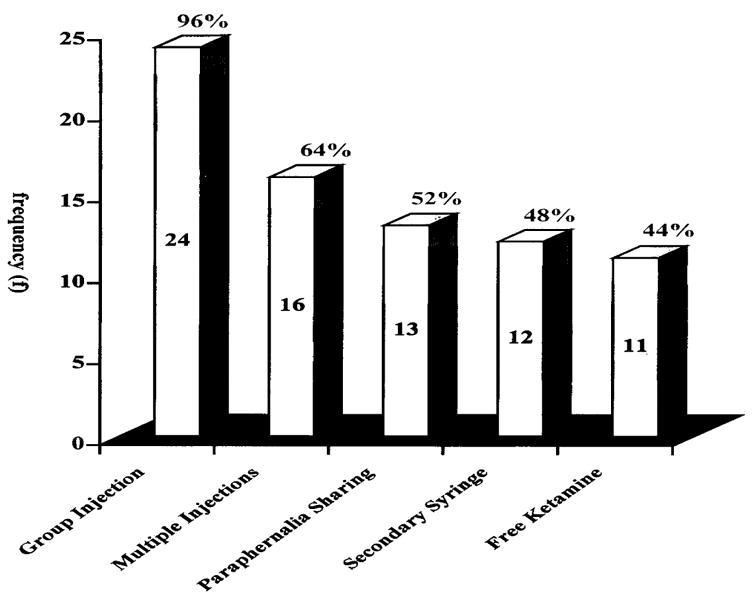
Risk Factors during Last Ketamine Injection Episode (N=25)
At the time of the youths’ most recent injection, the drug was injected both intramuscularly (68%) and intravenously (32%). As noted earlier, intravenous injectors typically had injected other drugs previous to ketamine, such as heroin or cocaine, and were accustomed to intravenous drug injections. The intramuscular ketamine injectors were either new injection drug users who did not want to inject the drug intravenously or were intravenous drug users who were initiated into ketamine injection by an injection group who administered the drug intramuscularly. Shooting ketamine intramuscularly produced a slower-acting, longer high, whereas administering ketamine intravenously led to a quicker, shorter high. Intravenous injections pose a greater risk for viral transmission than intramuscular injections since intramuscular injections typically do not pull blood into the needle or syringe.
Patterns of Ketamine Use
The frequency of injecting ketamine within the past year varied widely among the youth. For instance, 20% had injected ketamine only one time within the past year, while another 12% had injected ketamine 100 times or more (n = 4 cases or 16% were missing). Although, 10 was the median number of injections within the past year, or less than once per month. This variability in the number of ketamine injections within the past year reveals two primary facts about ketamine injection and ketamine use.
First, the dynamics surrounding injecting ketamine along with the pharmacological effects of the drug produced a range of experiences that some users found disturbing and impacted upon levels of use. Among youth who injected ketamine only one time in the past year were those who were reluctant to become regular users of drug injection paraphernalia, while others found the effects of ketamine unpleasant, which included vomiting. However, the great majority injected the drug multiple times in the past year – suggesting that most found the experience pleasurable and intriguing. Second, the number of ketamine injections in the past year was also impacted by the availability of the drug. Most reported that the supply of ketamine – particularly liquid ketamine – was variable so that a month or two might pass when the drug was very difficult to obtain. During these dry periods, youths reported injecting ketamine less frequently. In contrast, youths who had a steady supply of ketamine as a result of dealing the drug injected ketamine more frequently in the past year than those youth that did not deal the drug.
During the youths’ most recent injection, ketamine was obtained via three primary ways: received from friends for free, obtained as a result of dealing ketamine themselves, or bought from a drug dealer. Dealers obtained ketamine from two main sources: veterinarian offices, where it was stolen or diverted, or Mexico, where it was manufactured and packaged into 10 cc bottles, and could be purchased without a prescription. After obtaining bottles or cases of bottles, dealers sold bottles of liquid ketamine, known as a “lick,” or converted it into powder by heating the liquid until it became crystallized. In New York City, bottles of ketamine sold for between $60 and $80, while one bottle could be converted into powder valued at $200 or more.
The majority of youths (72%) reported that their most recent injection of ketamine occurred in New York City (80% when including suburban New Jersey). Other cities where the most recent injection occurred included Portland, Oregon; San Francisco; and rural locations in West Virginia and Montana during outdoor raves. However, this sample population is more mobile than these findings suggest. Including these five sites outside of New York City, youths reported injecting ketamine on other occasions in more than 35 cities and locations across the United State – large cities like Los Angeles and Seattle, but also smaller cities, such as Asheville, North Carolina and Grand Rapids, Michigan. These reports indicate that ketamine is injected across a much broader area than indicated by the current epidemiological data (CEWG, 1999; CEWG, 2000). Additionally, these findings point to the mobility of the youth population under study. Many youth traveled from city to city as a result of homelessness, while others traveled to visit friends or attend raves in other cities.
Ketamine: A Club Drug?
The convention of labeling ketamine as “club drug,” while capturing the fact that ketamine is commonly consumed in a social environment, does not accurately locate the settings where ketamine was most often injected among these youth. In fact, only 16% of the injections occurred at raves (more typically outdoor raves), and another 8% happened at indoor house parties. Instead, the most common setting was a street or park (36%), and another 8% injected ketamine inside a public bathroom. The remaining 32% injected inside an apartment or house among groups of injectors numbering between two and six persons. Additionally, after injecting ketamine in these typical settings, none of the youths reported attending a club or rave. (It should be noted that all of the youths had attended raves or clubs on other occasions.) Rather, the youths reported that injecting ketamine often created an experience in its own right that did not require a specialized setting, such as a rave. Interestingly, relatively mundane activities typically followed the injection or injections of ketamine, such as listening to music, watching television, walking the streets, talking about the high, consuming other drugs, or sleeping. Hence, these findings suggest that ketamine is injected recreationally in a variety of settings and is typically injected and experienced apart from the club or rave environs.
Discussion
Our findings indicate that ketamine injectors are an important population of young injection drug users worthy of further study. For as we report, the injection practices, injection groups, and use norms surrounding ketamine differ from heroin, cocaine, crack, and methamphetamine injection drug use: intramuscular injections were more common than intravenous injections; injection groups were often large; multiple injections within a single episode were common; bottles rather than cookers were shared; and the drug was often obtained for free. These findings suggest that the drug injection practices among ketamine injectors place themselves at risk for bloodborne pathogens, such as HIV, HBV, and HCV.
Additional research is necessary to follow young ketamine injectors longitudinally to learn whether, and under what circumstances, they transition to injecting other drugs. The majority of the youths in this sample had injected other drugs prior to ketamine injection initiation, but a large proportion began their injection drug use career with ketamine. The availability and supply of ketamine, which varies over the course of a year, may be an important factor in explaining the transition from ketamine injection to other injection drug use. Additionally, the type of ketamine available to users, such as powder versus liquid, may affect the transition from sniffing to injecting ketamine.
More research is needed to examine how the injection practices and injection groups among young ketamine injectors compare in different cities and locations. For as we indicated, New York City is only one of many cities where youth reported injecting ketamine. We anticipate variability in risk practices across settings since ketamine injection is a relatively new phenomenon and information about how to inject ketamine is diffuse among users.
We also indicated that involvement in the street economy – homelessness, drug dealing, and sex work – was common among this sample of young ketamine injectors. Future studies need to examine how the contingencies surrounding marginalized street existences, such as relationships with sex work partners and within drug dealing networks, affect trajectories into ketamine injection. Additionally, focusing on street-involved youth populations, such as ketamine injectors, is likely to yield information on emerging drug trends since youth are frequently enmeshed in varied drug-using and drug-selling networks.
We reported that a large proportion of users did not combine ketamine with other drugs. Rather, they injected only ketamine during their most recent ketamine injection event. This finding should temper certain assumptions about club drug use – that drugs, such as ketamine, are always or frequently used in combination with other drugs, such as MDMA and GHB, to create a synergistic drug experience. In particular, ketamine injection should not be viewed as synonymous with other club drug use, nor viewed as presenting the same health risks as other club drugs.
Likewise, calling ketamine a “club drug” may be a misnomer. The youths in this study largely reported injecting ketamine in settings other than clubs or raves. Whether due to the disorienting effects of injecting ketamine, the stigma often attached to injection drug use, or the pressure from law enforcement to police and sometimes close clubs, ketamine is most often injected in private dwellings. In other words, ketamine use – at least ketamine injection – has moved outside of the club environs and has become a recreational practice similar to (though not nearly as wide spread) smoking marijuana or ingesting LSD.
One limitation to this data, in addition to the small sample size, is the relatively homogenous demographic profile of the ketamine injectors interviewed: young, male, and white. While this profile may reflect the larger population of ketamine injectors, future research should continue to target street-involved youth but with a greater emphasis on obtaining a sample that includes more women and more members of racial and sexual minorities. Collecting a more diverse sample could reveal different injection practices and injection groups that may have further implications for infectious disease risk.
Lastly, ketamine injectors represent an emerging, though often hidden, population of injection drug users. As these findings indicate, ketamine injectors frequently obtained syringes from sources other than needle exchanges. This lack of direct contact with needle exchanges, while problematic in that ketamine injectors are not using a verifiable distributor of clean syringes, means that ketamine injection practices and related problems are less likely to be reported in syringe exchange data. Similarly, ketamine injectors, particularly those who only inject ketamine, are likely to be missed by studies focusing on heroin, cocaine, or methamphetamine injection. Hence, more studies focusing on ketamine injection are needed to gain additional understanding into the risks and experiences connected to injecting ketamine.
Acknowledgments
This research was conducted under the auspices of a grant from the National Institute on Drug Abuse (DA13893).
Contributor Information
Stephen E. Lankenau, Ph.D., is an assistant professor in the Department of Sociomedical Sciences at Columbia University’s Mailman School of Public Health. He conducts research on hidden populations, high-risk youth, and out-of-treatment drug users
Michael C. Clatts, Ph.D., is the Director of the Institute for Research on Youth at Risk (YAR) at National Development and Research Institutes, Inc. (NDRI). His principal area of interest is in community epidemiology and the development of community-based public health programs. He was one of the first social scientists involved in HIV research and, over the last 20 years, has lead a number of major epidemiological studies related to HIV prevention and care of those who are infected
References
- Clatts MC, Heimer R, Abdala N, Goldsamt L, Sotheran JL, Anderson KT, Gallo TM, Hoffer LD, Luciano PA, Kyriakides T. HIV-1 transmission in injection paraphernalia: Heating drug solutions may inactive HIV-1. JAIDS. 1999;22:194–199. doi: 10.1097/00126334-199910010-00013. [DOI] [PubMed] [Google Scholar]
- Community Epidemiological Working Group (CEWG) Proceedings of the Community Epidemiological Work Group. Vol. 1. Bethesda, MD: National Institutes of Health, Division of Epidemiology and Prevention Research, National Institute of Drug Abuse; 1999. Epidemiological trends in drug abuse. [Google Scholar]
- Community Epidemiological Working Group (CEWG) Proceedings of the Community Epidemiological Work Group. Vol. 1. Bethesda, MD: National Institutes of Health, Division of Epidemiology and Prevention Research, National Institute of Drug Abuse; 2000. Epidemiological trends in drug abuse. [Google Scholar]
- Curran V, Morgan C. Cognitive, dissociative and psychotogenic effects of ketamine in recreational users on the night of drug use and 3 days later. Addiction. 2000;95:575–590. doi: 10.1046/j.1360-0443.2000.9545759.x. [DOI] [PubMed] [Google Scholar]
- Des Jarlais DC, Friedman SR, Stoneburner R. HIV infection and intravenous drug use: Critical issues in transmission dynamics, infection outcomes, and prevention. Review of Infectious Disease. 1988;10:151–158. doi: 10.1093/clinids/10.1.151. [DOI] [PubMed] [Google Scholar]
- Dotson JW, Ackerman DL, West LJ. Ketamine abuse. Journal of Drug Issues. 1995;25:751–757. [Google Scholar]
- Fine J, Weissman J, Finestone EC. Side effects after ketamine anesthesia: transient blindness. Anesthesia and Analgesia. 1974;53:72–74. [PubMed] [Google Scholar]
- Fine PG. Low-dose ketamine in the management of opioid nonresponsive terminal cancer pain. Journal of Pain Symptom Management. 1999;17:296–300. doi: 10.1016/s0885-3924(98)00144-4. [DOI] [PubMed] [Google Scholar]
- Green SM, Hummel CB, Wittlake WA, Rothrock SG, Hopkins GA, Garrett W. What is the optimal dose of intramuscular Ketamine for pediatric sedation? Academy of Emergency Medicine, January. 1999;6:21–26. doi: 10.1111/j.1553-2712.1999.tb00089.x. [DOI] [PubMed] [Google Scholar]
- Jansen K. Ketamine: Dreams and realities. Sarasota, FL: Multidisciplinary Association for Psychedelic Studies; 2001. [Google Scholar]
- Lilly J. The scientist: A novel autobiography. Philadelphia: Lippincott; 1978. [Google Scholar]
- Nikolajsen L, Hansen PO, Jensen TS. Oral ketamine therapy in the treatment of postamputation stump pain. Acta Anaesthesiol Scandinavia. 1997;41:427–429. doi: 10.1111/j.1399-6576.1997.tb04710.x. [DOI] [PubMed] [Google Scholar]
- Perel A, Davidson JT. Recurrent hallucinations following ketamine. Anaesthesia. 1976;31:1081–1083. doi: 10.1111/j.1365-2044.1976.tb11948.x. [DOI] [PubMed] [Google Scholar]
- Reynolds S. Rave culture: Living dream or living death? In: Redhead S, editor. The clubcultures reader. Malden, MA: Blackwell Publishers; 1997. pp. 84–93. [Google Scholar]
- Siegel RK. Phenylcyclidine and ketamine intoxication: A study of four populations of recreational users. In: Peterson RC, Stillman RC, editors. Phencyclidine abuse: An appraisal. Rockville, MD: National Institutes on Drug Abuse (NIDA); 1978. pp. 119–147. NIDA research monograph 21. [Google Scholar]
- Weil A, Rosen W. Chocolate to morphine: Understanding mind-active drugs. Boston: Houghton Mifflin Company; 1983. [Google Scholar]


