Abstract
Objectives: This study assessed the information-seeking practices and needs of speech-language pathologists (SLPs). Improved understanding of these needs can inform librarians and educators to better prepare students in principles and methods of evidence-based practice (EBP) and, through continuing education (CE), promote the integration of EBP into clinical practice of SLPs.
Methods: A 16-question survey was mailed to 1,000 certified speech-language pathologists in the United States.
Results: Two hundred and eight usable surveys were returned for a response rate of 21%. For clinical questions, SLPs most often consulted with a colleague, participated in CE activities, and searched the open Internet. Few respondents relied on scholarly journal articles for assistance with clinical cases. The most prominent barriers to finding appropriate information were time and knowledge of where and how to find relevant information. Few reported having information literacy instruction by a librarian.
Discussion: If EBP is to become a viable practice in clinical decision making, there appears to be a tremendous need for information literacy instruction in the university curriculum, as well as through CE activities for currently practicing SLPs. Given respondents' reported lack of time and limited access to full-text journals containing evidence relevant to clinical practice, the field of speech-language pathology will need to generate readily accessible clinical summaries of research evidence through meta-analyses, systematic reviews, and clinical practice guidelines.
Highlights
Speech-language pathologists tend to consult colleagues rather than the peer-reviewed literature for assistance with a clinical query.
Lack of time, information literacy skills, and access were the most prominent barriers to evidence-based practice perceived by speech-language pathologists in this survey.
Speech-language pathologists and librarians should be aware that evidence in speech-language pathology can be found in a wide range of journals.
Implications
Librarians need to work with speech-language pathology educational programs to integrate a higher level of information literacy instruction into the curriculum.
Librarians can provide continuing education activities that emphasize information literacy for practicing clinicians.
INTRODUCTION
Speech-language pathologists (SLPs) assess and treat a broad array of communication impairments, such as adult and child language impairment, articulation, fluency, and voice disorders, as well as disordered swallowing function (dysphagia). Only very recently has evidence based practice (EBP) begun to take root in the field of speech-language pathology in the United States. New standards for receiving and maintaining the nationally recognized certificate of clinical competency (CCC), required of all practicing SLPs, became the impetus for EBP's implementation in 2005 [1]. In particular, CCC standard III-F requires the applicant to be knowledgeable about the research process and able to integrate research principles into clinical EBP. The SLP credentialing body, the American Speech-Language-Hearing Association (ASHA), which has over 120,000 members, envisions EBP as an “approach in which current, high-quality research evidence is integrated with practitioner expertise and client preferences and values into the process of making clinical decisions” [2]. As in other allied health fields, the field of speech-language pathology has long been accustomed to incorporating practitioner expertise and client values into decisions. The current challenges are for the profession to define what will constitute the best research evidence given the relative paucity of research evidence currently available and to determine how best to educate students and practicing clinicians to find and evaluate the existing research and then to integrate it into clinical practice.
In the medical and nursing disciplines, it has been recognized that the implementation of EBP may face barriers that go beyond the availability of relevant research evidence. Barriers may include lack of access to information, lack of proficiency in seeking information, and perceived value and relevance of information that is located, as well as convenience of the process when contrasted with other options such as peer consultation [3–8]. Similarly, in education surveys, it has become apparent that students often do not understand how to obtain information or weigh its sources and likely value [9, 10]. Despite the rapid extension of EBP to a number of disciplines, it is unclear how the current education and information-seeking needs of distinct groups of health professionals will enable its successful implementation.
Determining what constitutes appropriate information for making informed clinical decisions has been problematic throughout the health care arena. For example, physicians [3–5, 8, 11], nurses [6, 7, 12], physical therapists [13], rehabilitation therapists [14], and occupational therapists [15] have all been reported to place a higher value on consulting colleagues for information about clinical decision making than on scholarly sources of information. In a survey of practicing occupational therapists after the discipline adopted EBP guidelines, one study found that 79% of respondents indicated that they consulted colleagues or supervisors when seeking clinical guidance [15]. When practitioners consulted other sources, they were most likely to search the open Internet, an emerging but currently variable source of reliable information, as studies of individual health concerns indicate [16–19].
Similarly, it has been found that most rehabilitation therapists accepted their colleagues' information at “face value” [14]. Colleagues' availability or their past relationship with the clinician (e.g., classmates), rather than perceived expertise, were ranked as major factors in selecting a professional with whom to discuss case management. Taken together, virtually all surveys have found that colleagues were the primary source of information for practicing clinicians, followed by textbooks, continuing education workshops, and the open Internet. None of these is a substitute for locating peer-reviewed evidence in the published literature.
There is currently no reason to believe that SLPs behave in a significantly different manner than other health care professionals. A recent survey of SLPs in Australia found that half of the respondents use information from the open Internet and even fewer refer to professional journals for patient-related information. While three-quarters of the respondents reported using published clinical guidelines, the authors note that few guidelines actually exist and those that do are based on a broad mix of research and the knowledge and experience of practitioners [20].
Given that EBP has just started to gain momentum with SLPs in the United States—somewhat later than its professional mandate in Australia, Canada, and the United Kingdom—the researchers' aim is to explore the information-seeking needs and tendencies of practicing SLPs in the United States. Such information is critical to the appropriate design of curricula and tutorials that can improve practical implementation of EBP for SLP students prior to graduation from their professional training programs and then be applied toward continuing education (CE) efforts for practicing clinicians.
The following research questions were posed:
What are the primary and additional sources of evidence used by practicing SLPs to answer clinical questions?
What do SLPs perceive to be barriers to obtaining reliable information for case management?
METHODS
A survey was adapted for practicing SLPs based on the questions used to investigate the information-seeking behaviors of practicing occupational therapists, a related professional organization [15]. A pilot study was conducted to determine clarity of survey questions. Ten recent graduates from the master's program in the Department of Hearing and Speech Sciences at the University of Maryland, College Park, were emailed the survey and asked to review it and provide comments. No substantive changes were suggested by the participants. The final survey, which included sixteen questions, may be found in the online-only appendix. The survey and study protocol were approved by the University of Maryland Institutional Research Board.
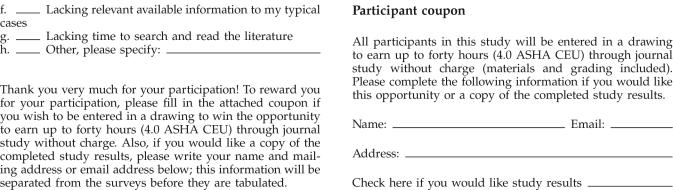
In February of 2005, a total of 1,000 randomly generated mailing labels for certified SLPs throughout the United States were purchased from ASHA, the national credentialing body for SLPs. The organization currently supplies mailing lists in print format only; thus, the survey was conducted via mail rather than email. Individuals whose affiliations were listed as colleges, universities, research facilities, or foundations were excluded from the list. The researchers intended to survey typical practitioners, rather than professors or research scientists. Surveys were mailed along with a cover letter and postage-paid return envelope. To increase incentive for completing the survey, a participant coupon was included at the end of the survey to enter participants ino a drawing to earn up to forty hours (ASHA CE units) through journal study sponsored by the university. Coupons were separated from completed surveys immediately upon receipt to preserve anonymity of responses.
RESULTS
Respondent demographics
Funding for the project permitted only a single mailing. Of 1,000 surveys mailed, 208 usable surveys were returned, providing a response rate of 21%. While somewhat low, this response rate closely mirrored other published studies of the ASHA membership, even those that used follow-up contact with survey recipients [21–24]. Response rates in these studies ranged from 20% to 27%.
The mean year in which respondents received their master's degree was 1992 (range 1959–2003), with a skew toward recent graduates. Therefore, the typical respondent was assumed to be in practice for about 13 years. Respondents reported working in a broad variety of settings. Some respondents indicated more than one primary location, which SLPs often do. Settings included public/private schools (K–12) (40%, 100/247), hospitals (14%, 35/247), private practice (13%, 33/247), nursing homes (6%, 15/247), rehabilitation centers (4%, 11/247), and other (23%, 60/247). Other responses included home health, early intervention program, independent subcontractor or consultant, or currently on leave. Of these, the most common were home health workers and early intervention program workers. As noted earlier, university and college-based ASHA members were excluded from the mailing.
Participant responses
When asked about the professional purposes for which they most often needed to find information, respondents provided a total of 659 potential purposes. The most frequently reported was needing to consult for information about patient or client care (30%, 200/ 659), followed by needing to answer a question posed by a patient, client, or family member (22%, 144/659); needing to answer a question posed by a colleague (18%, 120/659); and needing information to prepare for an in-service presentation (17%, 111/659). Less frequent purposes mentioned by respondents included needing information for a presentation at a professional meeting (8%, 55/659), writing a journal article or similar contribution (3%, 18/659), and “other” (2%, 11/659). Responses in this last category varied and included reasons such as presentations to parents or community groups, grant preparation, and study for certification examinations.
In reporting where they turn to when having a professional information need, respondents were able to choose up to three sources and rank them from most important (1) to less important (3). Numbers for the sources were then summed to provide a general profile of respondent tendencies. Personal contacts (e.g., colleagues, supervisors, ex-classmates) were most often consulted (164 responses), followed by the Internet (157 responses); continuing education workshops, seminars, or courses (154 responses); personal library (113 responses); community libraries (i.e., college, university, medical, hospital, public, or public school) (24 responses); and “other” (6 responses). “Other” included contacting national or state association offices or book vendors, such as Amazon.com. In virtually all cases, the value placed on the source reflected its overall ranking; in other words, not only were personal contacts mentioned most frequently, they were rated as most important. For example, 46% of those selecting personal contacts as a source ranked it as most important, the highest proportion so ranked. The same was true for the Internet (selected as most important by 37%, the second highest importance ranking). For continuing education and personal libraries, rankings were evenly split across the continuum from most important to least important.
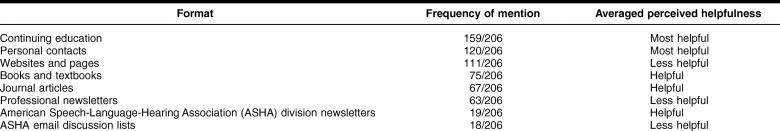
To determine what information formats were most helpful in satisfying professional education needs, respondents were again asked to choose up to three formats and rank them in order of importance, but this time as most helpful (1), helpful (2), or less helpful (3). Again, the number of times a format was chosen was summed to reflect overall tendencies (Table 1).
Table 1 Frequency of use and helpfulness of information formats
Continuing education experiences were mentioned most frequently and deemed the most helpful, with personal contacts ranked second as most helpful, followed by Websites or pages, which were frequently mentioned but considered less helpful. Again, as in the prior question, rankings were averaged across respondents. Books and textbooks, journal articles, and professional newsletters (e.g., ASHA Leader, Advance for SLPs) were considered moderately helpful. The least utilized and helpful formats were reported to be ASHA specialty interest division newsletters and mailing lists run by ASHA divisions or other groups.
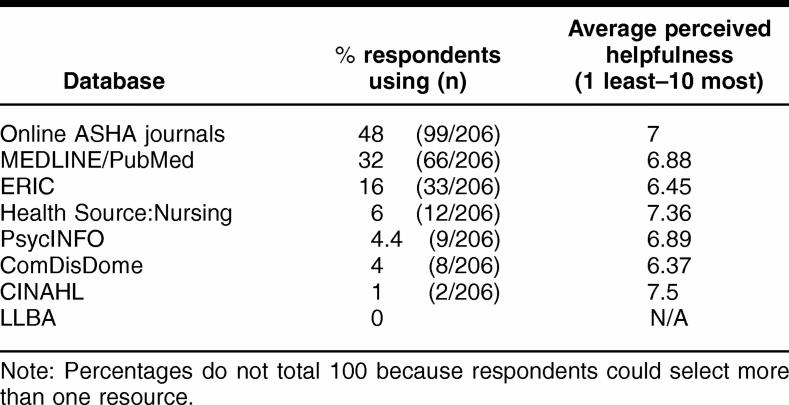
Respondents were also asked about their database use since graduation (Table 2). Fewer than one-third of the respondents (66/206) indicated that they had ever had occasion to search MEDLINE (either through PubMed or vendor). Those respondents who had searched MEDLINE since graduation considered the information they found only moderately helpful on a scale of 1 (not at all helpful) to 10 (extremely helpful). When queried about use of other resources, the most frequently mentioned sources were ASHA-published journals (e.g., Journal of Speech-Language and Hearing Research; American Journal of Speech-Language Pathology; Language, Speech and Hearing Services in Schools), all with current and past issues now available to members online at the ASHA Website. As noted in Table 2, the next most frequently mentioned database was ERIC, which had been used by relatively few respondents. All remaining sources had 6% or fewer responses and included Health Source: Nursing/Academic, PsycINFO, ComDisDome (a vendor that tailors sources of interest to speech-language pathologists), and CINAHL. Other sources were infrequently listed (3%). No respondent reported use of Linguistics and Language Behavior Abstracts (LLBA). Average helpfulness ratings were fairly uniform across all of these databases, ranging from a high of 7.5 for CINAHL (but rarely used) to 6.37 for ComDisDome.
Table 2 Database use by practicing speech-language pathologists
Respondents were asked to describe a recent patient care issue for which they had sought and found information. Based on the patient care issue described, the majority perceived themselves as very successful (55%, 106/191) when asked how successful they felt in analyzing, interpreting, and applying the information that they found. Fewer respondents felt “only OK” about their success (41%, 78/191). Very few (4%, 7/191) reported themselves as not very successful in being able to analyze and apply their findings. The researchers noted, however, that the evidence base for information that was located was likely to have been less than optimal, given responses to earlier questions.
Respondents' use of Websites was of interest. The majority of respondents noted consulting a Website to gain information about a clinical case (67%, 138/206). A wide array of Websites was mentioned, with only the ASHA Website mentioned by a substantive number of respondents. A high number of respondents reported not visiting any Websites routinely as part of their professional work (59%, 121/206). However, many (41%, 85/206) reported routine visits to specific Websites. Most of these sites were not sponsored by professional organizations or government clearinghouses but represented consumer group sites or private sites sponsored by practicing clinicians as resources for other clinicians (e.g., National Stuttering Association, Speechpathology.com, Advance for Speech Language Pathologists, Apraxiakids.org, etc.).
SLPs were asked what aspects of their graduate or professional education they felt helped them most in successfully seeking professional information. Respondents were able to choose up to three options. Requirements for prior class projects and papers (69%, 143/ 206) were reported to be of most help, with formal contacts with faculty (65%, 133/206) and networking with fellow students (65%, 133/206) each receiving an equal number of responses. Information contacts with faculty during office hours or in social contexts (43%, 88/206) were also reported as helpful. SLPs reported formal library instruction sessions (9%, 18/206) and informal contacts with librarians (5%, 10/206) much less frequently. From these data, it would appear that formal information literacy instruction was not a prominent focus of respondents' clinical education programs.
When asked specifically whether they felt that their graduate curriculum had adequately prepared them to handle lifelong learning needs, most SLPs responded affirmatively (60%, 122/203), followed by no (35%, 71/ 203) and somewhat (5%, 10/203). However, when asked to describe their level of preparation, most respondents' emphasized whether or not a particular disorder or technique had been covered in their graduate training, rather than information literacy skills, per se.
As the recent changes to the ASHA standards now require SLPs to implement EBP, the researchers sought to ascertain whether respondents understood the primary concepts underlying EBP. Thus, the survey queried SLPs as to what EBP meant and offered three, nonexclusive multiple-choice response options. The majority of SLPs thought that EBP required basing diagnostic and therapy practices on the research literature in a topic area (66%, 129/197), which was a reasonably correct definition. Many also thought that EBP required keeping complete records of all diagnostic and therapeutic procedures that one employed with a client (27%, 52/197). Fewer respondents thought that EBP required one to document the source of the information used in making clinical decisions in a client's file (7%, 14/197).
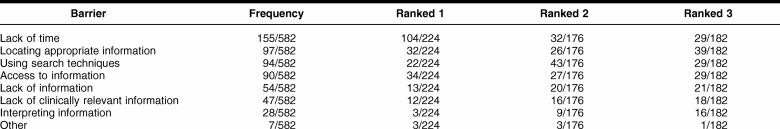
Survey participants were also asked to rank a list of potential barriers to obtaining good quality information to assist in making clinical decisions. Respondents were free to list additional barriers. Including barriers listed on the survey and those added by respondents, 582 obstacles were identified (Table 3). By far, the most commonly mentioned and highly ranked barrier was lack of time to search and read the literature (155/582). A total of 224 barriers received primary rankings, and time-related barriers constituted 69% (104/224) of these responses. The least problematic obstacle reported was interpretation of information that was retrieved.
Table 3 Barriers to obtaining quality information and importance ranking
DISCUSSION
Respondents in this study did not report a high level of information seeking that involved library or database resources. When practicing SLPs were confronted with a clinical question, the most popular behavior was “ask a colleague,” a response aligned with surveys of other clinicians including practicing physicians [3, 4, 8, 11] and other allied health professionals [12–15]. As in these other studies, this tendency to use colleagues as primary sources of clinical information was mentioned frequently, followed in popularity by CE activities and the open Internet. Very few respondents relied on professional journals in making clinical decisions or in answering professional information needs, a finding similar to that reported for Australian SLPs [20], the only other SLP population for which published information literacy information was available.
Consistent with their utilization patterns, surveyed practicing SLPs also found CE activities, personal contacts, and the open Internet most useful in providing them with clinical information. ASHA-certified SLPs are now required to complete thirty instructional contact hours in each three-year certification maintenance interval to retain their CCCs [25]. Although the requirement is recent, it appears that CE activities have become a main form of contact with the profession for many SLPs. However, as in many other professional organizations, the actual and full content of such activities are not exhaustively reviewed prior to approval, unlike peer-reviewed journal publication content.
ASHA-archived journals were a relatively popular choice for professional literature searches, but few other databases were reported to be used, including the freely available MEDLINE/PubMed. Any databases that required subscriptions (e.g., ComDisDome) or access to library resources to obtain access to full text were not frequently reported to be utilized by respondents. However, it should be noted that fewer than half of SLPs reported using the ASHA journal search and full-text utilities, despite the fact that they were free to members of ASHA. So, while ease of access may be a significant factor in the choices SLPs make, the fact remains that a majority of SLPs do not take advantage of their free access to ASHA journals. To maximize use of the archive, future study should examine whether this is because members are unaware of their benefit, do not have the necessary skills to search the journals, or do not find the journals' content relevant to clinical practice. Also, the ASHA journals represent only a subset of the wide range of journals that contain articles providing evidence needed for clinical decisions (e.g., New England Journal of Medicine, Journal of Communication Disorders, Stroke, Dysphagia, Journal of Fluency Disorders, Clinical Linguistics & Phonetics).
The majority of the respondents reported use of Websites to seek clinical information. The ASHA Website appears to be familiar to many, although others routinely visited less “authoritative” Websites regularly. With the increasing availability of information of varying types and quality on the Internet, the researchers believe this area is critical for student and practitioner education. Website evaluation in terms of authoritativeness, currency, purpose, and so on should be taught, as well as skills necessary to locate Websites that specifically provide evidence-based resources for SLPs. Among these are the Cochrane Collaboration <www.cochrane.org/reviews/>, the Academy of Neurologic Communication Disorders and Sciences <www.ancds.org/practice.html>, the Agency for Healthcare Research and Quality <www.ahrq.gov/clinic/epcix.htm>, and a potential future source for SLPs, the International Campbell Collaboration <www.campbellcollaboration.org>. Knowing the difference between general Internet search engines and scholarly article databases is essential but does not appear common from the survey responses, a problem also noted with practicing physicians [4].
SLPs most often reported learning how to seek and gain information from graduate program class requirements or related experiences (such as a research paper, a class with a professor, or discussions with fellow students). More than half of all respondents indicated that they had profited from each of these experiences. However, very few reported having had direct library instruction. The researchers believe that if students (and practicing clinicians) are to be expected to make evidence-based clinical decisions, EBP must be included and integrated into graduate coursework and curricula, along with direct training in effective strategies, techniques, and resources by a librarian.
SLPs' most frequently reported barriers to locating good information were lack of time, knowledge of where to find information, and knowledge of how to search for it, frequently reported barriers in other professions [3, 4, 6–8]. Finally, getting access to information (e.g., obtaining full text rather than abstracts, critical for successful EBP) was also reported as a barrier. Education and developing means of quick and easy access to pertinent information are areas needing immediate attention.
No study is without its limitations. One potential limitation of this study is the relatively low response rate (21%). While this rate is comparable to other surveys conducted with ASHA members, stronger conclusions could be drawn given a higher response rate. Additional funding to conduct a follow-up mailing could have helped this cause.
An additional limitation might have been that the survey was developed for a similar but different profession. Some of the questions were adapted, and others were added for the SLP population. While the researchers attempted to establish content validity through the review of the survey by ten recent graduates of a hearing and speech sciences program, this was the first use of the survey with SLPs, thereby potentially threatening internal validity.
Finally, the exclusion of university-based ASHA members (i.e., professors and research scientists) might be perceived as a limitation in that the study did not include the full range of ASHA certified member categories. It is important to note that the researchers intentionally excluded this subgroup with the intention of studying practicing SLPs. Educators could be included in a follow-up study to determine if there are differences between them and practitioners.
DIRECTIONS FOR FUTURE RESEARCH AND ACTION
Consistent with studies of other health-related professions, the most popularly reported source of information for SLPs was not peer-reviewed or scholarly publications, but rather discussions with peers. While ASHA has taken a leadership role and attempted to facilitate access by SLPs to the association's own wide number of scholarly publications, the availability of ASHA-published journals online does not appear to be evident to a number of respondents and should be made more apparent by the organization and by other relevant state and local agencies that oversee SLP practice. Relevant information in journals not published by ASHA will need to be made available as well. To address accessibility and time issues, as in other fields, clinical summaries such as meta-analyses, systematic reviews, and clinical practice guidelines will most likely need to be generated for practicing clinicians and made accessible on the Internet.
Graduate programs can better prepare students to become more effective professionals by integrating information literacy into the undergraduate and graduate curricula and integrating these skills with the concept of EBP [26]. As educators and organizers of information and with the current trend for librarians to integrate their work into that of their constituents, librarians can play a key role in the development and facilitation of EBP as it emerges in the field of speech-language pathology.
Some of the findings from this study warrant further exploration in future research. For example, because the majority of respondents in this study used Websites to seek clinical information, it would be interesting to gain more specific information about the types and quality of Websites visited along with the intended purpose for visiting them.
The current study provided an extensive array of responses that were difficult to analyze for quality on a finer level, rather they gave a more general idea of Website use. Because the respondents of this survey were skewed toward recent graduates, a follow-up study could contrast the searching behavior of more recent graduates with those who have been practicing clinicians for a longer period of time to determine similarities or differences in finding clinical “evidence” based on recent schooling versus more extensive clinical experience. Another area of potential research could compare practitioners with educators (e.g., university professors) in terms of their use of and attitudes toward information, particularly as it pertains to EBP. Finally, a study of measures taken by librarians to incorporate information literacy into the curriculum or CE activities would provide a helpful baseline for the development of workshops, materials, tutorials, or Websites to support the use of EBP in speech-language pathology.
Acknowledgments
Funding for this study was provided by a Library Faculty Research Funds grant, University of Maryland, College Park.
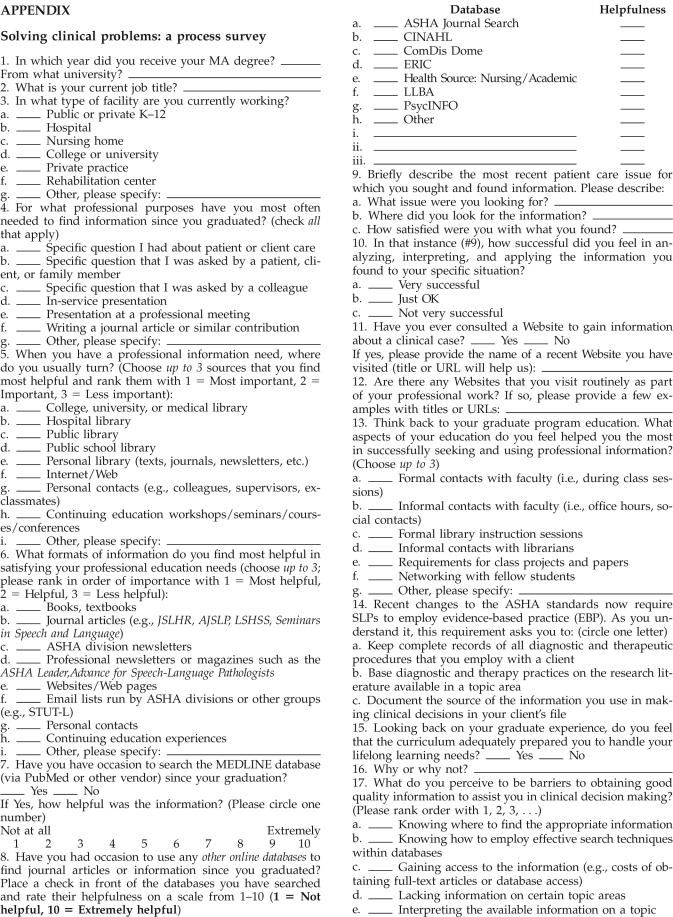
APPENDIX
Solving clinical problems: a process survey
REFERENCES
- American Speech-Language-Hearing Association. Background information and standards and implementation for the certificate of clinical competence in speech-language pathology. [Web document]. Rockville, MD: The Association, 2005. [rev. 8 Jul 2006; cited 2 Oct 2006]. <http://www.asha.org/about/membership-certification/handbooks/slp/slp_standards_new.htm>. [Google Scholar]
- American Speech-Language-Hearing Association. Evidence-based practice in communication disorders [position statement]. [Web document]. Rockville, MD: The Association, 2005. [cited 2 October 2006]. <http://www.asha.org/NR/rdonlyres/4837FDFC-576B-4D84-BDD6-8BFF2A803AD3/0/v4PS_EBP.pdf>. [Google Scholar]
- Coumou HCH, Meijman FJ. How do primary care physicians seek answers to clinical questions? a literature review. J Med Libr Assoc. 2006 Jan; 94(1):55–60. [PMC free article] [PubMed] [Google Scholar]
- Cullen RJ. In search of evidence: family practitioners' use of the Internet for clinical information. J Med Libr Assoc. 2002 Oct; 90(4):370–9. [PMC free article] [PubMed] [Google Scholar]
- Dawes M, Sampson U.. Knowledge management in clinical practice: a systematic review of information seeking behavior in physicians. Int J Med Inform. 2003;71:9–15. doi: 10.1016/s1386-5056(03)00023-6. [DOI] [PubMed] [Google Scholar]
- Dee C, Stanley EE. Information-seeking behavior of nursing students and clinical nurses: implications for health sciences librarians. J Med Libr Assoc. 2005 Apr; 93(2):213–22. [PMC free article] [PubMed] [Google Scholar]
- Estabrooks CA, O'Leary KA, Ricker KL, Humphrey CK.. The Internet and access to evidence: how are nurses positioned? J Adv Nurs. 2003;42(1):73–81. doi: 10.1046/j.1365-2648.2003.02581.x. [DOI] [PubMed] [Google Scholar]
- McAlister FA, Graham I, Karr GW, and Laupacis A. Evidence-based medicine and the practicing clinician. J Gen Intern Med. 1999 Apr; 14:236–42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Davis P. Effect of the Web on undergraduate citation behavior: guiding student scholarship in a networked age. [Web document]. 2003. [cited 2 Oct 2006]. <http://muse.jhu.edu/journals/portal_libraries_and_the_academy/v003/3.1davis.html>. [Google Scholar]
- Jensen J.. It's the information age, so where's the information? Coll Teach. 2004;52:107–12. [Google Scholar]
- Schaafsma F, Hulshof C, Van Dijk F, Verbeek J.. Information demands of occupational health physicians and their attitudes towards evidence-based medicine. Scan J Work Environ Health. 2004;30(4):327–30. doi: 10.5271/sjweh.802. [DOI] [PubMed] [Google Scholar]
- Cogdill KW. Information needs and information seeking in primary care: a study of nurse practitioners. J Med Libr Assoc. 2003 Apr; 91(2):203–15. [PMC free article] [PubMed] [Google Scholar]
- Jette DU, Bacon K, Batty C, Carlson M, Ferland A, Hemingway RD, Hill JC, Ogilvie L, and Volk D. Evidence-based practice: beliefs, attitudes, knowledge, and behaviors of physical therapists. Phys Ther. 2003 Sep; 83(9):786–805. [PubMed] [Google Scholar]
- Rappolt S, Tassone M.. How rehabilitation therapists gather, evaluate, and implement new knowledge. J Contin Ed Health Prof. 2002;22:170–80. doi: 10.1002/chp.1340220306. [DOI] [PubMed] [Google Scholar]
- Powell CA, Case-Smith J. Information literacy skills of occupational therapy graduates: a survey of learning outcomes. J Med Libr Assoc. 2003 Oct; 91(4):468–77. [PMC free article] [PubMed] [Google Scholar]
- Maloney S, Llic D, and Green S. Accessibility, nature and quality of health information on the Internet: a survey on osteoarthritis. Rheumatol. 2005 Mar; 44(3):382–5. [DOI] [PubMed] [Google Scholar]
- Mathur S, Shantin N, Brkaric M, Sood V, Kubeck J, Paulino C, and Merola AA. Surfing for scoliosis: the quality of information available on the Internet. Spine. 2005 Dec; 30(23):2695–700. [DOI] [PubMed] [Google Scholar]
- Pandolfini C, Bonati M. Follow-up of quality of public oriented health information on the World Wide Web: systematic re-evaluation. BMJ. 2002 Mar 9; 324(7337):582–3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sutherland LA, Wildemuth B, Campbell MK, and Haines PS. Unraveling the Web: an evaluation of the content quality. J Nutr Educ Behav. 2005 Nov/Dec; 37(6):300–5. [DOI] [PubMed] [Google Scholar]
- Vallino-Napoli LD, Reilly S. Evidence-based health care: a survey of speech pathology practice. Advan Speech Lang Pathol. 2004 Jun; 6(2):107–12. [Google Scholar]
- Manley SB, Frank EM, and Melvin CF. Preparation of speech-language pathologists to provide services to patients with a tracheostomy tube: a survey. Am J Speech Lang Pathol. 1999 May; 8(2):171–80. [Google Scholar]
- McCullough GH, Wertz RT, Rosenbeck JC, and Dinneen C. Clinicians' preferences and practices in conducting clinical/ bedside and videofluoroscopic swallowing examinations in an adult, neurogenic population. Am J Speech Lang Pathol. 1999 May; 8(2):149–63. [Google Scholar]
- Meline T, Paradiso T. Evidence-based practice in schools: evaluating research and reducing barriers. Lang Speech Hear Serv Sch. 2003 Oct; 34(4):273–83. [DOI] [PubMed] [Google Scholar]
- Tharpe AM, Fino-Szumski MS, and Bess FH. Survey of hearing aid fitting practices for children with multiple impairments. Am J Audiol. 2001 Jun; 10(1):32–40. [DOI] [PubMed] [Google Scholar]
- American Speech-Language-Hearing Association. Certification maintenance: basic requirements for maintaining the certificate of clinical competence (CCC-A and CCC-SLP). [Web document]. Rockville, MD: The Association, 2005. [rev. 7 Sep 2006; cited 2 Oct 2006]. <http://www.asha0/about/membership-certification/certification/fact_basics.htm>. [Google Scholar]
- Nail-Chiwetalu BJ, Bernstein Ratner N. Information literacy for speech-language pathologists: a key to evidence-based practice. Lang Speech Hear Serv Sch. 2006 Jul; 37:1–11. [DOI] [PubMed] [Google Scholar]