Abstract
Background
Rescue workers strive, after disasters, to help victims and restrict damage, often in dangerous circumstances. We examined the effect of a disaster on the physical and psychological health of rescue workers (firefighters, police officers and medical emergency services personnel) who provided assistance after the explosion of a fireworks depot in the Netherlands in May 2000.
Methods
We carried out a 4-year longitudinal study of 1403 rescue workers employed in or near the affected neighbourhood (the study group) and a control group of 1650 uninvolved rescue workers (from another city of similar size and urbanization). Health outcomes were measured as prevalence, incidence (both measured as the percent of workers who took sick leave), frequency of the absences and number of sick days (both per 100 workers), and duration (mean length of sickness absences, in days).
Results
Sick leave among the study workers increased substantially during the 18 months after the explosion. For example, the prevalence of absences attributed to psychological problems increased from 2.5% of workers during the 6 months before the disaster to 4.6% during the first 6-month period after the explosion and 5.1% during the second. That for respiratory problems rose from 5.4% predisaster to 14.9% 6–12 months afterward. In comparison with controls, immediate increases occurred in musculoskeletal, psychological, respiratory and nonspecific ill health (e.g., malaise, fatigue) during the first year postdisaster. Rates of sick leave for musculoskeletal and respiratory reasons remained elevated until 3 years postdisaster, whereas leave for psychological problems and other ill health had returned to predisaster levels by then. Neurological problems increased after a 1-year delay. No significant increase in gastrointestinal problems was observed among the study workers, in comparison with controls.
Interpretation
Many health problems arise immediately after a disaster and may persist for years. Health care workers should realize, however, that some disaster-related effects may not emerge until a year or more after the event.
Disasters strike suddenly, often involve large groups of people, cause substantial personal and societal damage, and lay a considerable burden on economic and public health resources.1–4 Rescue workers who rush to help victims and secure the area to prevent further casualties often face dangerous and demanding tasks that involve the risk of possibly fatal injury. Because of potential traumatic effects from these experiences, rescue workers are at risk of health problems after a disaster event.5
Although the negative effects of disasters on the health of primary victims are well documented,1,6–9 research on health consequences for rescue workers is relatively scarce. Rescue workers are, however, known to suffer psychological and physical health problems after disasters,5,10–14 and interest in this group is increasing.15 For example, after the 9/11 attack in Manhattan, rescue workers experienced high levels of musculoskeletal, respiratory and eye disorders;10 after the Oklahoma City bombing, firefighters showed significantly higher rates of posttraumatic stress disorder, depression and anxiety than before that event.14
Although rescue workers may suffer disaster-related health problems, their health seems to be affected less than that of primary victims, which suggests some level of additional resilience.1,5,14,16–19 Rescue work is generally performed by young, healthy men with extensive training and experience with calamities. Moreover, employers probably select personnel according to their suitability for emergency work, and self-selection makes it probable that only suitable individuals remain working in this demanding field.1,14,16,20
Because prior health information on people who undergo a calamity is ordinarily unavailable, it remains uncertain whether the health problems observed can be attributed to the disaster.21,22 In some countries, however, health information is routinely recorded in general practice, in hospitals and by occupational health services; this policy allows researchers to collect health data pre-and postdisaster and to validate whether the event directly affected the health of victims and rescue workers.22–26 Predisaster health information has previously been used to examine the effect of a disaster on the health of rescue workers in 2 studies: in Oklahoma14 and the Netherlands,25 respectively.
To investigate how a disaster affected the health of rescue workers, we made use of information on absences from work attributable to health problems (i.e., sickness absences or sick leave).27,28 Sick leave reflects the psychological, physical and social functioning of employees,29 and draws heavily on the country's economic and public health resources.30,31 It is therefore surprising that sick leave is rarely utilized in disaster research;25,32 our study may be considered an exploration of the feasibility of this approach.
Methods
On May 13, 2000, a fireworks depot in a residential neighbourhood of Enschede (a city of 150 000 in the Netherlands) exploded, killing 18 residents and 4 firefighters. Nearly 1000 people were injured, and over 1200 lost their homes.33
The target population of our study comprised rescue workers from Enschede and the surrounding municipalities, of whom practically all participated in rescue and recovery operations after the disaster. The electronic medical records of 1431 such rescue workers (hereafter referred to as the study workers) were obtained from the occupational health service from 6 months before (Nov. 13, 1999) through 31/2 years (42 mo) after the explosion on Nov. 12, 2003. Our final sample consisted of 1403 workers (98%) who were employed from at least 3 months before through 3 months after the event, including 547 firefighters, 799 police officers and 57 medical emergency service personnel (hereafter called medical personnel). During the 31/2-year period of follow-up, these study workers altogether worked 4145 person-years. Since 3 emergency services were involved, the nature of the disaster-related work and experiences varied considerably.19,34
The control group was composed of emergency personnel from another Dutch city with a similar level of urbanization and populace composition.35 In the control city, 1667 rescue workers were employed on the day of the disaster. Again, we included only those employed from at least 3 months before through 3 months after the disaster date (n = 1650; 99%): 177 firefighters, 1298 police officers and 175 medical personnel, who together worked 4675 person-years during the 31/2-year follow-up period.
Dutch law requires organizations to monitor the sick leave of their employees; until July 2005, it was mandatory that this be contracted out to an occupational health service. Employers notify the occupational health service of the dates that employees report being sick and resume work, and the service contacts the employee to establish the reason for absence. For shorter periods of sick leave, this information can be gathered via a telephone call or a response form. After 2–4 weeks of absence, the employee is invited to visit an occupational health physician who makes a formal diagnosis and assesses whether the employee requires additional care. To classify the health problems of employees, occupational health physicians use an adaptation of the International Classification of Diseases (ICD-10) for occupational medicine that is based on 12 “clusters” of organ systems, psychological problems and nonspecific symptoms.36
Because the occupational health service routinely registers sick leave, predisaster information was available for our study. Patients were informed about study participation by their occupational health physician via leaflets left in the waiting room and by the local newspapers, and could object to the use of their data (nobody did). To protect the anonymity of the study participants, the occupational health service removed all names, addresses and birth dates from the records but left sociodemographic data, including sex, age, employment admittance and dismissal dates, start and end dates of sickness absences, and diagnostic codes. We checked the records for inconsistencies; combined overlapping, consecutive or duplicate absences; and omitted any that lacked information on the causative illness or injury. Data collection followed the privacy protection guidelines of the Dutch Data Protection Authority; no explicit ethical approval or informed consent was needed.
Five indices of sick leave were generated to determine how sick leave was influenced by the disaster.37 These indices were computed per half-year period for the 6 most common clusters, and adjusted for person-time during which absence was counted in each period:
1. Prevalence: the percentage of workers with sick leave in current or new absences
2. Incidence: the percentage of workers with one or more new sick leaves
3. Frequency: the number of current or new sick leaves per 100 workers
4. Sick days: the number of days of sick leave per 100 workers
5. Duration of absences: the mean number of sick days per discrete sickness absence
Demographic characteristics of participants from both cities were compared by means of the χ2 test for frequencies and t tests for means. Sick leave information was analyzed in half-year periods from 6 months before the explosion until 3 years (36 mo) after. The subsequent 6-month period (i.e., months 37–42 postdisaster) served to follow up absences that had begun earlier.
Since repeated measurements were available, we used hierarchical linear models to compare changes in pre-and postdisaster sick leave between the 2 cities. The regression model was adapted to the data distribution of the respective index: linear regression for sick days and duration; Poisson regression for frequency; and logistic regression for prevalence and incidence.
To examine the effect of the disaster on the health of the study workers, changes in sick leave before and after the explosion were compared between study and control rescue workers. The pertinent variable (i.e., the group) was entered into the regression equation as interaction with 4 variables comparing sick leave after the explosion with that before. Three variables were generated to test whether absences increased during the 6 months immediately after the disaster (i.e., in months 1–6) and in the short (months 7–12) and longer terms (years 2 and 3) postdisaster, and a fourth to assess whether the longer-term difference was stable, increasing or decreasing. These regressions were adjusted for sex, age, job experience and occupation (firefighter, police officer or medical personnel). The coefficients reported denote changes in sick leave (pre-to postdisaster) of study workers compared with controls. Odds ratios are reported for logistic regression, rate ratios for Poisson regression, and β coefficients for linear regression, each with a 95% confidence interval.
Results
In the total, 3053 rescue workers were successfully monitored: 1403 study workers employed in the area of the Enschede disaster and 1650 control workers employed elsewhere. Most rescue workers were men (76.1%); women were significantly fewer in the study group (15%) than in the control group (31%; p < 0.001). The percentage of study firefighters was high, compared with controls (39% v. 11%, respectively; p < 0.001). Study workers and controls did not differ significantly in mean age (40.7 yr overall, standard deviation [SD] 9.0 yr) or mean job experience (13.6 [SD 10.4] yr).
Sick leave among the study workers was most frequent in the gastrointestinal, musculoskeletal, neurologic, psychological, respiratory and nonspecific ill-health clusters; data related to the blood, cardiovascular, skin, eye, endocrine, genitourinary and ear clusters were therefore not analyzed. In general, sick leave increased substantially during the 18 months after the explosion and then began to decline. In the second half of postdisaster year 3 (i.e., in months 31–36), the prevalence, incidence and frequency of sick leave among study workers returned to predisaster levels (Table 1). Although the number of sick days was still increased as of 3 years after the incident, it had begun to decrease.
Table 1
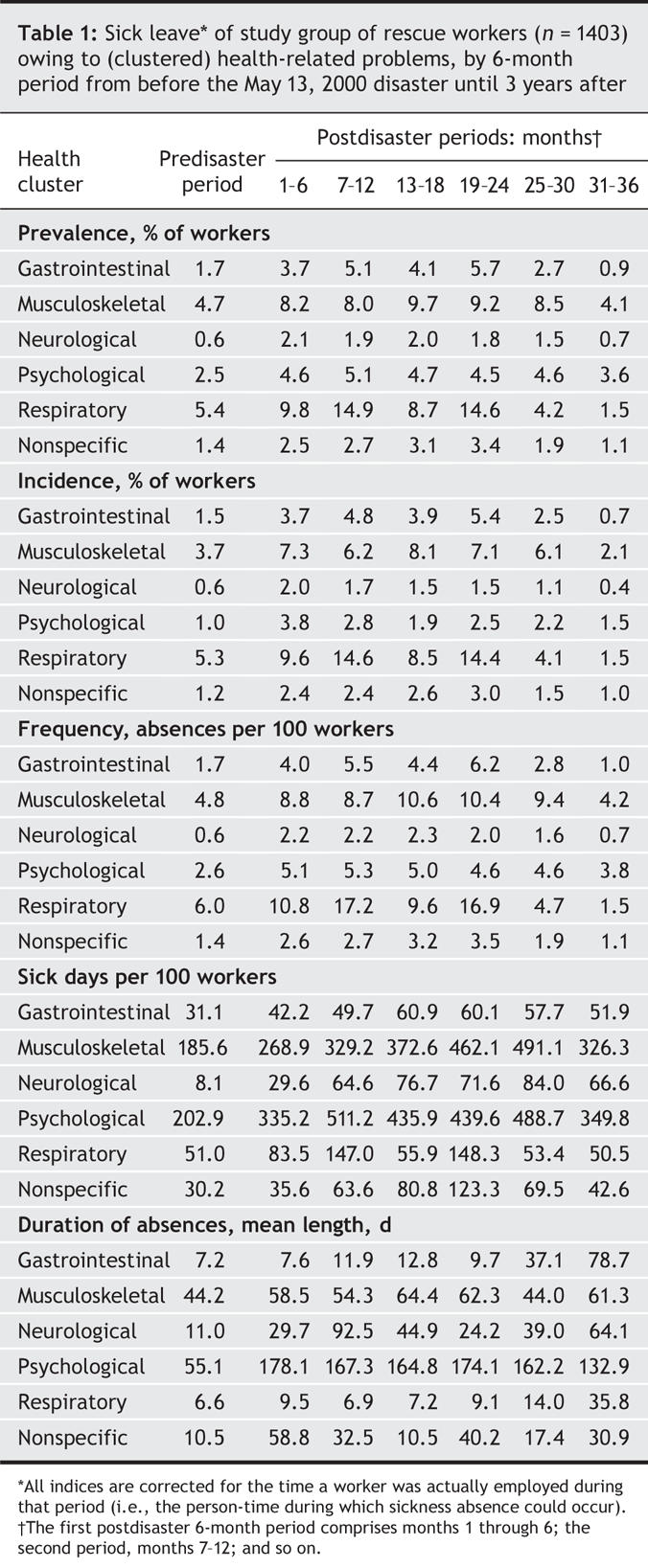
Increased sick leave among study workers does not permit the conclusion that their health problems were disaster-related; that would require that study workers show larger health changes from before to after the explosion than do controls. This was, in fact, the case, as indicated by odds and rate ratios exceeding 1 and estimated β coefficients above 0 (Appendix 1; available: www.cmaj.ca/cgi/content/full/176/9/1279/DC1). Odds ratios for the prevalence of sick leave among study workers compared with controls, for example, is shown in Fig. 1.
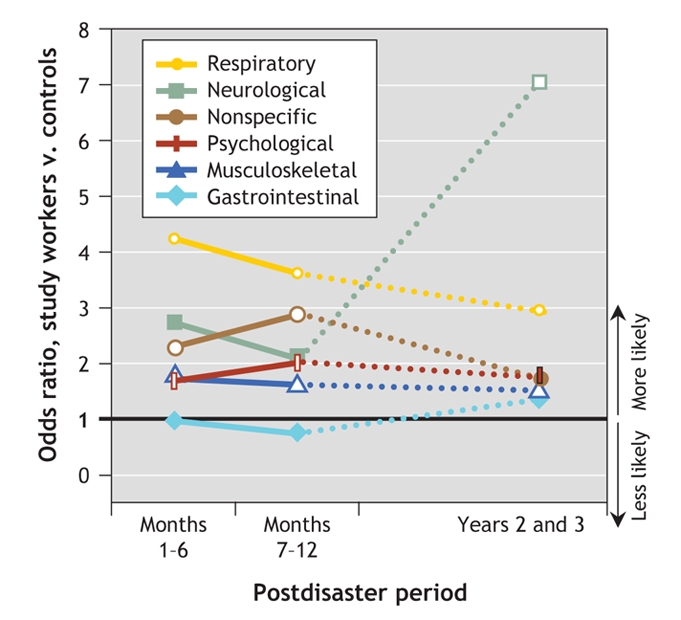
Fig. 1: Odds ratios for prevalences of sick leave, comparing the percentages of study workers who took sick leave against those of control workers. Results shown are for 6 health-related clusters of reasons why rescue workers were absent from work. Open (white-centred) symbols show statistical significance.
Gastrointestinal (nausea, vomiting, diarrhea): Although study workers' problems in this cluster were generally similar to those of controls, their absences were significantly longer. In years 2 and 3 postdisaster, study workers showed a decline in their prevalence, incidence and frequency of sick leave because of gastrointestinal illness, compared with controls.
Musculoskeletal (especially backache): Although study workers consistently showed larger increases in prevalence, incidence and frequency of absence, no significant group differences emerged in the number of sick days and duration (mean length) of absences for musculoskeletal reasons.
Neurologic (mainly migraine and headache): During the second 6-month period after the explosion (i.e., postdisaster months 7–12), the number of sick days increased. In years 2 and 3 postdisaster, the duration of related sickness absences in the study group was increased. Prevalence, incidence and frequency of absences were also increased, and in years 2 and 3 showed a considerable additional rise compared with controls (Fig. 1).
Psychological (mainly stress reactions such as posttraumatic stress disorder and burnout): The prevalence, incidence and frequency of related sick leave were greatly increased during the first year after the calamity, but returned to normal in subsequent years. Nevertheless, the number of sick days increased in months 7–12 and continued to be increased compared with controls. The duration of sick leave due to psychological problems, however, became longer only during the first 6 months after the explosion.
Respiratory (e.g., cough, sore throat, influenza): Prevalence, incidence and frequency of related absences peaked during months 1–6 after the event and remained high. Number of sick days was increased during the first year postdisaster, then normalized. During years 2 and 3 postdisaster, the mean duration of absences was lower in study workers than in controls, although the difference gradually decreased during this period.
Nonspecific ill health (primarily malaise and fatigue): Among study workers, prevalence, incidence and frequency of problems not specific to an organ system were higher during the first year; frequency increased further during the following 2 years. Compared with controls, however, study workers did not have more sick days or longer postdisaster absences due to nonspecific ill health.
Interpretation
This study is unique because we were able to investigate the impact of a disaster on the health of rescue workers using a control group as well as predisaster data.25,32 The health of study workers was clearly adversely affected by the explosion.10–13,25 Increases in psychological problems, as well as respiratory, musculoskeletal and nonspecific symptoms, emerged immediately afterward. Except for those attributed to psychological problems, these increases persisted for years. Moreover, the number of sick days due to respiratory symptoms was elevated during the first year postdisaster.
For psychological problems, a much greater increase in sick days was found, which persisted until the end of the study period. Nevertheless, 2–3 years after the disaster no significant difference was observed between study workers and controls for the incidence, prevalence and frequency of sick leave due to psychological problems. Neurologic symptoms did not increase until year 2, which became apparent in the prevalence, incidence, frequency and days of sick leave. Confidence intervals for neurologic symptoms were wide, presumably because predisaster rates were low, such that even some relatively large odds ratios during the first postdisaster year remained statistically nonsignificant.
Finally, even 2–3 years after the event, the incidences of sick leave among study workers for musculoskeletal, respiratory and neurologic symptoms continued to be higher than those of controls. Even toward the end of the study period, musculoskeletal and respiratory symptoms still caused increased sick leave.
Previous research on rescue workers focused more on disorders such as posttraumatic stress and depression than on physical health.1 Our study confirms that rescue workers do develop psychological problems after disaster work,10,38,39 and extends these findings to physical symptoms. Our study, like previous reports, suggests that rescue workers and primary victims suffer different types of health problems after a disaster. Rescue workers seem more susceptible to respiratory and musculoskeletal symptoms and alcohol abuse; primary victims, to psychological problems and gastrointestinal symptoms.10,14,24,40 Unfortunately, direct comparisons between rescue workers and disaster survivors are scarce in the literature. In addition, in published studies, it is important to adjust for predisaster differences between rescue workers and members of the general population (which includes the primary victims of the disaster event) that may affect their postdisaster health: First, compared with the general population, rescue workers are usually in a younger age range and predominantly male. Second, they receive emergency training, have experience with precarious situations and must be physically fit.19 Third, primary victims of a disaster are directly exposed to it, whereas rescue workers are often confronted only with its aftermath.1
This study had several limitations. First, although the use of sick leave data from occupational health service registrations rules out response bias, inconsistencies may arise from differences in how individual occupational physicians interpret their patients' symptoms. Second, some employees may continue working even though they are ill, and thus not report relevant health problems (particularly milder ones). Third, although the control city was chosen to maximize comparability with Enschede with respect to population demographics, individual study workers and controls were not matched; we therefore adjusted our comparisons between study-and control-group workers for their demographic characteristics. Because these limitations may have lowered the sensitivity of our analyses (that is, the limitations may have widened the confidence intervals), the health impact of the calamity may be underestimated. However, a strength of our study is that the health problems recorded were evaluated by physicians, whereas other studies have mainly used self-report. Moreover, the design of our longitudinal controlled study allows the conclusion that disasters generate health problems in rescue workers.
Few disaster studies have used electronic medical records from occupational health services.25,26 Perhaps the greatest advantage of sick-leave records, particularly in countries where the information is collected routinely, is that predisaster health information is available.29,41 Moreover, the demographic and occupational information in these databases facilitates the investigation of risk factors for and occupational differences in postdisaster health sequelae. An important clinical implication is that experience and training apparently do not make rescue workers immune to the consequences of disasters: they may indeed develop health problems. Our study has shown that rescue workers experienced health problems immediately after a disaster, and continued to do so throughout the study period. Health care workers should be made aware that disaster-related health problems may not emerge until several years after the disaster. It is important that symptoms are taken seriously and that aftercare is available, to allow rescue workers to continue or resume their work.
@ See related article page 1293
Supplementary Material
Acknowledgments
We are grateful to the emergency services of both cities for allowing us to use the sick-leave data of their employees, and to the occupational health services for making these records available. In particular, we thank the occupational physicians and others at the occupational health services for extracting the data from their records. We also thank Petra ten Veen for her help with data management.
Footnotes
This article has been peer reviewed.
Contributors: Mattijn Morren performed data collection and statistical analysis. Anja Dirkzwager contributed to the design of the study and performed data collection. Frans Kessels performed data collection. Joris Yzermans contributed to the design of the study and performed project management. All authors contributed to the writing of the article and approved the final version for publication.
This study was funded by the Dutch Ministry of Health, Welfare, and Sport.
Competing interests: None declared.
Correspondence to: Dr. Mattijn Morren, Netherlands Institute for Health Services Research, PO Box 1568, 3500 BN Utrecht, The Netherlands; fax +31 30 2729 729; m.morren@nivel.nl
REFERENCES
- 1.Norris FH, Friedman MJ, Watson PJ, et al. 60 000 disaster victims speak: part I. An empirical review of the empirical literature, 1981–2001. Psychiatry 2002;65:207-39. [DOI] [PubMed]
- 2.Noji EK. Public health issues in disaster. Crit Care Med 2005;33(Suppl 1):S29-S33. [DOI] [PubMed]
- 3.Domino ME, Fried B, Moon Y, et al. Disasters and the public health safety net: hurri cane Floyd hits North Carolina Medicaid program. Am J Public Health 2003;93:1122-7. [DOI] [PMC free article] [PubMed]
- 4.Aoki N, Nishimura A, Pretto EA, et al. Survival and cost analysis of fatalities of the Kobe earthquake in Japan. Prehosp Emerg Care 2004;8:217-22. [DOI] [PubMed]
- 5.Marmar CR, Weiss DS, Metzler TJ, et al. Longitudinal course and predictors of continuing distress following critical incident exposure in emergency services personnel. J Nerv Ment Dis 1999;187:15-22. [DOI] [PubMed]
- 6.Ursano R, Fullerton C, Kao T, et al. Longitudinal assessment of posttraumatic stress disorder and depression after exposure to traumatic death. J Nerv Ment Dis 1995;183:36-42. [DOI] [PubMed]
- 7.Leon GR. Overview of the psychosocial impact of disasters. Prehospital Disaster Med 2004;19:4-9. [DOI] [PubMed]
- 8.Katz CL, Pellegrino L, Pandya A, et al. Research on psychiatric outcomes and interventions subsequent to disasters: a review of the literature. Psychiatry Res 2002;110:201-17. [DOI] [PubMed]
- 9.Yzermans CJ, Dirkzwager AJE, Breuning E. Long-term health consequences of disaster: a bibliography. Utrecht: Netherlands Institute for Health Services Research; 2005.
- 10.Berríos-Torres SI, Greenko JA, Phillips M, et al. World Trade Center rescue worker injury and illness surveillance, New York, 2001. Am J Prev Med 2003;25:79-87. [DOI] [PubMed]
- 11.Feldman DM, Baron SL, Bernard BP, et al. Symptoms, respirator use, and pulmonary function changes among New York City fire-fighters responding to the World Trade Center disaster. Chest 2004;125:1256-64. [DOI] [PubMed]
- 12.Liao SC, Lee MB, Lee YJ, et al. Association of psychological distress with psychological factors in rescue workers within two months after a major earthquake. J Formos Med Assoc 2002;101:169-76. [PubMed]
- 13.Fullerton CS, Ursano RJ, Wang L. Acute stress disorder, posttraumatic stress disorder, and depression in disaster or rescue workers. Am J Psychiatry 2004;161:1370-6. [DOI] [PubMed]
- 14.North CS, Tivis L, McMillen JC, et al. Psychiatric disorders in rescue workers after the Oklahoma City bombing. Am J Psychiatry 2002;159:857-9. [DOI] [PubMed]
- 15.Slottje P, Huizink AC, Twisk JW, et al. Epidemiological study air disaster in Amsterdam (ESADA): study design. BMC Public Health 2005;5:54. [DOI] [PMC free article] [PubMed]
- 16.Dyregrov A, Kristoffersen JI, Gjestad R. Voluntary and professional disaster-workers: similarities and differences in reactions. J Trauma Stress 1996;9:541-55. [DOI] [PubMed]
- 17.Norris FH, Friedman MJ, Watson PJ. 60 000 disaster victims speak: part II. Summary and implications of the disaster mental health research. Psychiatry 2002;65:240-60. [DOI] [PubMed]
- 18.Ersland S, Weisæth L, Sund A. The stress upon rescuers involved in an oil rig disaster: “Alexander L. Kielland” 1980. Acta Psychiatr Scand Suppl 1989;355:38-49. [DOI] [PubMed]
- 19.Morren M, Yzermans CJ, Van Nispen RM, et al. The health of volunteer firefighters three years after a technological disaster. J Occup Health 2005;6:523-32. [DOI] [PubMed]
- 20.North CS, Tivis L, McMillen JC, et al. Coping, functioning, and adjustment of rescue workers after the Oklahoma City bombing. J Trauma Stress 2002;15:171-5. [DOI] [PubMed]
- 21.Dominici F, Levy JI, Louis TA. Methodological challenges and contributions in disaster epidemiology. Epidemiol Rev 2005;27:9-12. [DOI] [PubMed]
- 22.Reijneveld SA, Crone MR, Verhulst FC, et al. The effect of a severe disaster and the mental health of adolescents: a controlled study. Lancet 2003;362:691-6. [DOI] [PubMed]
- 23.Dorn T, Yzermans CJ, Kerssens JJ, et al. Disaster and subsequent health care utilization: a longitudinal study among victims, their family members and control subjects. Med Care 2006;44:581-9. [DOI] [PubMed]
- 24.Yzermans CJ, Donker GA, Kerssens JJ, et al. Health problems of victims before and after disaster: a longitudinal study in general practice. Int J Epidemiol 2005;34:820-6. [DOI] [PubMed]
- 25.Dirkzwager AJE, Yzermans CJ, Kessels FMJ. Psychological, musculoskeletal, and respiratory problems and sickness absence before and after involvement in a disaster: a longitudinal study among rescue workers. Occup Environ Med 2004;61:870-2. [DOI] [PMC free article] [PubMed]
- 26.Alexander DA, Wells A. Reactions of police officers to body-handling after a major disaster: a before-and-after comparison. Br J Psychiatry 1991;159:547-55. [DOI] [PubMed]
- 27.Marmot M, Feeney A, Shipley M, et al. Sickness absence as a measure of health status and functioning: from the UK Whitehall II study. J Epidemiol Community Health 1995;49:124-30. [DOI] [PMC free article] [PubMed]
- 28.Kivimäki M, Head J, Ferrie JE, et al. Sickness absence as a global measure of health: evidence from mortality in the Whitehall II prospective cohort study. BMJ 2003;327:364-9. [DOI] [PMC free article] [PubMed]
- 29.Benavides FG, Benach J, Mira M, et al. Occupational categories and sickness absence certified as attributable to common diseases. Eur J Public Health 2003;13:51-5. [DOI] [PubMed]
- 30.Houtman IRL. Work-related stress. Dublin: European Foundation for the Improvement of Living and Working Conditions; 2005.
- 31.Gründemann RWM, Van Vuuren CV. Preventing absenteeism at the workplace. Dublin: European Foundation for the Improvement of Living and Working Conditions; 1997.
- 32.Marmar CR, Weiss DS, Metzler TJ, et al. Stress responses of emergency services personnel to the Loma Prieta earthquake Interstate 880 freeway collapse and control traumatic incidents. J Trauma Stress 1996;9:63-85. [DOI] [PubMed]
- 33.Roorda J, van Stiphout WA, Huijsman-Rubingh R. Post-disaster health effects: strategies for investigation and data-collection experiences from the Enschede firework disaster. J Epidemiol Community Health 2004;58:982-7. [DOI] [PMC free article] [PubMed]
- 34.Van der Velden PG, Christiaanse B, Kleber R, et al. The effects of disaster exposure and post-disaster critical incidents on intrusions, avoidance reactions and health problems among firefighters: a comparative study. Stress Trauma Crisis 2006;9:73-93.
- 35.Statline. Statistics Netherlands. The Netherlands: Voorburg/Heerlen; 2005. Available: http://statline.cbs.nl/StatWeb/start.asp?lp=Search/Search (accessed 2007 March 20).
- 36.CAS. Classification of complaints, diseases, and causes for company and insurance doctors [in Dutch]. Voorlichtingscentrum Sociale Verzekering. Utrecht: Lisv; 1997.
- 37.Hensing G, Alexanderson K, Allebeck P, et al. How to measure sickness absence? Literature review and suggestion of five basic measures. Scand J Soc Med 1998;26:133-44. [DOI] [PubMed]
- 38.Sommers E, Porter K, DeGurski S. Providers of complementary and alternative health services in Boston respond to September 11. Am J Public Health 2002;92:1597-8. [DOI] [PMC free article] [PubMed]
- 39.Gallanter T, Bozeman WP. Firefighter illnesses and injuries at a major fire disaster. Prehosp Emerg Care 2002;6:22-6. [DOI] [PubMed]
- 40.Reacher M, McKenzie K, Lane C, et al. Health impacts of flooding in Lewes: a comparison of reported gastrointestinal and other illness and mental health in flooded and non-flooded households. Commun Dis Public Health 2004;7:39-46. [PubMed]
- 41.European Foundation for the Improvement of Living and Working Conditions (EUROFOUND). Preventing absenteeism at the workplace — European research report. Luxembourg: The Foundation, 1997.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


