Abstract
Background
Patient problem solving and decision making are recognized as essential to effective self-management across multiple chronic diseases. However, a health-related problem-solving instrument that demonstrates sensitivity to disease control parameters in multiple diseases has not been established.
Objectives
To determine, in two disease samples, internal consistency and associations with disease control of the Health Problem-Solving Scale (HPSS), a 50-item measure with 7 subscales assessing effective and ineffective problem-solving approaches, learning from past experiences, and motivation/orientation.
Design
Cross-sectional study.
Participants
Outpatients from university-affiliated medical center HIV (N = 111) and diabetes mellitus (DM, N = 78) clinics.
Measurements
HPSS, CD4, hemoglobin A1c (HbA1c), and number of hospitalizations in the previous year and Emergency Department (ED) visits in the previous 6 months.
Results
Administration time for the HPSS ranged from 5 to 10 minutes. Cronbach’s alpha for the total HPSS was 0.86 and 0.89 for HIV and DM, respectively. Higher total scores (better problem solving) were associated with higher CD4 and fewer hospitalizations in HIV and lower HbA1c and fewer ED visits in DM. Health Problem-Solving Scale subscales representing negative problem-solving approaches were consistently associated with more hospitalizations (HIV, DM) and ED visits (DM).
Conclusions
The HPSS may identify problem-solving difficulties with disease self-management and assess effectiveness of interventions targeting patient decision making in self-care.
Key words: problem solving, decision making, chronic disease, disease control, measure development, minority populations
Facilitating effective patient self-management of chronic disease is a challenge for health care professionals and patients.1,2 Patient problem solving and decision making are deemed important for translating education and adherence counseling into active self-management in daily life.3–5 Studies have identified patient problem solving as a predictor of coping and health behaviors in multiple diseases,6,7 and a recent meta-analysis found social problem-solving therapy effective in relieving emotional and physical symptoms in samples treated for depression, substance abuse, and cancer.8
Limitations in literature warrant further investigation. First, problem-solving treatments in primary care settings generally have not measured patient problem solving to screen patients for problem-solving intervention, or to evaluate whether interventions were effective in improving problem-solving ability.9–12 Second, there are currently no measures of patient health-related problem solving for use across chronic diseases or for patients with multiple health conditions. Although generic measures (Problem-Solving Inventory13 and Social Problem-Solving Inventory14) are available, generic scales are generally less sensitive to disease-specific clinical outcomes than disease- or health-specific measures.15–17 Finally, although improved disease control is often a desired intervention outcome, studies of associations between patient problem solving and clinical measures of disease control are few.
The purpose of this cross-sectional study was twofold: (1) to determine whether a health-related problem-solving measure (Health Problem-Solving Scale [HPSS]) demonstrates adequate internal consistency in two independent adult, outpatient, chronic disease samples (HIV, diabetes mellitus [DM]); and (2) to determine associations of the HPSS with selected disease control parameters (CD4, hemoglobin A1c [HbA1c], Emergency Department [ED] visits, and hospitalizations).
METHODS
Instrument Development
The HPSS was developed from two previous studies,5,18 and item and response formats were modeled after a standardized generic measure, the Social Problem-Solving Inventory.14 Based on a conceptual model of problem solving in chronic disease self-management, the HPSS assesses self-report of effective and ineffective approaches to managing health-related problems.5 Items were generated from a focus group study with adult diabetes patients, in which 251 patient descriptions of how they handle problem situations with self-management were coded then reviewed and categorized by an expert panel.18 Responses that differentiated participants in good versus poor disease control were developed into questionnaire items and grouped into subscales reflecting the coded categories reviewed by the expert panel. For the HPSS, wording for items used “health” or “health condition(s)”to refer to medical conditions rather than disease-specific terms.
The resulting HPSS had 56 items, 6 of which were dropped from the scale because of confusing wording during pretesting on a small sample. The final HPSS was a 50-item instrument with seven subscales representing coded categories from the conceptual model: (1) effective problem solving (EPS, e.g., “Before I do something that will affect my health, I think about all the options”), (2) impulsive/careless problem solving (IPS, e.g., “Sometimes, I know I am doing the wrong thing for my health problem, but I just cannot stop myself”), (3) avoidant problem solving (APS, e.g., “I put off trying to deal with problems with my health condition as long as I can”), (4) positive transfer of past experience/learning (PTR, e.g., “When I find something that makes my health condition better, then I make sure I remember what it was and how I did it”), (5) negative transfer of past experience/learning (NTR, e.g., “I get stuck doing the same things I have always done, even if those things do not help”), (6) positive motivation/orientation (PMO, e.g., “When I think about the problems that can happen because of poor health, I want to do even more to take care of my health condition”), (7) negative motivation/orientation (NMO, e.g., “I feel there is nothing I can do about problems that come up with my health”).
Respondents used a 5-point Likert scale ranging from “not at all true of me” (0 points) to “extremely true of me” (4 points). Subscale scores were calculated by summing scores for each item in the respective subscale. Health Problem-Solving Scale total score was derived using the formula:  , which sums the subscale averages, with reverse scoring of the negative subscales. Higher subscale scores indicate more of that problem-solving characteristic. Higher total HPSS scores indicate more effective health-related problem solving.
, which sums the subscale averages, with reverse scoring of the negative subscales. Higher subscale scores indicate more of that problem-solving characteristic. Higher total HPSS scores indicate more effective health-related problem solving.
Study Participants Outpatients were recruited from two university-affiliated medical center clinics selected to represent different populations with regard to disease and patient sociodemographic characteristics. The HIV sample was recruited from an HIV clinic whose patients are predominantly male, African-American, with Medicaid (60%). The DM sample was recruited from a Diabetes Center, whose patients are predominantly female, white, with 55% private insurance/self-pay (19% Medicaid). Eligibility criteria were ≥18 years of age, currently a clinic patient, with diagnosis of HIV or diabetes, able to give informed consent, and able to complete study questionnaires.
Procedure In clinic waiting rooms during routine appointment hours, a research assistant (RA) handed patients flyers describing the study. Interested patients were instructed to approach the RA to complete an informed consent followed by study questionnaires. Disease control data were gathered from participants’ electronic medical records. Participants received a $10 reimbursement. The study was approved by the Institutional Review Board.
Measures of Disease Control, Emergency Department Visits, and Hospitalizations For HIV and DM, CD4 count and HbA1c results, respectively, were obtained on the day of the clinic visit or the most recent date within 1 month of the clinic visit. The number of ED visits in the past 6 months and hospitalizations in the past year were self-reported and confirmed by medical record review. If patients underreported utilization data relative to the medical record, then medical record data were used. If participants overreported relative to the medical record, then the larger number was used to capture utilization that may have occurred outside the medical center.
Statistical Analyses Participant characteristics were analyzed using descriptive statistics. Gender, age, race/ethnicity, and disease duration were not associated with HPSS total or subscale scores in either sample; therefore, those variables were not included as covariates in further analyses. Cronbach’s alpha was used to determine internal consistency (reliability) of the HPSS total scale and subscales.19 Pearson’s product–moment correlation coefficients were used to measure associations between HPSS and CD4 and HbA1c. Because of departures from normality assumptions, Spearman’s rank correlation coefficients were used to measure associations between HPSS and hospitalizations and ED visits. Statistical analyses were conducted using SAS (Cary, NC, USA) statistical software package (version 9.1).
RESULTS
Participant Characteristics
Participants were 199 patients (90% response rate in HIV clinic, 86% in DM clinic). Incomplete HPSS protocols (n = 10, HIV) were excluded from analyses. Characteristics of the final HIV (N = 111) and DM (N = 78) samples are in Table 1.
Table 1.
Participant Characteristics, Disease Control, and HPSS Scores for HIV and DM Clinic Patients
| HIV (N = 111) | DM (N = 78) | |
|---|---|---|
| Age, mean (SD) | 45 (8.1) | 51.2 (14.7) |
| Male, n (%) | 64 (59.8) | 32 (41.0) |
| Race/Ethnicity, n (%) | ||
| White | 7 (6.25) | 43 (55.1) |
| Black/African-American | 99 (89.3) | 32 (41.0) |
| Hispanic/Latino(a) | 0 | 3 (3.9) |
| Native American | 2 (1.8) | 0 |
| Others | 3 (2.7) | 0 |
| Years of disease duration, n (%) | ||
| <1–5 | 29 (26.1) | 28 (35.9) |
| 6–10 | 33 (28.8) | 11 (14.1) |
| 10–20 | 41 (37.0) | 26 (33.3) |
| >20w | 9 (8.1) | 13 (16.7) |
| CD4 cells/mm3, mean (SD) | 324 (230) | – |
| HbA1c %, mean (SD) | – | 7.8 (1.6) |
| No. of ED visits in past 6 months, mean (SD) | 1.7 (2.9) | 0.9 (2.0) |
| No. of hospitalizations in past year, mean (SD) | 1.0 (1.7) | 0.7 (1.5) |
| HPSS total score | 19.7 (4.0) | 20.8 (3.9) |
| HPSS subscale scores | ||
| Effective problem solving | 22.8 (7.3) | 22.9 (6.5) |
| Impulsive/Careless problem solving | 6.3 (6.5) | 5.1 (5.8) |
| Avoidant problem solving | 6.3 (6.0) | 4.3 (5.5) |
| Positive transfer of past experience/learning | 13.6 (8.7) | 11.3 (7.7) |
| Negative transfer of past experience/learning | 12.5 (4.2) | 13.2 (3.8) |
| Positive motivation/orientation | 12.8 (3.8) | 13.4 (3.6) |
| Negative motivation/orientation | 5.7 (4.6) | 4.5 (4.5) |
DM = diabetes mellitus, HPSS = Health Problem-Solving Scale.
HPSS Characteristics and Internal Consistency
Administration time for the HPSS was generally 5 minutes, with a few patients requiring up to 10 minutes. Health Problem-Solving Scale total and subscale scores are presented in Table 1. Cronbach’s alpha for the HPSS total scale and subscales, in the HIV and DM samples, respectively, were are follows: HPSS total scale 0.86 and 0.89, EPS 0.82 and 0.82, IPS 0.85 and 0.88, APS 0.82 and 0.89, PTR 0.69 and 0.74, NTR 0.82 and 0.85, PMO 0.63 and 0.66, and NMO 0.74 and 0.83. These internal reliability coefficients were comparable in the two samples and within an acceptable psychometric range.19
Consistent with the theoretical model,5 HPSS subscales reflecting effective/positive problem-solving components were intercorrelated (HIV sample r = 0.70 to .73, all P < 0.001; DM sample r = 0.79 to .81, all P < 0.001), and subscales reflecting ineffective/negative components were intercorrelated (HIV sample r = 0.73 to .84, all P < 0.001; DM sample r = 0.78 to .85, all P < 0.001). Positive subscales were weakly correlated with their respective negative subscales.
Problem Solving and Disease Control
Associations between HPSS and CD4, HbA1c, hospitalizations, and ED visits were all in hypothesized directions in both HIV and DM (Table 2) (Fig. 1). Health Problem-Solving Scale subscales showed differential patterns of association in the two samples, with stronger associations of negative/ineffective subscales in HIV and stronger associations of positive/effective subscales in DM. Overall, associations were weaker in HIV than in DM.
Table 2.
Associations Between Patient Problem-Solving Scores and Disease Control
| HIV | DM | |||||
|---|---|---|---|---|---|---|
| CD4 | Hospitalizations | ED visits | HbA1c | Hospitalizations | ED visits | |
| r | ρ | ρ | r | ρ | ρ | |
| HPSS Total Score | 0.25* | −0.23* | −0.15 | −0.44† | −0.38* | −0.38* |
| HPSS Subscale Scores: | ||||||
| Effective problem solving | 0.09 | −0.02 | 0.0 | −0.45† | −0.12 | −0.25* |
| Impulsive/Careless problem solving | 0.16 | 0.19* | 0.11 | 0.15 | 0.14 | 0.22 |
| Avoidant problem solving | −0.23* | 0.27† | 0.16 | 0.11 | 0.25* | 0.38† |
| Positive transfer of past experience/learning | 0.19 | 0.02 | −0.07 | −0.53‡ | −0.21 | −0.25* |
| Negative transfer of past experience/learning | −0.22* | 0.29† | 0.14 | 0.30 | 0.38† | 0.38† |
| Positive motivation/orientation | 0.12 | −0.11 | −0.11 | −0.54‡ | −0.29* | −0.38† |
| Negative motivation/orientation | −0.26* | 0.26† | 0.25* | 0.30 | 0.42† | 0.34† |
r = Pearson’s product–moment correlation coefficients. ρ = Spearman’s rank correlation coefficients.
DM = diabetes mellitus, ED = Emergency Department, HPSS = Health Problem-Solving Scale.
*P < 0.05.
†P < 0.01.
‡P < 0.001.
Figure 1.
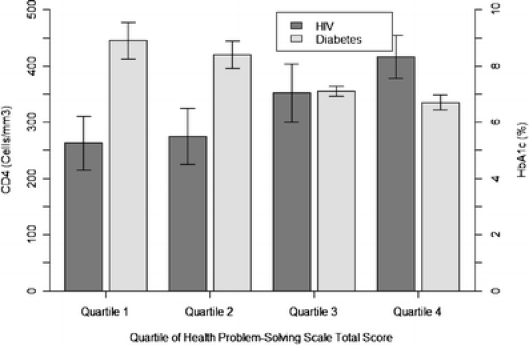
Mean CD4 or HbA1c by HPSS total score quartiles for HIV and diabetes samples, respectively, with standard error bars. Quartile 1 (lowest HPSS total scores) represents least effective problem solving (EPS) and quartile 4 (highest HPSS total scores) represents most EPS. Health Problem-Solving Scale quartile ranges for the HIV sample are 10.5–16.1 (Q1), 16.2–20.7 (Q2), 20.8–22.9 (Q3), and 23.0–28.0 (Q4). Health Problem-Solving Scale quartile ranges for the DM sample are 10.5–18.5 (Q1), 18.6–21.8 (Q2), 21.9–23.6 (Q3), and 23.7–28.0 (Q4). CD4 count is significantly different between the first and fourth HPSS quartiles and the second and fourth HPSS quartiles in the HIV sample (both P < 0.05). HbA1c is significantly different between the first and third HPSS quartiles, first and fourth HPSS quartiles, and second and fourth HPSS quartiles in the diabetes sample (all P < 0.05). Analysis of variance overall F test, P = .09 in HIV and P = 0.005 in diabetes.
DISCUSSION
In HIV and DM samples representing differing sociodemographic characteristics, the HPSS demonstrated good internal consistency and hypothesized associations with disease control variables. Differential associations of subscales with CD4, HbA1c, hospitalizations, and ED visits suggest that problem-solving skill, learning, and motivation components, may differ in their contribution to outcomes.14,17 This finding reinforces the importance of addressing multiple problem-solving components, not just rational problem-solving skill, for efficacy of problem-solving interventions.8
The current study demonstrates that the HPSS may have utility as a measure of patient health-related problem solving in multiple diseases. Analysis of the HPSS in larger and additional chronic disease samples is needed and encouraged to further determine psychometric properties of the scale and to reduce number of items for greater administration efficiency. Clinical utility of the HPSS includes use as a screening instrument to identify patients who may be most in need of problem-solving interventions as part of patient education and disease self-management training. Moreover, future reports on the scale’s sensitivity to change are warranted to establish its utility as an outcome measure for evaluating effectiveness of interventions in modifying patients’ problem-solving abilities for better disease management and control.
Acknowledgement
The authors wish to thank Bill Ruby, MD, Heather Campbell, MPH, Christopher Saudek, MD, and Sherita Hill Golden, MD, MHS for providing access to clinic patients recruited for participation in this study. This research was supported by a supplement to NIH grant R01 DK48117, grant NIH K01 HL076644, and the Johns Hopkins Center for Mind Body Research (R21 NS048593).
Potential Financial Conflicts of Interest None disclosed.
Appendix
Health Problem-Solving Scale
Please read the statements below. They are thoughts and feelings people sometimes have about taking care of their health condition(s) and problems that can come up with their health. Problems include trouble managing symptoms (like pain, fatigue, shortness of breath, or thirst) and difficulties sticking to your treatments (like taking medication, following a healthy diet, or doing exercise/physical activity). Problems with your health condition(s) can also include things like dealing with emotions, social relationships, or problems taking care of your health while trying to go about your everyday life.
Write down the number for how much these statements are true of how you think or feel. Please use these options:
I know that my choices about taking care of my health condition(s) make a difference in how things come out in the end.
I cannot find ways to stop problems with my health condition(s) from getting worse.
I find myself dealing with the same problems with my health over and over again.
I put off trying to deal with problems with my health condition(s) as long as I can.
I know exactly what types of problems I could have with my health condition(s) and my body each day.
I can find ways to manage how much my health condition(s) interfere with my life.
I always take time to consider how the things I choose to do can help or hurt my health condition(s).
Sometimes I decide that I am going to stop taking care of my health condition(s) and do the things I want to do.
I avoid the things that I figure out make my health condition(s) worse (such as certain foods, types of activity, places, or environments).
I try to solve problems with my health condition(s), but it seems like nothing works.
I try to conquer my health condition(s), but problems with my health are conquering me.
If I do not like the way treatments for my health condition(s) make me feel (for example, medications or doing exercise), then I stop taking those treatments.
When a problem with my health condition(s) happens, I am able to figure out what caused the problem.
Bad experiences with my health condition(s) discourage me from trying to solve new problems that come up with my health.
Dealing with my health problems makes me want to give up.
I use things that have worked before to solve new problems that come up with my health.
I get stuck doing the same things I have always done, even if those things do not help.
I am able to solve problems that come up with my health.
When I find something that makes my health condition(s) better, then I make sure I remember what it was and how I did it.
I can think of many different things to do to solve the problems I experience with my health condition(s).
When I have a problem with my health condition(s) that I do not know how to deal with, I find a way to get the answers.
I get so upset when a problem comes up with my health that it is hard for me to think straight.
I forget to do the things that I know work to make my health condition(s) better.
Before I do something that will affect my health, I think about all the options.
When I am having problems with my health, I avoid dealing with them.
Over time, it gets harder and harder for me to handle problems with my health.
Sometimes, I know I am doing the wrong thing for my health problem(s), but I just cannot stop myself.
I have no trouble putting plans for dealing with my health problems into actions.
Bad experiences with my health condition(s) have taught me that I cannot stop those problems from happening again.
I do the things I want to do, without paying much attention to how it affects my health condition(s).
When I am having problems managing my health condition(s), I keep it to myself (for example, do not tell my doctor, I miss appointments, or do not tell family or friends).
When I think about the problems that can happen because of poor health, then I want to do even more to take care of my health.
I would rather stay in bed than deal with problems that come up with my health.
I feel there is nothing I can do about problems that come up with my health.
Although I have had some problems with my health, I find myself still doing things that caused them (for example, unhealthy diet, unhealthy amount of exercise, smoking, or stress).
I know that what I do to take care of my health will make a difference.
If I see family or friends who have health problems do whatever they want, then it makes me go ahead and do what I want too.
If I really do not feel like doing things to control my health condition(s), then I choose not to do them.
When I am having a problem with my health, I try to forget all about it and go on like nothing is wrong.
If my family or friends have problems with their health, then I know that what happened to them is going to happen to me.
If it is too hard to stick with the treatment recommendations for controlling my health condition(s), then I do not dwell on finding ways to do it.
When I am having a problem with my health condition(s), I do the first thing that comes to mind rather than thinking through the options.
When I feel like there is nothing I can do about a problem with my health, I want to just lie down and go to sleep.
I decide how to handle everyday problems with my health based on what will be best for me in the long run—not what I might want today.
After I have a bad experience with my health condition(s), I come away knowing what to do and what not to do so the problem does not happen again.
I have used alcohol/drinking to try to escape dealing with my health problems.
Sometimes dealing with my health problems has felt so tough that I felt like I just wanted to die.
I tune out problems that come up with my health, like I am daydreaming.
I am able to figure out when problems are making my health condition(s) worse.
I get better and better at choosing the best way to solve problems with my health condition(s).
Scoring of HPSS subscales and total Scale:
Effective Problem Solving (EPS) = Item nos. 7, 9, 13, 20, 21, 24, 28, 44, and 49
Impulsive/Careless Problem Solving (IPS) = Item nos. 8, 12, 27, 30, 38, 39, 41, and 42
Avoidant Problem Solving (APS) = Item nos. 4, 25, 31, 33, 43, 46, and 48
Positive Transfer/Learning (PTR) = Item nos. 5, 16, 19, 45, and 50
Negative Transfer/Learning (NTR) = Item nos. 2, 3, 10, 14, 17, 23, 26, 29, 35, 37, and 40
Positive Motivation/Orientation (PMO) = Item nos. 1, 6, 18, 32, and 36
Negative Motivation/Orientation (NMO) = Item nos.11, 15, 22, 34, and 47
Reference
- 1.Coleman MT, Newton KS. Supporting self-management in patients with chronic illness. Am Fam Phys. 2005;72:1503–10. [PubMed]
- 2.Jerant AF, von Friederichs-Fitzwater MM, Moore M. Patients’ perceived barriers to active self-management of chronic conditions. Patient Educ Couns. 2005;57:300–7. [DOI] [PubMed]
- 3.Bodenheimer T, Lorig K, Holman H, Grumbach K. Patient self-management of chronic disease in primary care. JAMA. 2002;288:2469–75. [DOI] [PubMed]
- 4.US Institute of Medicine. Priority Areas for National Action: Transforming Health Care Quality. Washington, DC: National Academies Press; 2003. [PubMed]
- 5.Hill-Briggs F. Problem solving in diabetes self-management: a model of chronic illness self-management behavior. Ann Behav Med. 2003;25:182–93. [DOI] [PubMed]
- 6.Nezu AM, Nezu CM, Friedman SH, Faddis S, Houts PS. Helping Cancer Patients Cope: A Problem-Solving Approach. Washington, DC: American Psychological Association; 1998.
- 7.Glasgow RE, Toobert DJ, Barrera M Jr, Strycker LA. Assessment of problem-solving: a key to successful diabetes self-management. J Behav Med. 2004;27:477–90. [DOI] [PubMed]
- 8.Malouff JM, Thorsteinsson EB, Schutte NS. The efficacy of problem solving therapy in reducing mental and physical health problems: a meta-analysis. Clinical Psychology Review. 2007;27:46–57. [DOI] [PubMed]
- 9.Davies G, Koenig LJ, Stratford D, et al. Overview and implementation of an intervention to prevent adherence failure among HIV-infected adults initiating antiretroviral therapy: lessons learned from Project HEART. AIDS Care. 2006;18:895–903. [DOI] [PubMed]
- 10.Remien RH, Stirratt MJ, Dolezal C, et al. Couple-focused support to improve HIV medication adherence: a randomized controlled trial. AIDS. 2005;19:807–14. [DOI] [PubMed]
- 11.Williams JW Jr, Katon W, Lin EH, et al. The effectiveness of depression care management on diabetes-related outcomes in older patients. Ann Intern Med. 2004;140:1015–24. [DOI] [PubMed]
- 12.Mynors-Wallis L, Davies I, Gray A, Barbour F, Gath D. A randomised controlled trial and cost analysis of problem-solving treatment for emotional disorders given by community nurses in primary care. Br J Psychiatry. 1997;170:113–9. [DOI] [PubMed]
- 13.Heppner PP, Peterson CH. The development and implications of a personal problem-solving inventory. J Couns Psychol. 1982;30:537–45. [DOI]
- 14.D’Zurilla TJ, Nezu AM, Maydeu-Olivares A. Social Problem-solving Inventory-Revised (SPSI-R) Technical Manual. North Tonawanda, NY: Multi-Health Systems, Inc.; 2002.
- 15.Hayes JA, Black NA, Jenkinson C, et al. Outcome measures for adult critical care: a systematic review. Health Technol Assess. 2000;4:1– 111. [PubMed]
- 16.Ware JE Jr, Kemp JP, Buchner DA, Singer AE, Nolop KB, Goss TF. The responsiveness of disease-specific and generic health measures to changes in the severity of asthma among adults. Qual Life Res. 1998;7:235–44. [DOI] [PubMed]
- 17.Hill-Briggs F, Gary TL, Yeh HC, et al. Association of social problem solving with glycemic control in a sample of urban African Americans with type 2 diabetes. J Behav Med. 2006;29:69–78. [DOI] [PubMed]
- 18.Hill-Briggs F, Cooper DC, Loman K, Brancati FL, Cooper LA. A qualitative study of problem solving and diabetes control in type 2 diabetes self-management. Diabetes Educ. 2003;29:1018–28. [DOI] [PubMed]
- 19.Nunally JC, Bernstein IH. The assessment of reliability. Psychometric Theory, 3rd edn. New York: McGraw-Hill; 1994:248–92.


