Abstract
BACKGROUND
Current diabetes management guidelines offer blueprints for providers, yet type 2 diabetes control is often poor in disadvantaged populations. The group visit is a new treatment modality originating in managed care for efficient service delivery to patients with chronic health problems. Group visits offer promise for delivering care to diabetic patients, as visits are lengthier and can be more frequent, more organized, and more educational.
OBJECTIVE
To evaluate the effect of group visits on clinical outcomes, concordance with 10 American Diabetes Association (ADA) guidelines [American Diabetes Association, Diabetes Care, 28:S4–36, 2004] and 3 United States Preventive Services Task Force (USPSTF) cancer screens [U.S. Preventive Services Task Force, http://www.ahrq.gov/clinic/uspstf/resource.htm, 2003].
RESEARCH DESIGN AND METHODS
A 12-month randomized controlled trial of 186 diabetic patients comparing care in group visits with care in the traditional patient–physician dyad. Clinical outcomes (HbA1c, blood pressure [BP], lipid profiles) were assessed at 6 and 12 months and quality of care measures (adherence to 10 ADA guidelines and 3 USPSTF cancer screens) at 12 months.
RESULTS
At both measurement points, HbA1c, BP, and lipid levels did not differ significantly for patients attending group visits versus those in usual care. At 12 months, however, patients receiving care in group visits exhibited greater concordance with ADA process-of-care indicators (p < .0001) and higher screening rates for cancers of the breast (80 vs. 68%, p = .006) and cervix (80 vs 68%, p = .019).
CONCLUSIONS
Group visits can improve the quality of care for diabetic patients, but modifications to the content and style of group visits may be necessary to achieve improved clinical outcomes.
KEY WORDS: group visits, guideline concordance, type 2 diabetes control
BACKGROUND
Over 18 million people in the United States have diabetes mellitus (DM),1 costing an estimated $132 billion in 2002.2 Clinical practice guidelines, with measurable process-of-care indicators (e.g., periodic monitoring of HbA1c and LDL levels) and preventive services (e.g., foot examinations, vaccinations, and cancer screens) facilitate management of patients with type 2 DM. The typical 10 minute primary care visit provides little time to address the up to 11 recommendations for type 2 diabetes, much less the 24.5 recommendations for the 15.4 risk factors with which the average patient presents.3 The group visit model developed in managed care to improve efficiency and throughput of patients may provide an efficient way to improve process-of-care delivery.4 A recent article suggested group visits as a strategy to address adherence to guidelines.5
Group visit literature remains relatively sparse, with only 5 articles reporting on randomized controlled trials.4–8 Two studies have shown group visits to be less costly and have equal or better quality4,5; 1 study demonstrated 4 years of improved control in type 2 diabetic patients.6 Studies in disadvantaged patient populations are limited with the only reported study by our own group.5 This 6-month pilot study showed a trend towards improved clinical outcomes and better adherence to ADA process-of-care indicators in group visit patients compared to regular care. The study was limited due to only 1 physician leading group visits and the study duration being too short to impact clinical outcomes. Thus, we designed the current study with more patients, multiple providers, and longer duration (12 months) to more definitively evaluate the effectiveness of group visits in terms of quality of care and clinical outcomes in disadvantaged patients with type 2 diabetes.
RESEARCH DESIGN AND METHODS
Study Population
This study was conducted at the Adult Primary Care Center (APCC), Medical University of South Carolina (MUSC), serving approximately 6,000 predominantly minority, inadequately insured patients in Charleston, SC. Ten academic internal medicine faculty physicians see patients and supervise residents, nurse practitioners, physician assistants, and students. Eligible patients aged >18 years with poorly controlled diabetes mellitus (HbA1c > 8.0%) were identified through a query of the APCC electronic medical record. All subjects signed written informed consent documents approved by the MUSC Institutional Review Board. Exclusion criteria included: primary diagnosis of substance abuse or dependence; current pregnancy; dementia; and inability to hear, speak English, or obtain transportation to the clinic. One of 5 consistent interviewers invited identified patients to participate through telephone or on-site solicitation using a standardized script.
Power, Sample Size, and Randomization
The primary outcome was adherence to 10 American Diabetes Association (ADA) guidelines for diabetic care. The effect size of interest was a 0.15 difference in the adherence rate, obtained from the pilot study conducted by the group5; 186 subjects were required for a power of 80% at alpha of 0.05 to detect this difference after adjusting for possible dropouts and crossovers. Subjects meeting criteria for inclusion into the study were randomized after informed consent and baseline data collection using randlst software (http://odin.mdacc.tmc.edu/anonftp/) allowing for stratification and blocking. Subjects were stratified by race and gender using a block size of 4.
Intervention Condition
Group visits, co-led by 1 of 6 primary care internal medicine physicians and 1 of 3 registered nurses in the clinic, were modeled after those of the Cooperative Health Care Clinics (CHCC) developed by Beck and Scott.4 After reviewing pertinent literature and the CHCC orientation manual, participating physicians and nurses received onsite training by a senior internist who previously conducted group visit training. Additionally, the previous coordinator/trainer for CHCC providers and staff conducted a 3-hour educational session for clinic staff members.
Patients randomized to group visits were divided into 6 cohorts consisting of 14–17 patients each. The cohorts met monthly for 1 year on a different floor in the same building as the clinic. One-on-one visits were available for care needed between scheduled group visits or for specific medical needs not amenable to group visits (e.g., Papanicolaou (PAP) smears, abdominal exams, EKGs). Group visits were scheduled for 2 hours: 10–15 minutes for “warm-up” and socialization, 30–45 minutes for an interactive discussion of a health-related topic such as foot care or health eating strategies, and 60 minutes for one-on-one consultations with the physician. While vaccinations, foot exams, medication adjustments, laboratory orders, and referrals for retinal examinations could be done in the group visits, mammograms and PAP smears were scheduled separately. Group visit content, though patient-guided, was physician-directed to cover educational topics included in the core curriculum of Sadur et al.7 such as nutrition, exercise, foot care, medications, complications of diabetes, and the emotional aspects of diabetes.
Control Condition
Control patients received care in the clinic as usual, seeing faculty or resident physicians, physician assistants, nurse practitioners, or medical or physician assistant students with access to a dietician and diabetes educator. The volume of patients at the APCC, the clinic structure, and scheduling of patients does not provide for consistency in patients’ providers at each visit, with patients needing to be seen off schedule likely seeing providers other than their own.
Data Collection
Data were collected at baseline, 6 months, and 12 months. Research assistants, blind to study assignment, scheduled patients by mail and phone for data collection appointments and assisted those who needed help. Data collected included HbA1c levels, lipid profiles (total cholesterol, HDL, LDL, triglycerides), and blood pressures. Blood samples and blood pressures were collected by trained dedicated personnel blinded to patient assignments. Three BP readings were measured per subject while sitting upright after 5 minutes of rest 2 minutes apart.9 All blood samples were sent to the same laboratory for processing. Patients received modest compensation for transportation and time at each data collection point. Neither group of patients received any compensation for actual medical care though the visit deposit fee for group patients was $15/visit as compared to $45/visit for control patients. The cost of the 12 scheduled group visits (at $15/visit) was identical cost-wise to the guideline recommended quarterly visits for diabetic patients ($45/visit).
Upon study completion, medical records were blindly abstracted for the 10 ADA process-of-care indicators [>2 yearly HgA1cs,10,11 at least yearly cholesterol levels, treatment for LDL cholesterol levels >100 mg/dl, yearly ophthalmologic referrals, influenza vaccinations, foot exams, and checks for microalbuminuria, ACE-inhibitor or ARB use, daily aspirin (81 mg) unless contraindicated, and at least 1 pneumococcal vaccine] and 3 cancer screens recommended by the United States Preventive Services Task Force (USPSTF) including hemoccult cards for colon cancer screening in patients >50 years old,12 mammograms for breast cancer in women age 50–69 years, and PAP smears for cervical cancer screening at least every 3 years in women with previously normal PAP smears and intact uteri (more frequently if previous abnormal cytology).
Statistical Methods
Data were analyzed using the intention-to-treat principle once randomized and baseline parameters were recorded. The t test for continuous outcomes and nonparametric Wilcoxon rank sum test for ordinal outcomes were used to compare differences between group visit and control conditions. For process-of-care indicators, all patients randomized were analyzed. Clinical data (HbA1c, cholesterol, and blood pressure levels) for patients whose loss to follow-up was independent of treatment effect had their last observations carried forward in the analysis. Patients who were lost to follow-up with no available information had their missing observations replaced with the worst observations in their respective treatment groups.
Statistical analysis was performed in 2 levels. The first level was a cross-sectional analysis comparing group differences at each data collection point. Depending on the type of outcome (continuous or discrete), t test, Fisher’s exact test, or nonparametric Wilcoxon rank sum test was used to compare baseline characteristics between the 2 groups. Linear regression models were used for 6- and 12-month data adjusting for baseline covariates (such as the baseline clinical outcome measures, age, gender, race, educational level, reading level, and insurance type). The second level was longitudinal modeling analyzing data from all 3 data collection points. Mixed-effects models were used to fit the longitudinal data. Each model adjusted for baseline covariates, the dependency among repeated measures from the same subject, and the heterogeneity among different subjects. Initially, the mean number of the 10 ADA process-of-care indicators met in both groups was compared. These data were further dichotomized by classifying whether there was compliance with at least 3 items, 4 items, etc. The proportions of patients who met these criteria were presented and tests for 2 proportions from binary outcomes were performed to compare treatment differences. SAS 9.1 was used for all computations.
Results Over a 24-week period from September 2002 to February 2003, 506 patients whose last HbA1c level was >8.0% were contacted by phone or on-site, 186 of whom met criteria for inclusion into the study, agreed to participate, signed informed consent, and completed baseline assessments. Reasons for not participating were inability to make the baseline data collection appointment, and transportation issues. Of enrolled patients, 96 subjects were assigned to group visits and 90 to usual care. One patient in the control group died from unknown causes, and 2 group visit patients died during the study (1 from adenocarcinoma of unknown primary and the other from severe electrolyte anomalies due to recently diagnosed DiGeorge syndrome). Of the 27 patients who withdrew (13 control and 14 intervention patients), all but 1 indicated a reason. Missing data for those who withdrew from the study but continued to receive care at the clinic and had HbA1c levels unchanged or better than their last study obtained data (2 in intervention and 5 in control) were replaced by their last study observation in the analysis. Thus, we conservatively analyzed data that were the same as or worse than their new clinic data. For withdrawn patients about whom no information for withdrawal was given (2 in intervention and 5 in control), and for the patient who died before the study began but after collection of baseline data (1 intervention patient), worst observations for their treatment group were carried forward—again, a conservative approach to missing data.
Demographic variables were well balanced between patients randomized to group visits or usual care at baseline (Table 1). For all subjects in the study, the average age was 56.1 years, 72% were female, 82.8% African American, and 33% married at the time of the study. The mean self-reported educational level for these patients was 10 years with an average Rapid Estimate of Adult Literacy (REALM) Tool health literacy level of 6th grade.13 Most patients had Medicaid or Medicare; 28% were uninsured; and 26% reported working. Clinical variables were also well balanced at baseline (Table 1) with a mean HgbA1c level at baseline of 9.3% for group patients and 8.9% for control patients. The mean total cholesterol level for group patients was 193.4 and 196.1 mg/dl for control patients. Blood pressures, triglycerides, LDL, and HDL levels showed no significant baseline differences between the 2 groups.
Table 1.
Comparison of Sociodemographic Factors at Baseline
| Variable | Group | Control | P value |
|---|---|---|---|
| Number of patients | 96 | 90 | |
| Gender (F)(%) | 74 | 70 | 0.55 |
| Race (B)(%) | 82 | 84 | 0.69 |
| Marital status | |||
| Single | 30 | 32 | |
| Married | 36 | 30 | |
| Divorced | 11 | 10 | |
| Separated | 13 | 8 | |
| Widowed | 9 | 20 | 0.25 |
| Current tobacco use | 20 | 19 | 0.88 |
| Employment | |||
| Full-time | 13 | 21 | |
| Part-time | 10 | 8 | |
| Retired | 16 | 16 | |
| Unemployed | 59 | 54 | 0.46 |
| Age (years) | 55 | 57 | 0.126 |
| HbA1c (%) | |||
| Baseline | 9.3 ± 0.202 | 8.9 ± 0.223 | 0.193 |
| 6 months | |||
| 12 months | 9.1 ± 0.224 | 9.0 ± 0.260 | 0.688 |
| LDL (mg/dl) | |||
| Baseline | 110.6 ± 4.67 | 116.2 ± 4.75 | 0.397 |
| SBP mmHg | |||
| Baseline | 137 ± 2.33 | 132 ± 2.97 | 0.261 |
| DBP mmHg | |||
| Baseline | 77.3 ± 1.11 | 75.5 ± 1.72 | 0.377 |
Unadjusted analysis (Table 2) comparing patients in group visits to usual care showed group visit patients more likely to have had each of the ADA processes of care indicators, with use of ACEI/ARB and ASA, pneumovax, flu shot, foot examination, and ophthalmology referrals significantly better on an individual level. During the 1-year study, group patients were more likely to have had more of the 10 ADA process-of-care indicators (Fig. 1). More group patients had 3 or more process items met than control patients (p = .0312), a difference remaining highly significant (with all p > .0001) with the cut point moved from 3 to 7, 8, 9, or 10 items. For example, 64 intervention patients (68.4%) had at least 8 process-of-care indicators performed compared to 24 control patients (29.3%) (p > .0001); 41 intervention patients (64.1%) had at least 9 process-of-care indicators performed as compared to only 9 control patients (11%) (p > .0001); and 17 intervention patients (17.7%) and no control patients had all 10 process-of-care indicators performed (p > .0001). Combining all indicators, the mean number of criteria met in intervention patients was 7.93 ± 0.18 vs. 6.13 ± 0.22 in control patients (unadjusted p > .0001). A 2-sample Wilcoxon rank sum test also resulted in p > .0001. Significance persisted after controlling for selected covariates including intensity of care assessed by the number of primary care visits, and the number of comorbid risk factors. Women participating in group visits were significantly more likely to meet adherence to guidelines for PAP smears and screening mammograms; neither sex was more likely to meet adherence guidelines for colon cancer screening.
Table 2.
Unadjusted Comparison of Individual Process-of-care Variablesa
| Variable (%) | GV | UC | P value |
|---|---|---|---|
| ACEI/ARB | 89 | 64 | 0.0004 |
| Aspirin | 81 | 48 | <0.0001 |
| Chol. meas. | 79 | 61 | 0.0815 |
| Chol. treated | 76 | 59 | 0.1246 |
| HbA1c | 79 | 62 | 0.1193 |
| Microalbumin | 42 | 33 | 0.5119 |
| Pneumovax | 78 | 49 | 0.0004 |
| Influenza vaccine | 74 | 46 | 0.0008 |
| Foot examination | 65 | 28 | <0.0001 |
| Eye examination | 75 | 53 | 0.0171 |
aAnalysis by chi square
Figure 1.
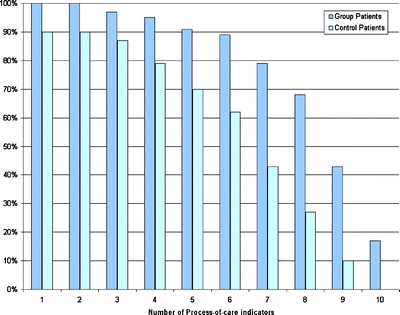
Process-of-care indicator adherence comparisons.
Data analyzed from group visits only revealed significant differences in ADA criteria met between the different physicians conducting groups. The estimated intracluster correlation coefficient (ICC) of the ADA criteria met is 0.25 (95% CI: 0.21, 0.29), indicating the ADA criteria met by subjects seen in the same physician group (within cluster) were more similar than the criteria met between subjects seen by different physicians groups (between cluster).
At 12 months both intervention and control patients had varying total cholesterol, triglyceride, LDL, and HDL levels, though none were significant. After examining data from all 3 visits, longitudinal mixed-effects models were fitted for each of the 5 clinical outcomes (HgbA1c. cholesterol, TG, HDL, and LDL). All models were adjusted for number of ADA criteria met, educational levels, health literacy levels, race, gender, insurance types, and interactions between any 2 of these covariates. Any interaction not found to be significant was dropped, and the model was fitted again. No significant treatment effects were found for any of these 5 clinical outcomes (p values range from 0.11 to 0.88). Repeat analysis using per protocol data gave similar results.
DISCUSSION
This study reveals significant differences between group visit (intervention) and control patients in adherence to ADA standards of care and guidelines for PAP smears and screening mammograms.10,12 Perhaps the longer duration of group visits provides more time to address guidelines than a typical primary care encounter. Additionally, providers can deliver consistent messages to multiple patients simultaneously in group visits, rather than repeating them individually to multiple patients. Monthly appointments provide more frequent contact with the physician increasing opportunities to systematically address guidelines. These findings support those from previous studies revealing more frequent primary care visits to be associated with an increased likelihood of diabetic patients having >2 HbA1c levels performed annually.11 Our study refutes results from previous studies suggesting women attending more frequent general internal medicine visits have a higher likelihood of receiving recommendations for mammograms without improved patient adherence14; group visit women had higher rates of adherence to guidelines for breast and cervical cancer screening.
Though group patients had more overall primary care visits, due to the group visits being scheduled monthly, they averaged 1.0 individual primary care visits over the year compared with 3.8 for control patients. Physicians and patients accepted group visits as physicians continued to schedule groups and patients continued to attend groups after the study period. Furthermore, the show rate for group visits was similar to that for the clinic.
Discussion of individual patient issues in groups may have contributed to other patients’ accepting process-of-care referrals and tests, from diminished anxiety and a desire to show other group members’ commitment to their own health care. With open general discussions in group visits, patients potentially educate each other about referrals and tests experienced; perhaps hearing information from their peers resulted in higher acceptance of suggestions from the physicians.
The direct effects of the education at each group visit are difficult to assess from this study, but improvement in concordance with process-of-care indicators in group patients compared with control patients suggests significant effects. Differences in the number of ADA criteria met by patients seen in groups led by different physicians suggest physician methodologies may have affected group teaching skills and educational topics selected, or there were differences in group dynamics affecting their approach to guideline adherence
Patients’ financial limitations likely led to significant differences in blood sugar, lipid, or blood pressure control, by prohibiting purchase of prescribed medications, thus creating a ceiling effect for benefits of improved guideline adherence. Lack of standardization of group visit content may also have contributed, as providers approached educational topics individually. Perhaps a manualized, consistent curriculum would improve clinical outcomes. The low health literacy level of most of the study patients and the lack of physicians’ awareness of their health literacy levels may have contributed to the lack of clinical outcomes. As group visits were conducted under the control of the providers, positive results (more process-of-care indicators met) were also under the providers’control. Clinical outcomes were under the patients’ control, depending on them following lifestyle guidelines and adhering to medication regimens. Incorporating motivational and behavioral strategies emphasizing patients’ daily responsibilities and skill building for healthy lifestyles compatible with diabetes may affect improvements in clinical outcomes. Also, the study may have lacked enough power to show a significant difference in the outcome clinical variables because the sample size was calculated to detect a difference in proportion of ADA processes of care met by those in group visits compared to usual care.
Six different providers conducting group visits strengthens in this study. These providers also had patients in the usual care arm as part of the general pool of clinic patients; thus, it is possible through contamination that providers may have adopted some of the group visit strategies (e.g., group visit educational content) for control patients. While unlikely, the time constraints of a typical primary care visit may have contributed to the failure to determine a difference in clinical outcome variables. Provider randomization to prevent contamination is unrealistic as it is unlikely in any practice that a provider would deliver care only in group visits.
CONCLUSION
This study of group visits in disadvantaged patients with type 2 diabetes reveals significant improvements in process-of-care indicators for diabetes and sex/age appropriate cancer screening without differences in medical outcomes. Those who conduct and study group visits may need to consider modifications to improve clinical outcomes while maintaining the gains made in guideline concordance and efficiency of care delivery.
Acknowledgement of Financial and/or Other Support
This project was supported by grant number 5 P01 HS10871 from the Agency for Healthcare Research and Quality, a grant from The Robert Wood Johnson Foundation, Princeton, New Jersey, and 1R21NS043569 from National Institutes of Health/NINDS.
Conflict of Interest Dr. Magruder, and Mr. Yeager reported receiving a $7,500 grant from Pfizer.Drs. Clancy, Magruder and Mr. Yeager received a $107,445 grant from Eli Lilly in 2005–2006. Dr. Magruder was the principal investigator.The other authors reported no conflicts of interest.
References
- 1.Centers for Disease Control and Prevention. National diabetes fact sheet, United States, 2003. Atlanta, GA, U.S. Department of Health and Human Services, Centers for Disease Control and Prevention; 2003.
- 2.American Diabetes Association. Economic costs of diabetes in the U.S. in 2002. Diabetes Care. 2003;26:917–32. [DOI] [PubMed]
- 3.Hofer TP, Zemencuk JK, Haywar RA. When there is too much to do: how practicing physicians prioritize among recommended interventions. J Gen Intern Med. 2004;19:646–53. [DOI] [PMC free article] [PubMed]
- 4.Beck A, Scott J, Williams C, et al. Cooperative health care clinics: a group approach to individual care. JAGS. 1997;45:543–9.
- 5.Clancy DE, Cope DW, Magruder KM, Huang P, Wolfman T. Evaluating concordance to American diabetes association standards of care for type 2 diabetes through group visits in an uninsured or inadequately insured patient population. Diabetes Care. 2003;26:2032–6. [DOI] [PubMed]
- 6.Trento M, Passera P, Borga E, et al. A 5-year randomized controlled study of learning, problem solving, and quality of life modifications in people with type 2 diabetes managed in group care. Diabetes Care. 2004;27:670–5. [DOI] [PubMed]
- 7.Sadur CN, Moline N, Costa M, et al. Diabetes management in a health maintenance organization. Diabetes Care. 1991;12:2011–7. [DOI] [PubMed]
- 8.Wagner EH, Grothaus LC, Sandhu N, et al. Chronic care clinics for diabetes in primary care: a system-wide randomized trial. Diabetes Care. 2001;24(4):695–700. [DOI] [PubMed]
- 9.Chobanian AV, Bakris GL, Black HR, et al. and the National High Blood Pressure Education Program Coordinating Committee. Seventh report of the joint National Committee on prevention, detection, evaluation, and treatment of high blood pressure. Hypertension. 2003;42:1206–52. [DOI] [PubMed]
- 10.American Diabetes Association. Standards of medical care for patients with diabetes mellitus (position statement). Diabetes Care. 2004;28:S4–36. [DOI]
- 11.Mayberry RM, Davis T, Alema-Mensah E, Samadi AR, Finley R, Jones A. Determinants of glycemic status monitoring in Black and White Medicaid beneficiaries with diabetes mellitus. J Health Care Poor Underserved. 2005;16(4 Suppl A):31–49. [DOI] [PubMed]
- 12.U.S. preventive services task force. Preventive Services Resource Links. Agency for healthcare research and quality, Rockville, MD. September 2003.Available from http://www.ahrq.gov/clinic/uspstf/resource.htm. Accessed 15 June, 2005.
- 13.Davis TC, Long SW, Jackson RH. Rapid estimate of adult health literacy in medicine: a shortened screening instrument. Fam Med. 1993;25:391–395. [PubMed]
- 14.May DS, Kiefev CI, Funkhouser E, Fouad MN. Compliance with mammography guidelines: physician recommendation and patient adherence. Prev Med. 1999;28(4):386–94. [DOI] [PubMed]


