Abstract
BACKGROUND
The University of California, Los Angeles (UCLA)/Charles R. Drew University Medical Education Program was developed to train physicians for practice in underserved areas. The UCLA/Drew Medical Education Program students receive basic science instruction at UCLA and complete their required clinical rotations in South Los Angeles, an impoverished urban community. We have previously shown that, in comparison to their UCLA counterparts, students in the Drew program had greater odds of maintaining their commitment to medically disadvantaged populations over the course of medical education.
OBJECTIVE
To examine the independent association of graduation from the UCLA/Drew program with subsequent choice of physician practice location. We hypothesized that participation in the UCLA/Drew program predicts future practice in medically disadvantaged areas, controlling for student demographics such as race/ethnicity and gender, indicators of socioeconomic status, and specialty choice.
DESIGN
Retrospective cohort study.
PARTICIPANTS
Graduates (1,071) of the UCLA School of Medicine and the UCLA/Drew Medical Education Program from 1985–1995, practicing in California in 2003 based on the address listed in the American Medical Association (AMA) Physician Masterfile.
MEASUREMENTS
Physician address was geocoded to a California Medical Service Study Area (MSSA). A medically disadvantaged community was defined as meeting any one of the following criteria: (a) federally designated HPSA or MUA; (b) rural area; (c) high minority area; or (d) high poverty area.
RESULTS
Fifty-three percent of UCLA/Drew graduates are located in medically disadvantaged areas, in contrast to 26.1% of UCLA graduates. In multivariate analyses, underrepresented minority race/ethnicity (OR: 1.57; 95% CI: 1.10–2.25) and participation in the Drew program (OR: 2.47; 95% CI: 1.59–3.83) were independent predictors of future practice in disadvantaged areas.
CONCLUSIONS
Physicians who graduated from the UCLA/Drew Medical Education Program have higher odds of practicing in underserved areas than those who completed the traditional UCLA curriculum, even after controlling for other factors such as race/ethnicity. The association between participation in the UCLA/Drew Medical Education Program and physician practice location suggests that medical education programs may reinforce student goals to practice in disadvantaged communities.
KEY WORDS: medical education, health care disparities, UCLA/Drew program
INTRODUCTION
Maldistribution of physicians persists throughout the United States, with an estimated 20% of the population living in federally designated Health Professional Shortage Areas (HPSAs).1 Strategies to alleviate physician shortages usually fall into one of three categories: applicant pool, medical education, and practice environment.2 Prior research has identified potentially favorable applicant characteristics, such underrepresented minority race/ethnicity,3–5 growing up poor6 or in an underserved area,3,7 participation in the National Health Service Corps,3 interest before medical school,3 and older age.8 However, it is not known whether the second strategy, medical education, can successfully translate this knowledge into changes in the physician workforce.
Rural education programs, particularly the Physician Shortage Area Program (PSAP) of the Jefferson College of Medicine, have shown the greatest success in producing physicians for rural areas.9,10 PSAP graduates are more likely to become rural family practitioners than other Jefferson students with similar backgrounds.10 Less is understood about the efficacy of medical programs that hope to relieve inner-city and minority populations. Traditionally black colleges such as Howard and Meharry have shown that in comparison to other black physicians, their graduates care for larger numbers of black patients, but not necessarily other disadvantaged groups.5,11 Direct comparisons to other minority groups or their own nonblack graduates have not been conducted.12,13
The UCLA/Drew Medical Education Program was developed under the mission of the Charles R. Drew University of Medicine and Science “to conduct education and research in the context of community service in order to train physicians and allied health professionals to provide care with excellence and compassion, especially to underserved populations.” A joint effort of the Charles R. Drew University of Medicine and Science (“Drew”, hereafter) and the David Geffen School of Medicine at the University of California, Los Angeles (UCLA), the program has selected applicants since 1981 for their commitment to this mission. In a survey of the 1996–2002 graduates, the percentage of UCLA/Drew students planning to practice in underserved areas increased from 68.5% at matriculation to 86% upon graduation. In contrast, traditional UCLA graduates with similar intentions decreased from 28% at matriculation to 20% at graduation.14 These differences remained after controlling for race, ethnicity, and other sociodemographic characteristics. The maintenance of Drew student commitment indicates program’s success in nurturing students’ goals throughout medical school.
The long-term effects of the program on eventual practice location have not been well characterized. Barnhart et al. surveyed the classes from 1985–1987 and found that Drew and minority graduates are more likely to practice in federally designated shortage areas, but neither association demonstrated statistical significance.15 However, this survey was restricted by its small sample size, absence of socioeconomic and demographic controls, and limited outcome measure.
In this study, we determined the locations of graduates from the first 10 years of the UCLA/Drew Program and their UCLA counterparts who are currently practicing in California. Practice locations were assessed for the predominance of disadvantaged populations and geographic designation of physician shortage. We examined the association between graduation from UCLA/Drew and practicing in a disadvantaged community, incorporating student demographics, socioeconomic status, and specialty choice predictors. We hypothesized that when controlling for premedical and educational factors, participation in the UCLA/Drew program predicts future practice in medically disadvantaged areas.
METHODS
Respondents
The study sample consisted of graduates of the UCLA School of Medicine and the UCLA/Drew Medical Education Program from 1985 to 1995, with a self-reported mailing address in California listed in the American Medical Association (AMA) Physician Masterfile in 2003. As residency and fellowship training may extend 7–10 years following graduation, we chose graduates from 1985–1995 to evaluate physicians who have had sufficient time to complete their education and choose a practice setting.
Data Sources
We conducted a retrospective analysis of secondary data collected by the Association of American Medical Colleges (AAMC) and the 2003 American Medical Association (AMA) Physician Masterfile. The student data were obtained from AAMC biographical files and the Prematriculation Questionnaire (PMQ). The PMQ is administered with the Medical College Admissions Test, before a student’s admission and matriculation into medical school. The AMA Masterfile information was then linked to the AAMC data by unique identifiers.
Physicians’ preferred mailing addresses were geocoded to a California Medical Service Study Area (MSSA), as described by Grumbach, et al.16 The sample was restricted to physicians currently practicing in California. Although there have been efforts to develop a standardized set of rational physician service areas throughout the US, these methods are still in the process of being validated.17 Moreover, definitions of disadvantaged areas—such as those used in this study—that categorize communities on the basis of minority resident population and household income are difficult to standardize across states (as opposed to within states) because of the wide variation across states. Those physicians with an address in California (67.9% of all graduates of both programs) were geocoded to a California Medical Service Study Area (MSSA).16 Data on the race/ethnicity and mean household income of the populations residing in each MSSA were obtained from the 2000 Census. The use of these archived data for research purposes was approved by the institutional review boards of both UCLA and Drew.
Outcome Variables
A medically disadvantaged MSSA was defined as meeting any one of the following criteria: (a) federally designated primary care Health Professional Shortage Area (HPSA) or Medically Underserved Area (MUA); (b) rural area; (c) high minority area; or (d) high poverty area. The State of California classifies an MSSA as “rural” if it has a population density less than 250 residents per square mile and contains no city with a population of 50,000 residents or greater. An area was defined as “high minority” if the percentage of African-American or Latino residents was greater than or equal to the 85th percentile of all areas for the state.4 An MSSA was coded as “high poverty” if the mean household income was in the lowest quartile of mean incomes for the state.4
Predictor Variables
Independent variables were chosen for their association with an intent to practice in underserved areas in prior studies.3–5, 7
Demographics Demographic variables were obtained from the AAMC biographical file. We included age at matriculation as a continuous variable. We dichotomized race/ethnicity into underrepresented minority groups (URM) and non-URM. Underrepresented minority groups were defined in accordance with the Association of American Medical Colleges policy during the study period: African American, Latino/Hispanic, and Native American/Alaskan/Hawaiian.18
Social Background Social background variables were collected from the PMQ. Parent education was categorized as: high school degree or less; some college or post-high school vocational training; college (4-year) degree; graduate or professional education. Parent employment was categorized as: professional/managerial/owner or not, to differentiate between occupations with relative affluence and those associated with lower socioeconomic status levels. We included high school community as a measure of where applicants spent at least some of their formative years. This variable was categorized into three types: urban, suburban, or rural area. State of origin was dichotomized as California versus non-California at the time of application.
Medical Education Medical education program was categorized as enrollment in the UCLA School of Medicine or the UCLA/Drew Medical Education Program. We also included year of graduation to address potential secular trends.
Specialty Physician specialty was dichotomized as primary care versus non-primary care. Primary care specialties included Family Medicine, General Internal Medicine, General Pediatrics, and Obstetrics And Gynecology.Although we have shown intent at matriculation to practice in an underserved community predicts student intent at graduation,14 this variable was not part of the Matriculation Questionnaire (MQ) until 1991, such that we were only able to obtain responses from 1994–1995 graduates. Similarly, we have demonstrated an association between intent at graduation and subsequent practice in underserved areas,14 but the graduation intent variable was assessed by the Graduation Questionnaire (GQ), for which the data were not complete until the class of 1996. Given our preference to focus on post-training physicians who have had time to settle into practice, we deemed that these recent graduates would not be appropriate for study.
STATISTICAL ANALYSIS
Bivariate analyses were performed to examine relationships between the predictor variables and the outcomes of interest, and odds ratios with 95% confidence intervals were calculated. We used the chi-squared test for categorical variables and t-tests for continuous variables.
In an assessment of potential multicolinearity, none of the variables had correlation greater than 0.70, the strongest being between father’s education and occupation (r = .52). We then fit two multivariate logistic regression models to estimate the association of the UCLA/Drew program with practice in underserved areas, in the context of previously identified predictors. Independent variables were included if they were associated with the outcome in bivariate analyses, or if previous literature review suggested they may be important for their content.3–5,7
We fit two regression models because the missing PMQ data led to a reduction in sample size of 37% (i.e., from 1,047 to 672 observations). For the first analysis (“model 1”), social background variables from the PMQ were excluded. In the second analysis (“model 2”), social background variables were added.
To assess potential interactions, we tested product terms of the UCLA/Drew program with URM race/ethnicity, gender, age, and parental education and occupation. We identified no significant interactions in multivariate analysis, and these terms were not included in the final models.
Although the proportions lost to follow-up because of out-of-state relocation for the Drew and UCLA graduates were not different (72.3% and 67.8%; P = .239), we performed a sensitivity analysis to assess the impact of different assumptions about the locations of the two groups on the results.
SPSS 11.0 for Windows and Mac OSX were used to perform statistical analyses.
RESULTS
The AMA Physician Masterfile lists records for 1,706 UCLA and UCLA/Drew graduates from 1985 through 1995. Slightly over two-thirds (N = 1,159) have remained in California. Of these physicians, 7.6% (n = 88) were excluded because they were listed as inactive, retired, or still in residency/fellowship training. Characteristics of the resulting 1,071 graduates are shown in Table 1. Eighty-eight percent graduated from the UCLA SOM, and 11.9% (N = 127), from the UCLA/Drew program. Twenty-three percent are underrepresented minorities (URM). Somewhat less than half (44.2%) are practicing in a primary care specialty.
Table 1.
Social, demographic, and practice characteristics of the 1985–1995 graduates of the UCLA/Drew Medical Education Program and the UCLA School of Medicine, practicing in California in 2003 (N = 1,071)
| Variable | Percent (%) | Number (N) | |
|---|---|---|---|
| Age | |||
| Mean (years) | 22.8 | ||
| Gender | |||
| Male | 62.0 | 660 | |
| Female | 38.0 | 405 | |
| Minority status | |||
| Non-URM* | 76.9 | 814 | |
| URM* | 23.1 | 244 | |
| State of origin | |||
| All other | 6.1 | 65 | |
| California | 93.9 | 1,003 | |
| Year of graduation | |||
| 1985 | 9.5 | 102 | |
| 1986 | 10.4 | 111 | |
| 1987 | 9.8 | 105 | |
| 1988 | 9.4 | 101 | |
| 1989 | 10.5 | 112 | |
| 1990 | 8.8 | 94 | |
| 1991 | 8.6 | 92 | |
| 1992 | 9.2 | 98 | |
| 1993 | 8.3 | 89 | |
| 1994 | 7.4 | 79 | |
| 1995 | 8.1 | 86 | |
| Medical school program | |||
| UCLA | 88.1 | 942 | |
| UCLA/Drew | 11.9 | 127 | |
| Mother’s level of education | |||
| High School or less | 29.3 | 262 | |
| Some college/ Business /Technical training | 23.2 | 208 | |
| College degree | 19.9 | 178 | |
| Graduate or professional work | 27.6 | 247 | |
| Father’s level of education | |||
| High School or less | 16.8 | 180 | |
| Some college/ Business /Technical training | 13.7 | 122 | |
| College degree | 19.0 | 169 | |
| Graduate or professional work | 47.1 | 420 | |
| Father’s occupation | |||
| Nonprofessional/manager | 22.6 | 160 | |
| Professional/Owner/Manager | 77.4 | 549 | |
| Mother’s occupation | |||
| Nonprofessional/manager | 57.9 | 407 | |
| Professional/Owner/Manager | 42.1 | 296 | |
| High school community | |||
| Type | Suburban: large and moderate size cities | 35.9 | 323 |
| Urban: large and moderate size cities | 49.0 | 441 | |
| Rural area to small city | 15.1 | 136 | |
| Specialty area | Non-primary care | 55.8 | 598 |
| Primary care | 44.2 | 473 | |
*URM Underrepresented minority
Practice in Medically Disadvantaged Areas
Twenty-nine percent of active graduates are located in one of the types of medically disadvantaged areas (MDAs, Table 2). Of these physicians, 38.7% are listed in federally designated HPSAs, while 31.6% are in high poverty areas. Only 16.8% practice in rural areas. Many practice in minority communities, with 51% in high black areas and 33% in high Hispanic/Latino areas. The total of the frequencies of each outcome exceeded 100% because 27% of graduates are located in an area that met multiple criteria for the disadvantaged designation.
Table 2.
Graduates Of The UCLA/Drew Medical Education Program And The UCLA School Of Medicine, 1985–1995: Practice In Medically Disadvantaged Areas In California* (N = 1,062)†
| Outcome variable | Total | UCLA/Drew | UCLA | P |
|---|---|---|---|---|
| Percentage (%) (No) | Percentage (%) (No) | Percentage (%) (No) | ||
| (1,062) | (124) | (938) | ||
| Any medically disadvantaged area (rural, high minority, high poverty, or HPSA/MUA) | 29.2 (310) | 53.2 (66) | 26.1 (244) | <.001 |
| HPSA/MUA | 11.2 (120) | 22.0 (28) | 9.8 (92) | <.001 |
| High poverty area | 9.2 (98) | 17.5 (22) | 8.1 (76) | .001 |
| High Black area | 14.8 (158) | 28.6 (36) | 12.9 (121) | <.001 |
| High Hispanic/Latino area | 9.7 (103) | 19.8 (25) | 8.3 (78) | <.001 |
| Rural area | 4.9 (52) | 4.0 (5) | 5.0 (47) | .607 |
Note that percent (%) do not total 100% because of multiple designations.
*Defined as: (a) any medically disadvantaged area (rural, HPSA, high poverty or high minority); (b) Health Professions Shortage Area (HPSA); (c) high poverty area (average income below 25th percentile for state); (d) high black area (above state 85th percentile); (e)High Hispanic/Latino area (above state 85th percentile); and (f) Rural area.
†Missing 0.8% (9/1,071): no MSSA (Medical Service Study Area) designation available
Graduates of the UCLA/Drew Program
Over 50% of UCLA/Drew graduates are located in MDAs, in contrast to 26.1% of UCLA graduates (Table 2). This association remained consistent for both URM and non-URM physicians (Fig. 1) and across all types of disadvantaged areas, with the exception of rural areas (Table 2). Compared with their UCLA counterparts, UCLA/Drew students had higher odds of practicing in a medically disadvantaged area (OR: 3.23; 95% CI: 2.20–4.73) (Table 3).
Figure 1.
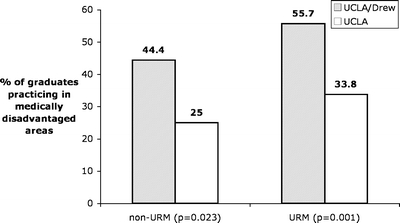
Percentage of graduates practicing in medically disadvantaged areas in California, by race/ethnicity and medical school program. URM Underrepresented minority, non-URM non-underrepresented minority (Asian-American/Pacific Islander, and Non-Latino Caucasian).
Table 3.
Graduates Of The UCLA/Drew Medical Education Program And UCLA SOM, 1985–1995: Bivariate And Multivariate Analysis Of Practice Location In Any Medically Disadvantaged Area
| Variable | Bivariate | Unadjusted | P | Multivariate | Model 1* | P | Multivariate | Model 2* | P |
|---|---|---|---|---|---|---|---|---|---|
| OR | 95% CI | OR | 95% CI | OR | 95% CI | ||||
| Age at matriculation (years) | 1.04 | 0.99–1.09 | .16 | 0.93 | 0.95–1.05 | .93 | 0.98 | 0.91–1.06 | .66 |
| Gender | |||||||||
| Male† | |||||||||
| Female | 0.97 | 0.74–1.28 | .85 | 0.85 | 0.63–1.13 | .26 | 0.92 | 0.62–1.36 | .67 |
| Race/ethnicity | |||||||||
| Non-URM† | |||||||||
| URM | 2.15 | 1.59–2.90 | <.00 1 | 1.59 | 1.11–2.27 | .011 | 1.52 | 0.92–2.50 | .10 |
| Region of origin | |||||||||
| All other† | |||||||||
| California | 1.51 | 0.88–2.77 | .18 | 1.43 | 0.77–2.68 | .26 | 1.20 | 0.58–2.50 | .62 |
| Medical Program | |||||||||
| UCLA† | |||||||||
| UCLA/Drew | 3.23 | 2.20–4.73 | <.00 1 | 2.49 | 1.60–3.88 | <.00 1 | 2.05 | 1.14–3.68 | .016 |
| Year of graduation (years) | 1.011 | 0.97–1.06 | 0.60 | 1.01 | 0.97–1.06 | .52 | 1.02 | 0.95–1.10 | .52 |
| Specialty choice | |||||||||
| Primary care | |||||||||
| Non-primary care† | |||||||||
| Primary care | 1.10 | 0.85–1.44 | .47 | 0.96 | 0.72–1.29 | .85 | 1.06 | 0.73–1.55 | .76 |
| Parents’ education | |||||||||
| Mother | |||||||||
| High school or less | 1.73 | 1.17–2.55 | .006 | 1.31 | 0.75–2.30 | .34 | |||
| Some college/business/technical training | 1.48 | 0.98–2.25 | .06 | 1.64 | 0.92–2.92 | .091 | |||
| College degree | 1.07 | 0.68–1.68 | .76 | 1.48 | 0.76–2.89 | .25 | |||
| Graduate or professional work† | |||||||||
| Father | |||||||||
| High school degree or less | 1.65 | 1.13–2.41 | .009 | 0.75 | 0.44–1.27 | .29 | |||
| Some college/business/technical training | 1.78 | 1.16–2.73 | .008 | 1.18 | 0.66–2.11 | .58 | |||
| College degree | 0.90 | 0.59–1.37 | .61 | 0.79 | 0.39–1.58 | .50 | |||
| Graduate or professional work† | |||||||||
| Parents’ occupation | |||||||||
| Mother | |||||||||
| Nonprofessional/manager | 1.44 | 1.03–2.02 | .04 | 1.66 | 0.96–2.86 | .068 | |||
| Professional/manager/owner† | |||||||||
| Father | |||||||||
| Nonprofessional/manager | 2.26 | 1.56–3.28 | <.001 | 1.00 | 0.64–1.54 | .99 | |||
| Professional/Manager/Owner† | |||||||||
| High school community | |||||||||
| Suburban: large and moderate size cities† | |||||||||
| Urban: large and moderate size cities | 1.19 | 0.86–1.63 | .30 | 0.93 | 0.63–1.38 | .73 | |||
| Rural area to small city | 1.25 | 0.81–1.95 | .31 | 0.96 | 0.56–1.62 | .87 | |||
*Model 1: N = 1,047 (Missing 2.24%; 24/1,071). Model 2 (inclusion of social background variables from the Prematriculation Questionnaire: N = 672 (Missing 37.3%; 399/1,071).
†Reference category
In multivariate analysis, only URM race/ethnicity (OR: 1.57; 95% CI: 1.09–2.25) and participation in the UCLA/Drew program (OR: 2.47; 95% CI: 1.59–3.83) remained predictive of practice in an MDA (Table 3). After controlling for both premedical and educational factors, the only variable associated with practice in an MDA was the UCLA/Drew indicator (OR: 2.05; 95% CI: 1.14–3.68).
The sensitivity analysis showed that, if we assume that 100% of out-of-state Drew graduates are not practicing in MDAs and holding the proportion of out-of-state UCLA graduates at 26%, the Drew effect remains (OR: 1.88). To conclude that no Drew effect exists, 100% of Drew graduates out-of-state would have to be practicing in non-MDAs, and 68% of out-of state UCLA graduates would have to be located in MDAs.
DISCUSSION
The Martin Luther King, Jr. Medical Center and the Charles R. Drew University of Medicine and Science provide care for one of the most impoverished populations in Los Angeles County. The results of this study suggest that the UCLA/Drew Medical Education Program has been preparing physicians in accordance with the Drew mission. Our findings are consistent with those for the Jefferson Physician Shortage Area Program (PSAP), which has demonstrated that after controlling for rural background and premedical interest, PSAP graduates are more likely to become rural family physicians.9 No factor has been as strongly linked service to the underserved as minority race/ethnicity. In this study, we found that after controlling for URM status, Drew graduates have greater odds of practicing in disadvantaged communities. We propose that an inner-city-based program may have a reinforcing effect on those students initially inclined to work in these communities.
As does the PSAP, the UCLA/Drew Program contains two main nontraditional components: first, an admissions process that emphasizes applicant commitment to service; and second, longitudinal clinical experiences in the target community. The Drew admissions committee assesses applicants’ involvement in community service, leadership potential, motivations, understanding of the needs of underserved populations, and the maturity and clarity of their career goals. In a previous study on student intentions, we found that students in UCLA/Drew program showed increased commitment over the course of medical school in contrast to their UCLA classmates with the same initial career goals, who experienced a decline in interest.14 In conjunction with our present findings, this suggests that the program’s success may be attributable in part to the selection and development of exceptionally motivated students.
Medical programs can provide a supportive environment for students in a number of ways. Although short-term rotations have no demonstrated effect, cumulative experiences during medical training predict family medicine residents’ intent to practice in underserved areas.19 After their first 2 years of basic science instruction at UCLA, students complete core clinical rotations at the King/Drew Medical Center (KDMC), participate in a longitudinal primary care clinic in a neighborhood health center, and conduct a research thesis specific to disadvantaged populations. As a result, students spend a majority of their clinical time in south Los Angeles and through their experiences, develop ties to the patient population and community. In addition, Drew students’ goals may be further nurtured and reinforced through interactions with like-minded peers and faculty. Furthermore, the student body at Drew is quite diverse, with ∼70% of students being of URM backgrounds. Students in medical schools with greater racial diversity have more favorable attitudes to underserved populations.20
One of the strengths of the present study is the robustness of the findings across several indicators of “medically disadvantaged areas.” The most common measures are federally designated “Health Professional Shortage Areas” (HPSAs) or Medically Underserved Areas (MUAs), but these classifications may have limited validity as indicators of community-level need. The HPSA “special population” criterion does not include groups with persistent health care access problems such as minorities other than Native Americans, and although under consideration, revised designation methods have yet to be formally adopted. We find these concerns especially pertinent to this study, because until recently, only the King-Drew medical facility received the HPSA designation, and not the surrounding poor, minority, inner-city community. Therefore, we expanded our measures beyond the HPSA designation to include minority and high-poverty populations and found again that Drew graduates had greater odds of practicing in disadvantaged areas than their UCLA counterparts. We found no relation between the Drew program and practice in rural areas—which, given the urban location of the program, was expected.
In the attempt to evaluate the efficacy of a program with a broadly stated mission, we encountered several limitations. The definition of medically “underserved” or “disadvantaged” area has not yet been operationalized for research at the national level, thus, restricting our analysis to California. We cannot dismiss the possibility that these physicians limited their practices to serving higher-income subgroups in their practice areas, but given the stringency of the outcome criteria, the vast majority of the population is likely to be medically disadvantaged. Nearly one-third of physicians did not complete the Prematriculation Questionnaire (PMQ), which limited our ability to account for socioeconomic background. We were also unable to determine if a graduate grew up in an underserved area, instead, using a type of high school community as an approximation of childhood environment. Furthermore, we did not assess student intentions before medical school, and thus, acknowledge an inherent selection bias in the type of student who chooses to enter the program. It is not feasible to conduct a randomized controlled trial or compare students with applicants who were accepted but chose not to enter the program. Because this study addressed two medical education programs in Los Angeles, the results may not be generalizable to other programs across the nation. Therefore, we limit our conclusions to suggest that the success of the program may be attributed significantly to the selection and training of exceptionally driven students. Overall, this study represents an important first step in illustrating the potential of medical education to shape physician supply and distribution.
The next step would be to examine the practice patterns of the graduates throughout the nation, including teaching and research activities that may also be aimed at health care inequities. Career paths have yet to be described, e.g., whether physicians practice in disadvantaged areas after their careers have been established or if increasing financial obligations or physician burnout lead to an exodus from these areas. Ideally, policymakers and educators would be able identify the key factors to retain physicians in underserved communities for the duration of their careers and demonstrate that having dedicated local care providers improves health outcomes.
As state initiatives have drastically reduced schools’ ability to ensure adequate minority student enrollment,21 the need to train committed physicians to serve poor and minority communities is perhaps greater than ever. We believe the UCLA/Drew Medical Education Program can serve as a model for other institutions to counter persistent disparities in access to physician services along lines of race, ethnicity, income, and geography.
Acknowledgments
We would like to acknowledge the contributions of Lois Colburn, LuAnn Wilkerson, EdD, Deborah Danoff, MD, Carol Hodgson, PhD, Kehua Zhang, Shobita Rajagopalan, MD, Deyu Pan, MS, Magda A. Shaheen, MD, PhD, Elizabeth Mertz, MPA, and the staff of AMA data services for their guidance and assistance. We would also like to thank Dr. Keith Norris for institutional support. Renee Taylor provided administrative assistance. Data analysis and manuscript development was supported by the National Center for Research Resources (P20-RR11145 and G12-RR03026-15), the National Center on Minority Health and Health Disparities (1 P20MD00148-01), the Agency for Healthcare Research and Quality (1R24-HS014022-01A1) and (T 32-HS00046), and the Bureau of Health Professions, Health Resources and Services Administration (U79HP00004). The abstract from this study was presented at the Society of General Internal Medicine 29th Annual Meeting Poster Session, April 27, 2006.
Drs. Edelstein and Heslin are employees of the Charles R. Drew University of Medicine and Science and are faculty members of the David Geffen School of Medicine at UCLA.
Conflicts of interest None disclosed.
References
- 1.COGME. Physician distribution and health care challenges in rural and Inner city areas, tenth report. Washington, D.C.: Council of Graduate Medical Education; February 1998.
- 2.Grumbach K, Coffman J, Liu R, Mertz E. Strategies for increasing physician supply in medically underserved communities in California. Berkeley: California Program on Access to Care, California Policy Research Center; 1999.
- 3.Rabinowitz HK, Diamond JJ, Veloski JJ, Gayle JA. The impact of multiple predictors on generalist physicians’ care of underserved populations. Am J Public Health. 2000;90(8):1225–1228. [DOI] [PMC free article] [PubMed]
- 4.Komaromy M, Grumbach K, Drake M, et al. The role of black and Hispanic physicians in providing health care for underserved populations. N Engl J Med. 1996;334(20):1305–1310. [DOI] [PubMed]
- 5.Keith SN, Bell RM, Swanson AG, Williams AP. Effects of affirmative action in medical schools: a study of the class of 1975. N Engl J Med. 1985;313(24):1519–1525. [DOI] [PubMed]
- 6.Cantor JC, Miles EL, Baker LC, Barker DC. Physician service to the underserved: implications for affirmative action in medical education. Inquiry. 1996;33(2):167–180. [PubMed]
- 7.Xu G, Veloski J, Hojat M, Politzer RM, Rabinowitz HK, Rattner SL. Factors influencing primary care physicians’ choice to practice in medically underserved areas. Acad Med. 1997;72(10 Suppl 1):S109–111. [DOI] [PubMed]
- 8.Xu G, Veloski JJ, Barzansky B. Comparisons between older and usual-aged medical school graduates on the factors influencing their choices of primary care specialties. Acad Med. Nov 1997;72(11):1003–1007. [DOI] [PubMed]
- 9.Rabinowitz HK. Critical factors for designing programs to increase the supply and retention of rural primary care physicians. JAMA. 2001;286(9):1041–1048. [DOI] [PubMed]
- 10.Rabinowitz HK, Diamond JJ, Markham FW, Hazelwood CE. A program to increase the number of family physicians in rural and underserved areas: impact after 22 years. JAMA. 1999;281(3):255–260. [DOI] [PubMed]
- 11.Keith SN, Bell RM, Williams AP. Affirmative action in medical education and its effect on Howard and Meharry: a study of the class of 1975. J Natl Med Assoc. February 1988;80(2):153–158. [PMC free article] [PubMed]
- 12.Lloyd SM, Johnson DG. Practice patterns of black physicians: results of a survey of Howard University College of Medicine Alumni. J Natl Med Assoc 1982;74(2):129–141. [PMC free article] [PubMed]
- 13.Johnson DG, Lloyd SM, Miller RL. A second survey of graduates of a traditionally black college of medicine. Acad Med. Feb 1989;64(2):87–94. [DOI] [PubMed]
- 14.Ko M, Edelstein RA, Heslin KC, et al. Impact of the University of California, Los Angeles/Charles R. Drew University Medical Education Program on medical students’ intentions to practice in underserved areas. Acad Med. 2005;80(9):803–808. [DOI] [PubMed]
- 15.Barnhart J, Shekelle P, Lewis C. The effect of a medical school’s admission and curriculum policies on increasing the number of physicians in primary care specialties. Acad Med. 1996;71(3):293–295. [DOI] [PubMed]
- 16.Grumbach K, Hart G, Mertz E, Coffman JM, Palazzo L. Who is caring for the underserved? A comparison of primary care physicians and nonphysician clinicians in California and Washington. Ann Fam Med. 2003;1(2):97–104. [DOI] [PMC free article] [PubMed]
- 17.Goodman DC, Mick SS, Bott D, et al. Primary care service areas: a new tool for the evaluation of primary care services. Health Serv Res. 2003;38:287–309. [DOI] [PMC free article] [PubMed]
- 18.Nelson AR, Betancourt JR, Bloche MG. Unequal Treatment: Confronting Racial and Ethnic Disparities in Health Care. Washington DC: National Academy Press. 2002.
- 19.Tavernier LA, Connor PD, Gates D, Wan JY. Does exposure to medically underserved areas during training influence eventual choice of practice location? Med Educ. 2003;37:299–304. [DOI] [PubMed]
- 20.Elam CL, Johnson MMS, Wiggs JS, Messmer JM, Brown PI, Hinkley R. Diversity in medical school: perceptions of first-year students at four southeastern US medical schools. Acad Med. 2001;76(1):60–65. [DOI] [PubMed]
- 21.Trounson R. UC Sets Record on Freshman Enrollees for Fall. California: Los Angeles Times. June 2, 2006.


