Abstract
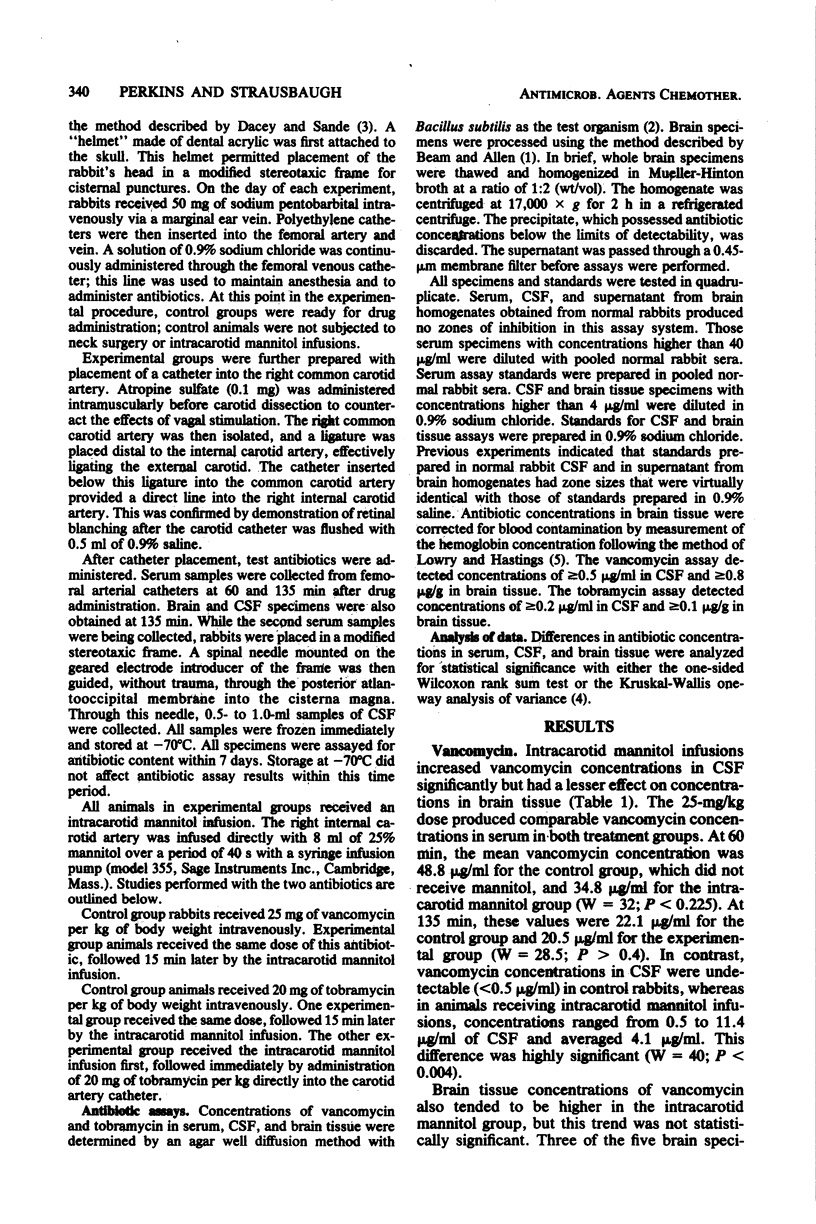
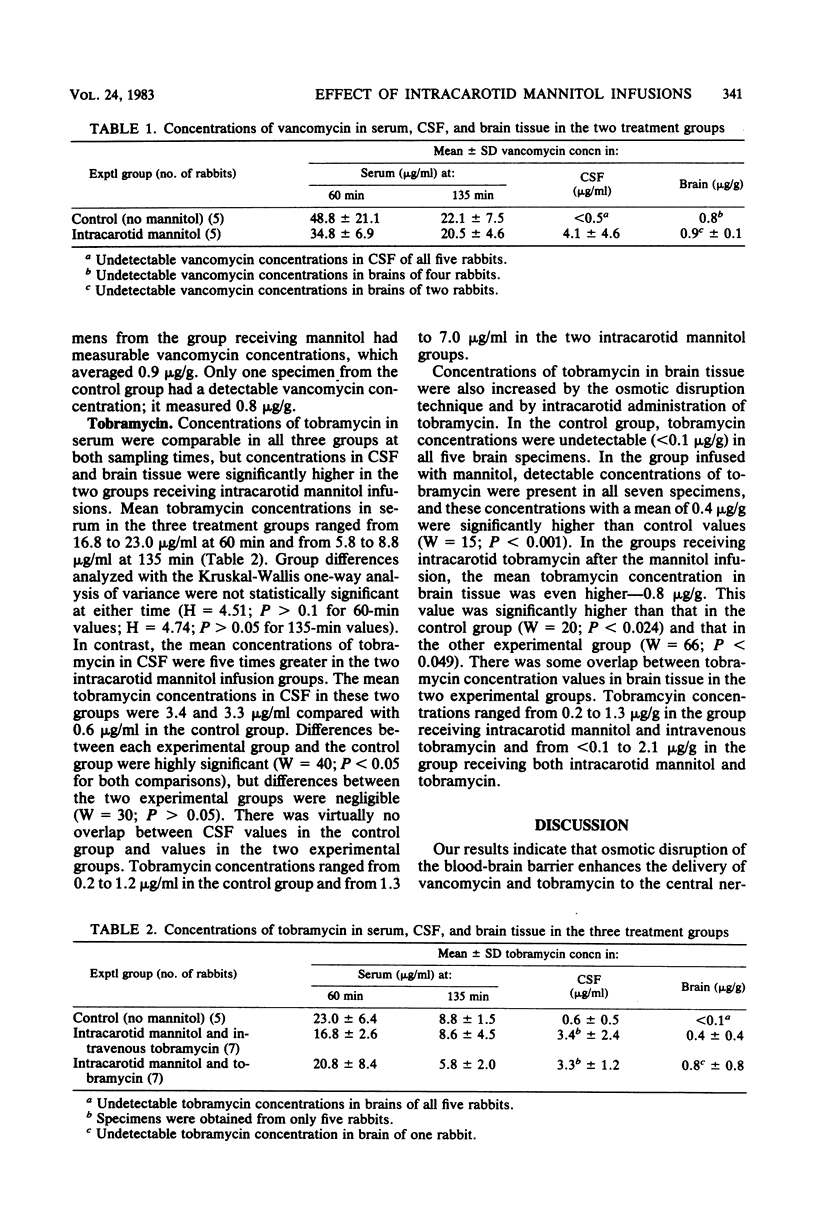
The rapid infusion of hyperosmolar solutions into the internal carotid artery transiently disrupts the integrity of the blood-brain barrier, permitting entry of substances normally excluded from the nervous system. This study examined the effect of such an infusion on the penetration of vancomycin and tobramycin into the cerebrospinal fluid and brains of normal rabbits. Groups of five to seven animals were assigned either to control groups, receiving vancomycin or tobramycin alone, or to experimental groups, receiving these antibiotics with 40-s intracarotid infusions of 8.0 ml of 25% mannitol. Serum, cerebrospinal fluid, and brain specimens were obtained for assay 135 min after dosage. Concentrations of these antibiotics in serum were comparable in control and experimental groups; concentrations of the antibiotics in cerebrospinal fluid were significantly higher in the experimental groups. Mean (+/- standard deviation) concentrations of the antibiotics in cerebrospinal fluid were, respectively, less than 0.5 and 4.1 +/- 4.6 micrograms of vancomycin per ml and 0.6 +/- 0.5 and 3.4 +/- 2.4 micrograms of tobramycin per ml in the control and experimental groups. The concentrations of these antibiotics in brains were also higher in the experimental groups. This trend achieved statistical significance in the tobramycin studies, where control animals uniformly had tobramycin concentrations in brains of less than 0.1 microgram/g and experimental group animals had a mean concentration of 0.4 microgram/g. Additional studies with tobramycin indicated that intracarotid antibiotic administration immediately after the mannitol infusion further augmented antibiotic concentrations in brains.
Full text
PDF
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Beam T. R., Jr, Allen J. C. Blood, brain, and cerebrospinal fluid concentrations of several antibiotics in rabbits with intact and inflamed meninges. Antimicrob Agents Chemother. 1977 Dec;12(6):710–716. doi: 10.1128/aac.12.6.710. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bennett J. V., Brodie J. L., Benner E. J., Kirby W. M. Simplified, accurate method for antibiotic assay of clinical specimens. Appl Microbiol. 1966 Mar;14(2):170–177. doi: 10.1128/am.14.2.170-177.1966. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dacey R. G., Sande M. A. Effect of probenecid on cerebrospinal fluid concentrations of penicillin and cephalosporin derivatives. Antimicrob Agents Chemother. 1974 Oct;6(4):437–441. doi: 10.1128/aac.6.4.437. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Neuwelt E. A., Frenkel E. P., Diehl J., Vu L. H., Rapoport S., Hill S. Reversible osmotic blood-brain barrier disruption in humans: implications for the chemotherapy of malignant brain tumors. Neurosurgery. 1980 Jul;7(1):44–52. doi: 10.1227/00006123-198007000-00007. [DOI] [PubMed] [Google Scholar]
- Neuwelt E. A., Frenkel E. P., Rapoport S., Barnett P. Effect of osmotic blood-brain barrier disruption on methotrexate pharmacokinetics in the dog. Neurosurgery. 1980 Jul;7(1):36–43. doi: 10.1227/00006123-198007000-00006. [DOI] [PubMed] [Google Scholar]
- Neuwelt E. A., Maravilla K. R., Frenkel E. P., Rapaport S. I., Hill S. A., Barnett P. A. Osmotic blood-brain barrier disruption. Computerized tomographic monitoring of chemotherapeutic agent delivery. J Clin Invest. 1979 Aug;64(2):684–688. doi: 10.1172/JCI109509. [DOI] [PMC free article] [PubMed] [Google Scholar]



