Diabetes mellitus is a heterogenous condition reflecting different metabolic disorders and accompanied by a variety of complications. However, it is hyperglycaemia that is the common feature and this is used to define diabetes. Diabetes was previously considered a disease of minor significance to world health. However, there has been an explosive increase in the number of people diagnosed with diabetes worldwide in the last few decades.1 The global figure of people with diabetes is set to rise from the current figure of about 180 million in 2000 to 220 million in 2010 and 320 million in 2025. The two major forms of diabetes are:
♦ type 1 diabetes, which is predominantly due to autoimmune mediated destruction of pancreatic β-cells and results in absolute insulin deficiency.
♦ type 2 diabetes, characterised by insulin resistance and/or relatively insufficient insulin secretion. Worldwide over 90% of patients with diabetes have type 2 diabetes. In Australia, the frequency of diabetes is 7.4% of the adult population of which only 50% are diagnosed.2
Rationale for Guidelines for the Detection of Diabetes
Diagnostic cut-off levels for diabetes have been determined using blood glucose concentrations which are associated with increased prevalence of diabetic complications. One study examined the prevalence of retinopathy and nephropathy in Pima Indians, a population with a very high frequency of type 2 diabetes mellitus. Fasting plasma glucose, 2-hour plasma glucose during an oral glucose tolerance test (OGTT) and haemoglobin A1C were all similarly predictive in identifying patients with an increased risk of future complications of hyperglycaemia.3
The old diagnostic cut-points for diabetes were higher than the currently used ones (see Table 1) and represent threshold values above which microvascular complications (particularly retinopathy) begin to occur, and below which these complications are very rare. However, if one looks at cardiovascular disease, which is a much greater cause of morbidity and mortality in patients with type 2 diabetes than are the specific diabetic complications, no such easy threshold can be defined. The risk of cardiovascular disease starts to rise at levels well below those at which diabetes is diagnosed and the relationship is continuous without a clear threshold effect.
Table 1.
Diabetes Mellitus and Prediabetic states as defined by the OGTT (75 g anhydrous glucose)
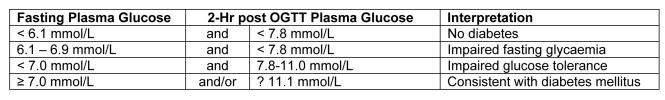
Studies comparing the value of fasting glucose with the diagnostic 2-hour value found that typically only 25% of individuals with a 2-hour plasma glucose of ≥11.1 mmol/L also had a fasting plasma glucose ≥7.8 mmol/L while over 90% of those with a fasting plasma glucose of ≥7.8 mmol/L had a 2-hour plasma glucose ≥11.1 mmol/L. This is consistent with the view that the fasting threshold of 7.8 mmol/L represented a more severe degree of hyperglycaemia than did the 2-hour post OGTT value of 11.1 mmol/L.
Investigations in populations from the Southern Hemisphere showed that across a number of populations, 7.0 mmol/L was the fasting value that gave a prevalence of diabetes with the closest match to that produced by a 2-hour post OGTT of 11.1 mmol/L.4
Recognising these discrepancies, the American Diabetes Association (ADA) and the WHO recommended changes to the diagnostic criteria of diabetes in 1997 and 1999 (see Table 1).5,6
In these criteria the diagnostic fasting level has been lowered to 7.0 mmol/L and a new category of impaired fasting glycaemia with fasting glucose levels of 6.1–6.9 mmol/L has been added. As the fasting plasma glucose is considerably more reproducible than the 2-hour post OGTT glucose level and is simpler to perform than the OGTT, the ADA also suggested that the fasting plasma glucose rather than the OGTT should be the diagnostic test of choice for clinical and epidemiological purposes. The ADA suggested abandoning the OGTT. This is in contrast to the WHO which advocates the retention of the OGTT. In a combined position statement the Australian Diabetes Society, New Zealand Society for the Study of Diabetes, the Royal College of Pathologists of Australasia and the Australasian Association of Clinical Biochemists have supported the WHO recommendations.7
Subsequent information seems to indicate that elevation of the fasting glucose and post OGTT hyperglycaemia seem to represent distinct, but overlapping entities. Fasting and 2-hour post OGTT glucoses have similar relationships with retinopathy, but the 2-hour post OGTT seems to give additional information in relation to future cardiovascular risk over the fasting glucose.8–10 Therefore we should not, at this stage, abandon the OGTT.
When should an OGTT be done?
The disadvantage of the OGTT is the fact that it is labour-intensive and cumbersome for patients. In order to optimise case findings of patients with undiagnosed diabetes in primary care in Australia, evidence-based guidelines from the National Health and Medical Research Council have been published.11 They advocate testing for undiagnosed type 2 diabetes in certain high-risk groups (see Table 2).
Table 2.
Recommendation for screening for type 2 diabetes in high-risk individuals.
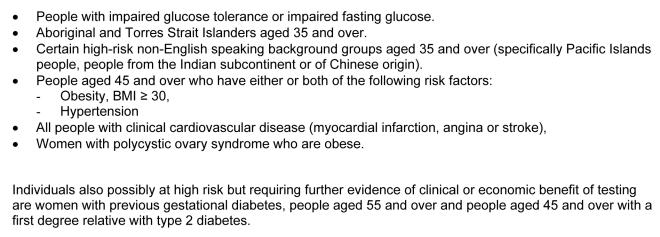
In these high-risk populations, plasma glucose (preferably fasting) is recommended as a screening test. According to the guidelines, if the plasma glucose is <5.5 mmol/L then diabetes is unlikely. A fasting plasma glucose of 7.0 mmol/L or more, or a random glucose of 11.1 mmol/L or more makes diabetes likely and the diagnosis is confirmed by a repeat abnormal test. If the plasma glucose is between 5.5 and 6.9 mmol/L fasting, or between 5.5 and 11.0 mmol/L non-fasting, an OGTT with 75 g anhydrous glucose is recommended.
Thus, blood testing is required only in those people with risk factors, ideally begins with a fasting glucose, and progresses to an OGTT where necessary. This approach has been evaluated using data from the general practice-based Australian Diabetes Screening Study and found to have a high level of detection of people with diabetes.12
Diagnosis of Gestational Diabetes
Pregnancy is characterised by a degree of insulin resistance caused by a number of placental diabetogenic hormones and by large fluctuations of serum glucose and insulin concentrations as the mother oscillates between the fed and fasted states. Gestational diabetes occurs when a woman's pancreatic function is not sufficient to cope with the relative insulin resistance created by the anti-insulin hormones and the increased fuel consumption necessary to provide for the growing foetus. Hyperglycaemia in pregnancy, if untreated, is associated with a number of complications; in particular foetal macrosomia, pre-eclampsia, neonatal metabolic complications (hypoglycaemia and hyperbilirubinaemia), an increase in perinatal mortality and an increased risk of development of diabetes, both in the mother and in the offspring.
Australian guidelines for gestational diabetes recommend universal screening.13 However, if selective screening is considered more appropriate because of limited resources or known low gestational diabetes incidence, it may be reserved for those at higher risk.
Factors that increase the risk of gestational diabetes are:
♦ increasing age, especially over 30 years
♦ higher body mass index
♦ a family history of diabetes
♦ belonging to a high-risk ethnic group (especially indigenous Australian, Pacific Island, Asian or Middle Eastern background).
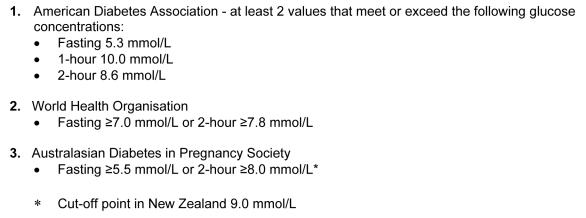
While some international data seem to indicate that a complex scoring system can be used to reduce the number of people screened without loss in sensitivity,14 data from Australia have been controversial. On the basis of their study, Moses and co-workers advocate that even women from a low-risk group, ie. lean, young Caucasian women, need to be tested.15 On the other hand, Davey and Hamblin feel, on the basis of their retrospective data of 6,000 women, that selective screening can be initiated.16 The current Australian recommendation is for universal screening with an initial glucose challenge test with 50 g glucose and 1-hour post challenge plasma glucose.13 Women with a blood glucose value at 1-hour post 50 g glucose ≥7.8 mmol/L are regarded as positive and they are recommended to have a 2-hour OGTT with 75 g glucose. This approach has a sensitivity of about 80% as compared to the full OGTT. While in the United States a 100 g 3-hour OGTT has been advocated, more commonly a 2-hour 75 g OGTT is performed in the rest of the world. Both the ADA and the WHO have endorsed this 2-hour 75 g OGTT for the diagnosis of gestational diabetes although they have different criteria for a positive test.17,18 Furthermore, the Australian Diabetes in Pregnancy Society has different values again (see Table 3).With these many differing current guidelines and without good interventional evidence recommending adherence to one over another, we recommend the Australasian Diabetes in Pregnancy Society guidelines.
Table 3.
Criteria for positive 2-hour 75 g OGTT for the diagnosis of gestational diabetes.
Summary
While considerable progress has been made over the last 10 years in the diagnosis of diabetes, there are still slight differences in the diagnosis of diabetes in different parts of the world. It has emerged over the last few years that, while impaired fasting glucose and impaired glucose tolerance are both associated with an increased risk of diabetes, the 2-hour glucose result in the OGTT seems to indicate an additional risk that is not captured with the fasting glucose. Protocols are being developed that allow significant success in targeted screening of populations. In gestational diabetes the situation is more confused and further interventional studies are required to identify whether all patients need to be screened for gestational diabetes or whether we can target certain groups. Both the ADA and WHO accept that frequent reviews of the cut-off values are required on the basis of emerging data from epidemiological studies around the globe.
References
- 1.Zimmet P, Alberti KGM, Shaw J. Nature. 2001;414:782–7. doi: 10.1038/414782a. [DOI] [PubMed] [Google Scholar]
- 2.Dunstan DW, Zimmet PZ, Welborn TA, et al. The rising prevalence of diabetes mellitus and impaired glucose tolerance: the Australian diabetes, obesity and lifestyle study. Diabetes Care. 2002;25:829–834. doi: 10.2337/diacare.25.5.829. [DOI] [PubMed] [Google Scholar]
- 3.McCance DR, Hanson RI, Charles M-A, et al. Comparison of tests for glycated haemoglobin and fasting and two hour plasma glucose concentrations as diagnostic methods for diabetes. BMJ. 1994;308:1323–8. doi: 10.1136/bmj.308.6940.1323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Finch CF, Zimmet PZ, Alberti KGMM. Determining diabetes prevalence: a rational basis for the use of fasting plasma glucose concentrations? Diabetic Med. 1990;7:603–10. doi: 10.1111/j.1464-5491.1990.tb01457.x. [DOI] [PubMed] [Google Scholar]
- 5.American Diabetes Association. Report of the Expert Committee on the diagnosis and classification of diabetes mellitus. Diabetes Care. 1997;20:1183–97. doi: 10.2337/diacare.20.7.1183. [DOI] [PubMed] [Google Scholar]
- 6.World Health Organization. Definition, Diagnosis and Classification of Diabetes mellitus and its Complications; Part 1: Diagnosis and Classification of Diabetes Mellitus. Department of Noncommunicable Disease Surveillance, Geneva, 1999.
- 7.Colman PG, Thomas DW, Zimmet PZ, Welborn TA, Garcia-Webb P, Moore MP. New classification and criteria for the diagnosis of diabetes mellitus. Position statement from the Australian Diabetes Society, New Zealand Society for the Study of Diabetes, the Royal College of Pathologists of Australasia and Australasian Association of Clinical Biochemists. Med J Aust. 1999;170:375–8. [PubMed] [Google Scholar]
- 8.Barzilay JI, Spiekerman CF, Wahl PW, et al. Cardiovascular disease in older adults with glucose disorders; comparison of American Diabetes Association criteria for diabetes mellitus with WHO criteria. Lancet. 1999;354:622–5. doi: 10.1016/s0140-6736(98)12030-5. [DOI] [PubMed] [Google Scholar]
- 9.DECODE Study Group. Glucose tolerance and mortality: comparison of WHO and American Diabetes Association diagnostic criteria. Lancet. 1999;354:617–21. [PubMed] [Google Scholar]
- 10.Unwin N, Shaw J, Zimmet P, Alberti G. International Diabetes Federation IGT/IFG Consensus Statement. Report of an Expert Consensus Workshop. Diabetic Medicine. 2002;19:708–23. [Google Scholar]
- 11.www.diabetesaustralia.com.au/docs/mellitus/Part3-FINAL.pdf accessed 1st April, 2003.
- 12.Hilton DJ, O'Rourke PK, Welborn TA, Reid CM. Diabetes detection in Australian general practice: a comparison of diagnostic criteria. Med J Aust. 2002;176:104–7. doi: 10.5694/j.1326-5377.2002.tb04314.x. [DOI] [PubMed] [Google Scholar]
- 13.Hofman L, Nolan C, Wilson JD, Oates JN, Simmons D. Gestational diabetes mellitus management guidelines. The Australasian Diabetes in Pregnancy Society. Med J Aust. 1998;169:93–7. doi: 10.5694/j.1326-5377.1998.tb140192.x. [DOI] [PubMed] [Google Scholar]
- 14.Naylor CD, Sermer M, Chen E, Farine D. Selective Screening for Gestational Diabetes Mellitus. N Engl J Med. 1997;337:1591–6. doi: 10.1056/NEJM199711273372204. [DOI] [PubMed] [Google Scholar]
- 15.Moses RG, Moses J, Davis WS. Gestational diabetes: do lean young Caucasian women need to be tested? Diabetes Care. 1998;21:1803–6. doi: 10.2337/diacare.21.11.1803. [DOI] [PubMed] [Google Scholar]
- 16.Davey RX, Hamblin PS. Selective versus universal screening for gestational diabetes mellitus: an evaluation of predictive risk factors. Med J Aust. 2001;174:118–21. doi: 10.5694/j.1326-5377.2001.tb143181.x. [DOI] [PubMed] [Google Scholar]
- 17.American Diabetes Association. Gestational Diabetes Mellitus. Diabetes Care. 2001;24:S77. [PubMed] [Google Scholar]
- 18.WHO Consultation: Definition, Diagnosis and Classification of Diabetes Mellitus and its Complications: Report of a WHO Consultation. Part I: Diagnosis and Classification of Diabetes Mellitus. WHO/NCD/NCS/99.2, World Health Organisation, Geneva, 1999.


