Abstract
Objectives. Evidence indicates that foreign-born Latinos have a health advantage compared with US-born persons of the same socioeconomic status. An explanation for this paradox has remained elusive. We examined the extent to which this paradox exists for the prevalence of asthma and other respiratory conditions. We then explored the role of neighborhood social context in understanding any observed advantage. We invoked theories of social organization, collective efficacy, and the urban ethnic enclave.
Methods. We combined data from the Project on Human Development in Chicago Neighborhoods Community Survey with 2 other data sources and used hierarchical generalized linear modeling techniques.
Results. We found a distinctly graded effect for asthma and other breathing problems among foreign-born Latinos, depending on community composition. Foreign-born Latinos embedded in a neighborhood that had a high percentage of foreign-born residents experienced a significantly lower prevalence of asthma and other breathing problems; those in communities that had a low percentage of foreign-born residents had the highest prevalence overall (even when compared with African Americans).
Conclusions. Foreign-born Latinos have a respiratory health advantage only in enclave-like settings. Contexts such as these may provide the cohesiveness critical for effective prevention.
Racial and ethnic disparities in health status continue to cause concern prompting numerous efforts in clinical practice and policy to enhance access to care, increase adherence to treatment regimes, and improve health habits. One anomaly in the disparities literature is the oft-documented “Latino Paradox.” Also described as the Hispanic or Epidemiological Paradox, these terms refer to the relatively good health and longer life span of foreign-born Latinos when expectations (in most analyses, primarily based on their socioeconomic status) suggest far greater morbidity and mortality than observed. The paradox has been documented for several health outcomes, including all-cause mortality, infant mortality, and functional status.1–3 Recent work indicates that the mortality paradox may be the result of return migration effects, at least for those of Mexican origin.4 Evidence related to morbidity, however, continues to indicate a health advantage for foreign-born Latinos when compared with their US-born counterparts.5
In addition to migration and associated data artifact explanations, social and cultural capital (i.e., community-level social cohesiveness, norms, and practices) have been hypothesized as mechanisms responsible for the relatively beneficial health trajectories of Latino immigrants.4,6 High levels of social capital may affect the community’s potential to encourage positive health habits or sanction negative ones. This hypothesized health behavior pathway, however, does not address larger forces that operate at the neighborhood level. Neighborhood-level influences, such as the availability of social support or the accessibility and quality of public parks, may have independent effects on health. Moreover, community characteristics may condition any Latino advantage; that is, foreign-born Latinos may benefit from being embedded in immigrant-dominated and potentially more supportive contexts.7 By contrast, foreign-born Latinos living in communities without a strong immigrant presence may be at a disadvantage.
Knowledge of the comparative morbidity experience of US-born and foreign-born Latinos is limited,7 as is understanding of the role of community context in shaping their health. Asthma, in particular, remains relatively understudied in the Latino population.8–12 The prevalence of asthma appears to vary across small areas and to be affected by neighborhood characteristics13; attention to social context is important to understanding the prevalence of asthma in population subgroups.14 The urban ethnic enclave provides a rich example of the form of community social context where networks are dense and the transmission of health-enhancing information is likely great. We examine the extent to which the Latino Paradox exists for asthma and other respiratory conditions. We then extend previous research by moving beyond individual-level predictors to examine the social context in which these conditions take root.
We employed theories of social organization, collective efficacy,15,16 immigrant adaptation, and the urban ethnic enclave17–19 to understand how neighborhood social context contributes to asthma and other respiratory conditions, by Latino foreign-born status. Social organization and collective efficacy theories enabled us to draw out components of community life that could be important both to the prevalence of respiratory conditions and to the social organizational features of the ethnic enclave. Structural features of the neighborhood (e.g., residential stability, ethnic heterogeneity, and economic status) set the stage for neighborhood social processes to emerge. These social processes—collective efficacy and social network interaction and social exchange—may have independent effects on health.20 Collective efficacy captures the level of trust and attachment in the neighborhood that can be drawn on for mutually beneficial action (i.e., the ability of the community to come together for the common good). For example, neighbors may take responsibility for maintaining safe streets and parks; residents are then drawn outdoors where they get exercise and fresh air. Neighbors do so because “it’s what we do in our community,” rather than because it directly benefits someone they know. Social interaction and social exchange, by contrast, capture the breadth of potentially health-protective social support within a community, and these measures speak to direct social interaction. For example, sharing health information or driving a neighbor to the doctor are the types of instrumental activities that result from dense network connections.
Our aim in applying these theoretical frameworks was to introduce a conceptualization of the enclave experience that is congruent with previous work but adds an emphasis on neighborhood-level social processes. The interdependence of individual and community characteristics may largely explain the Latino paradox: the relative health advantage of foreign-born Latinos may be contingent on features of their residential context.
METHODS
Data and Measures
To address our hypotheses we combined 3 data sources from the 1990s that provide individual-level outcomes nested in neighborhoods, as well as measures that capture individual- and neighborhood-level phenomena: (1) the Metropolitan Chicago Information Center Metro Survey (MCIC-MS), (2) the Decennial Census, and (3) the Project on Human Development in Chicago Neighborhoods Community Survey (PHDCN-CS).
MCIC-MS.
The MCIC-MS included a serial cross-section of adults aged 18 years and older who resided in the 6-county metropolitan Chicago area (on average, 3000 respondents per wave). To create the individual-level component of our final analytic data set, we pooled the City of Chicago subsample of the 1995, 1997, and 1999 waves of the MCIC-MS (n=3191). The outcome measure and individual-level covariates were derived from these data. The outcome measure was a dichotomous measure derived from the question, has a doctor ever told you that you have asthma, bronchitis, emphysema, or other breathing problems? Evidence indicated that this form of self-reported health status question is both reliable and valid.21 Although this question does not measure the presence of any 1 of these conditions individually, it does provide a comprehensive assessment of respiratory disorders. Prevalence data from the City of Chicago suggested that most of these cases may be asthma, but we note that our outcome measure was meant to capture breathing disorders beyond asthma.22,23 The individual-level covariates derived from the MCIC-MS included age, gender, race/ethnicity, marital status, income, education, home ownership, regular source of care, insurance status, current smoking behavior, and a physician-indicated weight problem. We compared Whites, Blacks, and Latinos born in and outside the United States. We chose to exclude those who identified as Puerto Rican (n=110). Although Puerto Ricans share a language and some common cultural elements with the Latinos in our sample, they are US citizens. Thus, migration patterns between the continental United States and Puerto Rico are more fluid. The unique status of Puerto Ricans renders comparisons difficult under the Latino paradox rubric.
Decennial Census.
Census data made it possible for us to construct measures of neighborhood socioeconomic structure and composition. Three of the 5 neighborhood-level measures came from these data. The first measure was a residential stability factor score that included the percentage of residents living in the same house since 1985 and the percentage of owner-occupied dwellings. The second measure was the logged value of a concentrated poverty factor score, which included the percentage of female-headed households, unemployed residents, and residents living below the poverty line or receiving public assistance. The third measure was the logged value of the percentage of foreign-born residents in the neighborhood.
PHDCN-CS.
The sampling design of the PHDCN-CS relied on 1990 US Census data for Chicago to identify 343 neighborhood clusters—groups of 2 to 3 census tracts that contain approximately 8000 people. Major geographic boundaries (e.g., railroad tracks, parks, freeways), knowledge of Chicago’s local neighborhoods, and cluster analyses of census data guided the construction of neighborhood clusters so that they were relatively homogeneous with respect to racial/ethnic mix, socioeconomic status, housing density, and family structure. Two measures of neighborhood social context were derived from these data. Collective efficacy was operationalized by combining measures of social cohesion and informal social control. Social cohesion was constructed from a cluster of conceptually related items from the PHDCN-CS that measured the respondent’s level of agreement (on a 5-point scale) with the following statements: (1) People around here are willing to help their neighbors, (2) This is a close-knit neighborhood, (3) People in this neighborhood can be trusted, and (4) People in this neighborhood generally don’t get along with each other. Health-related informal social control was determined from the respondent’s level of agreement with the following statements: (1) If I were sick I could count on my neighbors to shop for groceries for me, and (2) You can count on adults in this neighborhood to watch out that children are safe and don’t get in trouble. An additional informal social control item asked respondents how likely it was that people in their neighborhood would intervene if a fight broke out in front of their house. The informal social control items address expectations for beneficial health-related action as well as neighborhood supervision of potentially hazardous conditions or violent situations. The 7 items were combined to form a single scale of health-related collective efficacy.
The social interaction and exchange scale measured the frequency of interaction and network-based exchange among neighbors. By contrast to the generalized assessments of trust, solidarity, and shared expectations for informal social control included in the measure of collective efficacy, the social interaction and exchange scale was designed to capture actual ties between neighborhood residents. Respondents were asked, how often do you and people in this neighborhood (1) have parties or other get-togethers where other people in the neighborhood are invited, (2) visit in each others homes or on the street, (3) ask each other advice about personal things such as child rearing or job openings, and (4) do favors for each other?
Analysis
The clustering of respondents within Chicago’s neighborhoods rendered standard ordinary least squares techniques inappropriate because of the likely underestimation of standard errors. Our analysis strategy used hierarchical modeling techniques to investigate the prevalence of asthma and other breathing problems across neighborhoods.24,25 This approach had several advantages. First, the technique allowed for adjustment of standard errors for the effects of clustering within neighborhoods. Second, it facilitated examination of interactions between the individual-level foreign-born status and neighborhood-level factors. To correct independent neighborhood-level measures of collective efficacy and social interaction and exchange for missing data and differences in the reliability of estimates across neighborhoods, we used empirical Bayes residuals from a 3-level item-response model of the component items of these scales.26 We used the Hierarchical Linear and Nonlinear Modeling 6 software program (Scientific Software International, Lincolnwood, Ill) to conduct our analyses.
We began by calculating the means and standard deviations that described our study population, the individual-level component of our analysis (Table 1 ▶). The main feature of our analysis was a series of 6 nested hierarchical logit models (Table 2 ▶) that combined individual and neighborhood-level covariates. A “yes” response to the question about asthma and other breathing problems formed the outcome. The coefficients presented in Table 2 ▶ are odds ratios (with confidence intervals [CIs] in parentheses). We first analyzed individual-level factors, then sequentially introduced residential stability, concentrated poverty, percent foreign-born, collective efficacy, and social interaction and exchange. The interview year was included as a control variable across models. Our final model was as follows:
TABLE 1—
Summary Statistics of the Study Population (N=3191): Chicago, Ill, 1995, 1997, 1999
| Mean (SD) | |
| Outcome | |
| Asthma/breathing problems | 0.18 |
| Control variables | |
| Female | 0.59 |
| Age | 42.99 (16.14) |
| Race/ethnicity | |
| White | 0.42 |
| Black | 0.36 |
| Foreign-born Latino | 0.10 |
| US-born Latino | 0.06 |
| Other | 0.06 |
| Married | 0.39 |
| Income, $ | |
| < 9 999 | 0.09 |
| 10 000–14 999 | 0.07 |
| 15 000–19 999 | 0.08 |
| 20 000–24 999 | 0.08 |
| 25 000–29 999 | 0.11 |
| 30 000–39 999 | 0.16 |
| 40 000–49 999 | 0.14 |
| 50 000–69 999 | 0.11 |
| 70 000–89 999 | 0.07 |
| ≥ 90 000 | 0.08 |
| Education | |
| ≤ 4th grade | 0.01 |
| 5th–8th grade | 0.05 |
| 9th–12th grade, no diploma | 0.11 |
| High-school graduate | 0.16 |
| Trade or vocational school | 0.07 |
| Some college | 0.26 |
| College graduate | 0.17 |
| Some graduate study | 0.04 |
| Graduate degree | 0.13 |
| Home ownership | 0.43 |
| No regular source of medical care | 0.04 |
| Insurance | |
| Private insurance | 0.67 |
| Medicare | 0.08 |
| Medicaid | 0.08 |
| No Insurance | 0.17 |
| Current smoker | 0.29 |
| Weight problem | 0.20 |
TABLE 2—
Six Hierarchical Logit Models of Individual- and Neighborhood-Level Covariates of Asthma and Other Breathing Problems: Chicago, Ill, 1995, 1997, 1999
| Variable | Model 1 OR (95% CI) | Model 2 OR (95% CI) | Model 3 OR (95% CI) | Model 4 OR (95% CI) | Model 5 OR (95% CI) | Model 6 OR (95% CI) |
| Individual-level characteristics | ||||||
| Year | 1.01 (0.95, 1.07) | 1.01 (0.95, 1.07) | 1.01 (0.95, 1.08) | 1.01 (0.96, 1.08) | 1.01 (0.96, 1.08) | 1.01 (0.96, 1.08) |
| Age | 0.99 (0.99, 1.00) | 0.99 (0.99, 1.00) | 0.99 (0.99, 1.00) | 0.99 (0.99, 1.00) | 0.99 (0.99, 1.00) | 0.99 (0.99, 1.00) |
| Gender (female) | 1.41*** (1.17, 1.70) | 1.41*** (0.17, 1.70) | 1.41*** (1.17, 1.70) | 1.41*** (1.17, 1.70) | 1.40*** (1.16, 1.69) | 1.40*** (1.16, 1.69) |
| Race/ethnicitya | ||||||
| Black | 1.08 (0.88, 1.34) | 1.02 (0.73, 1.43) | 1.04 (0.75, 1.45) | 1.05 (0.76, 1.46) | 1.05 (0.76, 1.45) | 1.05 (0.76, 1.46) |
| US-born Latino | 0.68*** (0.44, 1.05) | 0.64** (0.42, 0.98) | 0.63** (0.41, 0.97) | 0.64** (0.42, 0.98) | 0.63** (0.41, 0.96) | 0.63** (0.41, 0.96) |
| Foreign-born Latino | 0.40*** (0.24, 0.67) | 0.38*** (0.22, 0.64) | 0.70 (0.37, 1.35) | 0.60 (0.29, 1.24) | 0.50** (0.26, 0.98) | 0.48** (0.23, 0.99) |
| Other | 0.62** (0.40, 0.97) | 0.61** (0.39, 0.97) | 0.61** (0.39, 0.97) | 0.62** (0.39, 0.97) | 0.62* (0.39, 0.97) | 0.62** (0.39, 0.97) |
| Married | 0.98 (0.80, 1.20) | 0.97 (0.79, 1.20) | 0.97 (0.79, 1.20) | 0.97 (0.79, 1.19) | 0.98 (0.79, 1.20) | 0.98 (0.79, 1.20) |
| Income | 1.03 (0.98, 1.08) | 1.04 (0.99, 1.09) | 1.04 (0.99, 1.09) | 1.04 (0.99, 1.09) | 1.04 (0.99, 1.09) | 1.04 (0.99, 1.09) |
| Education | 1.00 (0.94, 1.05) | 1.00 (0.95, 1.06) | 1.00 (0.95, 1.06) | 1.00 (0.95, 1.06) | 1.00 (0.94, 1.06) | 1.00 (0.94, 1.06) |
| Home ownership | 0.94 (0.75, 1.19) | 0.91 (0.71, 1.17) | 0.90 (0.70, 1.16) | 0.90 (0.70, 1.15) | 0.89 (0.70, 1.14) | 0.89 (0.70, 1.14) |
| No regular source of medical care | 0.72 (0.42, 1.23) | 0.71 (0.42, 1.22) | 0.71 (0.42, 1.22) | 0.71 (0.42, 1.20) | 0.73 (0.43, 1.24) | 0.72 (0.42, 1.23) |
| Insurance statusb | ||||||
| Medicare | 0.97 (0.66, 1.44) | 1.00 (0.67, 1.47) | 0.98 (0.66, 1.45) | 0.97 (0.66, 1.43) | 0.98 (0.67, 1.45) | 0.98 (0.67, 1.44) |
| Medicaid | 1.12 (0.78, 1.62) | 1.12 (0.77, 1.62) | 1.11 (0.77, 1.61) | 1.12 (0.77, 1.61) | 1.12 (0.78, 1.62) | 1.12 (0.77, 1.62) |
| No insurance | 1.23 (0.94, 1.61) | 1.22 (0.94, 1.60) | 1.23 (0.94, 1.60) | 1.23 (0.94, 1.60) | 1.25* (0.96, 1.62) | 1.24 (0.96, 1.62) |
| Current smoker | 1.26** (1.04, 1.53) | 1.25** (1.04, 1.52) | 1.25** (1.03, 1.52) | 1.25** (1.03, 1.52) | 1.24** (1.03, 1.51) | 1.24** (1.03, 1.51) |
| Weight problem | 1.76*** (1.43, 2.16) | 1.74*** (1.41, 2.15) | 1.75*** (1.42, 2.15) | 1.75*** (1.42, 2.15) | 1.73*** (1.41, 2.13) | 1.73*** (1.41, 2.14) |
| Neighborhood-level characteristics | ||||||
| Constant | ||||||
| Residential stability | . . . | 1.08 (0.98, 1.20) | 1.08 (0.98, 1.20) | 1.08 (0.97, 1.20) | 1.08 (0.98, 1.20) | 1.08 (0.98, 1.20) |
| Concentrated poverty | . . . | 1.00 (0.87, 1.16) | 1.01 (0.87, 1.17) | 1.01 (0.87, 1.17) | 1.02 (0.88, 1.18) | 1.02 (0.88, 1.18) |
| Logged percentage foreign born | . . . | 1.01 (0.88, 1.15) | 1.02 (0.90, 1.17) | 1.02 (0.90, 1.17) | 1.03 (0.91, 1.17) | 1.03 (0.91, 1.17) |
| Health-related collective efficacy | . . . | 0.89*** (0.80, 1.00) | 0.90** (0.80, 1.00) | 0.91* (0.82, 1.01) | 0.88* (0.77, 1.01) | 0.89* (0.78, 1.02) |
| Social interaction/exchange | . . . | . . . | . . . | . . . | 1.05 (0.93, 1.20) | 1.05 (0.93, 1.19) |
| Foreign-born Latino | ||||||
| Logged percentage foreign born | . . . | . . . | 0.57*** (0.37, 0.86) | 0.55*** (0.36, 0.83) | 0.64** (0.43, 0.96) | 0.62** (0.41, 0.93) |
| Health-related collective efficacy | . . . | . . . | . . . | 0.65 (0.37, 1.15) | . . . | 0.83 (0.46, 1.51) |
| Social interaction/exchange | . . . | . . . | . . . | . . . | 0.45*** (0.25, 0.80) | 0.47** (0.25, 0.86) |
| Intercept | 0.23*** (0.20, 0.27) | 0.24*** (0.20, 0.30) | 0.24*** (0.20, 0.29) | 0.24*** (0.20, 0.29) | 0.24*** (0.20, 0.29) | 0.24*** (0.20, 0.29) |
| Variance component | 0.08* | 0.06* | 0.05 | 0.04 | 0.04 | 0.04 |
aReference categories = White.
bReference category = private insurance.
*P< .10; **P < .05; ***P < .01
 |
(1) |
 |
(2) |
 |
(3) |
Finally, Figure 1 ▶ displays the predicted probabilities of asthma and other breathing problems for foreign-born Latino residents at selected levels of the percentage of foreign-born residents in the community.
FIGURE 1—
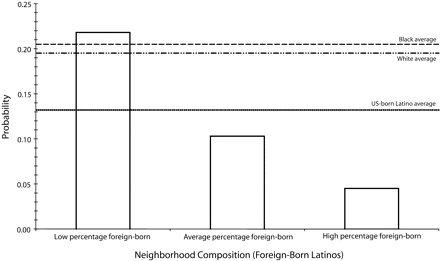
Predicted Probability of Asthma and Other Breathing Problems for Foreign-Born Latino Respondents, by Percentage of Foreign-Born Neighborhood Residents: Chicago, Ill, 1995, 1997, and 1999.
RESULTS
Approximately 18% of the MCIC-MS respondents had been told by a physician that they had asthma or other breathing problems. This result is similar to contemporary reports of asthma prevalence in Chicago, where data indicate that physician-diagnosed asthma approaches 20% in some neighborhoods.27 Just under 19% of Whites reported asthma or other breathing problems compared with 22.2% of Blacks, 14.8% of US-born Latinos, and 7.8% of foreign-born Latinos. Asthma also varied by the population composition of the community. Communities with large foreign-born populations reported that 16.3% of residents had asthma and other breathing problems; communities with medium and small foreign-born populations had rates of 16.8% and 22.2%, respectively.
As shown in Table 1 ▶, the sample was predominately women (59%) and middle aged (mean = 43 years). Whites made up 42% of the sample, African Americans 36%, foreign-born Latinos 10%, US-born Latinos 6%, and other racial/ethnic groups 6%. Education, income, insurance, and access to care values were relatively representative of the Chicago population. Approximately 29% currently smoked, and 20% had been told by a physician that they had a weight problem (both of which exacerbate asthma and other breathing problems). Although we report mean age and included age as a continuous variable in our multivariate models (described later) we did investigate age effects of asthma and other breathing problems by group: ≤ 18–35 (n = 1287), 36–54 (n = 1154), ≥ 55 (n = 750). If an age effect was present, it could mean, for instance, that our data contained more cases of emphysema than asthma at later ages.27 Reports of asthma and other breathing problems across these 3 age groups were strikingly similar at 18.4%, 17.9%, and 18.8%, respectively (analysis using the t test indicated no significant differences between age groups). We also focused on the younger age group (18–35 years) in our multilevel models and found comparable results to those models that included all ages. We still were not able to address the possibility of differential disease composition by age group, but given similar prevalence rates and model results, we elected to examine the full sample.
Multilevel results are presented in the 6 models shown in Table 2 ▶. Model 1 included individual-level factors only and indicates that female gender is predictive of asthma and other breathing problems, whereas Latino status, both US and foreign born, is protective (as is the status of “other” ethnicity). Smoking and a physician-indicated weight problem both significantly increased the odds of reporting asthma and other breathing problems; smokers were approximately 1.3 times more likely to report asthma and other breathing problems and individuals who had a physician-indicated weight problem were approximately 1.8 times more likely to make such a report. Model 2 introduced neighborhood-level variables and indicated that none of the structural indicators—residential stability, concentrated poverty, percentage foreign-born—had a significant effect on the likelihood of reporting asthma and other breathing problems. However, the effect of collective efficacy is significant, which is consistent with previous research13; each 1-standard-deviation increase in the collective efficacy score reduced asthma and other breathing problems by 11% (social interaction and exchange was not a significant predictor of asthma and other breathing problems in separate analyses).
Models 3 through 6 illustrate the results from cross-level interactions between neighborhood factors and the foreign-born Latino effect. Model 3 indicated that the percentage of foreign-born residents in the community interacts with individual-level Latino immigrant status. As the percentage of foreign-born residents increased, the protective effect of foreign-born Latino status was enhanced. This effect remained robust with the inclusion of collective efficacy (Model 4), which did not interact significantly with foreign-born status. By contrast, Model 5 indicated that social interaction and exchange significantly increased the protective effect of foreign-born status on the likelihood of asthma and other breathing problems. Finally, Model 6 included both collective efficacy and social interaction and exchange (adding social interaction and exchange to the model for the intercept as well). Collective efficacy remained insignificant, but both the logged percentage of foreign-born residents and social interaction and exchange variables retained their significance.
Figure 1 ▶ illustrates—using predicted probabilities from Model 6—the relationships among race/ethnicity, asthma and other breathing problems, and the percentage of foreign-born residents in the neighborhood (the latter represented at high [1.5 SD above the mean], average [the mean], and low [1.5 SD below the mean] values). We focused on the experience of foreign-born Latinos, but included the adjusted average effect from Model 6 for the other race/ethnic groups as reference points. We found a distinctly graded effect of the prevalence of asthma and other breathing problems that was dependent on the foreign-born residential composition of the community. Foreign-born Latinos experienced much lower rates of asthma (approximately 5%) when they lived in a neighborhood that had a high percentage of foreign-born residents. Conversely, their counterparts who lived in neighborhoods with a low percentage of foreign-born residents experienced very high rates of asthma and other breathing problems (approximately 22%)—higher, in fact, than the average level of asthma and other breathing problems for the other groups. Thus, the probability of asthma and other breathing problems for foreign-born Latinos appears contingent on the population composition of the community.
DISCUSSION
The relative health advantage of foreign-born Latinos has been observed across age groups, outcomes, and, in some cases, country of origin.2,29,30 Previous research has delineated the individual-level characteristics associated with this health advantage but, to our knowledge, has not examined the neighborhood social context in which these characteristics are embedded nor the interdependence between them. We identified a health benefit from foreign-born Latino status: Latinos born outside the United States experienced appreciably lower rates of asthma and other breathing problems. We found, however, that this benefit observed in the aggregate was heavily dependent on the communities in which foreign-born Latinos reside. When embedded in a neighborhood where the presence of other foreign-born residents is high, the risk of asthma and other breathing problems was abated. Conversely, foreign-born Latinos who lived in communities where there was a low percentage of foreign-born residents experienced the highest rates of asthma and other breathing problems overall. Thus, the Latino advantage with respect to asthma may accrue only when it is socially leveraged.
Consistent with the early theoretical and empirical research of urban sociologists Shaw and McKay,15 homogeneity with respect to ethnicity and immigrant status may increase information exchange through a common language. Shared culture or lifestyle behaviors also may be at play.31,32 We found divergent experiences by neighborhood context after the introduction of individual-level behavioral factors associated with asthma and other breathing problems (e.g., smoking, weight problem). Thus, the role of community and cultural supports may not only influence individual-level behaviors but may also affect health in their own right. Collective efficacy, found to be important to asthma rates in previous work,13 was not as important to the health of foreign-born Latinos as was the level of social interaction and exchange. Collective efficacy may operate differently for Latinos or it may not have the immediate or intimate effect that social networks provide.33 Communities that have limited social ties could attenuate the health benefit of immigrant status and offer further evidence that the Latino paradox is context dependent. Importantly, social network interaction and exchange does not explain the effect of percentage foreign born; rather, the effect of both characteristics suggests that neighborhood factors may be additive. A further implication of this finding is that analyses of the health advantage for foreign-born Latinos fail to take into account neighborhood context may substantially underestimate that benefit for immigrants who reside in ethnic enclaves.
Future analyses will explore differences by country of origin, given that migration patterns may differ across Chicago neighborhoods. For instance, Latinos who reside in communities that have a low percentage of foreign-born residents may be more vulnerable to asthma and other respiratory conditions. With respect to socioeconomic status, we did not find evidence that foreign-born Latinos who lived in communities with a low percentage of foreign-born residents were more disadvantaged when it comes to basic economic and demographic characteristics. Indeed, if anything, the foreign-born Latinos in communities of fewer foreign-born residents were more advantaged than were their counterparts in communities that had a higher percentage of foreign-born residents. The characteristics we considered may omit an important predictor of asthma and other breathing problems, but the overall profile suggests comparability or marginal advantage for foreign-born Latinos in communities of fewer foreign-born residents. On a related note, most Latinos in Chicago are Mexican (70.4%),34 so another extension of this work will focus on the asthma experience among Mexicans. Preliminary analyses of these data indicate that results from the Mexican sub-sample are consistent with those for all Latinos (results available from first author on request). Finally, additional analyses will incorporate alternative assessments of community, including constructs to assess specific characteristics of ethnic enclaves.
Some caveats merit consideration. First, our outcome was a composite measure of respiratory conditions. Asthma, bronchitis, emphysema, and other breathing disorders differ in etiology, so they also may differ in the extent to which they are affected by neighborhood factors; the role of neighborhood in the onset or trajectory of these respiratory conditions could vary in important ways. Future data collection efforts would benefit from a decomposition of these conditions so that neighborhood structural and social process measures could be examined for each. Second, reports of respiratory conditions are contingent upon a clinician’s evaluation. Even though we controlled for regular source of care in our models, this type of question may disproportionately underestimate the prevalence of asthma for those whose interaction with the medical care system is intermittent. Third, our study was confined to the City of Chicago, so the ability to generalize is limited. Analyses from other urban centers that have prominent Latino enclaves would allow for a richer understanding of the enclave experience and, depending upon availability of data, could address the independent mechanisms relevant for a host of respiratory conditions.
The Latino population is the fastest growing and largest population subgroup in the United States.35 Attention to the context in which Latinos reside could provide important insights into trajectories of acute and chronic conditions. The divergent experience of foreign-born Latinos illustrates that community is critical to shaping health. Research of this form contributes to our understanding of social capital and the extent to which it aids in ameliorating threats to respiratory health and, potentially, to other conditions. Knowledge of the community and its characteristics may provide the foundation for initiatives meant to disseminate information and address concerns about prevention, possible triggers, and treatment of asthma and other respiratory conditions.
Acknowledgments
Support for this research was provided by the National Institute on Aging and the Office of Behavioral and Social Sciences Research (grant R01AG022488).
We thank Robert Sampson, Felton Earls, and members of the Project on Human Development in Chicago Neighborhoods for providing access to the community survey, and the Metropolitan Chicago Information Center for access to the metro survey. We also thank David Meltzer for comments on an earlier version of this article and Sandra Thomas for her expertise in describing Chicago’s asthma prevalence.
Human Participant Protection This research was approved by the institutional review board at The University of Chicago.
Peer Reviewed
Contributors K. A. Cagney developed the research question, wrote the article, and identified analyses to be conducted. C. R. Browning contributed to article development and statistical analyses. D. M. Wallace conducted statistical analyses. All authors provided revisions to article drafts.
References
- 1.Cobas JA, Balcazar H, Benin MB, Keith VM, Chong Y. Acculturation and low-birthweight infants among Latino women: a reanalysis of HHANES data with structural equation models. Am J Public Health. 1996;86:394–396. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Markides KS, Coreil J. The health of Hispanics in the southwestern United-States - an epidemiologic paradox. Public Health Rep. 1986;101:253–265. [PMC free article] [PubMed] [Google Scholar]
- 3.Patel KV, Eschbach K, Ray LA, Markides KS. Evaluation of mortality data for older Mexican Americans: implications for the Hispanic paradox. Am J Epidemiol. 2004;159:707–715. [DOI] [PubMed] [Google Scholar]
- 4.Palloni A, Arias E. Paradox lost: explaining the Hispanic adult mortality advantage. Demography. 2004;41:385–415. [DOI] [PubMed] [Google Scholar]
- 5.Morales LS, Lara M, Kington RS, Valdez RO, Escarce JJ. Socioeconomic, cultural, and behavioral factors affecting Hispanic health outcomes. J Health Care Poor Underserved. 2002;13:477–503. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.LeClere FB, Rogers RG, Peters KD. Ethnicity and mortality in the United States: individual and community correlates. Soc Forces. 1997;76:169–198. [Google Scholar]
- 7.Eschbach K, Ostir GV, Patel KV, Markides KS, Goodwin JS. Neighborhood context and mortality among older Mexican Americans: is there a barrio advantage? Am J Public Health. 2004;94:1807–1812. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Sperber K, Ibrahim H, Hoffman B, Eisenmesser B, Hsu H, Corn B. Effectiveness of a specialized asthma clinic in reducing asthma morbidity in an inner-city minority population. J Asthma. 1995;32:335–343. [DOI] [PubMed] [Google Scholar]
- 9.Corn B, Hamrung G, Ellis A, Kalb T, Sperber K. Patterns of asthma death and near-death in an inner-city tertiary care teaching hospital. J Asthma. 1995;32:405–412. [DOI] [PubMed] [Google Scholar]
- 10.Diaz T, Sturm T, Matte T, et al. Medication use among children with asthma in East Harlem. Pediatrics. 2000;105:1188–1193. [DOI] [PubMed] [Google Scholar]
- 11.Findley S, Lawler K, Bindra M, Maggio L, Penachio MM, Maylahn C. Elevated asthma and indoor environmental exposures among Puerto Rican children of East Harlem. J Asthma. 2003;40:557–569. [DOI] [PubMed] [Google Scholar]
- 12.Homa DM, Mannino DM, Lara M. Asthma mortality in U.S. Hispanics of Mexican, Puerto Rican, and Cuban heritage, 1990–1995. Am J Respir Crit Care Med. 2000;161(2 Pt 1):504–509. [DOI] [PubMed] [Google Scholar]
- 13.Cagney KA, Browning CR. Exploring neighborhood-level variation in asthma and other respiratory diseases—the contribution of neighborhood social context. J Gen Intern Med. 2004;19:229–236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Gold DR, Wright R. Population disparities in asthma. Annu Rev Public Health. 2005;26:89–113. [DOI] [PubMed] [Google Scholar]
- 15.Shaw CR, McKay HD. Juvenile Delinquency and Urban Areas: A Study of Rates of Delinquents in Relation to Differential Characteristics of Local Communities in American Cities. Chicago, Ill: University of Chicago Press; 1969.
- 16.Sampson RJ, Raudenbush SW, Earls F. Neighborhoods and violent crime: a multilevel study of collective efficacy. Science. 1997;277:918–924. [DOI] [PubMed] [Google Scholar]
- 17.Waters MC, Eschbach K. Immigration and ethnic and racial-inequality in the United States. Annu Rev Sociol. 1995;21:419–446. [Google Scholar]
- 18.Portes A, Truelove C. Making sense of diversity: recent research on Hispanic minorities in the United States. Annu Rev Sociol. 1987;13:359–385. [Google Scholar]
- 19.Sanders JM, Nee V. Limits of ethnic solidarity in the enclave economy. Am Sociol Rev. 1987;52:745–773. [Google Scholar]
- 20.Browning CR, Cagney KA. Neighborhood structural disadvantage, collective efficacy, and self-rated physical health in an urban setting. J Health Soc Behav. 2002;43:383–399. [PubMed] [Google Scholar]
- 21.Patrick DL, Erickson P. Health Status and Health Policy: Allocating Resources to Health Care. New York, NY: Oxford University Press; 1993.
- 22.Naureckas ET, Wolf RL, Trubitt MJ, et al. The Chicago Asthma Consortium: a community coalition targeting reductions in asthma morbidity. Chest. 1999; 116(4 Suppl 1):190S–193S. [DOI] [PubMed] [Google Scholar]
- 23.Thomas S. Telephone surveys for asthma surveillance: The Chicago Respiratory Health Survey. Paper presented at: A Public Health Response to Asthma. February 15–17, 2000; Atlanta, GA.
- 24.Diez-Roux AV. Multilevel analysis in public health research. Annu Rev Public Health. 2000;21:171–192. [DOI] [PubMed] [Google Scholar]
- 25.Snijders T, Bosker R. Multilevel Analysis: An Introduction to Basic and Advanced Multilevel Modeling. London, England: Sage; 1999.
- 26.Raudenbush SW, Bryk AS. Hierarchical Linear Models: Applications and Data Analysis Methods. Thousand Oaks, Calif: Sage; 2002.
- 27.Whitman S, Williams C, Shah AM. Sinai Health System’s Community Health Survey: Report 1. Chicago, Ill: Sinai Health System; 2004.
- 28.Malik A, Saltoun CA, Yarnold PR, Grammer LC. Prevalence of obstructive airways disease in the disadvantaged elderly of Chicago. Allergy Asthma Proc. 2004;25:169–173. [PubMed] [Google Scholar]
- 29.Elo I, Turra C, Kestenbaum B, Ferguson BR. Mortality among elderly Hispanics in the United States: past evidence and new results. Demography. 2004;41:109–128. [DOI] [PubMed] [Google Scholar]
- 30.Abraido-Lanza AF, Dohrenwend BP, Ng-Mak DS, Turner JB. The Latino mortality paradox: a test of the “salmon bias” and healthy migrant hypotheses. Am J Public Health. 1999;89:1543–1548. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Fitzpatrick K, Lagory M. Unhealthy Places: The Ecology of Risk in the Urban Landscape. New York, NY: Routledge; 2000.
- 32.Sorlie PD, Backlund E, Johnson NJ, Rogot E. Mortality by Hispanic status in the United States. JAMA. 1993;270:2464–2468. [PubMed] [Google Scholar]
- 33.Klinenberg E. Heatwave: A Social Autopsy of Disaster in Chicago. Chicago, Ill: The University of Chicago Press; 2002.
- 34.Guzman B. The Hispanic Population. Washington, DC: US Census Bureau; 2001.
- 35.Greico EM, Cassidy RC. Overview of Race and Hispanic Origin 2000. Washington, DC: US Census Bureau; 2001.


